Translate this page into:
Paralabral cyst in cricketers – A case series
*Corresponding author: Sumanth Arjun Rajan, Department of Arthroscopy and Sports Medicine, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. arjun261083@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rajan S, Perumal S, Jeganathan P, Sanjay AK, Sivaraman A, Premkumar S, et al. Paralabral cyst in cricketers – A case series. J Arthrosc Surg Sports Med. 2025;6:65-9. doi: 10.25259/JASSM_36_2024
Abstract
Objectives:
Paralabral cysts of the shoulder are rare, and it is usually associated with labral tears. Repetitive stress on the labrum due to increased training history in cricketers can cause micro-tear of the labrum. These tears commonly occur during the early cocking phase in cricketers. These longstanding micro-tears usually form paralabral cysts where the tear operates as a one-way valve. It is fairly common in cricketers who had a longer duration of training and playing history. These cysts are commonly seen in posterior-superior labral tears and SLAP tears.
Materials and Methods:
Data were obtained from a total of 12 cricketers between the period of March 2022 and July 2023. All these athletes mostly came with complaints of chronic shoulder pain, and the diagnosis was confirmed with magnetic resonance imaging. All these patients were treated by arthroscopic cyst decompression with labral repair. A rehabilitation regimen was administered postoperatively to improve the functional ability of the shoulder and help the athlete to return-to-play. QuickDASH score was performed 12 months postoperatively to assess the effectiveness of the surgical outcome.
Results:
All the patients reported remission of pain and showed improvement in their QuickDASH scores compared to the pre-operative period. A properly supervised rehabilitation regimen helped the athlete to return to sport.
Conclusion:
Early diagnosis of paralabral cysts helps in preventing neurological compromise and quicker return-to-play in cricketers. Arthroscopic cyst decompression with labral repair, along with a criteria-based rehabilitation program helps in improving the functional outcome of the athlete.
Keywords
Cyst decompression
Functional outcome
Labral repair
QuickDASH
Rehabilitation
INTRODUCTION
Paralabral cysts are more common in males and are usually seen in the 3rd to 4th decade of life. They occur in 2–4% of the athletic population. The exact pathogenesis is not well known and they usually are similar to a synovial cyst, ganglion cyst, or a pseudocyst. They have a strong association with glenoid labral tears. Repetitive stress on the labrum due to increased training history in cricketers can cause micro-tear of the labrum. These longstanding micro-tears usually form paralabral cysts where the tear operates as a one-way valve, allowing synovial fluid to seep out of the joint but not back into it.[1]
Posterosuperior labral tears on the glenoid have been linked to paralabral cysts surrounding the spino-glenoid notch. There are several non-operative therapy methods available, including percutaneous needle aspiration oral analgesics such as non-steroidal anti-inflammatory drugs. If conservative measures are ineffective for treating symptomatic paralabral cysts, surgical methods such as open excision or arthroscopic decompression may be done.[1]
Although their natural origin is uncertain, these cysts usually persist and expand over time. Cysts have the potential to compress the suprascapular nerve and cause neuropathy. Muscle edema is the initial symptom of compression of the nerve. If the nerve is decompressed, the edema can be reversed. Chronic neuropathy causes fatty infiltration and possible permanent muscular loss.[2]
A clinical examination technique called Patte’s test is used to identify shoulder instability, especially anterior instability. Anterior instability is indicated if the patient feels uneasy or if the shoulder feels unstable during this technique. The paralabral cyst itself may exacerbate shoulder joint instability or impingement symptoms, making it more difficult to interpret Patte’s test results if it is present. Therefore, it is critical to take into account the cyst’s possible influence on shoulder stability and the interpretation of clinical tests such as Patte’s test while examining a patient with a paralabral cyst.[2]
Treatment options for labral tears and paralabral cysts have ranged from open excision to a variety of arthroscopic procedures, either with or without cyst decompression and labral repair. Labral repair alone results in cyst clearance, a favorable clinical outcome, and high patient satisfaction, according to control imaging (magnetic resonance imaging [MRI]).[2]
It is still up for debate whether cyst decompression should go hand in hand with labral repair. Good results have been reported after arthroscopic labral repair combined with cyst decompression. The decompression is accomplished intra-articularly or through the subacromial space. Certain studies found no appreciable difference between labral repair alone and labral repair in conjunction with arthroscopic cyst decompression.[1]
There are some challenges that cricketers face when they are diagnosed with a paralabral cyst. Pain in the shoulder prevents the athlete from performing overhead and throwing actions. The velocity of bowling or throwing speed is affected in cricketers due to the pathology occurring during the early cocking phase in SLAP tears. Hence, to restore the maximum bowling or throwing speed, appropriate surgical treatment and a structured rehabilitation program needs to be followed for return-to-sport.[3]
MATERIALS AND METHODS
This study was done at Sri Ramachandra Center for Sports Science between the periods of 2022–2023. A thorough clinical assessment of all the patients was done to assess the presence of any muscle atrophy secondary to nerve compression. Radiologically, X-ray and MRI were done for these patients to assess the location and extent of the paralabral cyst and confirm the presence of any associated labral tears [Figures 1 and 2]. Twelve local league male cricketers were taken in this study, and QuickDASH score was used to measure the outcome postoperatively [Figure 3]. The QuickDASH score focuses on assessing the extent of limitation of daily activities and high-velocity activities, including overhead motion. A score of (0–5) indicates an excellent outcome, (6–15) indicates a good outcome, (15–35) indicates a satisfactory outcome, and (>35) indicates a poor outcome. Ethics approval was obtained for the study in May 2022 and informed consent was taken from all the patients involved in this study.

- T1 weighted MRI saggital section with the white arrows showing paralabral cysts. MRI: Magnetic resonance imaging.

- T2 weighted MRI axial section with the white arrow showing paralabral cysts near the postero-superior labrum. MRI: Magnetic resonance imaging.
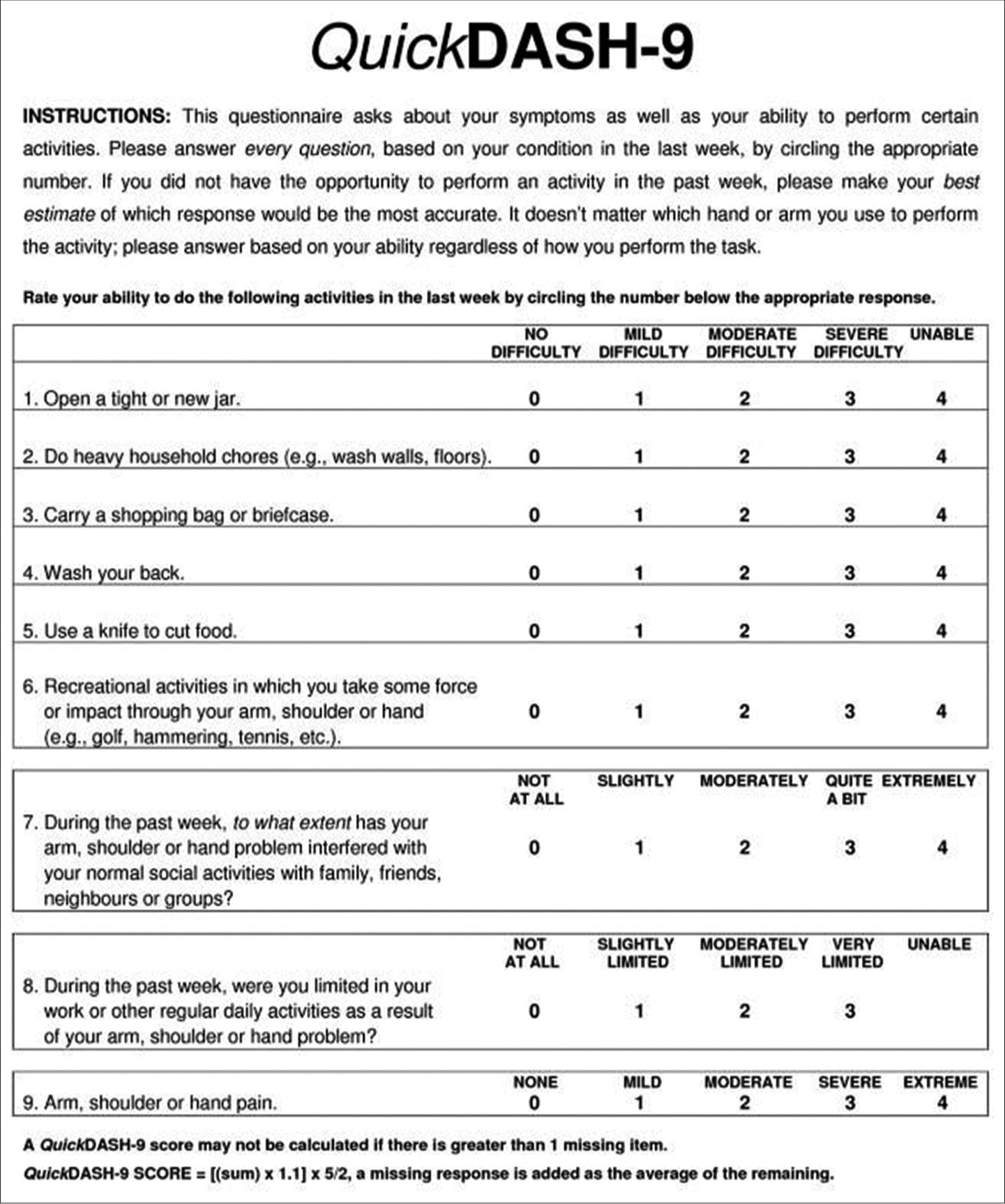
- Quick DASH score. DASH: Disabilities of Arm, Shoulder and Hand.
Inclusion criteria
Patients between the ages of 20 and 30 years were taken, and all of them were male. Patients with labral tears associated with paralabral cysts were included in this study.
Exclusion criteria
Patients with other upper limb injuries and no H/O sporting activities were excluded from this study. Patients aged <20 years and more than 30 years were not included in this study. Patients with signs of severe muscle atrophy and neurological weakness were not included in the study.
Surgical technique
Position
Left/right lateral decubitus position depending on the shoulder involved.
Procedure
Under general anesthesia, the patient was placed in a lateral decubitus position. Upper limb parts were painted and draped. Using the standard posterior portal, a diagnostic arthroscopy was done. The location of the paralabral cyst with tear was identified at the posterior-superior labrum. Anterosuperior and anteroinferior portals were established. Visualizing through anterosuperior portals, evacuation of the cystic fluid and decompression were done through the torn site of the labrum using a shaver from the posterior portal [Figure 4]. The decompression procedure was complete when the cystic fluid was evacuated as much as possible. The torn labrum was repaired using 1.7 mm All-suture anchors. Joint lavage was given [Figure 5]. The wound was closed in layers. Sterile dressing was done. Broad arm sling was given to all patients postoperatively for protective immobilization.
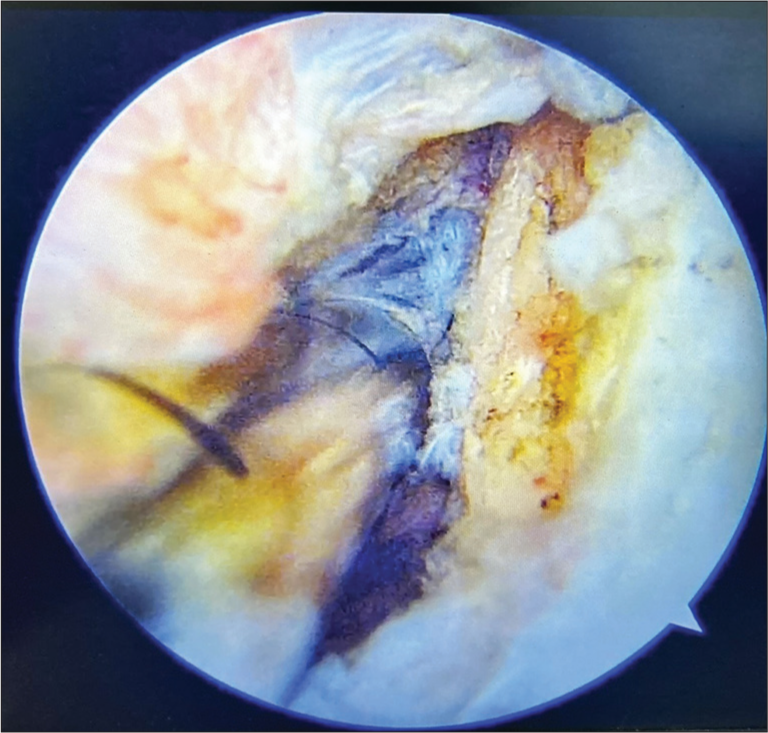
- Image showing cyst decompression.
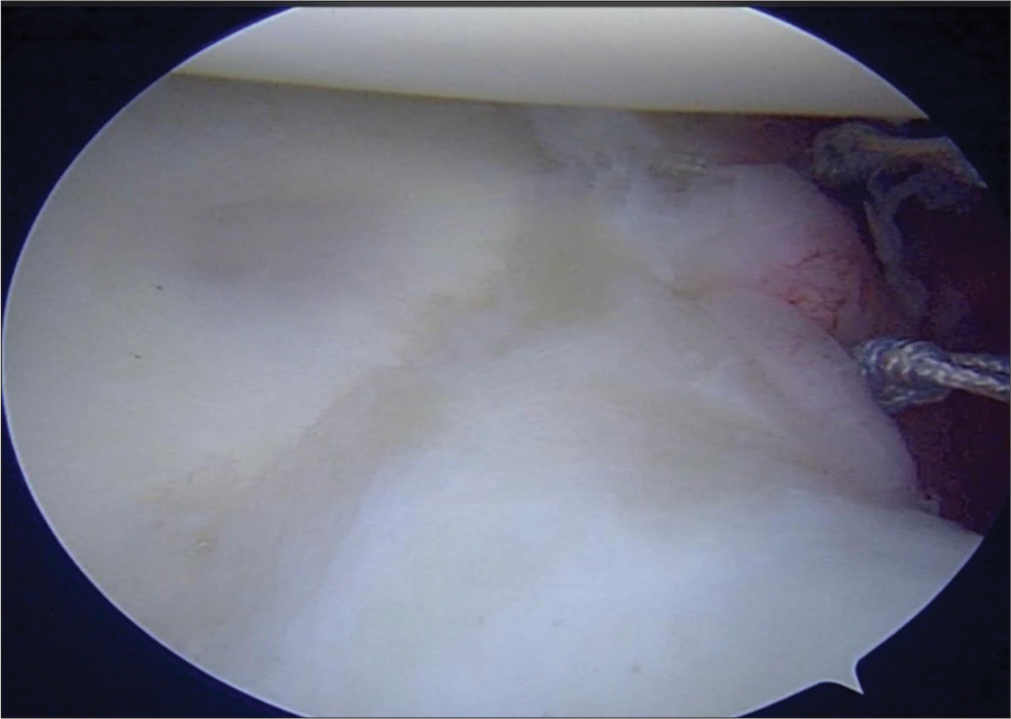
- Image showing posterior-superior labral repair.
RESULTS
The mean age of the patients in this study was 26 years (Range: 20–30 years). The mean duration of symptoms for cricketers included in this study was between 10 and 18 months. All the patients were local league male cricketers and right-sided arm dominance was more common among these cricketers. The most common location of these cysts, as detected on the MRI, was on the posterior aspect of the glenohumeral joint secondary to posterior-superior labral tears. Eight out of 12 cricketers had a posterior-superior labral tear, and the other four cricketers had a SLAP tear, which was confirmed with an MRI.
All the patients reported for follow-up at the end of one year. The mean QuickDASH score pre-operatively was 38.6%, and the mean QuickDASH score postoperatively was 2.3%.
All 12 patients had excellent results.
DISCUSSION
The long training and playing history of cricketers has seen an increase in the diagnosis of paralabral ganglion cysts. It is possible that it can go undiagnosed among overhead athletes. Electrophysiological testing has been used to discover and further standardize diagnostic criteria. It has been shown to confirm the diagnosis of suprascapular neuropathy in 43% of patients with clinical or radiographic suspicion of neuropathy.[4]
A trial of conservative management can be tried to treat paralabral cysts. Percutaneous aspiration, either computed tomography-guided or ultrasonography-guided, can be done to treat these cysts. After aspiration, corticosteroid injections can be given. If conservative management fails, arthroscopic surgery should be the next line of treatment.[5]
In a study done by Kim et al., the concomitant presence of ganglion cysts and SLAP lesions was found to be 89%. In some of these patients, typical SLAP lesions were not seen, and the lesion was seen as a fissure at the posterior part of the labrum.[6] The significance of decompressing a paralabral ganglion cyst in addition to repairing a SLAP tear is a topic of some debate; some authors support merely repairing the tear without actually decompressing the cyst. According to research by other writers, decompression promotes quicker recovery from neuropathy and quicker strength improvements. There is a method for decompressing the suprascapular nerve that involves the subacromial space, but it necessitates a large excision of the bursa and puts coracoclavicular ligaments and the nerve at risk for damage.[3]
Various studies have recognized that SLAP lesions are a causative factor of supraglenoid cysts. Cyst resection has been attempted through open or arthroscopic methods to remove these cysts; however, it is a challenging procedure, and pre-/post-operative morbidity is seen. In this procedure, complete removal of cysts is not guaranteed.[6]
The infraspinatus muscle is typically affected by a paralabral cyst compressing the suprascapular nerve in the spinoglenoid notch, although in certain situations, the teres minor muscle may also be affected. In a different study, 13 out of 20 patients with clinical atrophy and muscle edema on MRI had a damaged infraspinatus. Three of the six patients showed both edema and atrophy of the infraspinatus and the teres minor muscle in addition to atrophy and fatty infiltration of the teres minor muscle. A difference in muscle atrophy was observed between the infraspinatus and teres minor during the post-operative phase. If atrophy involved the infraspinatus postoperatively, it resolved completely, but if the teres minor was involved, the atrophy did not resolve completely.[7]
In this study, no major residual weakness of infraspinatus and teres minor was seen, and hence, electromyography (EMG) was not necessary for these patients. All 12 patients in this study underwent a paralabral cyst decompression with a labral repair to avoid any residual impingement of the cyst on the suprascapular nerve.
If the labral tear is corrected along with cyst decompression, patients should anticipate significant pain alleviation. If labral repair is carried out as soon as possible, there is a good chance that the muscle edema will recover.[8]
Decompression of cysts helps in quicker recovery of neuropathy and an increase in strength. The subacromial approach is usually followed for decompression, and this requires a significant resection of the subacromial bursa.[9] The limited capsulotomy technique is used for cyst decompression as it gives better visualization of the cyst. This technique helps in preserving sufficient capsular and ligamentous tissue which helps in maintaining the glenohumeral stability postoperatively. A complete decompression is not recommended because it places the suprascapular nerve at risk.[9]
Both simple posterior capsulotomy and arthroscopic labral repair with decompression of all intra-articular cysts were successful therapeutic options. If paralabral cysts were associated with further shoulder lesions, treating both lesions at the same time may improve clinical results at the end of follow-up; however, there may be a delay in the early stages of rehabilitation.[9]
Sometimes, locating the paralabral cyst during arthroscopy can be difficult and indigo carmine has been helpful in assessing the location. Under the guidance of ultrasound, indigo carmine was injected into the cyst just before performing the surgery. The leakage point of this dye can be identified during arthroscopy, and decompression of the cyst is performed until the dye is completely discharged. Postoperatively, an MRI was taken in these cases and it confirmed the resolution of the cyst.[10]
The incidence of paralabral cysts in decreasing order is anterior>posterior>superior>inferior. Inferior cysts are the least common and usually associated with a labral pathology. If these cysts present along with a labral tear, cyst decompression along with labral repair was done. However, if there was no associated labral tear, cyst decompression alone is done in these cases. If they are associated with axillary neuropathy, decompression of the cyst is warranted to prevent axillary nerve damage.[11]
Due to repetitive overhead throwing in sports like baseball, it was hypothesized by other authors that there was dynamic compression of the axillary nerve along with the musculocutaneous nerve in a case report study. In these cases, exploration of the brachial plexus was done endoscopically before performing a cyst decompression with labral repair. Diffuse fibrous adhesions around terminal branches of the plexus were observed during exploration, and this probably contributed to the clinical symptoms. Since this exploration may be hazardous, Klumpp et al. suggested that infraclavicular plexus dissection is a more viable option.[12]
In a study done on military personnel, the outcome of biceps tenodesis, along with an intra-articular arthroscopic paralabral cyst decompression, was assessed. Patients with SLAP lesions along with paralabral cysts were taken in this study. Preoperatively and postoperatively, ASES scores were taken, and an improvement in external rotation strength was observed in this population. These patients returned to duty postoperatively at a median duration of 20 weeks. Hence, the use of biceps tenodesis along with arthroscopic cyst decompression has been found to be an effective technique.[13]
In this study, arthroscopic labral repair with decompression of the paralabral cyst was the preferred surgical choice.
Strengths
A comparison of various techniques of paralabral cyst decompression with the technique used in this study has been done to highlight the pros and cons of different procedures. A valid QuickDASH score has been used in this study to effectively assess the outcome of the procedure postoperatively.
Limitations
More outcome scores which focus on the overhead activities of cricket bowlers can be used to assess the functional recovery of cricketers. EMG and nerve conduction study were not done in this study, because patients with severe muscle atrophy or signs of neurological weakness were not included. The sample size taken in this study was small and a bigger sample size could be taken to assess the effect of arthroscopic surgery along with a criteria-based rehabilitation in effective return-to-sport. Repeat MRI postoperatively was not taken to confirm complete decompression of the paralabral cyst and to assess any recurrences.
CONCLUSION
Early diagnosis of paralabral cyst helps in preventing neurological compromise and quicker return-to-play in cricketers. Arthroscopic cyst decompression with labral repair, along with a criteria-based rehabilitation program, helps in improving the functional outcome of cricketers.
Author contributions
SAR, SP, PJ, AKS, AS, SVDP, and AHM: Contributed equally to the design, methodology, and framing the content of the study.
Ethical approval
The study was approved by the Institutional Ethics Committee at Sri Ramachandra Institute of Higher Education & Research with approval no: T6376 on 13th May 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)- assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Arthroscopic all-intra-articular decompression and labral repair of paralabral cyst in the shoulder. J Shoulder Elbow Surg. 2015;24:e7-14.
- [CrossRef] [Google Scholar]
- Comparisons between treatment of isolated posterosuperior paralabral cysts and simultaneous treatment of cysts combined with associated shoulder pathologies: Arthroscopic treatment of posterosuperior paralabral cysts. Arch Orthop Trauma Surg. 2021;143:665-75.
- [CrossRef] [Google Scholar]
- Shoulder injuries in cricketers. J Postgrad Med Educ Res. 2015;49:194-6.
- [CrossRef] [Google Scholar]
- Paralabral cysts of the shoulder treated with isolated labral repair: Effect on pain and radiologic findings. J Shoulder Elbow Surg. 2018;27:1283-9.
- [CrossRef] [Google Scholar]
- Ultrasound-guided aspiration of a paralabral cyst at the spinoglenoid notch with suprascapular nerve compressive neuropathy. J Med Ultrasound. 2018;26:166.
- [CrossRef] [Google Scholar]
- Ganglion cyst of the spinoglenoid notch: Comparison between SLAP repair alone and SLAP repair with cyst decompression. J Shoulder Elbow Surg. 2012;21:1456-63.
- [CrossRef] [Google Scholar]
- Suprascapular neuropathy secondary to compressive paralabral cyst at the spinoglenoid notch. Am J Phys Med Rehabil. 2022;101:e128-9.
- [CrossRef] [Google Scholar]
- The SLAP lesion as a reason for glenolabral cysts: A report of five cases and review of the literature. Arch Orthop Trauma Surg. 2007;127:287-92.
- [CrossRef] [Google Scholar]
- Transcapsular decompression of shoulder ganglion cysts. Arthrosc Tech. 2018;7:e1263-7.
- [CrossRef] [Google Scholar]
- Arthroscopic decompression with indigo carmine for treating paralabral cysts in the shoulder. Orthop Traumatol Surg Res. 2016;102:1109-11.
- [CrossRef] [Google Scholar]
- Decompression of paralabral cyst near axillary nerve: A case report. J Orthop Case Rep. 2023;13:52-6.
- [CrossRef] [Google Scholar]
- Antero-inferior paralabral cyst of the shoulder: An atypical cause of rapidly evolving axillary and musculocutaneous nerve palsy. J Clin Orthop Trauma. 2020;11:S681-3.
- [CrossRef] [Google Scholar]
- Biceps tenodesis and intra-articular decompression for treatment of superior labral tear from anterior to posterior and associated paralabral cyst in active duty military. Mil Med. 2018;183:e194-200.
- [CrossRef] [Google Scholar]







