Translate this page into:
A novel glenoid classification for pre-operative planning in reverse shoulder arthroplasty: “Chandigarh Classification”
*Corresponding author: Manit Arora, Department of Orthopedics and Sports Medicine, Fortis Hospital Mohali, Mohali, Punjab, India. manit_arora@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arora M, Shah JV, Prajapati SS. A novel glenoid classification for pre-operative planning in reverse shoulder arthroplasty: “Chandigarh Classification”. J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_7_2025
Abstract
Objectives
Reverse shoulder arthroplasty has seen tremendous uptake over the past two decades with better implant designs, higher usage, and expanding indications. One of the major limitations of the traditional Walch classification for glenoid morphology is that it does not factor in the overall size of the glenoid and, hence, baseplate fit. The aim of the present retrospective cohort study was to develop a new classification system for glenoid morphology and undertake its frequency mapping in our patient population.
Materials and Methods
Institutional ethics approval was obtained from the Institutional Review Board before the initiation of the study. Data from a previously conducted computed tomography (CT)-based study at our institute of 600 normal shoulders were used to develop a new classification system for glenoid morphology. 2D and 3D CT scans of shoulders being operated for reverse shoulder arthroplasty from January 2022 to March 2023 were retrospectively included in the frequency mapping analysis. Inter-observer reliability of the new classification was also assessed.
Results
The new classification combines the circle concept (to assess baseplate fit) with the traditional Walch Classification (to assess glenoid wear and version). Glenoids are divided into two types: Type O (<25 mm maximum anteroposterior [AP] diameter) and Type N (≥25 mm maximum AP diameter). Each type is subdivided into 3 subtypes according to Walch A, B, and C. A total of 120 patients were included in the retrospective analysis, with the vast majority being either walch A with overhang of base plate (AO) (42%) or Walch A with normal fit baseplate (AN) variants (36%). The new classification has a high degree of inter-observer reliability (kappa value = 0.878).
Conclusion
Our proposed new glenoid classification (the “Chandigarh classification”) incorporates both glenoid size and wear pattern. The single highest frequency population was AO glenoids, suggesting that a large proportion of patients have baseplate overhang (with a 25 mm baseplate) on a relatively symmetrical glenoid.
Keywords
Arthroplasty
Classification
Glenoid bone loss
Reverse shoulder replacement
Shoulder arthroplasty
Shoulder replacement
INTRODUCTION
Reverse shoulder arthroplasty has seen increased uptake globally in recent years attributable to wider availability of the implant, better outcomes as compared to previous generations of prosthesis design, more surgical training and exposure, and expanding indications. The most common indications of glenohumeral pathology include rotator cuff tear arthropathy, glenohumeral arthritis with glenoid bone loss, acute and delayed treatment of proximal humerus fractures, failed anatomic shoulder arthroplasty, chronic shoulder dislocations in the elderly population, massive irreparable rotator cuff tears with or without arthritis, and rheumatoid arthritis.[1-5] Further, the latest data on long-term outcomes have been encouraging, with implant survivorship of 91–93% at 10-year follow-up and persistently improved outcome scores.[1,6] These findings, when combined with the expanding indications and our aging population, suggest that reverse shoulder arthroplasty (RSA) has a long future in the shoulder surgeon’s arsenal.
As the uptake of RSA has increased, so has the demand from surgeons for better pre-operative assessment of glenoid morphology to ensure better outcomes. A computed tomography (CT) scan is a very useful tool for the characterization of glenoid morphology. CT scan provides an accurate and detailed assessment of the glenoid with regard to the version, inclination, wear pattern, bone quality, and integrity of the glenoid vault. Proper pre-operative understanding of these factors guides implant choice.[7-9]
Walch et al. (1999) outlined a classification for glenoid wear in primary glenohumeral arthritis,[10] with a higher Walch classification being a negative predictor for post-operative clinical function, as well as progression of posterior bone loss over time.[11,12] Walch classified glenoid wear patterns as Types A, B, and C. Friedman et al. showed that CT scans were a good modality to assess these wear patterns.[13] However, the Walch classification has a major limitation in that it does not factor in the size of the glenoid.
Accordingly, the purpose of the present retrospective cohort study was to develop a new classification system for glenoid morphology that assesses both glenoid size and wear and to undertake its frequency mapping in our patient population.
MATERIALS AND METHODS
Patient recruitment, inclusion, and exclusion criteria
Institutional ethics approval was obtained from the institutional ethics review board before the initiation of the study. Data from a previously conducted CT-based study of 600 normal shoulders at our institute were used to assess average glenoid dimensions in our patient population (average glenoid max anteroposterior [AP] diameter 23.2 ± 0.6 mm). Based on this, we developed a new classification system that incorporates both glenoid size (as assessed by the beforementioned study) and glenoid wear pattern (Walch classification).
The new classification system was then studied retrospectively to assess frequency mapping in our patient population. A retrospective analysis of CT scans of patients undergoing RSA at our institute from January 2022 to March 2023 was carried out. Written informed consent was taken from all patients before using their CT scans in the analysis. Inclusion criteria were patients over the age of 60 years undergoing RSA at our institute during the retrospective study period, CT scans done at our institute (to eliminate cross-center bias), and those willing to participate in the study. Exclusion criteria were patients <60 years of age, patients who had CT scans done at outside centers, and patients unwilling to participate in the study.
Study power calculation
Using a correlation coefficient of 0.03 to study the null hypothesis, we found that the sample size should be 80 patients for a moderately high power and reduced error rate. Using 120 patients, the alpha score is <0.01.
CT scan-based measurements
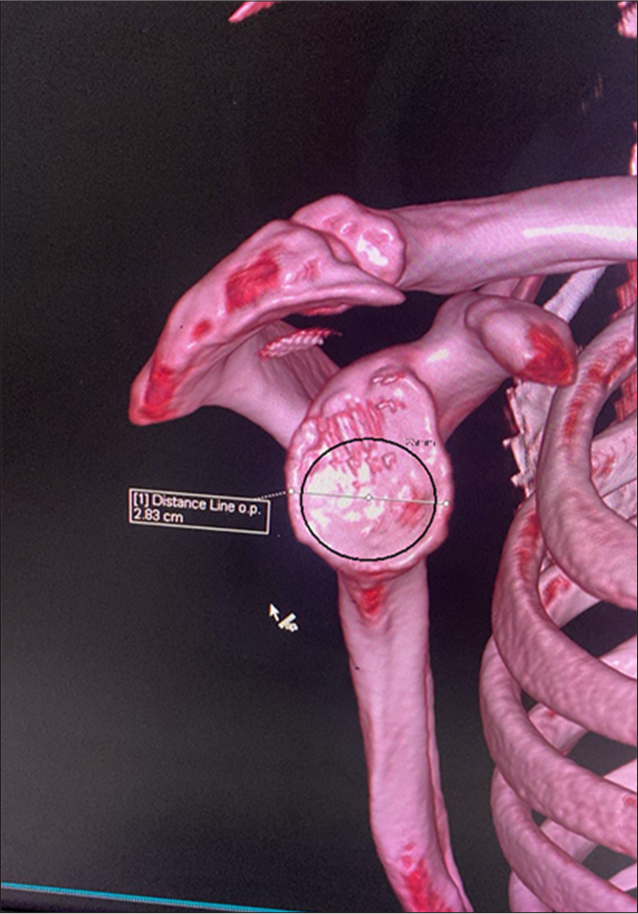
Two measurements were taken for all patients on 2D CT and 3D reformatted CT scans: Degree of retroversion (Walch Classification) and maximum AP dimension of the glenoid face (circle concept). The best way to assess the glenoid interface is through the three-dimensional reconstruction of two-dimensional CT images. These aid in understanding and defining patient-specific glenoid anatomy and location of wear.[14,15] Werner et al. showed that measurements of glenoid version and inclination were more accurate with 3D reconstruction images as compared to 2D reconstructions.[16] Walch classified glenoid wear patterns as Types A, B, and C. Friedman et al. showed that CT scans were a good modality to assess these wear patterns.[13] Since its inception, the classification has undergone refining by various authors, with the present classification as such [Figure 1]. For the present study to adapt to the new proposed glenoid model, we measured the retroversion according to the traditional and more simplistic Walch classification. Type A is centered or symmetric arthritis without posterior subluxation of the humeral head. Type B is characterized by asymmetric arthritis with posterior subluxation of the humeral head. Type C shows glenoid retroversion >25° (dysplastic in origin) regardless of glenoid erosion or the location of the humeral head with regard to the glenoid.[17]
![Modified Walch classification as it stands at present.[17]](/content/115/2025/0/1/img/JASSM-7-2025-g001.png)
- Modified Walch classification as it stands at present.[17]
The baseplate overhang was assessed using the circle concept to determine baseplate fit on glenoids [Figure 2]. A circle is defined as the maximum possible circular area placed over the patient’s inferior glenoid, which encloses it without any bone deficiency in any quadrant in a 3D CT scan-based enface view of the glenoid. The circle is used to represent the base plate of reverse arthroplasty (in this case, the smallest baseplate available, which is 25 mm but can be adapted per user), and the diameter of the circle relates to the size of the base plate. Thus, the circle uses the maximum AP dimension of the glenoid at its largest point to determine the ideal surface area available for baseplate fit. If the diameter of the circle (baseplate size) was larger than the maximum AP diameter of the glenoid, this was defined as O. If the diameter of the circle was smaller than the maximum AP diameter of the glenoid, this was defined as N.
- Circle concept. The circle is overlaid on a 3D computed tomography scan-based enface view of the glenoid and sized for the baseplate dimensions (in the representative case for a 25 mm baseplate).
Inter-observer reliability
To assess the inter-observer reliability, we selected 28 shoulders from our data set. The new classification model was sent to two previous fellows of the institute who were taught how to use the classification, and they were instructed that they would receive CT data for 18 patients and that they must classify each patient.
Data collection and statistical analysis
Retrospective analysis of pre-operative CT scans of enrolled subjects was carried out by a single author (SP). Frequency mapping of each CT scan was done according to the new proposed classification subtypes (AO, BO, CO, AN, BN, and CN). The age and gender of the patients were recorded at the time of index surgery. The statistical analysis was performed by a single-blinded author (JS) using IBM Statistical Package for the Social Sciences 20 software. Frequency mapping characteristics were studied using numerical charting. A simple t-test was used to assess for differences between groups with respect to age and gender. The significance level adopted was P < 0.05.
RESULTS
New proposed classification – “Chandigarh classification”
The new classification combines the circle concept (to assess baseplate fit) with the traditional Walch Classification (to assess glenoid wear and version). Circle measurements are based on the smallest available baseplate diameter (25 mm). Circles are divided into two types: Type O (<25 mm maximum AP diameter) and Type N (≥25 mm maximum AP diameter). The Type O circles will have an overhang of the smallest baseplate on the native glenoid, whereas Type N circles will have a just or normal fit on the glenoid. The new classification is outlined below [Table 1 and Figure 3].
| Type A Walch (concentric wear) | Type B Walch (asymmetric wear) | Type C Walch (dysplastic glenoid, >25° retroversion) | |
|---|---|---|---|
| Type O Circle (<25 mm maximum AP diameter) | AO | BO | CO |
| Type N Circle (≥25 mm maximum AP diameter) | AN | BN | CN |
O: Overhang of baseplate, N: Normal fit base plate, A/B/C: Walch classifications
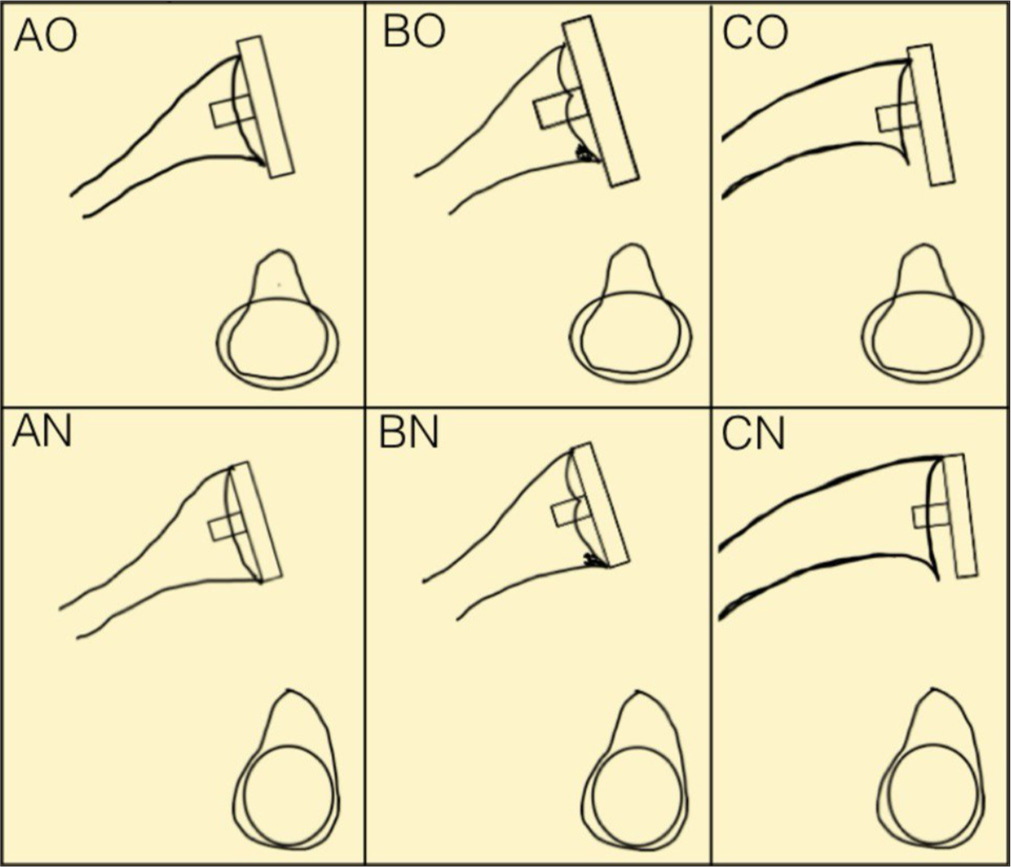
- Diagrammatic representation of the new proposed classification system. O: Overhang of baseplate, N: Normal fit base plate. A/B/C: Walch classification.
Frequency mapping data
A total of 120 patients were included in the retrospective analysis. A total of 68 females (57%) and 52 males (43%) were enrolled in the study. The average age of the patient population was 68.2 ± 6.4 years. 68% of patients (n = 82) were below 70 years of age and the remaining were more than 70 years of age at the time of index surgery.
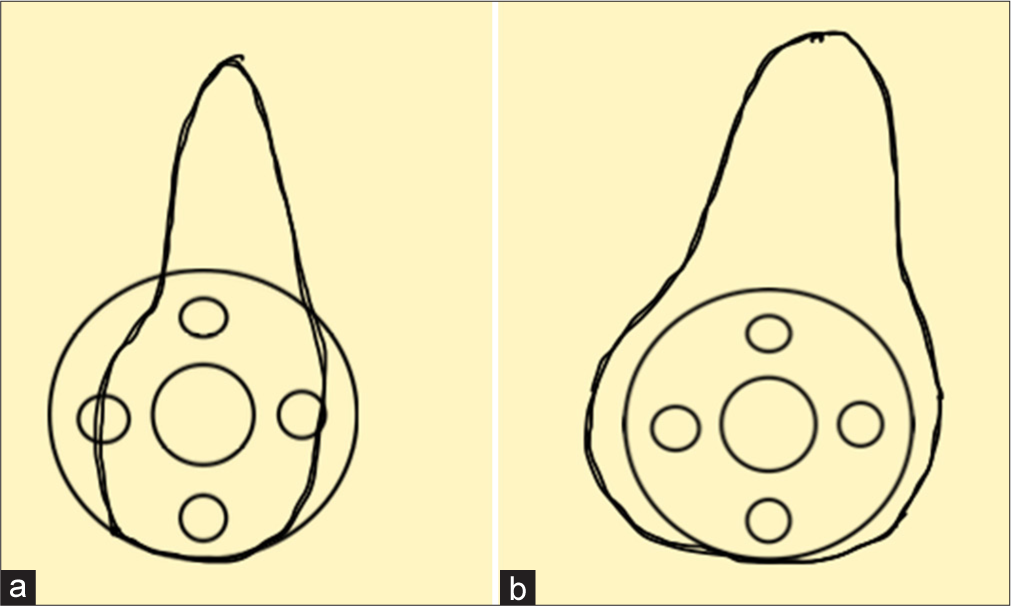
According to the new classification, the frequency mapping data are presented in Table 2 and Figure 4. Most patients were either type AO (42%) or AN variants (36%). 55% of patients (n = 66) had overhang (Type O) of the baseplate on the glenoid. Less than 10% of patients (n = 8; 7%) had severely retroverted glenoids (Walch C).
| Walch A | Walch B | Walch C | |
|---|---|---|---|
| Type O | 50 | 11 | 5 |
| Type N | 43 | 8 | 3 |
O: Overhang of baseplate, N: Normal fit base plate. A/B/C: Walch classification
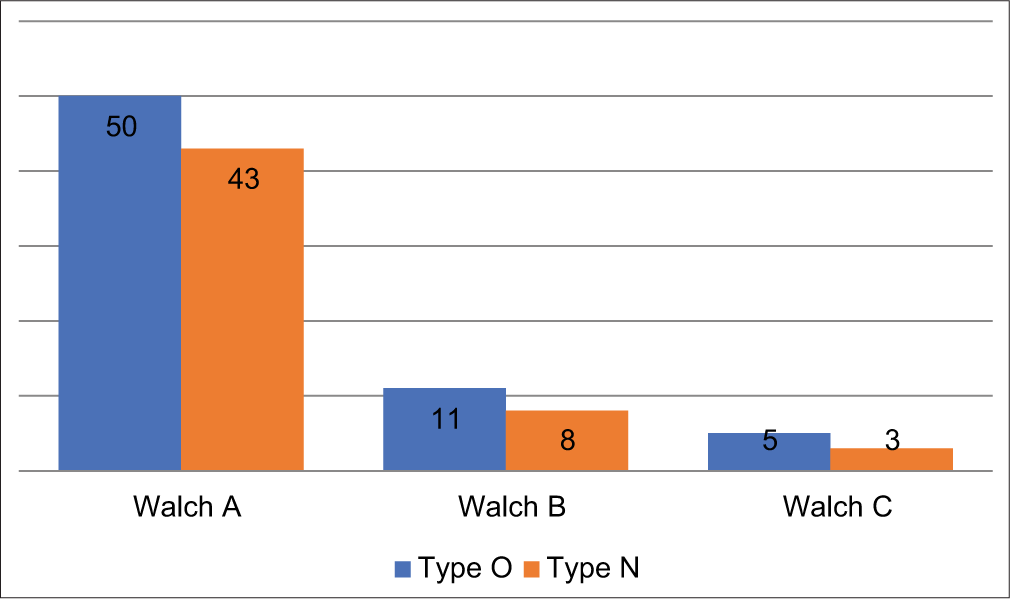
- Graphical representation of frequency mapping data of study population (n = 120 patients). O: Overhang of baseplate, N: Normal fit base plate. A/B/C: Walch classification.
Subgroup analysis
Age and gender were assessed for variation between the types of new proposed classification. Neither age nor gender showed any significant correlation between the subgroups of the new classification.
Inter-observer reliability
Rater 1 and Rater 2 reliability data for the subset of 28 patients are presented in Table 3. A good to strong level of agreement was seen between both raters, with a kappa value of 0.878 with a statistical significance of <0.005.
| Rater | Result | Rater 2 | Rater 2 | Total |
|---|---|---|---|---|
| Failure | Success | |||
| Rater 1 | Failure | 9 | 3 | 12 |
| Rater 1 | Success | 3 | 13 | 16 |
| Total | 12 | 16 | 28 |
DISCUSSION
Importance of baseplate and glenosphere positioning in shoulder arthroplasty
Reverse shoulder arthroplasty has seen increased uptake globally in recent years attributable to wider availability of the implant, better outcomes as compared to previous generations of prosthesis design, more surgical training and exposure, and expanding indications. With this increasing uptake comes a need to optimize outcomes, and one of the most important aspects of that is baseplate and glenosphere positioning in RSA. Glenosphere positioning has a significant impact on the clinical outcomes of RSA. Malpositioning increases the risk of complications, including dislocation, scapular notching, decreased range of motion, and component loosening.[18-20]
Glenosphere positioning is determined by surgical technique, and reasons for its malpositioning include inaccurate assessment of pathological anatomy, incorrect choice of implant and/or positioning of the implant to correct pathology and inaccurate execution of preoperative plan at the time of surgery.[21,22] All the above factors are influenced by both glenoid exposure and the degree of glenoid bone loss. In the setting of minimal glenoid bone loss, surgical decision-making is simpler with the use of intraoperative assessments such as the surface of the glenoid fossa, the “subchondral smile” method, or standard inferior tilt guides. However, some studies have shown that these references can also be unreliable.[23,24] In the setting of moderate-to-severe glenoid bone loss, surgical decision-making is much more difficult, hence the role of pre-operative planning or patient-specific instrumentation techniques.
As glenosphere positioning is determined by baseplate positioning primarily and the baseplate by the glenoid face hence the role of pre-operative glenoid planning is paramount. To better understand glenoid morphology, a host of classifications has been developed by various authors, however, the mainstay remains the Walch classification.
Walch classification and its limitations
Walch et al. (1999) outlined a classification for glenoid wear in primary glenohumeral arthritis,[10] with a higher Walch classification being a negative predictor for post-operative clinical function, as well as progression of posterior bone loss over time.[11,12] In the present study, we have used the traditional Walch classification; however, the Walch classification has undergone modifications over time. Type A is centered or symmetric arthritis without posterior subluxation of the humeral head. Type A1 has minor central wear or erosion, whereas Type A2 has severe or major central wear or erosion. Type B is characterized by asymmetric arthritis with posterior subluxation of the humeral head. Type B1 has no obvious glenoid erosion with posterior joint space narrowing, subchondral sclerosis, and osteophytes. Type B2 has apparent or obvious erosion of the posterior glenoid, forming a biconcave appearance of the glenoid. Type C shows glenoid retroversion >25° (dysplastic in origin) regardless of glenoid erosion or the location of the humeral head with regard to the glenoid.[17]
The classification has several limitations, especially the inconsistent reproducibility among orthopedic surgeons. As the Walch classification has expanded to include subtypes, intraobserver and interobsever reliability has decreased.[17,25] The distinction between type B and C glenoids due to dysplastic wear versus glenoid wear has also drawn controversy. The Walch classification also addresses only posterior wear, with no descriptions of anterior or superior wear patterns, and relies on 2D scans for assessment rather than 3D techniques, which are more adequate in the modern era of shoulder planning.[26]
Although the Walch Classification or its modification helps with pre-operative planning for the purpose of determining posterior asymmetry of the glenoid and the need for potential bone grafting or building the glenoid intra-operatively, it offers little in terms of the fit of the baseplate on the glenoid. In our practice, one of the common problems we have been facing is the ability to determine baseplate fit or overhang of the baseplate in our region, where the glenoid sizes are comparatively smaller as compared to Western populations. To this effect, we had previously performed a CT-based study to assess glenoid morphology (under publication), where we found that the average glenoid dimensions in our population (mean: 23.2 ± 0.6 mm) are smaller than the 25 mm baseplate. This means that some amount of baseplate overhang will exist in the majority of our patients, even with these small baseplates [Figure 5]. The morphology of the glenohumeral joint varies geographically.[27,28] Most of the literature on the morphology of the glenoid refers to the Western population. There are few such data for the Indian population.[29,30] Most Indian studies are anatomical studies on a cadaver with a small sample size, and a few are based on CT scans.[29,31,32] The CT scan gives us the advantage of assessing the morphology of the glenoid and humeral head preoperatively.
- Baseplate overhang seen in (a) South Asia due to smaller glenoid dimensions as compared to (b) western population.
This concept is important as it allows us to determine how much of the glenoid surface area of the native glenoid, irrespective of version, is available for the baseplate. Thus, baseplates can be sized accordingly and pre-operatively without the need for specific or advanced pre-operative planning software.
New classification addresses both fit and version of glenoid
With the new classification, both baseplate fit and version are factored into the pre-operative planning in a single classification. Technically, the AN fit is the best fit as it provides normal baseplate fitting along with a concentric wear pattern, whereas the CO fit is the worst fit as it provides an overhang of the baseplate with dysplastic wear of the glenoid. Frequency mapping data showed that the vast majority of patients were in the AO or AN subtypes. What is surprising to see is the large number of patients with an AO subtype, suggesting an overhang of the small baseplate on the native glenoid. This is an important assessment as it highlights that a significant proportion of patients in our population may not have the ideal baseplate coverage despite a decent version.
The new classification is simple and reproducible as it has six types and is based on readily available 2D CT scans and reformatted 3D CT scans, which are available at most hospitals. The reproducibility of the new classification system was tested using two raters with a high degree of inter-observer reliability. The new proposed classification should help surgeons in clinical decision-making by not only factor in the fit of the glenoid baseplate but also the version of the baseplate and the need for potential augmentation. Although our model has been developed with a 25 mm baseplate (the smallest baseplate size available to us in our region), surgeons may adapt the classification according to the smallest baseplate size available in their region.
Frequency mapping data versus available literature
The frequency mapping data of the new classification system yields some salient findings. First, 78% of patients had a Walch A glenoid, with <10% having a Walch C glenoid. Importantly, 55% of patients were in overhang with a circle diameter of <25 mm. The circle diameters method, established by Sugaya et al.,[33] allows us to better understand baseplate fit. Circle diameter measurements from our study show significantly lower measurements as compared to the max glenoid width of previous studies,[34-38] with 55% of patients having a circle diameter <25 mm. This bears biomechanical significance because although using smaller baseplates has not been shown to lead to higher strain at the baseplate-glenoid interface,[39] it may actually increase the impingement-free range of motion of the shoulder.[40]
Limitations of the new classification
The new proposed classification has its own limitations. First, the baseplate size used is 25 mm (the smallest available baseplate in our region), however, this may be adapted as per the user. Second, the traditional Walch classification rather than the modified Walch classification has been used. The rationale behind this was to keep the proposed new classification as simple to reproduce as possible, especially for younger surgeons.
CONCLUSION
The modified Walch classification for assessing glenoid wear does not factor into the size of the glenoid or maximum AP dimension. Our proposed new classification, the “Chandigarh classification,” employs the circle method to help incorporate both glenoid size and version. The new classification has high inter-observer reliability and should aid surgeons in pre-operative planning for RSA.
Author contributions
MA: Conceptualized the manuscript, was primary author, and did statistical analysis; JS: Involved in editing the manuscript, figures, and table preparation; SP: Involved in data collection.
Ethical approval
The research/study was approved by the Institutional Review Board at Institutional Ethics Review Committee Fortis Mohali, number 2021-65/3, dated 2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am. 2013;95:2050-5.
- [CrossRef] [PubMed] [Google Scholar]
- Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop. 2010;468:1526-33.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of acquired glenoid bone defects on surgical technique and clinical outcomes in reverse shoulder arthroplasty. J Bone Joint Surg Am. 2010;92:1144-54.
- [CrossRef] [PubMed] [Google Scholar]
- Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Jt Surg Am. 2013;95:1297-304.
- [CrossRef] [PubMed] [Google Scholar]
- Pre-operative planning for reverse shoulder replacement: The surgical benefits and their clinical translation. Ann Jt. 2019;4:4.
- [CrossRef] [Google Scholar]
- Long-term outcomes of reverse total shoulder arthroplasty: A follow-up of a previous study. J Bone Joint Surg Am. 2017;99:454-61.
- [CrossRef] [PubMed] [Google Scholar]
- Quantification of regional variations in glenoid trabecular bone architecture and mineralization using clinical computed tomography images. J Orthop Res. 2018;36:85-96.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative assessment and characterization of glenoid bone loss in a spectrum of patients with glenohumeral osteoarthritis. Musculoskelet Surg. 2016;100:179-85.
- [CrossRef] [PubMed] [Google Scholar]
- Cement stress predictions after anatomic total shoulder arthroplasty are correlated with preoperative glenoid bone quality. J Shoulder Elbow Surg. 2017;26:1644-52.
- [CrossRef] [PubMed] [Google Scholar]
- Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14:756-60.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of medium-term clinical outcomes after total shoulder arthroplasty. Arch Orthop Trauma Surg. 2017;137:187-93.
- [CrossRef] [PubMed] [Google Scholar]
- Progression of glenoid morphology in glenohumeral osteoarthritis. J Bone Joint Surg Am. 2018;100:49-56.
- [CrossRef] [PubMed] [Google Scholar]
- The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am. 1992;74:1032-7.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of CT-based measurements of glenoid version for total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:166-71.
- [CrossRef] [PubMed] [Google Scholar]
- Use of three-dimensional computed tomography for the analysis of the glenoid anatomy. J Shoulder Elbow Surg. 2005;14:85-90.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of three-dimensional planning on decision-making in total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1477-83.
- [CrossRef] [PubMed] [Google Scholar]
- Revisited: Walch classification of the glenoid in glenohumeral osteoarthritis. Shoulder Elbow. 2012;4:11-5.
- [CrossRef] [Google Scholar]
- Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: An analysis of 476 shoulders. J Shoulder Elbow Surg. 2017;26:1253-61.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of scapular neck length to scapular notching after reverse total shoulder arthroplasty by use of plain radiographs. J Shoulder Elbow Surg. 2014;23:882-7.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89:588-600.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional preoperative planning software and a novel information transfer technology improve glenoid component positioning. J Bone Joint Surg Am. 2014;96:e71.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of glenoid deformity on glenoid component placement in primary shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:48-55.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of the subchondral smile and surface referencing techniques in reverse shoulder arthroplasty. Orthopedics. 2016;39:e615-20.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of placement of the glenoid component in reversed shoulder arthroplasty with and without navigation. J Shoulder Elbow Surg. 2011;20:21-6.
- [CrossRef] [PubMed] [Google Scholar]
- Inter-rater reliability of an arthritic glenoid morphology classification system. J Shoulder Elbow Surg. 2008;17:575-7.
- [CrossRef] [PubMed] [Google Scholar]
- Classifications in brief: Walch classification of primary glenohumeral osteoarthritis. Clin Orthop Relat Res. 2017;475:2335-40.
- [CrossRef] [PubMed] [Google Scholar]
- Morphologic variability of the shoulder between the populations of North American and East Asian. Clin Orthop Surg. 2016;8:280-7.
- [CrossRef] [PubMed] [Google Scholar]
- What differences in morphologic features of the knee exist among patients of various races? A systematic review. Clin Orthop. 2017;475:170-82.
- [CrossRef] [PubMed] [Google Scholar]
- Morphometric analysis of glenoid cavity of dry scapulae and its role in shoulder prosthesis. Int J Res Med Sci. 2017;4:2770-6.
- [CrossRef] [Google Scholar]
- 3D CT scan-based study of glenoid morphology in Indian population: Clinical relevance in design of reverse total shoulder arthroplasty. J Clin Orthop Trauma. 2020;11(Suppl 4):S604-9.
- [CrossRef] [Google Scholar]
- The glenoid cavity: Its morphology and clinical significance. 2016. Available from: https://www.biomedscidirect.com/2166/the_glenoid_cavity_its_morphology_and_clinical_significance/articlescategories [Last accessed on 2021 Aug 05]
- [Google Scholar]
- IJARS - Glenoid cavity index, Gleno-humeral joint, Glenoid cavity, Humerus, Shoulder joint. Available from: http://ijars.net/article_fulltext.asp?issn=0973-709x&year=2019&month=July&volume=8&issue=3&page=AO06-AO09&id=2487 [Last accessed on 2022 Mar 02]
- [Google Scholar]
- Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85:878-84.
- [CrossRef] [PubMed] [Google Scholar]
- Glenoid size, inclination, and version: An anatomic study. J Shoulder Elbow Surg. 2001;10:327-32.
- [CrossRef] [PubMed] [Google Scholar]
- A Morphometric study of the patterns and variations of the acromion and glenoid cavity of the scapulae in Egyptian population. J Clin Diagn Res JCDR. 2015;9:AC08-11.
- [CrossRef] [PubMed] [Google Scholar]
- The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992;74:491-500.
- [CrossRef] [PubMed] [Google Scholar]
- Computational assessment of glenoid morphology in us and Australian patients. Orthop Proc. 2016;98B(Supp 9):6.
- [Google Scholar]
- Three-dimensional assessment of the normal Japanese glenoid and comparison with the normal French glenoid. Orthop Traumatol Surg Res. 2017;103:1271-5.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of glenosphere and baseplate parameters on glenoid bone strains in reverse shoulder arthroplasty. BMC Musculoskelet Disord. 2019;20:587.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of baseplate size on primary glenoid stability and impingement-free range of motion in reverse shoulder arthroplasty. BMC Musculoskelet Disord. 2014;15:417.
- [CrossRef] [PubMed] [Google Scholar]







