Translate this page into:
Advances and trends in multiligament injuries of the knee relevant to low-resource settings

*Corresponding author: Michael F. G. Held, Department of Orthopedic Surgery, University of Cape Town, Groote Schuur Hospital H49 OMB, Cape Town, South Africa. michael.held@uct.ac.za
-
Received: ,
Accepted: ,
How to cite this article: Held MF, North D, Von Bormann RB, Wascher DC, Richter DL, Schenck RC. Advances and trends in multiligament injuries of the knee relevant to low-resource settings. J Arthrosc Surg Sport Med 2020;1(1):118-125.
Abstract
Recent advances in the management of multiligament knee injuries have led to improvements in diagnosis and management and allowed enhanced understanding of the biomechanics of ligament reconstructions. Most studies arise from subspecialist knee centers in high-income countries and can inform global strategies, but each patient encounter and environment is unique and not all recommendations may be feasible in every setting. For ligamentous injuries, the gold standard is acute arthroscopic, single-stage ligament reconstruction, although this is not always possible in the limited resource setting (LRS). For these circumstances, non-operative management, although rarely promoted, may be preferred in selected patients. Furthermore, acute surgery relies on adequate post-operative physiotherapy, otherwise a delayed surgical approach should be considered. Reconstruction remains the gold standard, but acute repair is an option for medial collateral and posterior cruciate ligaments and for avulsion fractures. For a vascular examination, a careful clinical assessment and routine angiography should be done in LRS. Due to the heterogeneity of injury and patient profile, outcomes vary widely and need to be interpreted in the context of the surgical setup. The main complications of these injuries are stiffness, residual laxity, and surgical site infections. Future trends will need to include a global perspective and provide solutions for surgeons in various parts of the world.
Keywords
Knee dislocation
Multiple knee ligament injury
Multiligament knee injuries
Limited resource setting
INTRODUCTION
Multiligament knee injuries (MLKIs) have been described as the disruption of two or more of the main ligaments of the knee[1,2] caused either by a dislocation or substantial subluxation. Although rare, it is a devastating injury with associated damage to other structures and often results in long- term disability. The priority in MLKIs is to manage limb threatening injuries to large vessels and soft-tissue integument; however, ipsilateral fractures and nerve injuries can further complicate treatment. The recovery of knee function is mainly dependent on the stability and motion of the knee joint, which is determined by capsular-ligamentous integrity. Schenck (ICL 1994) has proposed a widely used system, which was later modified by Wascher[3] [Table 1] to classify these injuries based on the anatomic structures torn. Yet, the complex trauma load of orthopedic and non-orthopedic injuries, as well as certain patient factors, creates heterogeneous injury patterns which make controlled research trials difficult. This results in the best available research being descriptive, retrospective studies with low level of evidence.
| Type | Description |
|---|---|
| I | Injury to a single cruciate ligament (ACL or PCL), variable collateral ligament involvement |
| II | Injury to both cruciate ligaments (ACL and PCL) with intact collaterals |
| IIIM | Injury to the ACL, PCL, and medial collateral ligament and posteromedial corner |
| IIIL | Injury to the ACL, PCL, and lateral collateral ligament and posterolateral corner |
| IV | Injury to the ACL, PCL, medial collateral ligament and posteromedial corner, and lateral collateral ligament andposterolateral corner |
| V | Multiligament knee injury with periarticular fracture |
| C | Modifier for arterial injuries |
| N | Modifier for nerve injuries |
ACL: Anterior cruciate ligament, PCL: Posterior cruciate ligament
This article summarizes the key points of the current literature on MLKIs, which mostly originates from high-income countries and sub-specialized knee centers. It specifically focuses on associated injuries, conservative and operative treatment options, timing and staging of surgery, reconstruction techniques, surgical repair and graft options, as well as patient outcomes. Although important advances have been made in knee arthroscopy, ligament reconstruction and patient management, recommendations are not always applicable in settings with limited resources available. Challenges encountered in these situations include long delays to presentation, as well as the lack of sufficient access to operating room time, arthroscopic equipment, newer fixation devices, and allografts. Patients are often uninsured; work informally as manual laborers and their access to physiotherapy is very limited. This article aims to provide an approach for surgeons practicing in these limited resource settings (LRS).
ASSOCIATED INJURIES
The majority of MLKIs occur as a result of high-velocity trauma and severe injuries to the head, chest, and abdomen as well as remote fractures are often seen in these patients. A thorough prioritized trauma evaluation is mandatory in all patients with high-velocity MLKIs.[4-6] The momentary deformity during a knee dislocation causes significant traction forces on important juxta-articular soft-tissue structures [Figure 1].
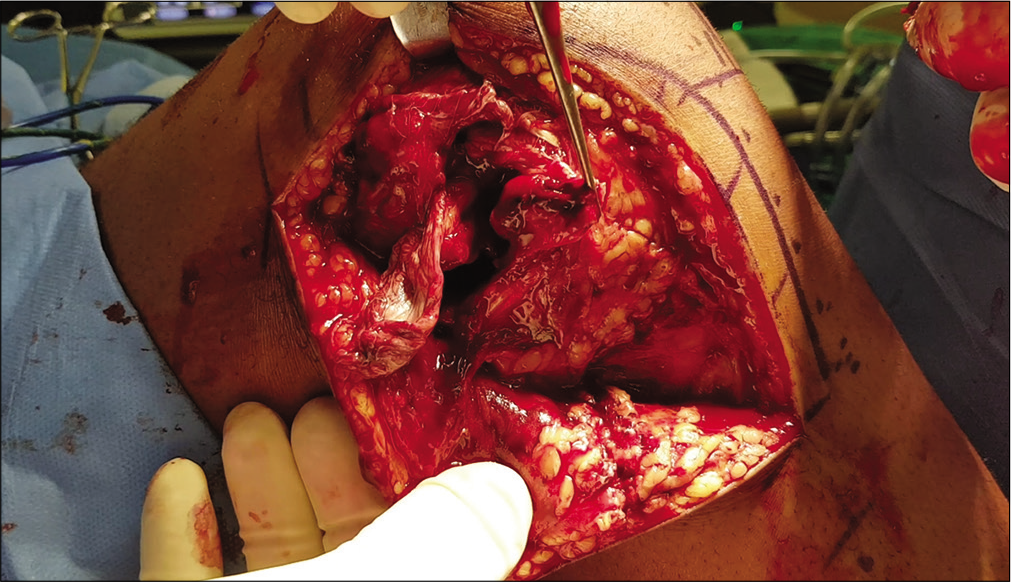
- Intraoperative image of a knee dislocation after skin incision. Extensive damage to the skin and soft-tissue integument as well as ligamentous structures is caused by the momentary deformity.
After excluding life-threatening injuries, the limb should be assessed for open wounds, neurovascular injuries, and extra- articular fractures [Figure 2].
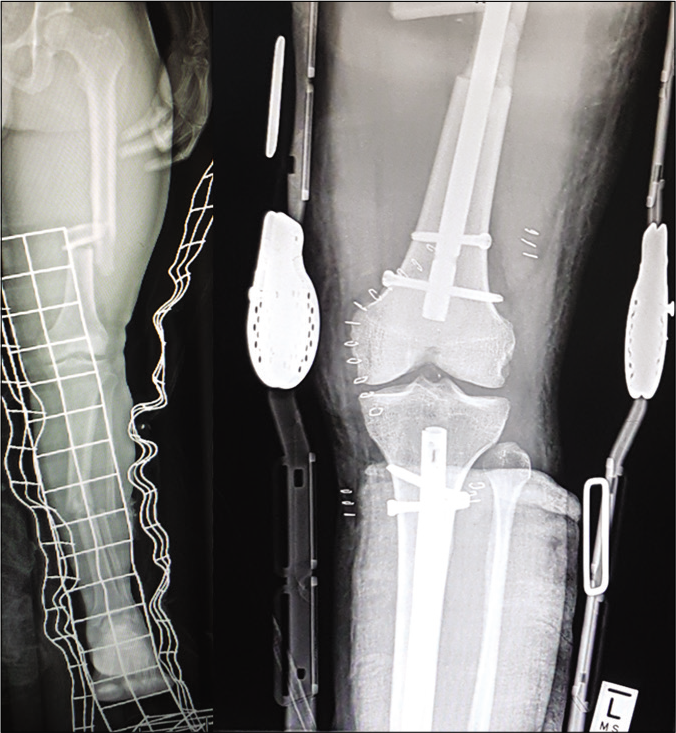
- AP X-ray of a patient with a multiligament knee injury and associated ipsilateral tibia and femur fractures. The knee injury is treated in a range of motion brace as the fractures take priority over ligamentous reconstruction.
The reported prevalence of associated vascular injuries ranges from 3% to 64%.[3,5] Urgent reperfusion is key as the amputation rate can reach up to 86% when it is delayed for more than 6–8 h post-injury.[7,8] Although vascular compromise is the single most important red flag to exclude, the diagnostic workup remains controversial. Many centers have adopted selective angiography as a gold standard, which recommends further investigation only when the ankle-brachial (blood pressure) index is <0.8, or when there is an expanding popliteal hematoma.[9-12] In many centers, this is not feasible due to the lack of sufficiently trained staff available for frequent reassessments and future trends will likely see hospitals adjust these protocols. Routine angiography has value as it can categorically exclude vascular disruption, in particular intimal flap tears which can lead to delayed occlusion. A single-shot arterial, on-table angiogram before surgical exploration, is a low-cost alternative to evaluate limbs with an absent pulse, active bleeding, expanding hematoma, a popliteal bruit, or distal ischemia.[13]
Nerve injury is frequently associated with vascular injury and should be seen as a red flag for vascular injury, even with normal ankle-brachial index.[5] Similar to the vessels, the peroneal nerve is also tethered proximally and distal to the knee and is therefore commonly injured with an incidence of 25–35%.[5] Surgically, early neurolysis is recommended to decompress an incomplete injury. Nerve grafts for a segment <6 cm can be considered but the outcomes remain poor.[14] A posterior tibial transfer can treat a disabling foot drop which does not recover after 1 year.[5] Future trends may include an earlier restoration of ankle dorsiflexion before knee ligament reconstruction to improve the initial rehabilitation process. This also avoids knee hyperextension associated with a foot drop, which can potentially lead to increased load on ligament reconstruction.
CONSERVATIVE TREATMENT VERSUS SURGICAL MANAGEMENT
Overall, literature shows improved outcomes for MLKIs treated surgically compared to those treated non-operatively.[15,16] In a comprehensive review, patients treated surgically had improved functional outcome measures, developed fewer contractures and residual instability, and returned to work and sporting activity faster.[15] For these reasons, most surgeons only consider conservative management for patients who are frail or unfit for surgery. However, we realize that non-operative management is commonly used in settings with limited resources, and foresee a trend that it will begin to receive more attention in a specialized patient population. Acceptable outcomes [Figure 3] can be achieved with closed reduction and immobilization for a period of 4–6 weeks in patients who comply with non-weight bearing. But regular radiographic follow-up is important to assess for loss of reduction [Figure 4].

- Images of a patient demonstrating crouching and jumping 4 months after his knee dislocation as shown on the X-ray. This was an acceptable knee function to the patient who declined further surgical intervention.
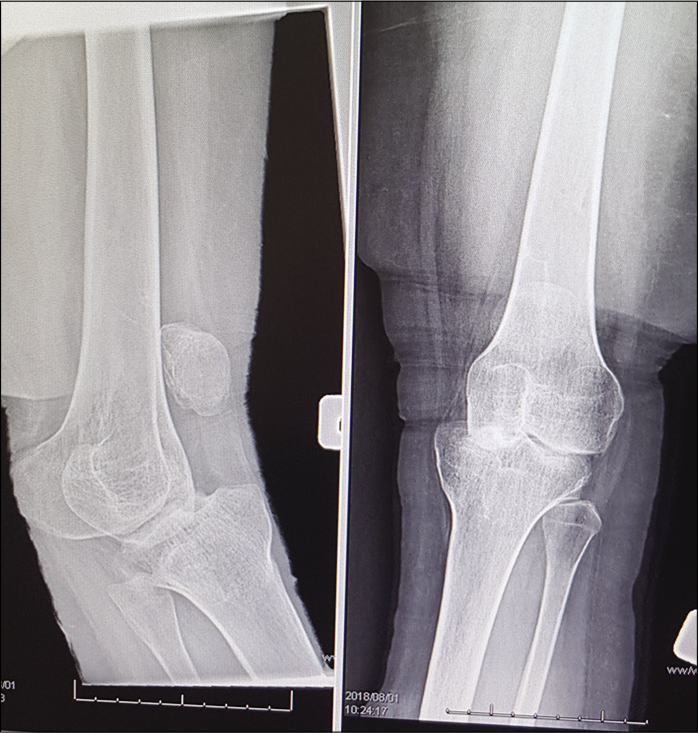
- X-rays of a chronic knee dislocation treated in a rural South African hospital. Regular radiographic must be done when treating patients nonoperatively to avoid this at all costs.
Immobilization in the form of a rigid cast should also not exceed 6 weeks as it can lead to permanent loss of motion.[17] In the morbidly obese, open injuries, vascular injuries, and patients unable to comply with rehabilitation protocols, definitive surgical treatment can take the form of an external fixator for 4–6 weeks. A manipulation under anesthesia with or without arthroscopic lysis of adhesions at the time of removal usually improves range of motion, but care should be taken to avoid complications that may be associated with pin site sepsis, especially if further ligament reconstruction is planned.
TIMING AND STAGING OF SURGERY
The timing of surgical reconstruction in MLKIs is controversial and both acute and delayed management may lead to similar outcomes.[18] Acute surgery is arbitrarily defined as performing surgery within 3 weeks from the date of injury. After this time frame, scarring may obscure the injured ligaments and peroneal nerve, making soft- tissue planes more challenging to define and nerve dissection similarly more difficult. The advantage of acute reconstruction or repair of ligaments leads to an earlier restoration of normal joint kinematics and in combination with early post-operative mobilization protocols; this may lead to better functional outcomes.[19] It also avoids the increased incidence of meniscal and cartilage injuries associated with the delayed surgery.[6,20] The disadvantage of acute surgery is the increased risk of residual instability associated with repairs,[21,22] especially of the posterolateral corner (PLC), and increased risk of arthrofibrosis.[23]
Delayed reconstruction, on the other hand, may allow some extra-articular ligaments to heal and full range of motion to be recovered before surgery. Overall, most authors agree that early post-operative rehabilitation is the single most important factor influencing outcome. Thus, future trends will likely focus on improving rehabilitation and base the decision of acute versus delayed management on the access to and quality of physiotherapy. As such, for most LRS, delayed management is a common strategy to avoid stiffness and allows collaterals and the posterior cruciate ligament (PCL) to potentially heal which will avoid additional ligament reconstruction in some patients.
TECHNIQUES
Repair
Outcomes for ligamentous repair in MLKIs are commonly reported to be inferior to reconstruction.[24,25] Yet, bony avulsions form an exception for which repair is favored[26] and some suggest to repair ligaments acutely when they are torn at their insertions.[27]
Furthermore, collateral ligaments have an acceptable healing capacity although with distinct differences for the medial and lateral side. For the lateral side of the knee, the results for primary repair alone are poor with a recent study showing a 38% failure rate for lateral repair with delayed cruciate reconstruction.[21] Specifically in MLKI, with MCL, and PCL injuries, good results have been demonstrated with repair.[25] This should however be undertaken early as healing potential decreases with time. The renewed interest in repair has coincided with an increase in the augmentation of primary repairs with synthetic augments or “internal bracing” [Figure 5].

- Arthroscopic image of a synthetic augmentation (braded suture tape) for a posterior cruciate ligament injury.
The proposed advantages are that smaller tunnels are needed, native anatomy is preserved, and donor site morbidity is eliminated without the need of autografts.[28,29] However, the literature consists largely of surgical techniques and case series,[30] with limited biomechanical or clinical evidence supporting their use. Future trends will therefore likely further explore the treatment of MLKIs with repair and internal bracing, especially for MCL and PCL injuries. For LRS this is an attractive option as surgical time is reduced by eliminating graft harvest and stability might be improved compared to repair alone.
Reconstruction
Although anatomic ligament reconstruction is accepted by many as the gold standard, this is largely based on biomechanical studies with limited clinical evidence available on their use in the setting of MLKIs. The use of graft options, such as autograft, allograft, and synthetic ligaments depends on availability, surgical preference and technique, and the number of ligaments requiring reconstruction.[31] Autografts can be harvested from the affected or contralateral leg and include hamstring tendons, bone-patella tendon-bone, and quadriceps tendon with or without a bone block. Recently, the use of peroneus longus [Figure 6] as an autograft option was reported as an acceptable option for anterior cruciate ligament (ACL), PCL, and PLC reconstructions.[32,33]

- Cadaver specimen with harvested peroneus longus tendon, demonstrating a long graft with large diameter.
Allografts have been used successfully for MLKIs, which eliminates donor site morbidity and reduces operating time.[31] However, there is an increased risk for disease transmission, increased cost, limited availability in many areas, and higher failure rates when irradiated grafts are used.[31] Earlier generation synthetic ligaments have led to high failure rates and synovitis.[34,35] However, newer synthetic ligaments, such as the ligament augmentation and reconstruction system, have decreased failure rates, sterile effusions, and synovitis with acceptable outcomes in acute MLKIs.[34,35]
Cruciate ligaments
At present, a single bundle anatomic ACL reconstruction is favored. This can be performed in a single-stage with concomitant ligament reconstructions or in a staged manner after healing of PCL and collateral ligament repair/ reconstruction.
For PCL reconstructions, there is currently debate between the use of single bundle and double bundle techniques. For single bundle reconstructions tibial inlay and transtibial techniques are used, with no significant differences in outcomes.[36] Double bundle techniques aim to reconstruct both the anterolateral and posteromedial bundles which lead to improved knee kinematics and rotational as well as posterior stability[37,38] in biomechanical studies. However, there is no difference to date in clinical outcomes between the two techniques.[39,40] Double bundle reconstruction techniques typically require the use of an additional graft which may be limited in the LRS.
Medial collateral ligament (MCL) and posteromedial corner (PMC)
The primary medial stabilizers of the knee include the superficial MCL, posterior oblique ligament (POL), and the deep MCL. They function as primary and secondary static stabilizers to valgus, and external and internal rotation.[41] Recently, established anatomic knowledge of the medial side of the knee has advanced the reconstructive options with numerous techniques. For the PMC, we prefer to use a doubled semitendinosus autograft to reconstruct the superficial MCL and an imbrication of the posteromedial capsule to tighten the POL.[42] This technique avoids the need for an additional POL graft and similarly lowers the risk of tunnel collision in the MLKI reconstruction setting. A recent biomechanical study (McIver et al., presented at the 2020 Annual Orthopaedic Research Society Meeting in Phoenix, USA) showed this had similar improved knee stability when compared to the LaPrade and Wijdicks MCL reconstruction technique[41] using two free grafts. It also indicated that it may provide better valgus stability throughout full knee range of motion while avoiding potential limitations of graft loosening or tunnel collision.
Lateral collateral ligament (LCL) and PLC
Multiple techniques have been described to reconstruct the LCL or PLC [Figure 7]. These can be broadly divided into non-anatomical or anatomical techniques.[21,43] The non-anatomical techniques can be fibular based or tibial based two-tailed reconstructions. The anatomical techniques reconstruct the LCL, popliteofibular ligament, and the popliteus tendon.[43] The anatomical techniques have been shown to be biomechanically superior, however, with similar clinical outcomes.[21,43] Recently, newer anatomic reconstruction techniques have been described utilizing a single autograft, either semitendinosus or peroneus longus.[44,45] However, biomechanical and clinical testing is required to validate these methods.

- Schematic drawing of various techniques to reconstruct the posterolateral corner. Blue: Larson’s loop. Green: Arciero. Orange: LaPrade. Orange far right: Biceps tenodesis.
The future trends in graft choice and ligament reconstruction will likely explore infrequently used autograft options and optimize techniques to improve biomechanics with the least graft material necessary. Especially for LRS with limited availability or quality of allograft, single bundle autograft reconstruction with simple and inexpensive fixation methods will remain the treatment choice for most surgeons. PLC reconstructions can be performed using techniques described by LaPrade or Arciero. A recent biomechanical study[46] showed these to be equally effective; however, the Arciero reconstruction requires only a single semitendinosus graft, whereas LaPrade’s technique requires an additional gracilis graft. Another option for the PLC is performing a biceps tenodesis. Fanelli and Edson have reported good results with this procedure.[47]
OUTCOMES
Following surgical treatment of MLKIs, good functional outcomes and ligament stability are reported at short to medium term follow-up.[48-50] However, it is critical to discuss expectations and goals with the patient, understanding that this will never be a “normal” knee. Despite good functional outcomes, there is a high incidence of osteoarthritis developing in the affected knee, ranging from 23% to 87%.[49,50] Factors associated with an increased risk of osteoarthritis are high energy injuries,[48] age over 30 years,[50] and associated cartilage or meniscal injuries.[51] There is a considerable risk of complications in MLKIs ranging from 6% to 73.9%.[1,24,48,52] The incidence of surgical complications varies depending on the severity of the injury, the treatment used, and patient factors such as obesity [Figure 8].[30,49] Some of the more commonly described complications include neurovascular injury, infection, arthrofibrosis, deep venous thrombosis, recurrent instability, and compartment syndrome. Post-operative infections occur in up to 17% of patients,[24,52] and is associated with increased surgical time, obesity, and diabetes mellitus.[51]

- Obesity in patients with knee dislocations is one of the most important risk factors for complications and poor outcome in knee dislocations. Patients are often multimorbid, diabetic, legs cannot be braced, and non-weight bearing is a challenge.
Perioperative antibiotics should be routinely utilized. Post- operative arthrofibrosis is also common, with up to 20–25% of cases requiring either manipulation under anesthesia or arthroscopic lysis of adhesions. Future studies may look at strategies, such as the he use of indomethacin, to try to reduce the incidence of arthrofibrosis. Patients with more than 2 ligaments injured and a surgical intervention within the first 3 weeks have a significantly higher risk of knee stiffness.[51] Deep vein thrombosis and pulmonary embolus are another non-orthopedic complication after a surgical intervention in MLKIs which can be limited with routine thromboprophylaxis with aspirin or enoxaparin.[53]
CONCLUSION
This article provided an overview of recent advances in the management of MLKIs. Vascular examination should include a careful clinical assessment and routine angiography, if available. A large portion of peroneal nerve injuries need tendon transfer surgery which may be done before or after a knee ligament reconstruction. Non- operative management is acceptable for selected patients and in certain circumstances. Acute surgery needs optimal postoperative physiotherapy; otherwise, delayed surgical treatment should be done. Ligament reconstruction is the treatment of choice, but in bony or ligamentous avulsions, early repair can be considered with good healing potential. Current advances should be critically assessed and adopted for the management of MLKIs in LRS to nurture future trends with a global perspective.
References
- Surgical treatment of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23:2983-91.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of combined PCL-ACL medial and lateral side injuries (global laxity): Surgical technique and 2-to 18-year results. J Knee Surg. 2012;25:307-16.
- [CrossRef] [PubMed] [Google Scholar]
- High-velocity knee dislocation with vascular injury. Treatment principles. Clin Sports Med. 2000;19:457-77.
- [CrossRef] [Google Scholar]
- Staged management of knee dislocation in polytrauma injured patients. Injury. 2013;44:S40-5.
- [CrossRef] [Google Scholar]
- Demographics and injuries associated with knee dislocation: A prospective review of 303 patients. Orthop J Sports Med. 2017;5:2325967117706521.
- [CrossRef] [PubMed] [Google Scholar]
- Management of multiligament knee injuries. EFORT Open Rev. 2020;5:145-55.
- [CrossRef] [PubMed] [Google Scholar]
- What is the frequency of vascular injury after knee dislocation? Clin Orthop Relat Res. 2014;472:2615-20.
- [CrossRef] [PubMed] [Google Scholar]
- Knee dislocations with vascular injury: Outcomes in the lower extremity assessment project (LEAP) study. J Trauma Acute Care Surg. 2007;63:855-8.
- [CrossRef] [PubMed] [Google Scholar]
- Knee dislocation and vascular injury: 4 year experience at a UK major trauma centre and vascular hub. Injury. 2016;47:752-6.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular injuries following knee dislocation. J Knee Surg. 2020;33:351-6.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular injuries in knee dislocations: The role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86:910-5.
- [CrossRef] [PubMed] [Google Scholar]
- Can vascular injury be appropriately assessed with physical examination after knee dislocation? Clin Orthop Relat Res. 2016;474:1453-8.
- [CrossRef] [PubMed] [Google Scholar]
- High rate of popliteal artery injuries and limb loss in 96 knee dislocations. SA Orthop J. 2016;15:72-6.
- [CrossRef] [Google Scholar]
- Treatment of peroneal nerve injuries in the multiligament injured/dislocated knee. J Knee Surg. 2016;29:287-92.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of operative and nonoperative treatment of multiligament knee injuries: An evidence-based review. Sports Med Arthrosc Rev. 2011;19:167-73.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30:718-27.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic dislocation of the knee. A report of forty-three cases with special reference to conservative treatment. J Bone Joint Surg Br. 1972;54:96-102.
- [CrossRef] [PubMed] [Google Scholar]
- Early versus delayed surgery results in similar outcomes following multiligament knee injury; a prospective cohort. Orthop J Sports Med. 2019;7:2325967119S00299.
- [CrossRef] [Google Scholar]
- Early surgery of multiligament knee injuries may yield better results than delayed surgery: A systematic review. J ISAKOS. 2019;4:26-32.
- [CrossRef] [Google Scholar]
- Delay in surgical management of multiligament knee injuries is associated with cartilage and meniscus injury. Orthop J Sports Med. 2019;7:2325967119S00300.
- [CrossRef] [Google Scholar]
- A systematic review of the outcomes of posterolateral corner knee injuries, Part 1: Surgical treatment of acute injuries. Am J Sports Med. 2016;44:1336-42.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the posterolateral corner of the knee. Arthroscopy. 2005;21:1051-9.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple-ligament knee injuries: A systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91:2946-57.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic and management strategies for multiligament knee injuries: A critical analysis review. JBJS Rev. 2016;4:01874474-20160200000001.
- [CrossRef] [PubMed] [Google Scholar]
- Primary ligament sutures as a treatment option of knee dislocations: A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1502-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of multiligament knee injury: State of the art. J ISAKOS. 2017;2:152-61.
- [CrossRef] [Google Scholar]
- The multiple ligament-injured knee: When is primary repair an option? Knee. 2020;27:173-82.
- [CrossRef] [PubMed] [Google Scholar]
- Repair and augmentation with internal brace in the multiligament injured knee. Clin Sports Med. 2019;38:275-83.
- [CrossRef] [PubMed] [Google Scholar]
- Multiligament repair with suture augmentation in a knee dislocation with medial-sided injury. Arthrosc Tech. 2018;7:e839-43.
- [CrossRef] [PubMed] [Google Scholar]
- Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med. 2018;46:2291-8.
- [CrossRef] [PubMed] [Google Scholar]
- Graft selection in surgicalreconstruction of the multiple-ligament-injured knee. Oper Tech Sports Med. 2003;11:218-25.
- [CrossRef] [Google Scholar]
- Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3552-9.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior cruciate ligament reconstruction with peroneus longus tendon graft: 2-years follow-up. Ann Med Surg. 2019;43:38-43.
- [CrossRef] [PubMed] [Google Scholar]
- Synthetic devices for reconstructive surgery of the cruciate ligaments: A systematic review. Arthroscopy. 2015;31:957-68.
- [CrossRef] [PubMed] [Google Scholar]
- LARS synthetic ligaments for the acute management of 111 acute knee dislocations: Effective surgical treatment for most ligaments. Knee Surg Sports Traumatol Arthrosc. 2018;26:3673-81.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior cruciate ligament: Current concepts review. Arch Bone Joint Surg. 2018;6:8-18.
- [Google Scholar]
- Single-bundle and double-bundle posterior cruciate ligament reconstructions: A systematic review and meta-analysis of 441 patients at a minimum 2 years' follow-up. Arthroscopy. 2017;33:2066-80.
- [CrossRef] [PubMed] [Google Scholar]
- Kinematic analysis of the posterior cruciate ligament, Part 2: A comparison of anatomic single-versus double-bundle reconstruction. Am J Sports Med. 2013;41:2839-48.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of single-bundle and double-bundle isolated posterior cruciate ligament reconstruction with allograft: A prospective, randomized study. Arthroscopy. 2014;30:695-700.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective randomized study comparing arthroscopic single-bundle and double-bundle posterior cruciate ligament reconstructions preserving remnant fibers. Am J Sports Med. 2011;39:474-80.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical technique: Development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. 2012;470:806-14.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of medial instability of the knee. Sports Med Arthrosc Rev. 2015;23:77-84.
- [CrossRef] [PubMed] [Google Scholar]
- Posterolateral corner repair and reconstruction: Overview of current techniques. Ann Joint. 2018;3:89.
- [CrossRef] [Google Scholar]
- Anatomic posterolateral corner reconstruction with autogenous peroneus longus Y graft construct. Arthrosc Tech. 2019;8:e1501-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic posterolateral corner reconstruction using single graft plus adjustable-loop suspensory fixation device. Arthrosc Tech. 2019;8:e301-9.
- [CrossRef] [PubMed] [Google Scholar]
- A biomechanical comparison of the Arciero and Laprade reconstruction for posterolateral corner knee injuries. Orthop J Sports Med. 2019;7:2325967119838251.
- [CrossRef] [PubMed] [Google Scholar]
- Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2-to 10-year follow-up. Arthroscopy. 2004;20:339-45.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome after knee dislocations: A 2-9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17:1013-26.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term followup of surgically treated knee dislocations: Stability restored, but arthritis is common. Clin Orthop Relat Res. 2014;472:2712-7.
- [CrossRef] [PubMed] [Google Scholar]
- High prevalence of knee osteoarthritis at a minimum 10-year follow-up after knee dislocation surgery. Knee Surg Sports Traumatol Arthrosc. 2017;25:3914-22.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical outcomes after traumatic open knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2009;17:1027-32.
- [CrossRef] [PubMed] [Google Scholar]
- Single-stage multiple-ligament knee reconstructions for sports-related injuries: Outcomes in 194 patients. Am J Sports Med. 2019;47:2563-71.
- [CrossRef] [PubMed] [Google Scholar]
- Low frequency of symptomatic venous thromboembolism after multiligamentous knee reconstruction with thromboprophylaxis. Clin Orthop Relat Res. 2014;472:2705-11.
- [CrossRef] [PubMed] [Google Scholar]






