Translate this page into:
Arthroscopic capsular release for adhesive capsulitis secondary to diabetes provides better functional outcome than conservative management
*Corresponding author: Skand Sinha, Sports Injury Centre, VMMC, New Delhi, Delhi, India. skandsinha@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bansiwal K, Bhavani P, Singh B, Goyal A, Naik AK, Sinha S. Arthroscopic capsular release for adhesive capsulitis secondary to diabetes provides better functional outcome than conservative management. J Arthrosc Surg Sports Med 2022;3:12-7.
Abstract
Objectives:
Comparison of outcome of subacromial bursal resection with capsular release for adhesive capsulitis of shoulder secondary to diabetes, with conservative management.
Materials and Methods:
This study was conducted on 68 patients of adhesive capsulitis of shoulder secondary to diabetes. The patients were divided into two groups: Arthroscopic capsular release group (group I n 32) and Conservative management group (Group II n 36) after fulfilling inclusion/ exclusion criteria. Follow-up was done at 2, 6, 24 weeks, 6 months, 1 year, and 2 years. In addition to pre-operative measurement, at each follow-up pain was assessed by visual analog scale (VAS), range of motion (ROM) was assessed by goniometer and functional outcome was assessed by Constant-Murley score. Values obtained were filled in Excel sheet and analyzed by independent t-test, Wilcoxon Rankosin test, and Analysis of Variance test on Statistical Package for the Social Sciences software.
Results:
Two patients in Group I and six in Group II were lost to follow-up. There was statistically significant improvement in VAS of both groups at each follow-up, but the noticeable difference was that the patients in arthroscopic release group were pain free by 6 weeks and the pain relief was sustained till final follow-up. In contrast, though there was pain relief in conservative group but they were not completely pain free till final follow-up. There was statistically significant improvement in Constant Murley score in both groups at each follow-up but arthroscopic release group achieved near normal score by 6 months and the improvement was maintained till last follow-up. The comparison of mean and median values of ROM, between the arthroscopic capsular release group and conservative group were statistically significant (P value of 0.001) for each movement.
Conclusion:
The improvement in ROM, decrease in pain, and functional outcome are better in diabetic patients with adhesive capsulitis undergoing Arthroscopic capsular release than conservative management.
Keywords
Adhesive capsulitis shoulder
Arthroscopic release
Conservative management
INTRODUCTION
Adhesive capsulitis results in severe and painful restriction of shoulder range of motion (ROM) due to formation of excessive scar tissue across the joint.[1,2] It adversely affects activities of daily living and consequently impairs quality of life.[3,4] The incidence of idiopathic stiff shoulder is 2–5%[5] but is up to 30% more in diabetic patients, where symptoms are severe and less responsive to treatment.[6]
Current modalities of treatment are physiotherapy,[7,8] intra-articular injection,[9,10] manipulation under general anesthesia (GA),[11] arthroscopic capsular release,[12] Open capsular release,[13,14] or combination of any of the above.
Conservative management is time consuming and requires high degree of compliance.[15] The outcome of intra-articular steroid injection is unpredictable. Manipulation under GA is fraught with risk of fracture of humerus and glenoid[11,16] especially in elderly with osteopenic skeleton. Because of the limitations of above-mentioned treatment modalities, arthroscopic capsular release has become a preferred treatment method in refractory cases. Studies have shown that the added subacromial decompression improved outcome especially in terms of relieving pain.[17-19] However, there are no clear-cut guidelines in the literature regarding preferred method of treatment for this condition, more so in a cohort of diabetic patients.
Aim of this study was time wise serial prospective comparison of clinical outcome after arthroscopic Capsular Release and subacromial decompression with conservative treatment in adhesive capsulitis of shoulder secondary to diabetes in Indian population.
MATERIALS AND METHODS
This study was conducted at a tertiary care hospital after local Institutional Review Board approval. Sixty-eight consecutive patients of adhesive capsulitis with diabetes were included in the study. In addition to thorough clinical examination, radiograph and MRI was done. They were divided into two groups, one was arthroscopic capsular release group (Group I, n = 32) and second was conservative management group (Group II, n = 36).
All medically controlled diabetic patients of adhesive capsulitis with restriction of passive external rotation of at least 50% as compared to normal shoulder, restriction of all movements, pain at night causing sleep disturbance, were included in the study for conservative management [Figure 1].
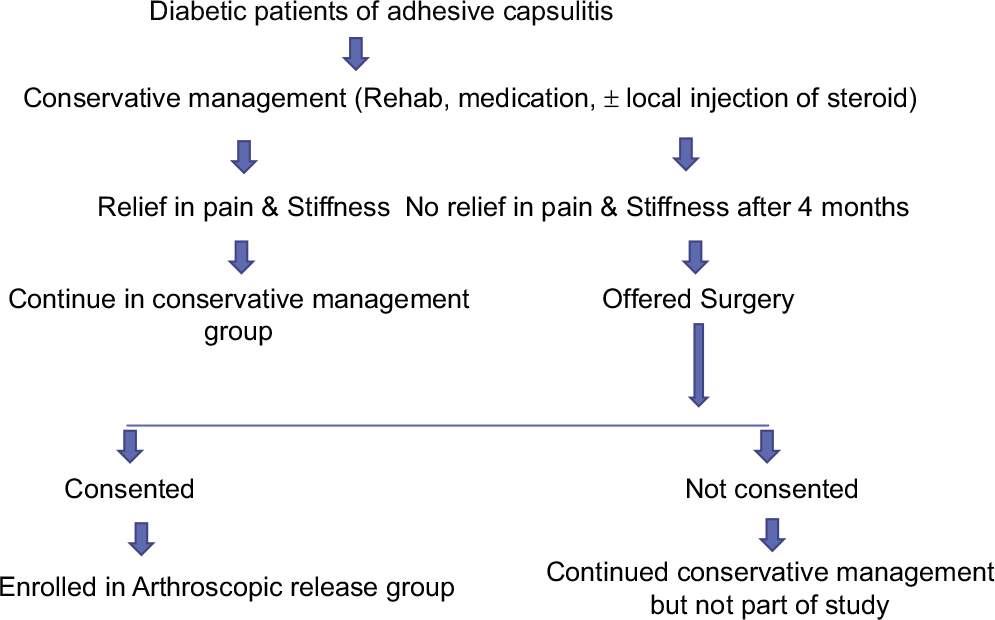
- Patient recruitment protocol.
The patients who failed to improve on conservative management for 4 months were included for arthroscopic release.[5,20] Failure of conservative management was defined as no improvement in ROM and persistent pain especially night pain and was validated by qualified clinician not involved in surgery.
Patients of primary adhesive capsulitis and adhesive capsulitis secondary to other causes other than diabetes, evidence of glenohumeral joint arthritis at the primary procedure, clinical evidence of full or partial thickness rotator cuff tear, subacromial impingement, any fracture involving the shoulder girdle, the previous surgery of the affected shoulder were excluded from the study.
Patients were subjected to standard rehabilitation program [Table 1].
| Rehab for conservative management | Post-operative Rehab | |
|---|---|---|
| 0–2 weeks | 1. Moist heat 2. TENS/UST 3. Anti-inflammatory |
1. Cryotherapy 2. TENS/UST 3. Anti-inflammatory |
| (Supervised Exercise) 1. Codman`s/Pendulum exercise 2. Periscapular strengthening 3. Posterior/Inferior mobilization |
(Supervised Exercise) 1. Rhythmic stabilization for Internal Rotation/External rotation 2. ROM exercise (Active assisted/Active) 3. Periscapular strengthening exercise 4. Stretching exercise |
|
| (Home Exercise) 1. Pendulum exercise 2. ROM exercise in flexion/abduction/ER/IR (passive and active assisted with wand) |
(Home Exercise) 1. Pendulum exercise 2. Active ROM exercise in flexion/abduction/ER/IR in pain tolerance 3. Passive ROM |
|
| 3–12 weeks (Home Exercise) |
In addition to above 1. Active ROM exercise 2. Periscapular strengthening exercise 3. Stretching exercise |
In addition to above 1. Rotator cuff muscle strengthening |
| 12 weeks–1 year | In addition to above 1. Rotator cuff muscle strengthening |
1. Soft tissue therapy for tight pectoral/periscapular muscles 2. ROM exercises at end range 3. Advanced rotator cuff and scapular muscle strengthening 4. Stretching exercise program 5. Plyometric exercise |
| 1–2 years (Home Exercise) |
1. Soft tissue therapy for tight pectoral/periscapular muscles 2. ROM exercises at end range 3. Advanced rotator cuff and scapular muscle strengthening 4. Stretching exercise program 5. Plyometric exercise |
ROM: Range of motion, ER: External rotation, IR: Internal rotation
Conservative management group
All patients in this group continued with standard Adhesive Capsulitis Rehabilitation protocol as shown in the [Table 1].[21] Nineteen cases in this group were given intra-articular steroid.
Arthroscopic capsular release group
Operative procedure
All surgeries were performed by same surgical team under general anesthesia in the lateral decubitus position. Standard posterior viewing portal made after skin preparation and draping. Diagnostic arthroscopy was performed to evaluate for other associated pathologies. Anterior portal was created in the supero-lateral rotator interval beneath the biceps tendon. Release with electro-cautery/arthroscopic punches was started from rotator interval progressing to antero-inferior part of capsule proceeding to postero-inferior part of capsule and finally posterior part. Rotator interval was released including coracohumeral ligament and capsule till coraco-acromial ligament becomes apparent. Biceps tendon and medial sling of the long head of biceps tendon were preserved. Middle glenohumeral ligament is divided and is continued inferiorly staying about 5 mm lateral to the labrum, down to the level of the inferior glenohumeral ligament under direct vision. Then the portals were exchanged, and the posterior capsule is divided preserving the underlying infraspinatus muscle. The dissection is carried out inferiorly down to the 7 o’ clock position. Care was taken during release of inferior capsule because of proximity of axillary nerve and vessels. When full thickness of capsule is released, underlying muscle is visible. After completing the capsular release, the arthroscope is inserted into the sub-acromial space to release any adhesions and debride inflamed bursa using lateral portal. Skin sutures were applied at the portal sites. Routine antibiotics, diclofenac/paracetamol injection, and tablet were instituted. After arthroscopic capsular release, the patients were advised post-operative rehabilitation protocol as shown in [Table 1].
Primary outcomes were measured in terms of VAS, ROM (forward flexion, Abduction, External rotation [ER], and Internal rotation [IR]), and Constant Murley score (CMS). These were recorded serially for every case of either group at pre-operative period, 2 weeks, 6 weeks, 24 weeks, 1 year, and 2 year. Scoring and outcome measurement was done by two authors not involved in surgery. Every parameter was measured thrice, and the best value was recorded.
Statistical analysis
All values obtained serially at different time were filled in excel sheet and analyzed by Statistical Package for the Social Sciences software (version 21). Both inter- and intra-group statistical analysis was done. For descriptive analysis, mean and standard deviation calculated for the continuous variables and for the non-normal continuous variables, median, and interquartile range was calculated. Independent t-test was applied to compare the difference between the two groups of continuous variables that followed normal distribution. Wilcoxon Rankosin test was applied to compare the difference between the groups when continuous variable did not follow normal distribution. Intra-group statistical analysis was done by Analysis of Variance (ANOVA) test.
RESULTS
Two patients in Group I and six in Group II were lost to follow-up. The demographic characteristics of is presented in the [Table 2]. There was no significant difference (P: 0.8) in mean age of Group I (51.4 ± 7.3) and Group II (51.9 ± 7.4). The intra-group analysis using ANOVA test [Table 3] is as follows. The change in mean values of CMS and VAS score with time in weeks of both the groups is shown in [Figures 2 and 3].
| Arthroscopic release Group I | Conservative Group II | |
|---|---|---|
| Enrolled patients | 32 | 36 |
| Loss to follow-up | 2 | 6 |
| Final number | 30 | 30 |
| Age (mean) | 51.40±7.3 | 51.9±7.4 |
| Male | 12 (40%) | 14 (46.66%) |
| Female | 18 (60%) | 16 (53.33%) |
| Right | 17 (56.7%) | 16 (53.3%) |
| Left | 13 (43.3%) | 14 (46.66%) |
| Mean duration of symptoms | 4.2 months | 3.7 months |
| Variables | Group | Arthroscopic release | Conservative | ||
|---|---|---|---|---|---|
| Time | Mean±SD | P-value | Mean±SD | P-value | |
| CMS | 0 | 21.07±5.50 | <0.001 | 21.37±5.67 | <0.001 |
| 2 week | 64.63±5.62 | 24.77±5.44 | |||
| 6 week | 77.8±5.87 | 31.53±4.61 | |||
| 12 week | 88.9±4.97 | 40.23±3.78 | |||
| 6months | 98±1.23 | 49.57±3.55 | |||
| 1 year | 100 | 59.23±3.47 | |||
| 2 year | 100 | 71.97±5.79 | |||
| VAS score | 0 | 8.4±0.89 | <0.001 | 8±1.11 | <0.001 |
| 2 week | 2.5±0.57 | 7.87±0.82 | |||
| 6 week | 0 | 7.33±0.88 | |||
| 12 week | 0 | 6.63±0.93 | |||
| 6months | 0 | 5.83±0.87 | |||
| 1 year | 0 | 4.5±0.86 | |||
| 2 year | 0 | 2.6±0.62 | |||
CMS: Constant Murley score, VAS: Visual analog scale
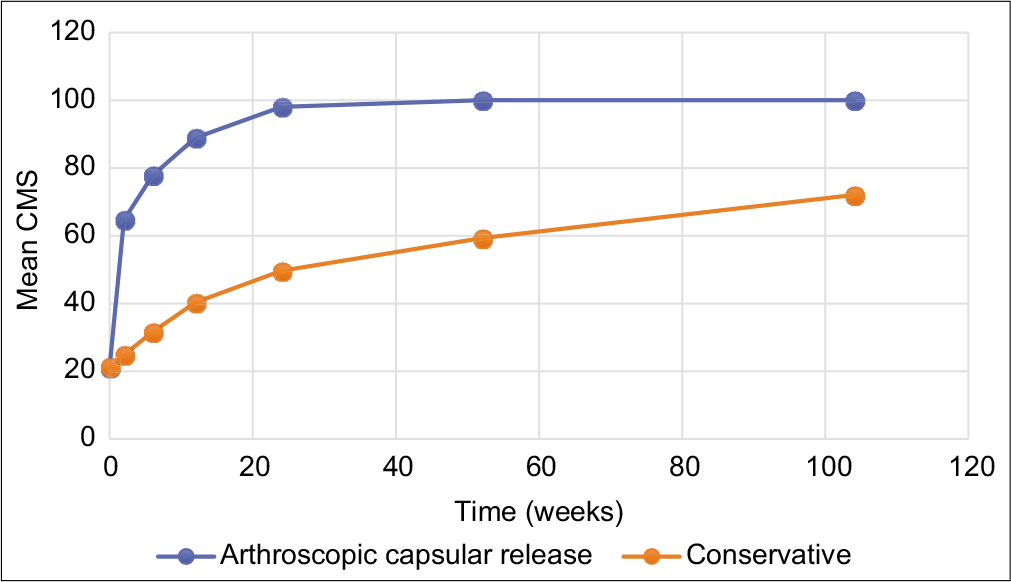
- Improvement of CMS of both groups with time. CMS: Constant murley score
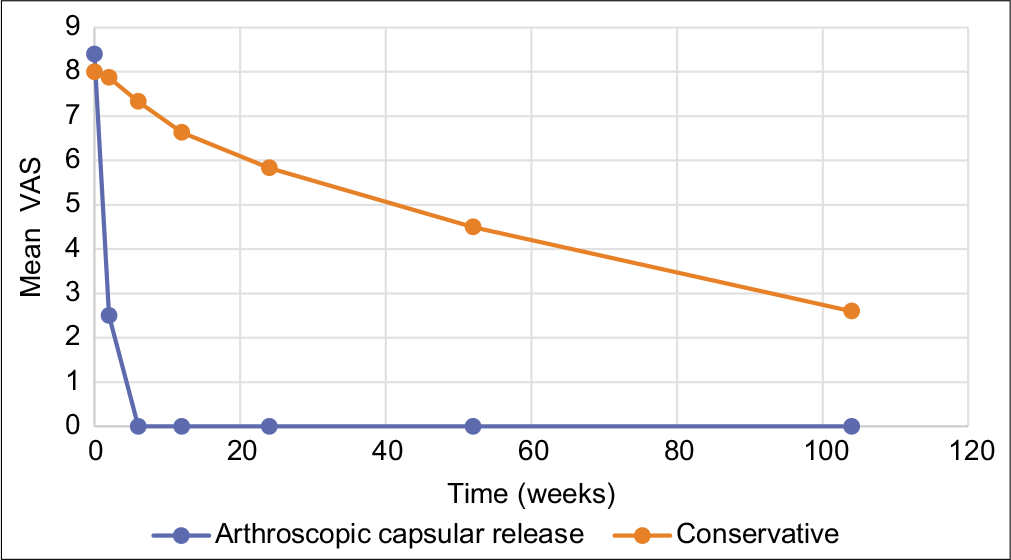
- Improvement of mean VAS score with time. VAS: Visual analog scale
There was statistically significant improvement in VAS of both groups at each follow-up, but the noticeable difference was that the patients in arthroscopic release group were pain free by 6 weeks and the pain relief was sustained till final follow-up. In contrast, though there was pain relief in conservative group but they were not completely pain free till final follow-up.
There was statistically significant improvement in CMS in both groups at each follow-up, but arthroscopic release group achieved near normal score by 6 months and the improvement was maintained till last follow-up.
The comparison of mean and median values of ROM, between the arthroscopic capsular release group and conservative group were statistically significant (P value of 0.001) for each movement [Table 4]. Patients of arthroscopic release group could attain nearly full ROM as early as 6 weeks and could maintain the improvement till last follow-up. In contrast, there was remnant loss of all movements in conservative group at 2 years.
| Arthroscopic release Mean±SD |
Conservative Mean±SD |
Mean difference | Overall 95% CI |
P-value | |
|---|---|---|---|---|---|
| Improvement in abduction | 123.8±12.7 | 59.5±7.7 | 64.29 | (82.23–99.97) | <0.001 |
| Improvement in flexion | 119±11.8 | 62.3±7.9 | 56.67 | (82.88–98.45) | <0.001 |
| Improvement in external rotation | 30.3±4.7 | 15.3±4.1 | 15 | (20.57–25.09) | <0.001 |
| Improvement in extension | 25.5±4.8 | 8.8±5.7 | 16.67 | (14.61–19.72) | <0.001 |
| Improvement in internal rotation | 20.7±4.1 | 12.2±3.1 | 8.5 | (14.97–17.87) | <0.001 |
| Improvement in abduction | 123.8±12.7 | 59.5±7.7 | 64.29 | (82.23–99.97) | <0.001 |
ROM: Range of motion
In inter-group comparison of CMS and VAS score [Table 5], there was no difference at point of recruitment (p = 0.84), but there after at every time of follow-up the difference between both groups was significant (P = 0.001). The P value for difference of mean CMS could not be calculated at 1 year and 2 year follow-up between both groups as the mean of arthroscopic release group had reached 100.
| Variables | Time | Arthroscopic release | Conservative management | Mean Difference (95% CI) | P-value |
|---|---|---|---|---|---|
| Mean±SD | Mean±SD | ||||
| CMS | 0 | 21.07±5.50 | 21.37±5.67 | 0.3 (19.79–22.65) | 0.836 |
| 2 weeks | 64.63± 5.62 | 24.77±5.44 | 39.87 (39.32–50.08) | <0.001 | |
| 6 weeks | 78.57±5.27 | 31.53±4.61 | 47.04 (47.88–60.61) | <0.001 | |
| 12 weeks | 89.34±4.41 | 39.90±3.36 | 49.45 (57.98–71.26) | <0.001 | |
| 6 months | 98±1.23 | 49.57±3.55 | 48.43 (67.44–80.13) | <0.001 | |
| VAS Score | 0 | 8.4±0.89 | 8±1.11 | 0.4 (7.94–8.46) | 0.131 |
| 2 weeks | 2.52±0.57 | 7.79±0.73 | 5.28 (4.39–5.82) | <0.001 | |
| 6 weeks | 0 | 7.33±0.88 | 7.33±0.88 | - |
CMS: Constant Murley score, VAS: Visual analog scale
For VAS, difference of mean was statistically significant (P < 0.001) at 2 weeks, as VAS score was nearly zero at 6 weeks for arthroscopic capsular release group and remained so until final follow-up. Inter-group analysis of CMS and VAS shown in [Table 5].
DISCUSSION
The most noticeable result of this study was achieving near complete and painless ROM by arthroscopic capsular release in adhesive capsulitis of shoulder secondary to the diabetes in Indian population. The results of arthroscopic release are superior to conservative management as shown by analysis of VAS, CMS, and ROM serially at different time of follow-up, in evenly matched group without confounding factors.
There was complete and consistent pain relief in arthroscopic release group by as early as 6 weeks and it persisted till last follow-up, whereas residual pain persisted in the conservative group. The reported persistent pain relief after arthroscopic release in this study is consistent with that in the literature.[22-24]
Ebrahimzadeh et al.[25] reported maximum pain relief around 3.6 ± 2.1 months after arthroscopic capsular release (37% of the cases were diabetic). One of the factors that could contribute to early pain relief in this study was subacromial decompression, which was performed in addition to capsular release in all cases. Subacromial decompression as an adjunct to capsular release is mentioned sparingly in the literature.[17-19] Early pain relief is of paramount importance so as to push the patients too early and aggressive post-operative rehabilitation. Addition of subacromial decompression to arthroscopic capsular release for pain relief needs to be analyzed further in a randomized control trial (RCT) trial in future.
In this study, there was residual pain and motion deficit at the final follow-up of 2 years in conservative group. Similar observation regarding residual pain and deficient motion has been reported in the literature.[26,27] Shaffer et al.[28] reported remnant motion deficit rate of 60% at a mean follow-up of 7 years. The improvement in VAS in conservative group of this study is comparable to previously reported study,[29] but it could not match that of arthroscopic release group.
In this study, there was significant improvement in the ROM of forward flexion, abduction, external rotation, and internal rotation in arthroscopic release group when compared with conservative group. All patients of arthroscopic release group could attain full ROM whereas none of the case of conservative group could achieve full ROM by the end of the study. The improvement of ROM after arthroscopic release is consistent with the previous studies.[22-25]
Time for improvement in ROM reported by Ebrahimzadeh et al.[25] was 3.6 ± 2 months. The lesser time taken to achieve full ROM in this study could be attributed to rigorous post-operative pain relief coupled with aggressive rehabilitation.
It is well-established that because of inflammation of capsule in adhesive capsulitis there is fibroblast and myofibroblast proliferation leading to abundant Type 3 collagen deposition and thick fibrous tissue formation. Coracohumeral ligament (CHL) and Superior glenohumeral ligament (SGHL) are essentially involved and it causes restriction of ER that is last to be regained. Complete arthroscopic release of rotator interval (SGHL and CHL) is essential to regain ER as in this study. All the patients of this study had undergone complete release of capsule leaving behind only superior capsule because that part of capsule is always in full length when arm is by side.
Though UK Frost study documented no difference in outcome between conservative and operative group, in this study, it was noticed that there was early pain relief and recovery of ROM in arthroscopic release group and this improvement was sustained till the last follow-up, whereas conservative group patients had remnant pain and limitation of movement. Early pain relief and regaining of ROM have significant effect on quality of life[30] proving superiority of arthroscopic release.
The superiority of arthroscopic release over conservative management is also depicted by the functional outcome in terms of CMS, which was significantly better at each follow-up. Similar results are reported in the literature.[24,25] Because of improved pain relief after arthroscopic release, these patients were noticed to regain strength faster, were more comfortable with aggressive rehabilitation, and had sustained relief.
Limitations
The limitations of this study were small sample size and non-randomized allocation into groups.
CONCLUSION
Arthroscopic capsular release provides earlier and lasting pain relief with near complete recovery of ROM, consistent across all patients. The clinical outcome is superior to conservative management.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg. 2011;19:536-42.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1:180-9.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and prognostic factors for postoperative frozen shoulder after shoulder surgery: A prospective cohort study. Arch Orthop Trauma Surg. 2017;137:293-301.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with pain, disability and quality of life in patients suffering from frozen shoulder. Arch Bone Jt Surg. 2016;4:243-7.
- [Google Scholar]
- Current review of adhesive capsulitis. J Shoulder Elbow Surg. 2011;20:502-14.
- [CrossRef] [PubMed] [Google Scholar]
- Adhesive capsulitis of the shoulder and diabetes: A meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016;6:26-34.
- [CrossRef] [PubMed] [Google Scholar]
- A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. J Shoulder Elbow Surg. 2014;23:500-7.
- [CrossRef] [PubMed] [Google Scholar]
- Gentle thawing of the frozen shoulder: A prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two years. J Shoulder Elbow Surg. 2004;13:499-502.
- [CrossRef] [PubMed] [Google Scholar]
- Glenohumeral corticosteroid injections in adhesive capsulitis: A systematic search and review. PM R. 2014;6:1143-56.
- [CrossRef] [PubMed] [Google Scholar]
- Nonoperative management of adhesive capsulitis of the shoulder: Oral cortisone application versus intra-articular cortisone injections. J Shoulder Elbow Surg. 2010;19:172-9.
- [CrossRef] [PubMed] [Google Scholar]
- Manipulation under anaesthesia for the treatment of frozen shoulder. Int Orthop. 2003;27:107-9.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized controlled trial of arthroscopic capsular release versus hydrodilatation in the treatment of primary frozen shoulder. J Shoulder Elbow Surg. 2018;27:1401-6.
- [CrossRef] [PubMed] [Google Scholar]
- Recalcitrant chronic adhesive capsulitis of the shoulder. J Bone Joint Surg Am. 1989;71A:1511-5.
- [CrossRef] [Google Scholar]
- Open surgical release for frozen shoulder: Surgical findings and results of the release. J Shoulder Elbow Surg. 2001;10:353-7.
- [CrossRef] [PubMed] [Google Scholar]
- Disorders of the Shoulder: Diagnosis and Management (2nd ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2007.
- [Google Scholar]
- Glenoid fracture during manipulation under anesthesia for adhesive capsulitis: A case report. J Shoulder Elbow Surg. 2011;20:e23-6.
- [CrossRef] [PubMed] [Google Scholar]
- 360 degree arthroscopic capsular release in patients with adhesive capsulitis of the glenohumeral joint indication, surgical technique, results. Knee Surg Sports Traumatol Arthrosc. 2001;9:178-86.
- [CrossRef] [PubMed] [Google Scholar]
- An arthroscopic technique for treating patients with frozen shoulder. Arthroscopy. 1999;15:2-11.
- [CrossRef] [PubMed] [Google Scholar]
- Is the extended release of the inferior glenohumeral ligament necessary for frozen shoulder? Arthroscopy. 2010;26:529-35.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of adhesive capsulitis of the shoulder: A critical analysis review. JBJS Rev. 2018;6:e5.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Orthopaedic Rehabilitation: An Evidence-based Approach (4th ed). Amsterdam, Netherlands: Elsevier; 2017. p. :402-48.
- [Google Scholar]
- Long-term outcomes after arthroscopic capsular release for idiopathic adhesive capsulitis. J Bone Joint Surg Am. 2012;94:1208-16.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic release of adhesive capsulitis. J Shoulder Elbow Surg. 2004;13:180-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of shoulder stiffness. Clin Orthop Relat Res. 2001;390:119-28.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes after arthroscopic release for recalcitrant frozen shoulder. Arch Bone Jt Surg. 2014;2:220-4.
- [Google Scholar]
- Predictors of outcome after nonoperative and operative treatment of adhesive capsulitis. Am J Sports Med. 2011;39:567-74.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. J Bone Joint Surg Am. 2000;82:1398-407.
- [CrossRef] [PubMed] [Google Scholar]
- Frozen shoulder: A long-term follow up. J Bone Joint Surg Am. 1992;74:738-46.
- [CrossRef] [PubMed] [Google Scholar]
- Manual therapy is an effective treatment for frozen shoulder in diabetics: An observational study. Eklem Hastalik Cerrahisi. 2012;23:94-9.
- [Google Scholar]
- Management of adults with primary frozen shoulder in secondary care (UK FROST): A multicentre, pragmatic, three-arm, superiority randomised clinical trial. Lancet. 2020;396:977-89.
- [CrossRef] [Google Scholar]






