Translate this page into:
J arch: A contemporary soft-tissue landmark for anatomic placement of femoral tunnel in remnant-preserving anterior cruciate ligament (ACL) reconstruction
*Corresponding author: Vatsal Khetan, Sports Medicine, Sportsmed Mumbai, Mumbai, Maharashtra, India. drvatsalortho2015@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khetan V, Thakkar S, Usman S, Sabnis B, Joshi A. J arch: A contemporary soft-tissue landmark for anatomic placement of femoral tunnel in remnant-preserving anterior cruciate ligament (ACL) reconstruction. J Arthrosc Surg Sports Med 2022;3:78-83.
Abstract
Objectives:
Femoral tunnel placement is a critical step in ACL reconstruction surgery. Surgeons usually end up clearing the soft tissue to access the bony landmarks. Biological ACL reconstruction with preservation of soft tissue can be done with reliable soft tissue landmarks. Our objective is to assess the reliability of a soft tissue landmark- femoral ACL remnant, for appropriate femoral tunnel placement in soft tissue preserving ACL reconstruction.
Materials and Methods:
This study was a retrospective analysis of prospectively collected data of 40 consecutive patients who underwent primary ACL reconstruction in January 2018 by a single surgeon. An inverse J shaped tissue arch was identified and used as soft tissue landmark for anatomic placement of femoral tunnel. This arch was a part of femoral ACL remnant. MRI films were examined post-operatively to determine the position of the femoral tunnel. Postoperatively, MRI of these patients were reviewed to evaluate the femoral tunnel position in terms of depth and height from the proximal condylar surface and notch roof, respectively.
Results:
The center of the femoral tunnel was found to be at a mean depth of 27.12 ± 2.2% from the proximal condylar surface (parallel to Blumensaat’s line) and a mean height of 30.96 ± 2.75% from the notch roof (perpendicular to Blumensaat’s line), which is at par with previously defined data given by various studies.
Conclusion:
J arch can be used as a dependable soft tissue landmark and a guide for the anatomic placement of femoral tunnel in biological ACL Reconstruction.
Keywords
Femoral tunnel placement
J arch
Biological reconstruction
Remnant preserving
INTRODUCTION
Anterior cruciate ligament (ACL) reconstruction is a fairly successful intervention with a reported medium to the long-term success rate of 80–98%.[1] However, this success largely depends on many factors such as the operating technique, operating surgeon’s expertise, the position of the graft, graft choice, graft fixation, and post-operative rehabilitation.[2]
One of the prime steps in arthroscopic ACL reconstruction (ACL R) for the anatomical placement of the graft is the proper positioning of an appropriate femoral tunnel.[3] Not only is this important for the restoration of normal knee kinematics, but improper tunneling is one of the most common causes of failed ACL R.[4-6]
In order to achieve a more anatomic femoral tunnel placement, that is, a more posterior and proximal femoral tunnel, there has been a shift from transtibial to transportal femoral tunnel drilling.[7,8] However, this method requires debriding of all the soft tissues on the medial wall of the lateral femoral condyle for accurate identification of the bony anatomy and landmarks. In the search for these anatomical landmarks, namely, lateral intercondylar ridge, lateral bifurcate ridge, the apex of deep cartilage, the distance of the proximal to distal femoral intercondylar notch wall, or the ruler method, the native biology is brushed aside.[9-12]
Preserving soft-tissue remnants on both, the femoral and tibial sites, has a positive effect on graft revascularization and ultimately ligamentization. There is better proprioception in the healed ACL.[13-16]
The authors have consistently identified an inverse J-shaped soft-tissue arch from the femoral ACL remnant in most of our patients. This arch was a part of the ACL remnant on the femoral side, irrespective of remnant tissue present over the tibial surface,[17] which was consistently found in 80% of our cases. It corresponds exactly with an accurate femoral tunnel position. The senior author has been using this landmark for drilling femoral tunnel in ACL R for over 10 years.
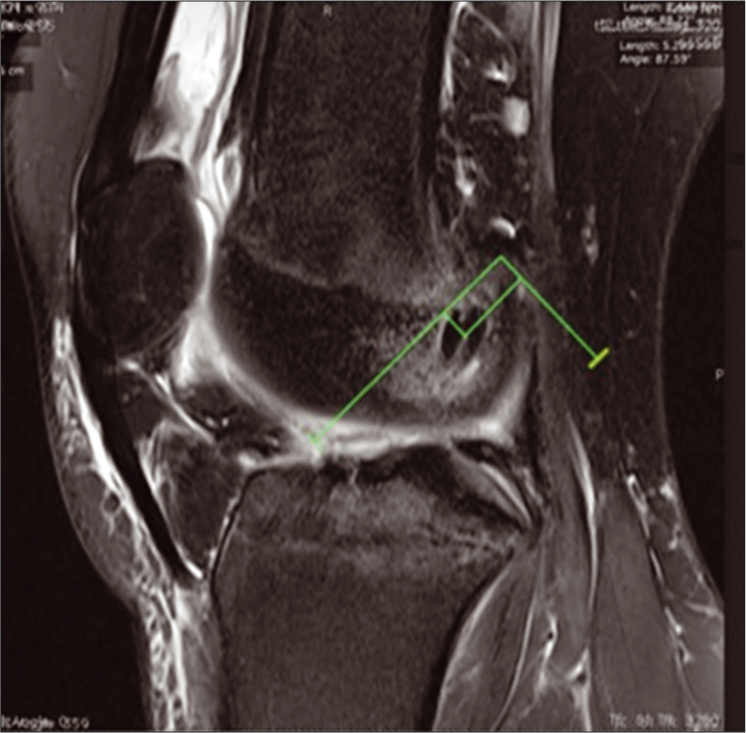
One of the standard techniques to define the femoral tunnel position is to measure its coordinates through the radiographic quadrant technique first described by Bernard et al.[18] This can be used postoperatively and has already been confirmed several times using various X-ray, computed tomography (CT), and magnetic resonance imaging (MRI)-based grids [Figure 1]. The centric position of the ACL bundle has been found to exist in various shapes and positions ranging from 23% to 43% (depth) × 27% to 44% (height).[3,11,19]

- Bernard and Hertel – X-ray, CT, and magnetic resonance imaging-based grids.
The aim of the present study was to verify and establish the reliability of the J arch as a contemporary landmark for femoral tunnel placement. It was hypothesized that the coronal and sagittal coordinates of the femoral tunnel in the MR images will match the previously published data from cadaver studies.
The authors would like to present their results regarding the reliability of this soft-tissue landmark in accurately placing the femoral tunnel using an MRI-based post-operative assessment.
MATERIALS AND METHODS
This study is a retrospective analysis of prospectively collected data of 40 patients who underwent primary ACL reconstruction in January 2018, by a single surgeon. The inclusion criterion was primary ACL reconstruction.
Multiligament injury, revision ACL reconstruction, additional extra-articular procedures, and open physis were excluded from this study.
Postoperatively, MRI of these patients was reviewed to evaluate the femoral tunnel position in terms of depth and height from the proximal condylar surface and notch roof, respectively. Patients who were unable to undergo a post-operative MRI due to financial or logistical reasons were also excluded from the study.
Surgical technique
A transportal anatomical ACL reconstruction technique was used in the present study.
The patient was placed in the supine position on a standard operation table with a thigh post. A thorough arthroscopic evaluation was initially performed. Any meniscal and chondral pathology was assessed and treated.
As a part of this study, the configuration of the ACL remnant and its attachments to the femur and tibia were characterized. The intercondylar notch was carefully inspected and probed to identify the tear pattern of ACL. The impinging ACL nodule was carefully debrided without disturbing the intact remnant. Autologous quadrupled semitendinosus graft was harvested and prepared in all cases. The femoral tunnel was made using a side-specific flexible femoral jig (VersiTomic-Stryker). The knee was kept in 100° flexion and J arch was used as the soft-tissue landmark for the placement of the guide wire for the femoral tunnel [Figures 2 and 3].
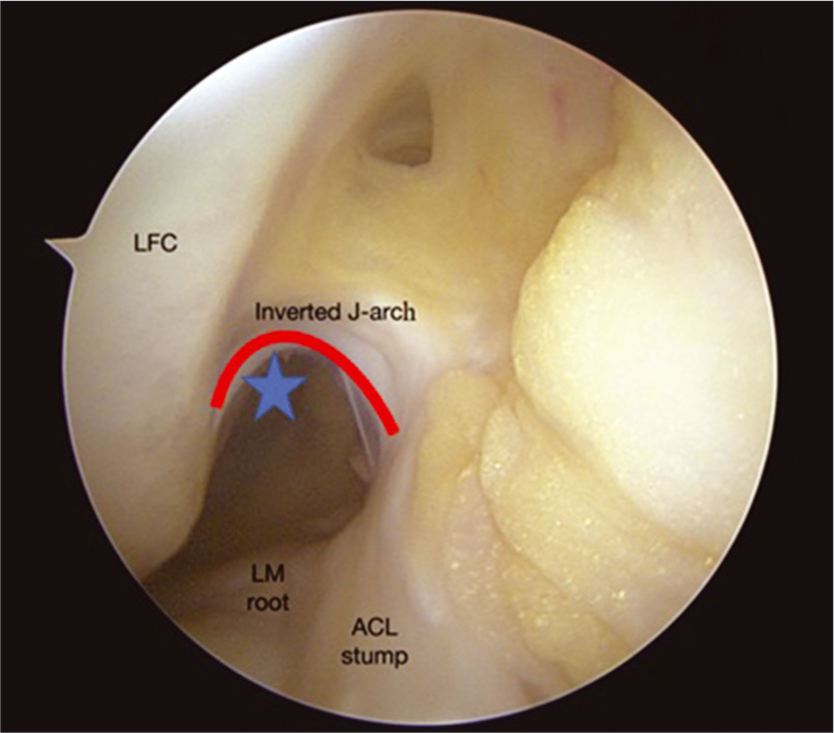
- Arthroscopic view showing the J arch (red line) under which the guidewire is passed to create the femoral tunnel (star).
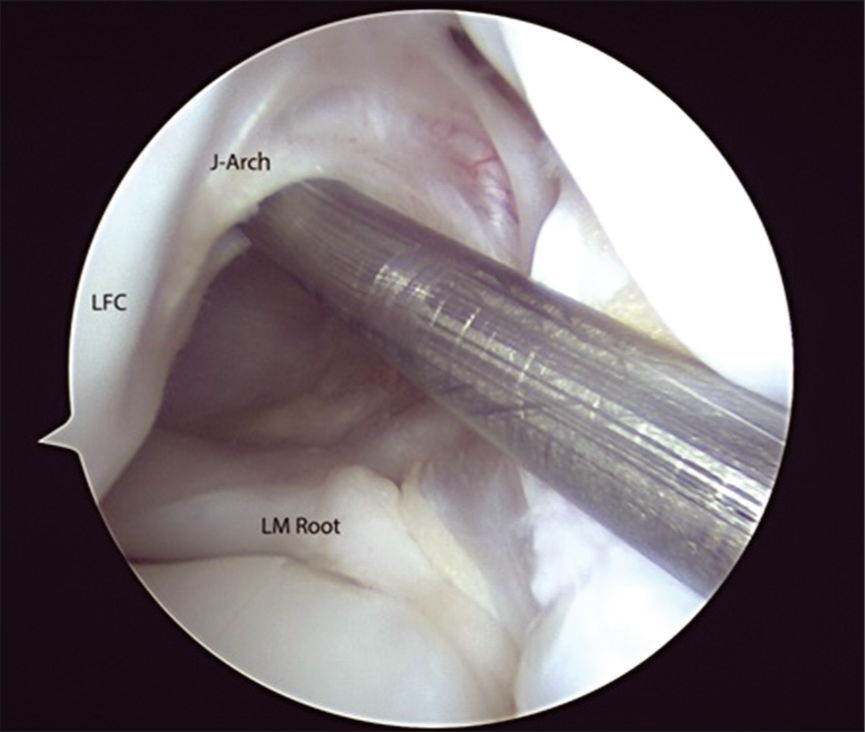
- Arthroscopic view showing the passage of guidewire in the femoral tunnel under the J arch. Also seen are the root of lateral meniscus and the lateral femoral condyle.
The length of the femoral tunnel was measured using an outside-in-depth gauge. Accordingly, the desired length of the femoral tunnel was drilled with a flexible reamer with a diameter corresponding to the graft size. The remaining tunnel length was drilled with a 4.5 mm reamer for the passage of Endobutton.
The tibial tunnel was drilled with standard rigid reamers progressively up to the same diameter as that of the graft, and the tunnel debris was cleared without damaging the ACL remnant. A sleeve of the ACL remnant fibers on the ACL footprint was created to enclose the ACL graft. Endobutton with continuous loop (EndoCL, Smith and Nephew, USA) and suture disk (Adler) was used to fix the graft on the femoral and tibial sides, respectively. Cyclical loading of the knee was performed.
MRI analysis
Postoperatively, an MRI was performed with a 3T Magnetom Spectra (Siemens Healthineers, USA) using an 18-channel receiver/transmitter knee coil. The knee was placed into the coil in the neutral position.
The MR images were evaluated separately on a Digital Imaging and Communications in Medicine software by an orthopedic surgeon (Group 1) and a musculoskeletal radiologist (Group 2) who were unaware of patients’ clinical data. This was done to avoid interobserver bias.
The location of the femoral insertion sites was measured as coordinates in an x-y orientation as described by the radiographic quadrant method[18] applied on MR images [Figure 1]. The femoral coordinates were aligned parallel (x) to and perpendicular (y) to the Blumensaat’s line (the roof of the intercondylar fossa) [Figures 4 and 5].

- Using magnetic resonance imaging- finding femoral coordinates- aligned parallel to (x) and perpendicular to (y) (seen as green lines here) the Blumensaat’s line (the roof of the intercondylar fossa).
- MRI with calculation of femoral coordinates, shown by the green box made between the green lines parallel and perpendicular to Blumensaat’s line.
Sagittal proton-density (PD) images were used to create the grid in an x-y orientation on the femoral condyle such that the Blumensaat’s line was parallel to the x-axis. Other sagittal PD images were then used to measure the maximum height (H) and depth (D) of the femoral condyle in millimeters in the x-y orientation, respectively, from the proximal condylar surface and the notch roof. On this femoral grid, the depth (A) and height (B) of the femoral condyle were represented on the x-axis and y-axis, respectively, by superimposing the sagittal PD image showing the entry point of the femoral tunnel. The length of the x-axis was equivalent to the maximum length of the femoral condyle from the proximal condylar surface parallel to Blumensaat’s line and the length of the y-axis was the maximum height of the femoral condyle perpendicular to the Blumensaat’s line. The distance from the center of the femoral tunnel insertion site to the x- and the y-axis was measured. The tunnel location was expressed in terms of percentage of length (A/D × 100) and height (B/H × 100) of tunnel insertion site from the proximal condylar surface and the notch roof, respectively, to that of the maximum condyle measurement.
Statistical analysis
Statistical analysis was performed using STATA 15 (StataCorp) software for Windows.
The mean height and depth (with standard deviation) of the femoral tunnel position were analyzed using descriptive analysis.
RESULTS
Forty patients were included for the purpose of this study (n = 40). The mean age of the patients in the present study was 28.67 ± 9.53 years. There were 26 male and 14 female patients. Out of these, 25 patients had suffered an injury while being engaged in sports. The ACL was reconstructed in 26 left and 14 right knees with the mean injury to surgery interval of 12.57 ± 8.43 months and a mean graft diameter of 8.31 ± 0.47 mm.
The mean depth and height of the femoral tunnel aperture were 27.12 ± 2.2% from the proximal condylar surface (parallel to Blumensaat’s line) and 30.96 ± 2.75% from the notch roof (perpendicular to Blumensaat’s line), respectively. Our result was found to be at par with data from the previous studies.
The depth calculation done by the orthopedic surgeon (Group 1; 10.58 ± 1.09) and musculoskeletal radiologist (Group 2; 10.58 ± 1.05) was compared. Paired sample t-test results indicate that there is no significant difference in the two means obtained by two different methods (df 39; 95% CI, P > 0.01).
Further, to examine the exact agreement on both groups, the interclass correlation was performed using a two-way mixed with an absolute agreement model. The results indicate that interobserver reliability is good for tunnel depth (≥0.75) and tunnel height (≥0.60).
DISCUSSION
Anatomical tibial and femoral tunnel placements are crucial steps in any ACL R surgery. The correct placement of these tunnels not only restores normal knee kinematics but also a failure to achieve accurate tunnel placement may result in higher graft forces, anterior tibial translation, and graft impingement.[4,20,21] This, in turn, causes graft failure and results in a poor surgical outcome.[5,6,22–28]
The importance of an anatomical femoral tunnel specifically has been shown in various studies.[6,29-31] This has led to the popularization of transportal femoral drilling over the native, ACL footprint.[32]
Transportal drilling requires the clearing of all the soft tissue on the medial wall of the lateral femoral condyle to identify the anatomy of ACL attachment areas and their positions relative to reproducible landmarks such as the lateral intercondylar ridge, lateral bifurcate ridge, and the apex of deep cartilage.[9,10]
Native biology has its own importance. Preserving this biology leads to a better chance of graft ligamentization and vascularization.[33] Additionally, the mechanoreceptors located in the ACL remnant tissue contribute to the proprioceptive function in the knee joint.[34] ACL reconstructive surgeries that have preserved the native tissue have shown higher healing potential, superior functional recovery, earlier return to sports, and a lower reinjury rate than those where the tissue was cleared.[35]
Therefore, the authors believe in using soft-tissue landmarks for identifying the femoral tunnel positioning intraoperatively with a minimum amount of remnant debridement to preserve the native tissue.[36]
The authors operate at a high-volume ACL R center, performing about 700 ACL R per year. The same surgical technique utilizing flexible reamers for femoral tunnel drilling without excising any soft-tissue ACL remnant on the femoral side is followed in all patients. During the course of the senior surgeon’s practice, a femoral ACL remnant in the form of an inverted J-shaped arch of tissue was consistently found in most of our primary ACL R cases and served as a landmark for femoral tunnel placement over the subsequent years with successful results. The authors wished to share this discovery and its applications with the scientific community for the benefit of the patients, as an improvement in surgical outcome will lead to a better quality of life and higher patient satisfaction.
The main aim of this research was to demonstrate the use of the femoral remnant tissue, seen as the inverse J arch, as a reliable soft-tissue landmark for appropriate femoral tunnel placement, without disturbing the native biology including the ACL remnant, Hoffa’s fat pad, and ligamentum mucosum [Figures 4-6].
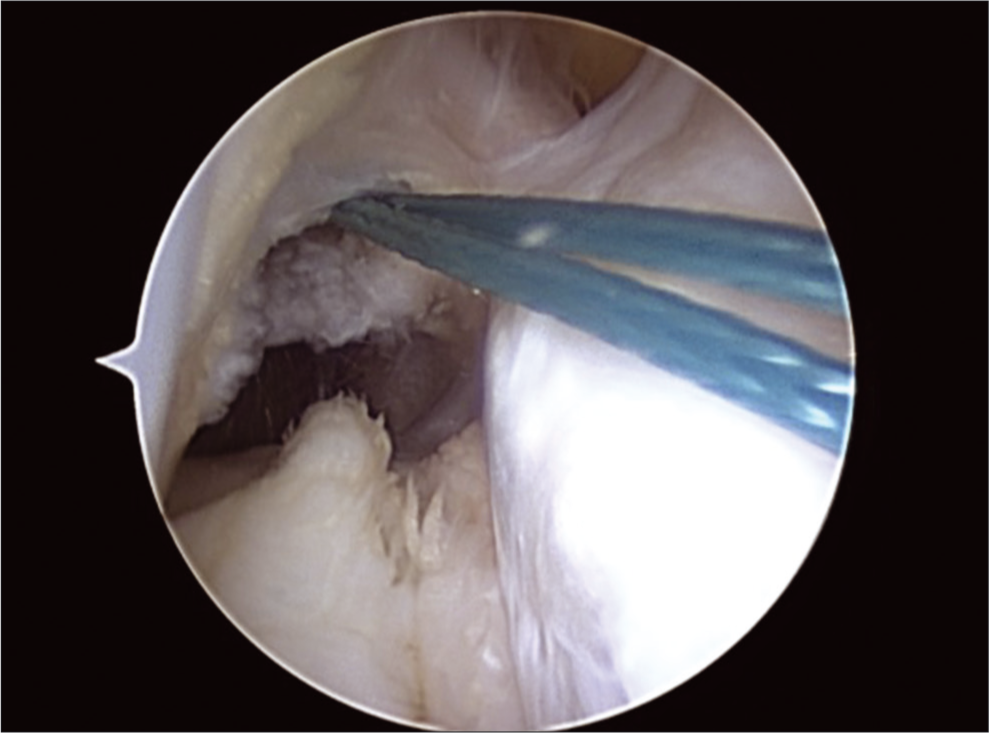
- Threads passing through the femoral tunnel.
The mean depth and height of the femoral tunnel aperture were 27.12 ± 2.2% from the proximal condylar surface (parallel to Blumensaat’s line) and 30.96 ± 2.75% from the notch roof (perpendicular to Blumensaat’s line), respectively, as recorded in the MR images, postoperatively. These findings fall within the acceptable range of values given by Bernard et al. (24.8 × 28.5%).[18] A meta-analysis of several cadaver studies shows that the location of the center of the ACL is highly variable, ranging from 23% to 43% × 27% to 44% along the Blumensaat’s line from the posterior margin and perpendicular to Blumensaat’s line from the roof, respectively.[11] When using the quadrant method, our results lie within this range, as compared to several studies.[18,36-39]
[Table 1] shows the relative positions of the centers (in percentage) of the ACL and the positions of the actual anatomical centers in other studies and the current study in the deep shallow direction at Blumensaat’s line and the high-low direction at condyle depth.
Several other anatomical studies, however, have reported contrary results with a maximum depth of 19% and a maximum height of 13% difference compared to the present study’s tunnel position.[28,40,41]
Kopf et al. performed a systematic review of the literature examining the femoral anatomy of the ACL.[42] They reviewed 20 studies from the PubMed and Cochrane collaboration databases and included papers in both English and German languages. They concluded that there is a great diversity in the descriptions of the size and shape of the femoral origin of ACL. These discrepancies may be explained by a difference in dissection protocols, variation in imaging techniques, and the difficulty to define the exact center of the ACL footprint. Attempts to compile studies of femoral anatomy of ACL were again made by Piefer et al. and Sullivan et al. in systematic literature reviews.[11,43] Coordinates of their pooled ACL center were 28.5% × 35.2% and 31% × 32%, respectively. However, the concept of an averaged ACL center resulting from studies with different methods is questionable.[38]
Overall, the authors feel that the inverse J arch serves as a good anatomical landmark that aids in the placement of the femoral tunnel with the resulting tunnel dimensions in range with the presently accepted range provided by other studies. The 3T-MRI was used as the imaging modality in this study. The modified quadrant method that was originally described using 3D CT is also applicable to MR images, although some difficulties may be encountered in the measurement of the femoral tunnel.[22,37,44] CT and radiographs also have the potential risk of exposure to a significant amount of radiation. It is also difficult to achieve a true lateral image of the knee on a radiograph and the femoral tunnel aperture cannot be identified precisely.
However, there are certain limitations to our study. (1) All surgeries were performed by a single surgeon skilled in remnant preserving ACL R. (2) This technique cannot be reproduced in primary ACL R in which this femoral remnant is missing. (3) There is no control group in this study. As a result, it is unknown whether the presence of a large femoral remnant had any influence on the tunnel position. (4) The interval between surgery and post-operative MRI was not taken into consideration. As a result, tunnel enlargement could have led to improper calculations. However, femoral tunnel widening is seldom seen when extracortical fixation methods are used.[45]
CONCLUSION
The study shows that the inverse J arch soft-tissue ACL remnant can be used reliably to produce the anatomical femoral tunnel placement in ACL R.
This negates the need for the debridement of the medial wall of LFC, thus aiding in biological (tissue preserving) ACL R.
Level of Evidence: IV
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Anterior cruciate ligament reconstruction with quadrupled semitendinosus tendon minimum 6 year clinical and radiological follow-up. The Knee 2007. ;. ;14:321-7.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2016;44:1861-76.
- [CrossRef] [PubMed] [Google Scholar]
- The posterior horn of the lateral meniscus is a reliable novel landmark for femoral tunnel placement in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:1384-91.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic single-graft anterior cruciate ligament reconstruction restores rotational stability: A robotic study in cadaveric knees. Arthrosc J Arthrosc Relat Surg. 2015;31:1981-90.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199-217.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res. 2002;20:1016-24.
- [CrossRef] [Google Scholar]
- The Ability of 3 different approaches to restore the anatomic anteromedial bundle femoral insertion site during anatomic anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg. 2011;27:200-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of transtibial and transportal techniques in drilling femoral tunnels during anterior cruciate ligament reconstruction using 3D-CAD models. Open Access J Sports Med. 2014;5:65-72.
- [CrossRef] [PubMed] [Google Scholar]
- Osseous landmarks of the femoral attachment of the anterior cruciate ligament: An anatomic study. Arthroscopy. 2007;23:1218-25.
- [CrossRef] [Google Scholar]
- The apex of the deep cartilage: A landmark and new technique to help identify femoral tunnel placement in anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg. 2015;31:1777-83.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament femoral footprint anatomy: Systematic review of the 21st century literature. Arthrosc J Arthrosc Relat Surg. 2012;28:872-81.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of a new technique to determine midbundle femoral tunnel position in anterior cruciate ligament reconstruction using 3-dimensional computed tomography analysis. Arthroscopy. 2011;27:1259-67.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy. 2008;24:560-8.
- [CrossRef] [PubMed] [Google Scholar]
- Biologically enhanced ACL reconstruction. Orthop Traumatol Surg Res. 2010;96:810-5.
- [CrossRef] [PubMed] [Google Scholar]
- Sparing the anterior cruciate ligament remnant: Is it worth the hassle? Br Med Bull. 2012;104:91-111.
- [CrossRef] [PubMed] [Google Scholar]
- The anterior cruciate ligament remnant: to leave it or not? Arthroscopy. 2013;29:1253-62.
- [CrossRef] [PubMed] [Google Scholar]
- Variation in anterior cruciate ligament scar pattern: Does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthrosc J Arthrosc Relat Surg. 2005;21:19-24.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral insertion of the ACL Radiographic quadrant method. Am J Knee Surg. 1997;10:14-21. discussion 21-22
- [Google Scholar]
- The anterior cruciate ligament: A study on its bony and soft tissue anatomy using novel 3D CT technology. Knee Surg Sports Traumatol Arthrosc. 2017;25:236-44.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanical effect of tunnel placement on ACL graft forces in double-bundle ACL reconstruction a 3D computational simulation. Int J Med Robot. 2017;13:1840.
- [CrossRef] [PubMed] [Google Scholar]
- MRI assessment of tibial tunnel and its relation to complication following arthroscopic reconstruction of anterior cruciate ligament. Egypt J Radiol Nucl Med. 2014;45:811-7.
- [CrossRef] [Google Scholar]
- Paper # 20: The incidence of failed ACL reconstruction by tunnel malposition. Arthroscopy. 2011;27:e84.
- [CrossRef] [Google Scholar]
- Analysis of Different Causes and Risk Factors of Anterior Cruciate Ligament Reconstruction Failure. Available from: http://www.eoj.eg.net/article.asp?issn=1110-1148;year=2016;volume=51;issue=3;spage=263;epage=269;aulast=El [Last accessed on 2019 Dec 27]
- [CrossRef] [Google Scholar]
- The elongation behavior of the anterior cruciate ligament graft in vivo: A long-term follow-up study. Am J Sports Med. 2001;29:161-6.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of femoral tunnel position in single-bundle ACL reconstruction on functional outcomes and return to sports. Knee Surg Sports Traumatol Arthrosc. 2014;22:97-103.
- [CrossRef] [PubMed] [Google Scholar]
- Sagittal knee stability after anterior cruciate ligament reconstruction with a patellar tendon strip: A two-year follow-up study. Am J Sports Med. 1994;22:518-23.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med. 1996;24:335-41.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of tibial and femoral tunnel position on clinical results after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:355-64.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of different causes and risk factors of anterior cruciate ligament reconstruction failure. Egypt Orthop J. 2016;51:263-9.
- [CrossRef] [Google Scholar]
- Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg. 2012;25:361-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anteromedial portal technique for creating the anterior cruciate ligament femoral tunnel. Arthroscopy. 2008;24:113-5.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: A biomechanical and histological study. Am J Sports Med. 2016;44:1708-16.
- [CrossRef] [PubMed] [Google Scholar]
- Morphologic evaluation of remnant anterior cruciate ligament bundles after injury with three-dimensional computed tomography. Knee Surg Sports Traumatol Arthrosc. 2016;24:148-53.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament remnant and its values for preservation. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2016;7:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament tunnel placement: Comparison of insertion site anatomy with the guidelines of a computer-assisted surgical system. Arthroscopy. 2003;19:154-60.
- [CrossRef] [PubMed] [Google Scholar]
- Radiologic evaluation of the insertion sites of the 2 functional bundles of the anterior cruciate ligament using 3-dimensional computed tomography. Am J Sports Med. 2009;37:2368-76.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic positions of femoral ACL, AM and PL centres: Accuracy of guidelines based on the lateral quadrant method. Knee Surg Sports Traumatol Arthrosc. 2017;25:2321-9.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic landmarks for tunnel positioning in double-bundle ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2011;19:792-800.
- [CrossRef] [PubMed] [Google Scholar]
- Roentgenographic measurement study for locating femoral insertion site of anterior cruciate ligament: A cadaveric study with X-Caliper. Int Orthop. 2009;33:133-7.
- [CrossRef] [PubMed] [Google Scholar]
- The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am. 2010;92:1418-26.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc. 2009;17:213-9.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic anatomy of the native anterior cruciate ligament: A systematic review. HSS J. 2015;11:154-65.
- [CrossRef] [PubMed] [Google Scholar]
- Tunnel positioning assessment after anterior cruciate ligament reconstruction at 12 months: Comparison between 3D CT and 3D MRI. A pilot study. Orthop Traumatol Surg Res. 2017;103:937-42.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral and tibial tunnel widening following anterior cruciate ligament reconstruction using various modalities of fixation: A prospective observational study. J Clin Diagn Res. 2016;10:RC09-11.
- [CrossRef] [PubMed] [Google Scholar]






