Translate this page into:
A novel biplanar repair technique for tendoachilles tendon ruptures
*Corresponding author: Angad Jolly, Department of Orthopaedics, Sir Ganga Ram Hospital, New Delhi, India. angad.yahoo.hotmail@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhasin VB, Singh A, Jolly A, Palatty C. A novel biplanar repair technique for tendoachilles tendon ruptures. J Arthrosc Surg Sports Med 2023;4:1-5.
Abstract
Objectives:
Achilles tendon is one of the most commonly ruptured tendons in the body. Conservative and operative treatment is both well-described in the literature. Surgical treatment carries risks and complications, which we tried to overcome with our novel biplanar repair technique.
Materials and methods:
The unique features of our technique include an incision with intact skin bridge, repair of tendoachilles tendon with mediolateral and anteroposterior tunnels in calcaneal tuberosity and a post-operative cast permitting knee flexion, preventing knee extension.
Results:
The results of this technique after 1 year of follow-up showed no wound-related complications, no rerupture, and an average American Orthopedic Foot and Ankle Society score of 92.
Conclusion:
It is a promising technique and further studies are needed to compare the results of our technique with existing ones over longer periods.
Keywords
Tendoachilles
Surgical repair
Biplanar technique
INTRODUCTION
Achilles tendon is the strongest tendon in the human body and is also one of the most commonly ruptured tendons.[1] The common mechanisms of injury that leads to Achilles tendon ruptures are sports injuries, road traffic accidents, and penetrating trauma.[2] Achilles tendon ruptures are often seen in young active adults who desire to return to their work or sporting activities following treatment. Conservative treatment by casting has been known to give good results, but is associated with higher incidence (up to 30%) of rerupture and delayed return to activities.[3,4] Due to this, surgical treatment has gained preference for the treatment of Achilles tendon rupture.[5]
Surgical treatment of Achilles tendon tears has its own set of risks and associated complications which make this form of treatment challenging. Some common complications are wound necrosis, deep infection, sural nerve injury, and rerupture of tendon.[6]
Wound-related complications following surgery are common due to the superficial location of the tendon and associated surrounding soft-tissue injury.[7] A wound-related complication rate of up to 17% and deep infection rate of up to 4% have been reported across different methods of Achilles tendon repair.[8] These complications can significantly hamper rehabilitation and leave patients with a poor functional outcomes.[7]
Rerupture rates of up to 5.6% following surgical treatment and up to 20.8% following conservative treatment have been reported in various studies.[9-12] Attempts at augmenting the tendon repair by various techniques have also failed in improving rerupture rates.[13]
Many studies have been undertaken over the years to evaluate minimally invasive and percutaneous techniques of tendon repair to minimize wound-related complications and rerupture rates following surgery, although none have established any clear advantage of such procedures.[14-17] Our institute thus came up with a novel technique to repair torn Achilles tendon, where a bridge of skin is left intact between two longitudinal incisions and the tendon is sutured by a biplanar technique to achieve a strong repair. It was hypothesized that this technique would reduce wound-related complications as well as rerupture rates.
MATERIALS AND METHODS
Six patients presenting with closed complete Achilles tendon tears between 2018 and 2022 were operated on using our repair technique at our institute. Diagnosis was made by clinical examination and was confirmed by magnetic resonance imaging (MRI). All of the patients included in this study were operated on and followed up by the same surgeon. All six patients in our study had complete ruptures of tendoachilles.
Surgical technique
Once the patient is anesthetized, a pneumatic tourniquet is applied to the thigh and the patient is then placed in the prone position on the operating table. Surgical area is thoroughly prepared, painted with chlorhexidine and betadine, and then draped. The tourniquet is inflated and a midline incision of about 3 cm is given over the tip of the calcaneal tuberosity extending proximally. The torn end of the Achilles tendon is identified and the paratenon is separated and incised using dissecting scissors. The paratenon incision is carried proximally by passing the scissors in the same plane upward till the musculotendinous junction of triceps surae. Another midline longitudinal skin incision of about 5 cm is given over the musculotendinous junction while maintaining a skin bridge of about 5 cm in between the two incisions. [Figure 1] The Achilles tendon is identified and the torn edge is delivered through the proximal incision while leaving behind the paratenon with the subcutaneous tissue [Figure 2]. The irregular edges of the torn tendon are debrided. Two separate number 5 non-absorbable polyester threads are now taken and the tendon is secured by whip stitch technique in two separate planes. The first thread is sutured in the mediolateral direction and the second in the anteroposterior direction, thus securing the tendon in two planes [Figure 3]. Now going back to the first incision, the soft tissues around the tuberosity are separated to clearly define the insertion of the Achilles tendon. Once it is identified, two separate drill holes (with a 2.5 mm drill bit) are made in the tuberosity, one in the mediolateral direction and one in the anteroposterior direction [Figures 4-6]. The torn end of the Achilles tendon is delivered back into the distal incision over a curved hemostat. Now, the ends of the mediolateral and anteroposterior stitches are passed into the respective bone tunnels over a shuttling thread. The ankle is put into plantar flexion before tightly tying the two threads separately [Figure 7]. Incisions are closed in layers. A cast is applied with the ankle in plantar flexion and is maintained for 3 weeks. The cast applied in the operation theater is specifically designed to permit knee flexion while preventing the terminal 30–40° of extension of the knee. The cast is applied in about 40° of knee flexion such that the proximal end of the cast ends around the calf posteriorly and extends just above the knee anteriorly. This anterior extension of the cast restricts the terminal 40° of knee extension and prevents undue stress on the tendon repair.

- Incision is given with skin bridge.

- Delivering the tendon through proximal incision and applying whip stitch.
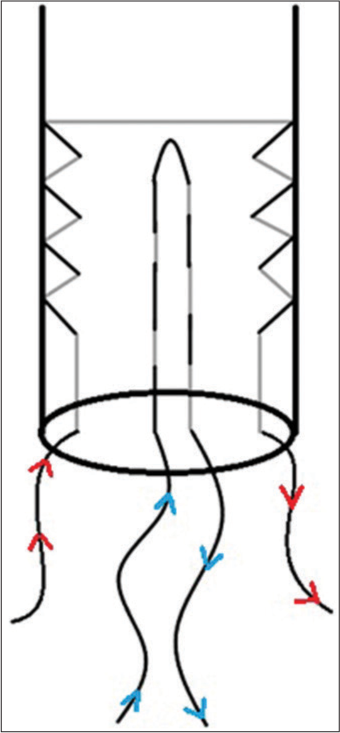
- The tendon is prepared by two whip stitches, one anterior to posterior (blue) and the other from medial to lateral (red).

- Drilling holes in calcaneal tuberosity.
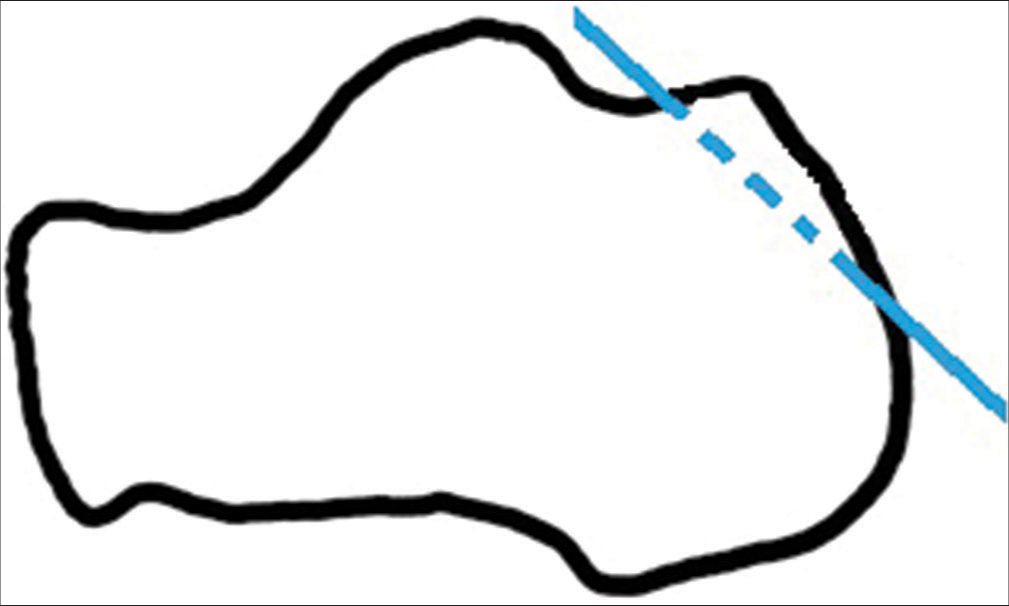
- Drill holes through calcaneal tuberosity. Anterior to posterior. It accommodates the stitches marked in blue arrow.
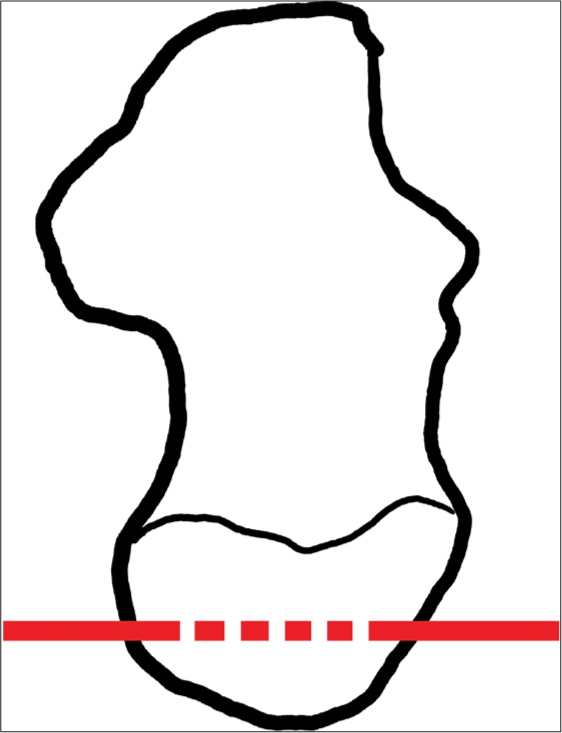
- Drill holes through calcaneal tuberosity. Medial to lateral. It accommodates the stitches marked in a red dashed line.

- Tying the tendon to calcaneal tuberosity through two tunnels.
The patients were discharged with the below knee cast in situ and were followed up on the 21st day for suture removal. A new below knee fiber cast is applied after suture removal with the foot in the plantigrade position and partial weight-bearing as tolerated is started. This cast is retained until about 10 weeks after surgery following which it is removed and ankle mobilization exercises are started. Heel cord stretching exercises are started at 3 months following surgery to improve dorsiflexion range of the ankle joint and full weight-bearing ambulation is achieved by this time.
The patient was then followed up at 6 months, 9 months, and 12 months following surgery. At each visit, the surgical scar was analyzed, active range of movements was recorded, calf circumference measured, and American Orthopedic Foot and Ankle Society (AOFAS) Ankle – Hindfoot score was calculated. Unique features of our technique:
Incision with skin bridge
Repair of tendoachilles tendon with mediolateral and anteroposterior tunnels in calcaneal tuberosity
Post-operative cast permitting knee flexion, preventing knee extension.
RESULTS
None of the patients included in the series developed any surgical site related complications like wound dehiscence, necrosis, infection, or sural nerve injury [Figure 8]. There was no case of rerupture either in any of the six patients.

- Healthy surgical scar.
At the 12 month follow-up, the average AOFAS score of our patients was 92.
The average difference in calf circumference of the operated and uninvolved limb was 2.4 cm at 3 months. This difference gradually reduced to an average of 0.3 cm at 12 months follow-up.
The average range of active dorsiflexion at 12 months follow-up was 16.5° and active plantar flexion was 41.2°.
DISCUSSION
Tendoachilles tendon tears are well-described in the literature and are commonly seen in athletes and sports injuries, but can occur in people with sedentary lifestyles as well.[18] The incidence of tendoachilles tendon tears is on the rise and is most significantly seen to increase in males aged 30–39.[19] The most common site of rupture of tendoachilles tendon is reported to be 3–6 cm above the os calcis as this is a watershed region that has compromised vascularity.[20] Besides trauma, the tendon is prone to rupture following steroid therapy, hypercholesterolemia, gout, rheumatoid arthritis, and following renal transplant.[21,22]
The best modality of treatment for acute tendoachilles tendon ruptures remains contentious and no consensus has been reached between conservative versus operative treatment. Among operative techniques, percutaneous repair has proven to reduce risk of infection and wound necrosis compared to open repair techniques, but has an increased incidence of rerupture of tendon.[23] The Dresden technique is a popular, percutaneous technique being used with excellent results in acute TA tears, but the requirement of special instrumentation and the minor wound-related problems (27%) and rerupture rates (1–3%)[24,25] encourages us to develop better techniques with easily available surgical materials.
In the bid to reduce surgery related complications, evolution of surgical techniques continues. Our institute came up with this technique and has proven to give good results. At present, we have included only six patients in our case series and we continue to use this technique to treat all patients with closed, acute tendoachilles tears. Further studies are needed to evaluate a larger cohort of patients treated by this technique and to compare the results of our technique with existing ones over longer periods.
CONCLUSION
The most important take away message from our study is that maintaining a skin bridge can overcome wound related complications in surgical repair of Tendoachilles tendon tears. Repairing the tendon in 2 planes through the calcaneal tuberosity can reduce chances of re-rupture and a postoperative cast that allows knee flexion while preventing complete extension is useful in preventing knee stiffness while the tendon heals. We will continue to study and evolve this technique and compare it with other surgical methods to treat Tendoachilles tears, and publish our results as we collect more scientific data.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Long-term prognosis of patients with achilles tendinopathy. An observational 8-year follow-up study. Am J Sports Med. 2000;28:634-42.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical series of three hundred and twenty two cases of Achilles tendon section with laceration. Int Orthop. 2016;41:309-13.
- [CrossRef] [PubMed] [Google Scholar]
- A new incision for surgery on tendo Achillis using a distally-based fasciocutaneous flap. J Bone Joint Surg Br. 2002;84:1142-4.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous versus open repair of the ruptured Achilles tendon: A comparative study. Am J Sports Med. 2005;33:1369-79.
- [CrossRef] [PubMed] [Google Scholar]
- Operative versus nonoperative treatment for acute Achilles tendon rupture: A meta-analysis based on current evidence. Int Orthop. 2012;36:765-73.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of acute Achilles tendon ruptures: A systematic overview and meta-analysis. Clin Orthop Relat Res. 2002;400:190-200.
- [CrossRef] [PubMed] [Google Scholar]
- Rerupture and deep infection following treatment of total Achilles tendon rupture. J Bone Joint Surg Am. 2002;84A:2016-21.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of Achilles and posterior tibial tendon surgeries. Clin Orthop Relat Res. 2001;391:133-9.
- [CrossRef] [PubMed] [Google Scholar]
- Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791-9.
- [CrossRef] [PubMed] [Google Scholar]
- Review of the operative treatment of Achilles tendon rupture. Clin Orthop Relat Res. 1985;201:80-3.
- [CrossRef] [Google Scholar]
- Operative versus nonoperative management of acute Achilles tendon rupture: Expected-value decision analysis. Am J Sports Med. 2002;30:783-90.
- [CrossRef] [PubMed] [Google Scholar]
- Operative versus nonoperative treatment of acute Achilles tendon ruptures: A quantitative review. Clin J Sport Med. 1997;7:207-11.
- [CrossRef] [PubMed] [Google Scholar]
- Augmented compared with non-augmented surgical repair after total Achilles rupture: Results of a prospective randomized trial with thirteen or more years of follow-up. J Bone Joint Surg. 2016;98:85-92.
- [CrossRef] [PubMed] [Google Scholar]
- Open versus minimal invasive repair with Achillon device. Foot Ankle Int. 2009;30:391-7.
- [CrossRef] [PubMed] [Google Scholar]
- Limited open repair of Achilles tendon ruptures: A technique with a new instrument and findings of a prospective multicenter study. J Bone Joint Surg Am. 2002;84:161-70.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive versus open surgery for acute Achilles tendon rupture: A systematic review. Br Med Bull. 2014;109:45-54.
- [CrossRef] [PubMed] [Google Scholar]
- Is percutaneous repair better than open repair in acute Achilles tendon rupture? Clin Orthop Relat Res. 2012;470:998-1003.
- [CrossRef] [PubMed] [Google Scholar]
- Review of the vascularisation of the human Achilles tendon. Injury. 2005;36:1267-72.
- [CrossRef] [PubMed] [Google Scholar]
- Use of fluroquinolone and risk of Achilles tendon rupture: A population-based cohort study. Eur J Clin Pharmacol. 2007;63:499-503.
- [CrossRef] [PubMed] [Google Scholar]
- Partial Achilles tendon ruptures associated with fluoroquinolone antibiotics: A case report and literature review. Foot Ankle Int. 1996;17:496-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fluoroquinolones and Achilles tendinopathy in renal transplant recipients. Transplantation. 1994;58:736-7.
- [CrossRef] [PubMed] [Google Scholar]
- Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. A prospective, randomized clinical and radiographic study. J Bone Joint Surg Am. 1999;81:983-90.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous Achilles tendon repair with the Dresden instrument. Clinical and MRI evaluation of 90 patients. Foot Ankle Surg. 2020;26:209-17.
- [CrossRef] [PubMed] [Google Scholar]
- The percutaneous suture of the Achilles tendon with the Dresden instrument. Oper Orthop Traumatol. 2006;18:287-99.
- [CrossRef] [PubMed] [Google Scholar]






