Translate this page into:
Chronic lateral ankle instability: Results of two-staged approach, correlation with magnetic resonance imaging findings, and incidence of associated pathologies – A 4-year follow-up study

-
Received: ,
Accepted: ,
How to cite this article: Dalal S, Morgan G. Chronic lateral ankle instability: Results of two-staged approach, correlation with magnetic resonance imaging findings, and incidence of associated pathologies – A 4-year follow- up study. J Arthrosc Surg Sport Med 2020;1(2):178-85.
Abstract
Objectives:
About 20% of ankle sprains have persistent symptoms even after 6 weeks–3 months of conservative treatment of physiotherapy and bracing. We followed a two-staged operative treatment protocol for the management of patients with persistent chronic lateral ankle instability. This study aims to analyze the outcomes of this two-staged treatment protocol and also to compare the magnetic resonance imaging (MRI) and arthroscopic findings in such patients and note the presence of associated pathologies.
Materials and Methods:
This is a retrospective study of 87 patients operated for chronic lateral ankle instability in two stages: (1) Diagnostic examination under anesthesia and ankle arthroscopy and (2) modified Brostrom procedure.
Results:
With a mean follow-up of 4 years, 31% of the patients had a complete resolution of their symptoms 4 months after the first procedure. Mean American Orthopaedic Foot and Ankle Score (AOFAS) and visual analog scale (VAS) scores show a significant improvement in functional outcomes in both the groups (P < 0.05). Moreover, the MRI findings were equivocal or false negative in 60% of the patients. We also observed associated pathologies such as synovitis, osteochondral defect of talus, and anterolateral impingement in 40% of the patients.
Conclusion:
The two-staged treatment of ankle arthroscopy and modified Brostrom procedure is highly effective in resolution of the symptoms of patients with chronic lateral ankle instability. As MRI is not very sensitive and because of the associated intra-articular lesions found in this spectrum of patients, a primary ankle arthroscopy followed by a staged Brostrom procedure has shown to improve outcomes significantly with optimal intervention.
Keywords
Chronic ankle instability
Ankle arthroscopy
Brostrom level of evidence-IV
INTRODUCTION
Ankle sprains, constituting 3–5% of A&E visits, are common injuries seen in the young, athletic population with a majority involving the lateral ligamentous complex.[1] Plenty of literature has been written about the operative and non-operative treatment of symptomatic lateral ankle sprains and the sequelae of chronic instability of the ankle.[2,3,4,5,6,7,8] Approximately 20% of patients suffering from lateral ankle sprains, will have chronic symptomatic ankle instability.[2,3,4,5,6,7,8,9] The management of chronic ankle instability (CAI) in patients who have failed a course of aggressive and supervised physical therapy poses a challenge to the orthopedic surgeon. Although magnetic resonance imaging (MRI) has a high specificity and positive predictive value for establishing the diagnosis of anterior talofibular ligament (ATFL) and calcaneal fibular ligament (CFL) lesions and can be used for the assessment of associated pathology, the sensitivity of MRI is low and in a symptomatic patient with normal ligaments on MRI, arthroscopy may be required for a definitive diagnosis.[3,5,10,11]
Moreover, in patients with CAI, there is a cohort of patients with associated intra-articular pathology which may cause persistent symptoms despite a satisfactory and stable reconstruction.[4,12,13,14] Common intra-articular findings are synovitis, loose bodies, anterolateral impingement, osteochondral lesions of the talus, adhesions, and osteophytes.[13,14] A thorough arthroscopic evaluation and treatment of intra-articular pathology before ligament surgery is recommended by several authors.[13,14,15]
Many different techniques, anatomical or non-anatomical, have been described in the operative treatment for chronic lateral ankle instability.[7,8,16,17] This manuscript describes a variant to the modified Brostrom’s repair using two suture anchors for anatomical reconstruction of both the ATFL and CFL, along with advancing the extensor retinaculum to reinforce the repair.[18,19,20]
With this background of low sensitivity of MRI for diagnosing CAI and the need for arthroscopy for definitive diagnosis and management of associated pathologies, we followed a two-staged treatment protocol for the management of patients with chronic lateral ankle instability: (1) Examination under anesthesia and ankle arthroscopy and (2) modified Brostrom repair. The primary aim of this study is to analyze the functional outcomes of this two-staged treatment protocol and the secondary aims are to compare the MRI and arthroscopic findings in patients with CAI and to note the presence of associated pathologies.
MATERIALS AND METHODS
Management protocol
The management protocol for ankle sprains in our institute is as shown in the [Flowchart 1].
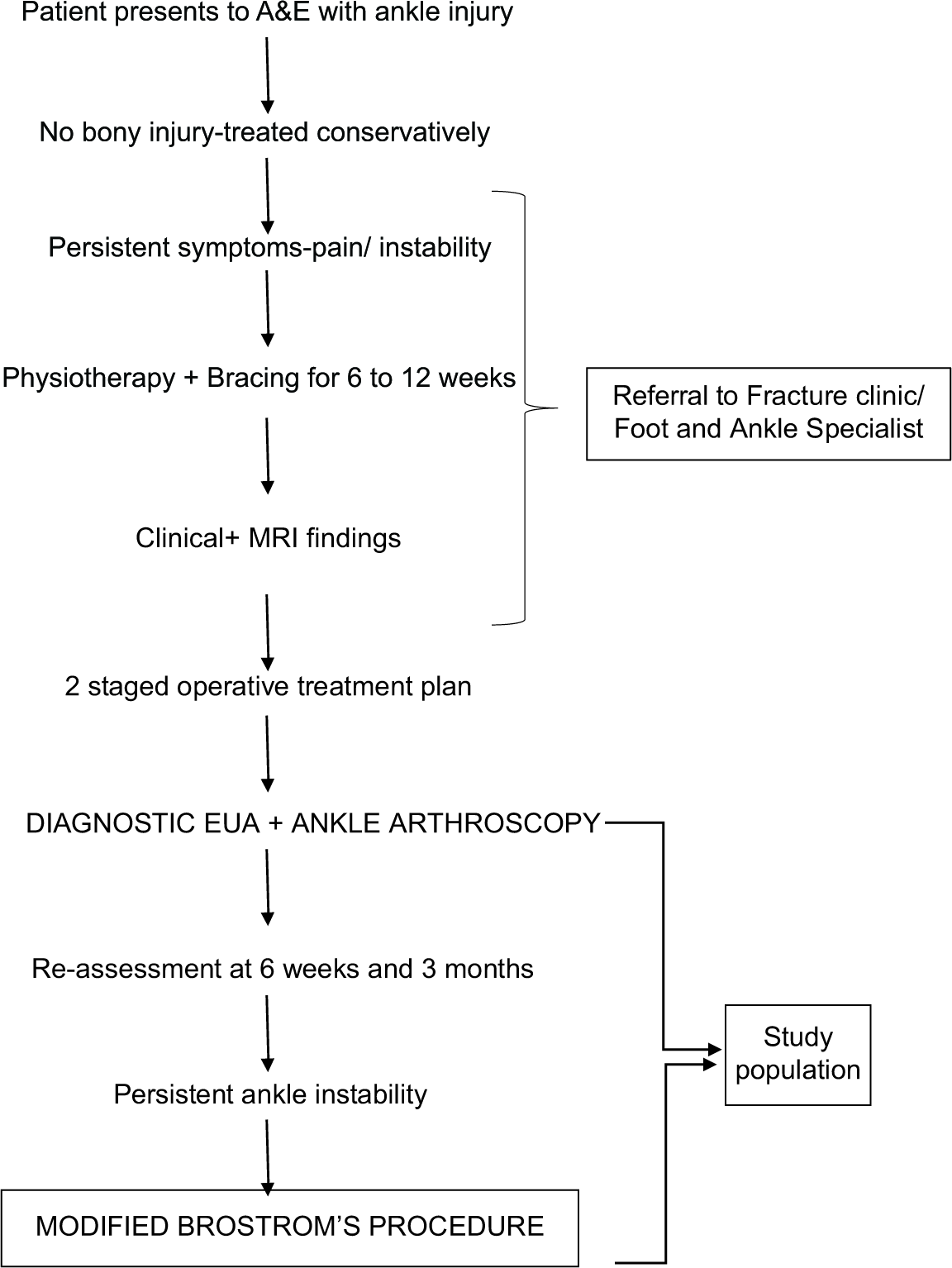
- Showing management protocol of patient presenting with ankle sprain.
Patients
This is a retrospective case series. All patients who complain of pain and instability of the ankle despite supervised rehabilitation were assessed in our foot and ankle clinic, as shown in the management protocol. The single-staged versus two-staged treatment options were discussed with the patient and an informed decision was then made regarding further treatment plan. Advantages of this two-staged approach are that a small proportion of patients may have a relief of their symptoms after a primary ankle arthroscopy and treatment of associated conditions, without the need for a definitive Brostrom procedure, which needs extensive rehabilitation and post-operative care for 3–6 months. Further, the quality of tissue dissection and the reliability of repair is also debatable.[13,21] Disadvantages include the need for two separate surgeries (and hence its anesthetic and operative morbidities) if the patient is persistently symptomatic. Further discussion has been in the discussion section. Ninety-one consecutive patients who were identified with symptoms of persistent chronic ankle stability and equivocal or positive clinical and radiological findings underwent the two-staged operative treatment protocol as shown above, after informed consent. Two patients’ detailed clinical records were not found and two patients’ were lost to follow-up, leaving a total of 87 patients (41 females and 46 males) who were finalized for our study for further analysis. The patient demographics are shown in [Table 1]. Our patient inclusion criteria for this two-staged treatment protocol were patients having symptoms of pain and/or instability refractory to at least 6 weeks course of formal physical therapy, who have consented for this two-staged treatment approach. MRI was requested on every patient to evaluate for intra-articular pathology and condition of the ATFL and CFL ligaments. There is no control group and all the 91 consecutive patients were included in the study to avoid any bias.
| Characteristic | Value |
|---|---|
| Patients (n) | 87 |
| Female patients (%) | 41 (47%) |
| Male patients (%) | 46 (53) |
| Mean follow-up, years (range) | 4 (1.2–6.5) |
| Mean age, years (range) | 40 (20–63) |
| Mean interval from injury to 1st surgery, months (range) | 3 (2.1–8) |
Intervention
Enhanced recovery after surgery protocol was used for all surgeries.[22] All patients received a single intravenous dose of cefuroxime 1.5 g at the time of induction. Thigh tourniquet was used.
Stage 1
All patients underwent a diagnostic examination under anesthesia with anterior drawer test and talar tilt test. Varus and valgus stress views of the ankle were taken under fluoroscopy control. This was followed by a diagnostic ankle arthroscopy with anteromedial and anterolateral portals to confirm the presence of lateral ligament insufficiency and other associated pathologies. Any associated intra-articular pathology which can be treated arthroscopically was dealt with at this stage. Additional procedures including synovial debridement, excision of anterolateral impingement body, and microfracture were undertaken. We did not address the reconstruction of torn ligaments (if any) at this stage. Patients were allowed full weight-bearing mobilization immediate postoperatively and followed up in clinic at 2 weeks, 6 weeks, and 3 months from the time of surgery to monitor the symptoms and instability.
Stage 2
This stage is only undertaken if: (1) EUA and arthroscopic findings confirm the presence of lateral ligament insufficiency and (2) the patient is persistently symptomatic after 6 weeks or if there is no improvement in symptoms at the end of 3 months. The patient undergoes a variant of the modified Brostrom’s procedure using two suture anchors.[20]
A 5 cm slightly curved incision was made over the lateral malleoli. The edge of the inferior extensor retinaculum was identified and dissected. The capsule and remnants of ATFL and CFL were then identified, with inferior retraction of peroneal tendons. Next, the tip of the fibula at the ATFL and CFL footprint was curetted to provide a bleeding bony bed for healing. Drill holes were then made at the ATFL and CFL footprint insertion site. A suture anchor was placed at the anatomic footprint of each, the ATFL and CFL, respectively, in the distal fibula (Zimmer-Biomet JuggerKnot 1.4 mm suture anchor system). Care was taken to make sure that the drill hole tunnels did not intersect each other.
Following that, the ATFL and CFL remnants, along with the capsular-periosteal flap, were tied down to the two suture anchors with the foot at neutral dorsiflexion and slight eversion. The extensor retinaculum was advanced and repaired using 1–0 Vicryl, to the distal fibular periosteum to reinforce the repair (with the foot in neutral dorsiflexion and slight eversion. Finally, the skin was closed subcutaneously using 2–0 Vicryl sutures followed by 3–0 nylon interrupted stitches. Wound was dressed with jelonet, inadine, and sterile gauze. A below-knee backslab was given at the end of the surgery in neutral position.
Post-operative protocol
Postoperatively, all patients were placed in a well-padded below-knee backslab with the foot in neutral and kept non-weight-bearing on the affected side until their follow-up visit after 14 days. At the first post-operative follow-up visit, ankle incision was inspected and the stitches were removed. The patients were then placed in a short-leg walking cast for the next 6 weeks. Protected and progressive weight-bearing was allowed over the following 6 weeks using crutches. During weeks 8–12, patients were then placed in a TriLok Ankle Brace (BioSkin, Medford, USA) and started on gentle active assisted range of motion of the ankle. Proprioception and strength training were also started during the 8–12 weeks interval under supervised physiotherapy with further progression to plyometrics. Patients were allowed to return to sports or normal activities without any limitations after week 16.
Outcomes
Operative and clinical records were reviewed for the progress and follow-up. MRI findings were compared with EUA and arthroscopic findings. Associated pathologies found during ankle arthroscopy were noted. Clinical and functional progress for all patients was noted at the time of pre- assessment and postoperatively at 6 weeks, 3 months, and 6 months. Hamilton, VAS, and AOFAS scores were used to evaluate the functional outcomes preoperatively and at final follow-up.[23] Immediate or late complications, any operative interventions, and revision surgeries were identified by a thorough review of the clinical records.
Statistical analysis
All statistical analyses were performed using IBM SPSS Software version 17 and by a blinded author. For all variables including age and follow-up, descriptive statistics with mean, range, and standard deviation were reported. Chi-square test and t-test were used to calculate P-values for difference in outcome scores. P = 0.05 was considered statistically significant.
RESULTS
The number of patients in the two-staged operative treatment plan and the comparison with associated lesions are shown in [Figure 1]. All patients (n = 87) had lateral instability confirmed during EUA and arthroscopy (1st stage). Twenty- seven of the 87 patients operated for CAI had a resolution of their symptoms and returned to normal activities 4 months after the first procedure, without any symptoms of pain or instability or the “ankle giving away” or “rolling over.” Fourteen patients out of the 27 (52%) had associated pathologies which were primarily managed at the time of ankle arthroscopy.

- Graph showing results of two-staged operative treatment and comparison with associated lesions.
Rest of the 60 patients had to undergo the second surgery (i.e., modified Brostrom’s procedure) for persistence of symptoms. Twenty-one out of the 60 patients (35%) had associated intra-articular pathologies which were managed in the first stage. However, the instability symptoms continued to persist after that, which necessitated the second procedure. Fifty-six out of 60 patients returned to their baseline activities 4 months after the second procedure. The details of the associated pathologies are shown in [Table 2] (note that some patients had multiple associated pathologies).
| Patient subgroup | Associated pathologies | Number of patients |
|---|---|---|
| Ankle arthroscopy | Synovitis | 13 |
| OCD | 3 | |
| Anterolateral impingement | 6 | |
| Loose body | 2 | |
| Arthrofibrosis | 5 | |
| Early arthritis | 1 | |
| Modified Brostrom procedure | Synovitis | 17 |
| OCD | 5 | |
| Anterolateral impingement | 9 | |
| Loose body | 3 | |
| Arthrofibrosis | 8 | |
| Early arthritis | 2 |
Functional outcomes
The Hamilton functional outcomes at the final follow-up are shown in [Table 3]. Only three patients in Brostrom group had fair outcomes (symptomatic, not fully functioning), whereas one patient had poor outcome (worse than before surgery). Rest of the patients had either excellent (asymptomatic, full activities) or good outcomes (some symptoms, full activities) at final follow-up. There is no significant difference between the outcomes of two groups (P = 0.46).
| Excellent (%) | Good (%) | Fair (%) | Poor (%) | |
|---|---|---|---|---|
| Ankle arthroscopy | 63 | 37 | 0 | 0 |
| Brostrom procedure | 55 | 40 | 3 | 1 |
The pre-operative and final follow-up mean AOFAS and VAS scores of both the groups are shown in [Figure 2]. Paired test performed on both groups shows a significant improvement in the post-operative outcomes (P < 0.05). However, there is no difference in the outcomes between arthroscopy and Brostrom group (P = 0.1).
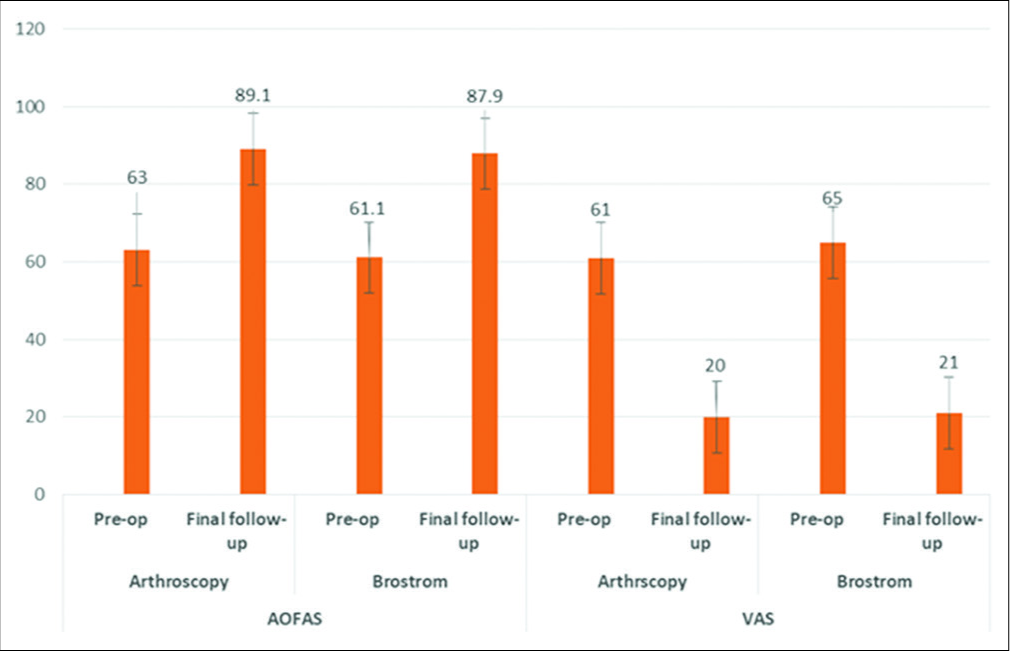
- Graph showing comparison of mean American Orthopaedic Foot and Ankle Score and visual analog scale scores – pre-operative and at final follow-up for both groups.
The overall complications are shown in [Figure 3]. Three patients had superficial nerve paresthesia postoperatively which resolved spontaneously. One patient was on long- term warfarin, developed SPN paresthesia and hematoma in the ankle joint post-ankle arthroscopy, which needed open incision and drainage. Two patients developed scar hypersensitivity which was treated conservatively using deep sensitization techniques. Four patients had a revision Brostrom’s procedure with augmentation of the repair using a suture tape and interference screw construct called an Internal Brace™ (Arthrex, Naples, FL),[24] 3 of whom had a history of retrauma. One patient, who has hyper laxity, had persistent problems after the primary Brostrom’s procedure following which she had a revision surgery using an internal brace to augment the construct.
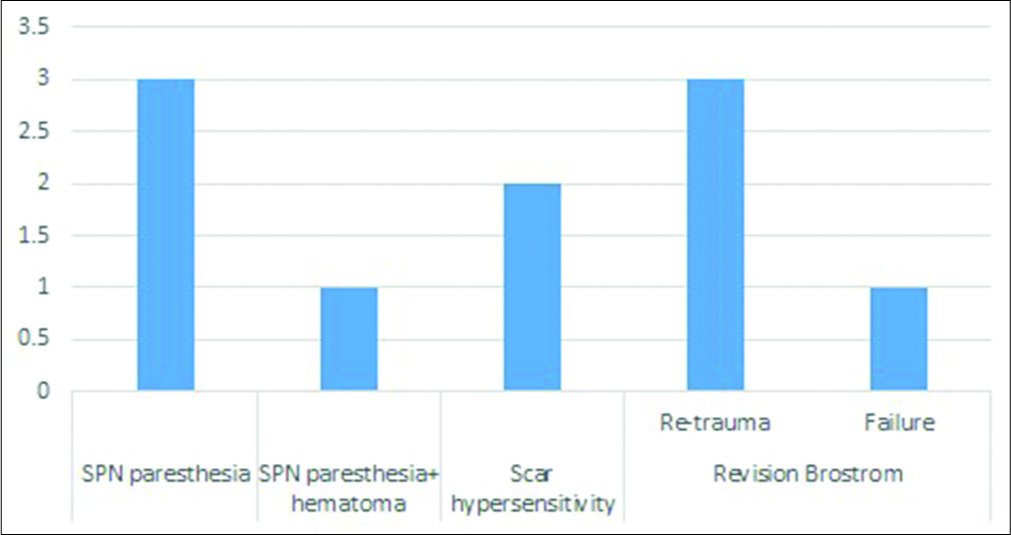
- Post-operative complications.
Comparing the MRI with arthroscopic and EUA findings of the entire study population, for all the patients (n = 87) having lateral instability confirmed under EUA and arthroscopy,[25] the MRI findings are shown in [Figure 4]. Fifty-three out of 87 patients (60%) had equivocal or false-negative MRI findings. All MRIs were reported by a consultant musculoskeletal radiologist in our institute. Out of the 53 patients, 34 went on to undergo the second-staged surgery. In 33 patients who have been classified on the basis of MRI as having an intact ATFL, it was reported as the ATFL as thickened, irregular, ill-defined, attenuated, thin, or having a strain injury, but “intact.”

- Graph showing number of patients having magnetic resonance imaging findings as shown blue and the number of patients who needed to undergo Brostrom procedure (orange).
DISCUSSION
Evidence from peer-reviewed literature suggests that the characteristics of patients developing persistent chronic lateral ankle instability are not homogeneous. There are a number of anatomical factors and pathological conditions which can contribute to the etiology of CAI. A good knowledge of these characteristics will help in improving the decision-making for the treatment.
In our study, we found associated intra-articular pathological lesions in 35/87 patients (40%). This is similar to other studies who have noted that 20–40% of patients with chronic instability have associated disorders.[13,15] Moreover, 52% of the patients who had a relief of their symptoms after the first surgery had associated intra-articular pathology, thus indicating the possible cause of their symptoms.
In the ankle affected by chronic instability, synovitis is a common finding as it represents the reaction to an injury of the lateral ligament complex.[26] In our case series, synovitis was detected and treated in 30/87 patients (34%), demonstrating a strong association between instability and synovial hypertrophy. Apart from treating synovitis itself, arthroscopic debridement permits better visualization and allows treatment of the underlying factors responsible for causing synovitis (soft-tissue injuries and osseous pathology or degenerative arthritis).[15] Among the lateral ankle ligaments, the ATFL is easily accessible during arthroscopy as it is continuous with the joint capsule.[27] The debridement of the borders of the torn ligament and the adjacent area stimulates the healing process with fibrous tissue formation from the surrounding capsule. In the study done by Ventura et al., they evaluated the results of the four step arthroscopic treatment of 90 patients for CAI.[28] About 96.6% rated the success of the surgery as good to excellent, in spite of the ligament tear being not addressed in the form of repair. In our study, 31% (27/87) of the patients who had undergone the first surgery had a complete relief of their symptoms and were able to return to their baseline activities.
We also observed that MRI findings in diagnosing lateral ligament injuries showed false-negative or equivocal findings in 60% of the cases. In the study done by Park et al., the MRI findings of ATFL injury showed a sensitivity of 75%, 75%, and 44% for complete tears, partial tears, and sprains, respectively.[10] The MRI findings of CFL injury showed a sensitivity of 50%, 83%, and 100% for complete tears, partial tears, and sprains, respectively. The study done by Desmond et al. shows ATFL sensitivity of 64–78% and specificity of 80–86%, whereas CFL sensitivity was 45–71% with specificity of 89–97%, and these values support the results of Park et al., that is, lower sensitivity but higher specificity for lesions in the ATFL and the CFL.[10,29] Cao et al., in a systemic review of 15 studies, observed that the pooled sensitivity and specificity of MRI in diagnosing ATFL injury was 0.83 and 0.79, whereas that for CFL injury was 0.56 and 0.88.[30] In our study, 34/53 patients who had false-negative or equivocal report of the MRI scans had to undergo the second procedure, indicating that EUA and arthroscopic assessment must be done for a definite diagnosis, if the patient is persistently symptomatic and the MRI is equivocal.
This modification to the original Brostrom’s technique has better versatility of utilizing suture anchors and more reliable repair of the ATFL and CFL. Moreover, the suture anchor placement at the footprints of the lateral ligaments allows addressing each of the ligaments individually, to repair them anatomically. Important points to remember during surgery include (1) meticulous elevation of the retinaculum and capsule so that there is adequate length for advancement and repair, (2) attention not to incorporate the peroneal tendon into the repair, while repairing the CFL, and (3) the most essential component of this procedure is to fix the reconstruction with the patient’s foot in neutral and slight eversion which will tighten up the lateral instability. This technique, which was utilized by the authors in our series of patients with chronic lateral ankle instability, was able to return 95% of the patients to their previous activity level. The major complication rate included a 3.5% rerupture rate (3/87 patients) past the 1 year post-operative period due to traumatic injuries. However, it must be noted that this technique has already been described in literature previously by Li et al.[20]
The rationale for formulating a two-staged treatment plan was that: (1) Soft-tissue dissection, identification of fascial planes and ligaments separately is difficult due to fluid extravasation post ankle arthroscopy.[13] (2) The quality of repair is not predictable because of the fluid accumulation and swelling in the soft tissues of the ankle.[22] The authors believe that once the associated intra-articular pathologies are managed during the initial arthroscopy and the swelling settles down, the patient should be reassessed again to check for lateral instability and if still symptomatic, should proceed to the definitive procedure in the form of anatomical repair. It would not be wrong to argue that excellent results have been achieved with single-staged arthroscopy with lateral ligament repair, and it would be an unnecessary waste of time and resources to delay the definitive procedure if needed.[31,32] However, it must be noted that 27 patients (31%) in our patient population did not need that definitive procedure, in spite of confirmed lateral instability in the first stage. Hence, the associated morbidities and the longer rehabilitation of the definitive procedure were also avoided. Moreover, the clinical and functional outcome scores are similar at final follow-up. A cost-benefit analysis would be ideal to analyze the outcomes but that is beyond the scope of this study. However, the message is this two-staged treatment plan should be discussed with the patients with the advantages and disadvantages and further decisions should be taken accordingly.
This study has the following limitations: (1) We have not compared out results with any control group who have been managed with a single-staged approach. (2) EUA and arthroscopic assessment of instability were not classified into different grades. Retrospectively, the authors believe that development and correlation of such grading with their clinical scores and follow-up can help in predicting the outcomes in a better way. (3) Moreover, not all etiological aspects are yet defined and it is still not clear as to why 13 out of the 27 patients who did not have any notable intra-articular pathology had a relief of their symptoms. There is a paucity of literature explaining the cause and target approach for such patient symptoms. A well-known pathological condition is the patient with persisting complaints of functional instability associated with pain, but without any objective characteristics. This may be explained by formation of scar tissue and arthroscopic approach may be useful to assess the ankle joint in these situations.[33]
CONCLUSION
The two-staged approach of ankle arthroscopy and the modified Brostrom technique is safe and effective in treating patients with CAI. As MRI is not very sensitive and because of the associated intra-articular lesions found in this spectrum of patients, this two-staged approach has shown to improve functional outcomes with optimal intervention.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11:659-62.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int. 1994;15:72-4.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral instability of the ankle treated by the Evans procedure. A long-term clinical and radiological follow-up. J Bone Joint Surg Br. 1988;70:476-80.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988;70:581-8.
- [CrossRef] [PubMed] [Google Scholar]
- Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12:129-35.
- [CrossRef] [PubMed] [Google Scholar]
- Operative and functional treatment of rupture of the lateral ligament of the ankle. A randomised, prospective trial. J Bone Joint Surg Br. 2003;85:525-30.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am. 1985;67:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- The long-term results of Watson-Jones tenodesis. J Bone Joint Surg Br. 1984;66:371-5.
- [CrossRef] [Google Scholar]
- Surgical treatment of the unstable ankle. J Am Acad Orthop Surg. 1998;6:368-77.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of MRI findings in chronic lateral ankle ligament injury: Comparison with surgical findings. Clin Radiol. 2012;67:313-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic and magnetic resonance image appearance and reconstruction of the anterior talofibular ligament in cases of apparent functional ankle instability. Am J Sports Med. 2008;36:1542-7.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic lateral ankle instability: The effect of intra-articular lesions on clinical outcome. Am J Sports Med. 2008;36:2167-72.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic lateral instability: Arthroscopic findings and long-term results. Foot Ankle Int. 2007;28:24-31.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of lateral ankle instability syndrome. Am J Sports Med. 1988;16:501-11.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30:402-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of modified Brostrom and Evans procedures in simulated lateral ankle injury. Med Sci Sports Exerc. 2006;38:1025-31.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction for lateral instability of the ankle. J Bone Joint Surg. 1984;66:336-9.
- [CrossRef] [Google Scholar]
- Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551-65.
- [Google Scholar]
- Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1:84-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: Functional outcomes after the modified brostrom repair using suture anchors. Am J Sports Med. 2009;37:488-94.
- [CrossRef] [PubMed] [Google Scholar]
- Technique tip: Limiting fluid extravasation into soft tissues during ankle arthroscopy before lateral ankle ligamentous reconstruction. Foot Ankle Int. 2007;28:739-41.
- [CrossRef] [PubMed] [Google Scholar]
- Enhanced recovery after surgery for primary hip and knee arthroplasty: A review of the evidence. Br J Anaesth. 2016;117:62-72.
- [CrossRef] [PubMed] [Google Scholar]
- The addition of an “internal brace” to augment the Broström technique for lateral ankle ligament instability. Tech Foot Ankle Surg. 2016;15:47-56.
- [CrossRef] [Google Scholar]
- Accuracy of plain radiographs versus 3D analysis of ankle stress test. Foot Ankle Int. 2011;32:994-9.
- [CrossRef] [PubMed] [Google Scholar]
- Soft-tissue disorders of the ankle: A comprehensive arthroscopic approach. Clin Podiatr Med Surg. 2002;19:271-83.
- [CrossRef] [Google Scholar]
- Anatomy of lateral ankle ligaments and their relationship to bony landmarks. Surg Radiol Anat. 2006;28:391-7.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic four-step treatment for chronic ankle instability. Foot Ankle Int. 2012;33:29-36.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of magnetic resonance findings, and incidence of associated pathologies-A 4-year follow-up study imaging in diagnosing lateral ankle ligament injuries: A comparative study with surgical findings and timings of scans. Asia Pac J Sports Med Arthrosc Rehabil. 2016;7:15-20.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging diagnosis for chronic lateral ankle ligament injury: A systemic review with meta-analysis. J Orthop Surg Res. 2018;13:122.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Int. 2015;5:213-7.
- [Google Scholar]
- Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: A systematic review. Foot Ankle Surg. 2018;24:11-8.
- [CrossRef] [PubMed] [Google Scholar]
- The role of arthroscopy in the treatment of functional instability of the ankle. Foot Ankle Surg. 2013;19:273-5.
- [CrossRef] [PubMed] [Google Scholar]






