Translate this page into:
A novel arthroscopic repair method for anterior horn of the lateral meniscus horizontal tear with all-suture anchor
*Corresponding author: S. Venkatesh Kumar, Department of Orthopaedics, Baby Memorial Hospital, Kannur, Kerala, India. mailvenkatesh91@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jyothiprasanth M, Venkatesh Kumar S, Jithin CR. A novel arthroscopic repair method for anterior horn of the lateral meniscus horizontal tear with all-suture anchor. J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_16_2025
Abstract
The tear of the anterior horn of the lateral meniscus (AHLM), especially the horizontal tear pattern, is usually accompanied with anterolateral meniscal cysts and usually was treated by the arthroscopic cystectomy and AHLM repair with outside-in technique (OIT). Anatomically, a substantial gap exists between the AHLM and anterior capsule, which would be increased after cysts debridement making the meniscal repair difficult to be performed by the OIT, resulting in high tension between the AHLM and the anterior capsule, which would further increase during knee flexion causing anterior knee pain. In this study, we propose a technique to restore the AHLM stability with an all-suture anchor placed at the native anatomical site of AHLM instead of suturing it to the capsule in tension as it is traditionally done.
Keywords
All-suture anchor
Anterior horn of lateral meniscus repair
Knee arthroscopy
Meniscal cyst
Meniscal cyst release
New repair technique
INTRODUCTION
The outside-in technique (OIT) is conventionally used for repairing tears in the anterior horn of lateral meniscus, it has main disadvantage of placing repair sutures between the anterior horn of lateral meniscus (AHLM) and the capsule which results in tension as there is anatomically more distance between the AHLM and the anterior capsule compared to the anterior horn of Medial meniscus which lies close to the anterior capsule.[1,2] Furthermore, natively more mobile lateral meniscus movements will be restricted if it is sutured more anteriorly than its normal anatomy.[3,4] Therefore, we devised an AHLM repair technique using an all suture anchor in a case of horizontal tear of AHLM with associated meniscal cyst. We recommend these techniques as an alternative method for repairing an anterior horn tear of the lateral meniscus.
CASE PRESENTATION
A young male in his 40 s, who was from a lower-middle-class socioeconomic status who sustained a road traffic accident 6-month back, consulted our outpatient department with complaints of the right knee pain and instability while walking and climbing stairs following the fall. He has taken treatment initially from a nearby hospital, where X-rays were taken and no bony injuries were found. On examination of the right knee, tenderness is noted in the anterior aspect of the lateral joint line. During examination of the right knee range of motion (ROM), mild tenderness is noted during terminal extension. The McMurray’s test for the lateral meniscus was positive during extension. Anterior drawer test and Lachman tests for anterior cruciate ligament (ACL) were positive. Varus stress test for the lateral collateral ligament (LCL) was positive. Other ligamentous tests were found to be normal. There is no distal neurovascular deficit noted in the leg.
INVESTIGATIONS
No bony injury or abnormalities with no arthritic changes were noted in the knee joint on the right knee anteroposterior and lateral X-rays. A knee magnetic resonance imaging (MRI) was advised to evaluate meniscal and ligamentous injuries. MRI knee revealed an oblique horizontal AHLM tear in the right knee with associated edematous collection indicating a meniscal cyst [Figure 1]. Associated high-grade ACL tear and LCL mid-substance tear were noted. Other ligamentous structures were normal, and no associated bony injuries or edema were noted in the MRI. The routine laboratory reports and inflammatory/infection markers were normal.
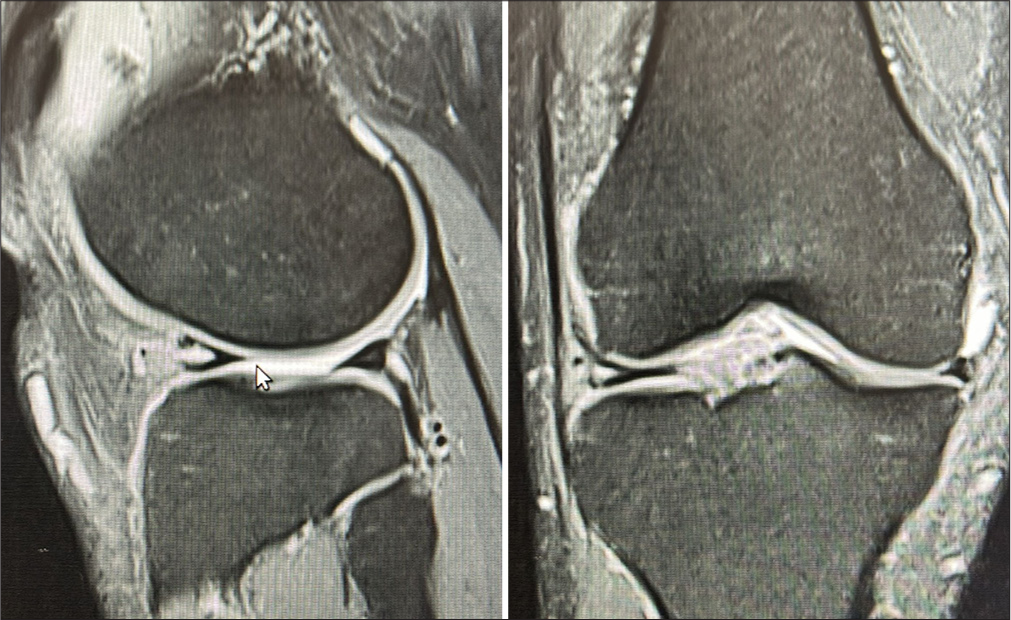
- The magnetic resonance imaging of the right knee revealed an oblique horizontal anterior horn of the lateral meniscus tear with an associated meniscal cyst.
SURGICAL PROCEDURE
The patient was placed supine in the operation theater (OT) table. An arthroscopic anterolateral viewing portal was made using an 11-number blade, and following that, the arthroscope was introduced, and initial diagnostic arthroscopy was performed. An arthroscopic anteromedial working portal was made. A high ACL tear at its femoral insertion site was noted, and the ACL tear was reconstructed using peroneus autograft. For LCL injury, the Larson procedure was done using a semitendinosus autograft.
TECHNIQUE VIDEO
Arthroscopically, a horizontal tear was noted in the AHLM [Figure 2], and freshening up the margins of the anterior horn revealed a concealed cyst. The cyst was de-bulked using arthroscopic radiofrequency system to reveal a horizontal tear in the AHLM, which must be a causative factor of the cyst in first place [Figure 3]. The AHLM footprint area in the proximal tibial intercondylar region was freshened and prepared. A single loaded 1.3 mm “All suture” anchor was placed in the prepared area following drilling through the anchor sleeve, and a suture bite was taken through the AHLM tear by the knee scorpion device. A passport cannula was placed in the anteromedial portal for smooth passage of knots to secure the meniscal repair. A sliding knot is placed to repair the tear to the footprint of the AHLM instead of the usual meniscocapsular repair [Figure 4 and Video 1].

- Arthroscopic view of a horizontal tear in the anterior horn of the lateral meniscus.
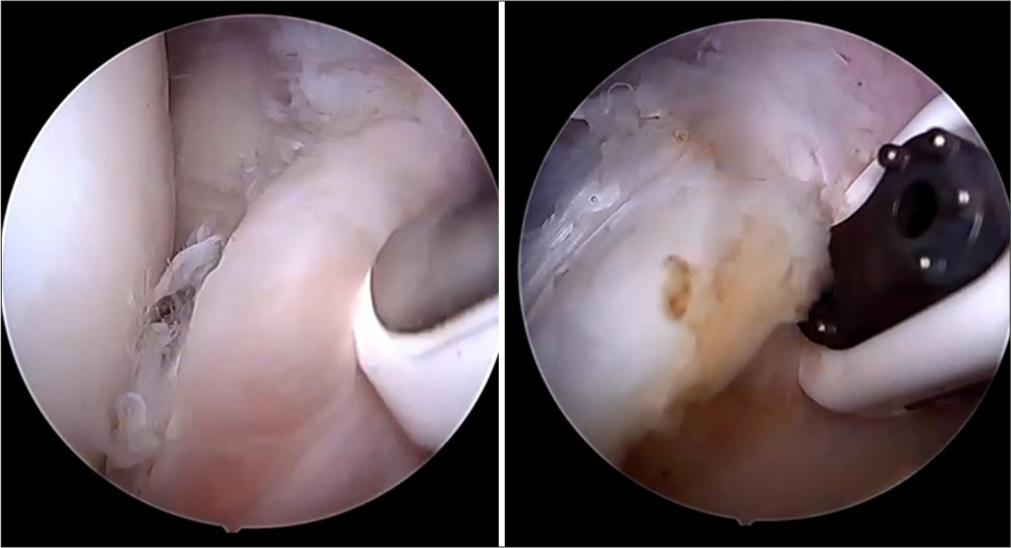
- The cyst was de-bulked using arthroscopic radiofrequency system to reveal a horizontal tear in the anterior horn of the lateral meniscus.
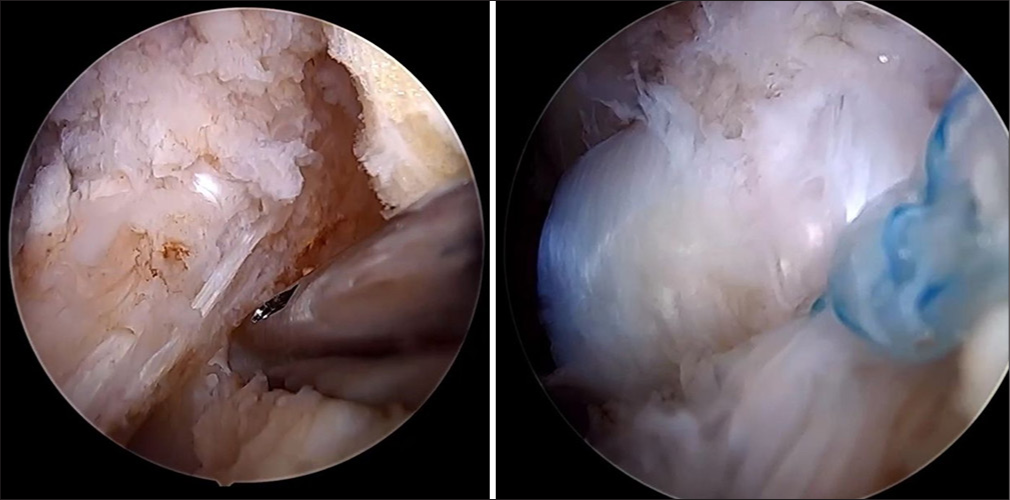
- A sliding knot is placed to repair the tear to the footprint of the anterior horn of the lateral meniscus instead of the usual meniscocapsular repair.
Video 1:
Video 1:The arthroscopic technique where an all-suture anchor is placed at the native anatomical site of anterior horn of the lateral meniscus.OUTCOME AND FOLLOW-UP
There was no bleeding or discharge from the surgical site throughout the post-operative period. The patient was placed in a long knee brace in full extension postoperatively. The patient was advised to be strict non-weight-bearing for 6 weeks postoperatively. A gradually progressive 0–90° knee active and passive ROM is performed during the non-weight-bearing period. Toe-touch weight-bearing is allowed in the brace locked in extension following 6 weeks. After 2 weeks, partial weight-bearing is gradually transitioned to full weight-bearing. After the 6th week, the brace is removed and full 0–120° ROM exercises were performed. Two intra-articular platelet-rich plasma (PRP) injections were given at one-week intervals. Patient’s active knee ROM was 5–110° without any pain or instability during the follow-up [Figure 5].

- Patient’s active knee range of motion was 5-110° without any pain or instability during the follow-up.
DISCUSSION
The horizontal AHLM tears are frequently associated with meniscal cysts because the horizontal cleavage tear causes joint fluid to seep through the macro- and micro-tears. This is because the one-way valve mechanism may permit synovial fluid to build up inside the meniscal cavity, particularly during weight-bearing and knee ROM. Meniscal cysts on the lateral meniscus were typically symptomatic and subjected to a thorough investigation.[5] There is disagreement regarding the association between meniscal cysts and lateral meniscal tears; some studies[6] report a 100% association, while other studies[7,8] report an 85% association.
Surgical intervention is required for those experiencing symptoms. These days, arthroscopic and mini-open excision, which aims to remove the entire cyst and a total arthroscopic procedure consisting of meniscectomy and cyst decompression, are the two most commonly used arthroscopic techniques for the treatment of parameniscal cysts.[9]
Large cysts should be treated primarily by arthroscopic subtotal meniscectomy or partial menisectomy. Multiple loculi should be broken down using a combined arthroscopic and mini-open approach, and arthroscopic decompression of the cyst should be tried.[10,11]
The function and mechanics of the knee joint depend on the presence of anatomically intact AHLM. Significantly higher tibiofemoral peak forces in the medial and lateral compartments are indicative of an AHLM rupture. The importance of repairing AHLM tears is indicated by the restoration of peak forces to their pre-injury state.[12] To repair the AHLM and maintain the structural integrity of the AHLM, we suggest a unique all-suture anchor fixation in the present study.
The outside-in method has been frequently employed for AHLM repair. Because the AHLM is positioned more posteriorly than the medial meniscus, extra-articular knot tying may result in abnormally increased knot tension between the meniscus and the joint capsule or pain from joint capsule entrapment.[13] Furthermore, the knots are positioned subcutaneously over the capsule.[14]
According to Fu et al.,[13] their technique involves forming and pulling a FiberWire loop to grasp the AHLM, and then using a PushLock to firmly fix the AHLM, suture strands are attached on the anterior border of the lateral tibial plateau. In a comparable manner, Pimprikar and Patil[15] repaired the AHLM using a knotless anchor rather than a suture anchor, allowing a predictable tension across the repair when deployed.
In our case, we used a single loaded 1.3 mm all-suture anchor on the anterior margin of the lateral tibial plateau corresponding to AHLM footprint and sutures are passed through the horizontal tear using knee scorpion device. A sliding knot is placed over the horizontal tear to firmly fix the AHLM in its anatomical site without tension. However, in the traditional OIT used for AHLM repair, the AHLM is sutured to the anterior capsule.
For better outcomes, we used PRP injection in the surgically repaired knee as part of our meniscal repair program. Due to the cyst’s deep location in the meniscus’s red-red zone, biological considerations might be taken into account to aid in biological repair. Trephination, synovial abrasion, injection of a fibrin clot, and PRP are common techniques to improve the vascularity and healing of the meniscus.[16] After meniscal tissue repair with PRP augmentation, the increased platelet counts enable the release of growth factors, which may encourage angiogenesis and soft-tissue healing [17-19] with encouraging outcomes.
CONCLUSION
Our surgical technique is more anatomical and practical technique as we used an all-suture anchor to fix the horizontal tear of AHLM into its native footprint in the anterolateral tibial plateau with good functional outcome without any common post-operative complaints of traditional AHLM capsule-meniscal repair.
Acknowledgment:
We thank orthopedic consultants Dr. Akhil K Thomas, Dr Aghosh MC and Clinical Pharmacologists Dr. Sarang P, Dr Ajinas T P, Dr. Mohamed Hadi Mansoor from Baby Memorial Hospital, Kannur, Kerala, India, for their valuable support in the preparation of the manuscript.
Author contributions:
JM: Concepts, design, definition of intellectual content, manuscript editing, and review; VKS: Literature search, manuscript preparation, manuscript editing, and review; JCR: Literature search and manuscript preparation. All the authors have read and approved of the manuscript, and each author believes that the manuscript represents honest work.
Ethical approval:
The Institutional Review Board approval is not required as this study involves a new technique that the authors have invented intra-operatively.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Anterior horn meniscal repair using an outside-in suture technique. Arthrosc Tech. 2016;5:e1111-6.
- [CrossRef] [PubMed] [Google Scholar]
- A modified outside-in suture technique for repair of the middle segment of the meniscus using a spinal needle. Knee Surg Relat Res. 2014;26:43-7.
- [CrossRef] [PubMed] [Google Scholar]
- The basic science of human knee menisci: Structure, composition, and function. Sports Health. 2012;4:340-51.
- [CrossRef] [PubMed] [Google Scholar]
- Horizontal cleavage tear meniscal repair using all-inside circumferential compression sutures. Arthrosc Tech. 2023;12:e1319-27.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of meniscal cysts: Incidence, location, and clinical significance. AJR Am J Roentgenol. 2001;177:409-13.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of cysts of the lateral meniscus. J Bone Joint Surg Br. 1993;75:299-302.
- [CrossRef] [PubMed] [Google Scholar]
- Cysts of the lateral meniscus: Arthroscopy versus arthroscopy plus open cystectomy. Arthroscopy. 1989;5:274-81.
- [CrossRef] [PubMed] [Google Scholar]
- Injuries of the knee joint /I.S. Smillie. 1978. Edinburgh, New York: Churchill Livingstone, Distributed by Longman; Available from: https://nla.gov.au/nla.cat-vn2535334 [Last accessed on 2025 Mar 18]
- [Google Scholar]
- Comparison of the recurrence risk of parameniscal cysts between patients treated with arthroscopic excision and arthroscopic decompression techniques. Knee Surg Sports Traumatol Arthrosc. 2016;24:1547-54.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopy alone or in association with open cystectomy: In treatment of lateral meniscal cysts. Knee Surg Sports Traumatol Arthrosc. 2003;11:30-2.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of meniscal cysts. Arthroscopy. 1993;9:591-5.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior horn lateral meniscus tear, repair, and meniscectomy. J Knee Surg. 2014;27:229-34.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic repair for the anterior horn of the lateral meniscus with suture anchor. Arthrosc Tech. 2023;12:e635-8.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016-30.
- [CrossRef] [PubMed] [Google Scholar]
- Repair of the anterior horn of the lateral and medial meniscus with knotless suture anchor. Arthrosc Tech. 2024;13:103044.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma in meniscal repair: Does augmentation improve surgical outcomes? Clin Orthop Relat Res. 2015;473:1665-72.
- [CrossRef] [PubMed] [Google Scholar]
- The regenerative effects of platelet-rich plasma on meniscal cells in vitro and its in vivo application with biodegradable gelatin hydrogel. Tissue Eng. 2007;13:1103-12.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of platelet-rich plasma in arthroscopic repair for discoid lateral meniscus tears. BMC Musculoskelet Disord. 2019;20:113.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma reduces failure risk for isolated meniscal repairs but provides no benefit for meniscal repairs with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47:1789-96.
- [CrossRef] [PubMed] [Google Scholar]







