Translate this page into:
Long-term outcomes of anterior cruciate ligament reconstruction: Peroneus longus versus hamstring tendons
*Corresponding author: Sudeep Kumar, Department of Orthopaedics, All India Institute of Medical Sciences, Patna, Bihar, India. drsudeeportho@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Charan Teja KV, Kumar S, Kumar A, Haripriya H. Long-term outcomes of anterior cruciate ligament reconstruction: Peroneus longus versus hamstring tendons. J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_46_2024
Abstract
Objectives
Management of anterior cruciate ligament (ACL) injuries evolved over the years, and the standard of care is arthroscopic ACL reconstruction (ACLR) with various graft options. The purpose of our study is to evaluate how good an alternative peroneus longus tendon (PLT) can be when used as a graft in primary ACLR by comparing the functional outcomes of patients undergoing ACLR with PLT versus Hamstring tendon (HT).
Materials and Methods
Quasi-experimental study involving 40 patients each in the PLT group and HT group was performed. The knee functional outcomes were compared using the International Knee Documentation Committee (IKDC) score and Tegner Lysholm (TL) knee score measured preoperatively, at 3-, 6-, and 24-month post-surgery. Ankle site morbidity was measured by the foot and ankle disability index (FADI) score and the American Orthopedic Foot and Ankle Society score.
Results
IKDC score in PLT group and HT group was 59.3 ± 16.08 and 48.25 ± 15.81 preoperatively, and it improved to 97.5 ± 2.58 and 92.8 ± 5.12 at 24 months, respectively. The median TL scores were 68.5 (Interquartile range [IQR] 42.3-80) and 71.5 (IQR 62.3-77) and improved to 100 (IQR 96-100) and 100 (IQR 98-100) at 24 months in PLT and HT groups, respectively. FADI and AOSFA scores for the ankle were 100 preoperatively. They dropped to 98.05 ± 1.96 and 98.05 ± 2.24 at 3 months after PLT harvest. Both the scores improved to 100 by 6 months. Graft diameter averaged at 8.78 ± 0.95 mm in the PLT group and 8.12 ± 1.10 mm in the HT group.
Conclusion
Harvesting PLT is relatively easier and faster, yielding sufficient-sized tendons consistently compared to HTs. Both performed similarly in regard to patient-reported outcome measures measured and followed over 2 years. No graft failures were there in both the groups. We conclude that PLTs perform similar to HT autografts when used for primary ACLR without any associated ankle site morbidity.
Keywords
Anterior cruciate ligament reconstruction
Arthroscopy
Autograft
Hamstring tendon graft
Peroneus longus tendon graft
INTRODUCTION
Anterior cruciate ligament (ACL) is one of the most common knee ligament injuries, with incidence rates ranging from 30 to 78 per lakh population in a year.[1] Management of these injuries has evolved over the years, and currently, arthroscopic ACL reconstruction (ACLR) is performed as standard. Allograft availability is a concern in many parts of the world, and most surgeons resort to hamstring tendon (HT) autografts. Donor site morbidity, residual weakness, inadvertent amputation of tendons during harvest, and insufficient graft thickness are major concerns with HT grafts. In revision scenarios and multi-ligamentous knee injuries, usage of peroneus longus tendon (PLT) graft is common, and harvesting it is relatively easier and straightforward forward yielding satisfactory graft thickness.
The minimum dimensions of the prepared tendon graft need to be 70 mm long and at least 8 mm thick for optimal function and lower failure rates.[2] When these are not met, surgeons opt for augmenting with other alternative grafts or allografts. Our current investigation on comparing the functional outcomes of patients operated for ACLR with PLT versus HT will evaluate how good an alternative PLT can be when used as a graft in primary ACLR and also evaluate if there is any ankle site morbidity following its harvest. We hypothesize that PLT will provide adequately sized grafts that are functionally as good as HT grafts with no added ankle site morbidity.
MATERIALS AND METHODS
After obtaining approval from the Institutional Review Board and Ethics Committee, recruitment of subjects was started. Our study was based on the hypothesis that harvested peroneus longus grafts should be able to provide functional results on par with the HT when used for primary ACLR, and our secondary objective was to assess the morbidity in the ankle following PLT harvest. All the patients undergoing arthroscopic ACLR in our institute were explained about the study, and all their queries were resolved before obtaining informed consent. All consenting adults from the age group 18 to 60 years clinically diagnosed with ACL injuries having magnetic resonance imaging (MRI) features without any concomitant ligament injuries or arthritic changes in the knee or ankle were included in the study. Patients with multi-ligamentous knee injuries, revision surgeries, or having features of osteoarthritis of the knee or ankle on X-rays were excluded from the study. Our quasi-experimental study was non-randomized and used power from a previous study by Rhatomy et al.[3] and calculated the sample size to be 80, with 40 subjects in each group. We set the cutoff period of follow-up to be a minimum of 24 months for the study subjects, with periodic reviews during the rehabilitation period.
Subjects were assigned into two groups – when PLT was used as the PLT group and when HT autograft was used as the HT group. All the surgeries in both groups were performed by the same lead surgeon and assistant surgeon (who is also the principal investigator [PI]) and their team. All the assessments preoperatively and post-surgery were done by the same PI. The assessments included a clinical examination of the knee where the Lachman test, anterior drawer test, and pivot shift tests were performed and graded to supplement MRI findings, and other injuries were ruled out. Radiological evaluation of the knee and ankle are performed by x-rays to rule out arthritic changes.
All surgeries were performed under neuraxial anesthesia in the supine position, and a pneumatic tourniquet was used. Standard anterolateral and anteromedial portals were used and diagnostic arthroscopy was performed to confirm the findings and proceeded to graft harvest. The HT was harvested using standard techniques after dissecting out all fascial bands. For harvesting the PLT, a 2 cm long incision is made over the posterior border of the fibula about 2 cm proximal to the lateral malleolus, the tendon of peroneus longus and muscular peroneus brevis is identified, an open tendon stripper is used to harvest the PLT proximally, and the distal part of it is sutured to the peroneus brevis with the ankle in neutral position before cutting it [Figure 1].

- (a) Surface marking of distal fibula and proposed incision line. (b) Showing isolation of the peroneus longus tendon. (c) Harvesting the tendon by passing an open tipped tendon stripper proximally leaving the distal part intact. (d) Showing the harvested tendon with distal attachment intact.
Grafts in both groups were prepared in similar fashion with ACL Tightrope RT (Arthrex, Naples, FL) on the proximal end and distally sutured with FiberWire from the same manufacturer [Figure 2]. The prepared graft is then passed through the tunnels and cycled to remove creep, and fixed in the tibial tunnel with a bio-interference screw (Arthrex, Naples, FL). Wound closure was done and all patients followed the same rehabilitation protocol postoperatively.
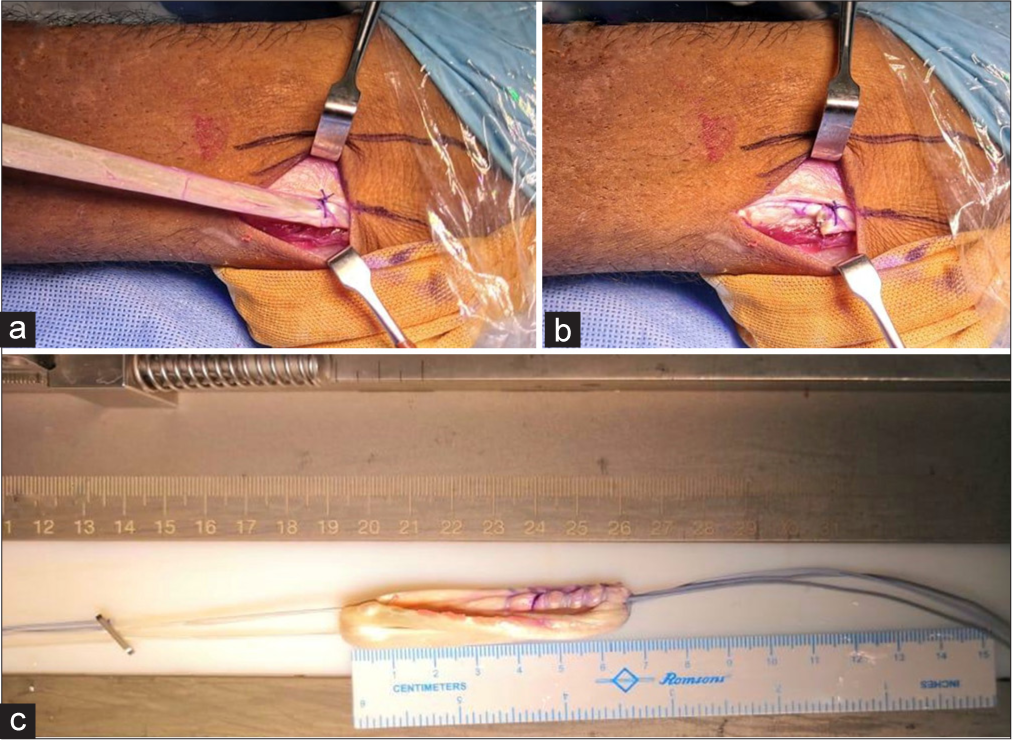
- (a) Peroneus longus tendon stitched to peroneus brevis using absorbable suture just proximal to the peroneal retinaculum. (b) Tendon is cut and showing the remnant stitched with peroneus brevis. (c) Prepared graft using the tendon on graft preparation board.
Outcome measures
Clinical assessment and patient-reported outcome measures (PROMs) were performed preoperatively, at 3, 6, and 24 months postoperatively. The PROMs included the International Knee Documentation Committee (IKDC) score[4] and Tegner Lysholm (TL) knee score[5] for evaluating the knee in both groups. The ankle is evaluated using the foot and ankle disability index (FADI) score[6] and the American Orthopedic Foot and Ankle Society score.[7]
All the data generated through our study were imported into IBM Statistical Package for the Social Sciences Statistics 20 software for further analysis, and descriptive and statistical data were derived.
All eighty subjects completed the minimum follow-up period with none lost to follow-up during the study period.
RESULTS
The demographics of the subjects and descriptive data of dimensions of the graft obtained after preparation in both the groups showed that the PLT group had thicker grafts measuring 8.78 ± 0.95 mm while the HT group was 8.12 ± 1.10 mm. Data are presented in Table 1.
| Parameter | PLT group | HT group |
|---|---|---|
| Number | 40 | 40 |
| Mean age (in years) | 24.9±6.55 | 28.35±8.04 |
| Mean duration from injury to surgery (months) | 14.6±11.61 | 12.05±10.23 |
| Mean graft diameter (in mm) | 8.78±0.95 | 8.12±1.10 |
PLT: Peroneus longus tendon, HT: Hamstring tendon
PROMs
The IKDC score among both the groups is provided in Table 2 shows that the values are significant by independent t-test (P < 0.05) in all the measures. The TL score, when compiled statistically the data was found to be not normally distributed and the descriptive statistics of the same is provided in Table 3. The ankle scores were assessed only in the PLT group, and it was found that all the patients had maximum possible scores (100) in both FADI and AOSFA preoperatively, and the mean values dropped after surgery at the 3rd month to 98.05 ± 1.959 and 98.05 ± 2.235, respectively. At 6 months, the scores were again the maximum possible in all the patients and they persisted into 24-month follow-up. The statistics of FADI and AOSFA scores are provided in Table 4.
| IKDC score | PLT group | HT group | P-value |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Pre-operative | 59.3±16.08 | 48.25±15.81 | 0.035 |
| 3 months | 78.95±7.61 | 68.1±11.58 | 0.001 |
| 6 months | 91.60±4.98 | 82.3±5.8 | 0.001 |
| 24 months | 97.5±2.58 | 92.8±5.12 | 0.005 |
IKDC: International knee documentation committee, PLT: Peroneus longus tendon, HT: Hamstring tendon, SD: Standard deviation
| TL score | PLT group | HT group |
|---|---|---|
| Median (I.Q.R) | Median (I.Q.R) | |
| Pre-operative | 68.5 (42.25-80) | 71.5 (62.25-77) |
| 3 months | 90 (86.75-93.25) | 90 (89-91) |
| 6 months | 96 (95-99.75) | 98.5 (96-100) |
| 24 months | 100 (96-100) | 100 (98-100) |
TL: Tegner Lysholm, PLT: Peroneus longus tendon, HT: Hamstring tendon, I.Q.R: Interquartile range
| Ankle | FADI score | AOSFA score | P-value |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Pre-op | 100±0 | 100±0 | <0.001 |
| 3 months | 98.05±1.96 | 98.05±2.24 | <0.001 |
| 6 months | 100±0 | 100±0 | <0.001 |
| 24 months | 100±0 | 100±0 | <0.001 |
FADI: Foot and ankle disability index, AOSFA: American orthopedic society foot and ankle, SD: Standard deviation
None of the patients in the PLT group developed arthritic changes in the ankle at the end of follow-up, and none of the subjects in either group had their reconstruction failed during the study period.
DISCUSSION
The knee joint, being an inherently unstable joint by its bony design, is mainly stabilized by the ligaments and muscle tendons around it. The main contributors to the stability are the cruciate ligaments. ACL is very commonly injured by forceful valgus and external rotation movement of the knee during road traffic accidents and sports activities. Arthroscopic ACLR performed to address these injuries is a well-established procedure with multiple graft options such as bone-patellar tendon-bone (BPTB), HT, quadriceps tendon, PLT grafts, and allografts.
The most suitable graft that can be utilized for ACLR is not established.[8,9] The BPTB graft is considered to be the gold standard among the grafts but its harvest is riddled with complications and post-operative discomfort and pain. HTs, being comparatively easy to harvest and have greater strength than BPTB grafts, became a natural choice for most surgeons. However, the HT graft harvest is not without complications. The HT protects the reconstructed ACL from anterior drawer force exerted by the strong quadriceps tendon contractions. Their absence or weakness after harvest and utilization as graft makes the graft vulnerable and can alter the knee dynamics. The allografts and biomaterials are costly and limited in availability in most places.
The PLT grafts combine most benefits of both grafts, negating the disadvantages by being very easy to harvest, no alteration of hamstring strength or change in knee dynamics and having comparable strength. In a study by Kerimoğlu et al.,[10] the maximum tensile strength of native ACL was found to be 1725N while that of a single strand of PLT was found to be 1950N, making it biomechanically as strong as the native ACL. The usage of PLT tendons as grafts is not an alien idea, as they are already being utilized in revision ACLR and multi-ligament knee injuries. Ankle instability following its harvest is considered to be the main concern, so in our study, we addressed this concern and evaluated their effectiveness and suitability for choosing them as graft choices for primary ACLR.
Findings from our study showed that the harvested PLT provides equivalent functional results, PROM score improvements, and failure rates when used for arthroscopic ACLR compared to the commonly used HT grafts. There is a slight decrease in PROMs of the ankle on three-month follow-ups, and by the sixth month, all the ankles were at their full functional status in all patients and continued through the follow-up. There is no long-term ankle morbidity in patients after PLT harvest. Our findings are similar to a study by Kumar et al.[11] in which they have concluded that PLT is an appropriate autograft for ACLR, and they found no effect on gait parameters and no ankle instability was recorded. We did not notice any increase in surgical timing in the peroneus longus group. Furthermore, there were no complications, such as infection of the knee or infection of the donor site, in either of the groups.
We acknowledge a few limitations in our study, such as the small sample size. A better statistical power would have been achieved in a study of a larger sample size if incorporated, and randomization is done. Longer follow-ups up from 2 years to 5 years may aid in further evaluation of ankle morbidity and better comparison of functional outcomes. Subjects in the study were involved only in recreational sports, no professional athletes. Involving professional athletes in the study will evaluate how the graft will function in these populations. It can also show how the ankles perform after PLT harvest once they return to sports activities. We did not get any females in our study. Harvest of PLT graft should be evaluated in females to find out how ankles will respond in the population as the footwear and cosmetic preferences vary.
CONCLUSION
The present study found harvesting PLT to be relatively easier and faster, yielding sufficient-sized tendons consistently compared to HTs. Both the tendons performed similarly in regards to PROMs measured and followed over 2 years. There was no ankle morbidity associated with harvesting PLTs after 6 months of the procedure. No graft failures were there in both groups. We conclude that PLTs perform similarly to HT autografts when used for primary ACLR without any associated ankle site morbidity.
Author contributions
KVCT: Contributed in conception of study, literature research, collected and analyzed data, drafted and edited the manuscript and assumed overall accountability of the article; SK and AK: Primary surgeons, had role in conception, reviewing and final approval of the article; HH: Contributed in analyzing experimental studies, data analysis and statistical analysis.
Ethical approval
The research/study approved by the Institutional Review Board at All India Institute of Medical Sciences, Patna, number AIIMS/Pat/IEC/PGTh/Jan19/09, dated November 5, 2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Epidemiology of recurrent anterior cruciate ligament injuries in national collegiate athletic association sports: The injury surveillance program, 2004-2014. Orthop J Sports Med. 2018;6:2325967118777823.
- [CrossRef] [PubMed] [Google Scholar]
- Autograft diameter in ACL reconstruction: Size does matter. SICOT J. 2021;7:16.
- [CrossRef] [PubMed] [Google Scholar]
- Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3552-9.
- [CrossRef] [Google Scholar]
- Reliability and validity of the international knee documentation committee (IKDC) subjective knee form. Joint Bone Spine. 2007;74:594-9.
- [CrossRef] [PubMed] [Google Scholar]
- The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37:890-7.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability and sensitivity of the foot and ankle disability index in subjects with chronic ankle instability. J Athl Train. 2005;40:35-40.
- [Google Scholar]
- Correlation of the AOFAS scores with a generic health QUALY score in foot and ankle surgery. Foot Ankle Int. 2007;28:494-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction using autologous double hamstrings: A comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br. 2007;89:1165-71.
- [CrossRef] [PubMed] [Google Scholar]
- A biomechanical comparison of three lower extremity tendons for ligamentous reconstruction about the knee. Arthroscopy. 2003;19:1091-6.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction with the peroneus longus tendon. Acta Orthop Traumatol Turc. 2008;42:38-43.
- [CrossRef] [Google Scholar]
- A study on peroneus longus autograft for anterior cruciate ligament reconstruction. Int J Res Med Sci. 2020;8:183-8.
- [CrossRef] [Google Scholar]







