Translate this page into:
Clinicoradiological evaluation of modified posterior shoulder stretching and rehabilitation exercises versus rehabilitation exercises alone in the management of subacromial impingement syndrome
*Corresponding author: Shwetasri Mohanta, Department of Sports Medicine, Sports Injury Centre, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. shwetasri.mdsem@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mohanta S, Lal H, Kumar J, Vakharia K, Srivastava A. Clinicoradiological evaluation of modified posterior shoulder stretching and rehabilitation exercises versus rehabilitation exercises alone in the management of subacromial impingement syndrome. J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_11_2025
Abstract
Objectives:
The objectives of the study are to assess and evaluate the clinicoradiological outcomes of the addition of modified posterior shoulder stretching exercises (MPSSEs) to the rehabilitation exercises in the management of subacromial impingement syndrome (SAIS).
Materials and Methods:
60 patients were divided into 2 groups: A control group receiving standard rehabilitation and an intervention group receiving standard rehabilitation and MPSSEs. Outcome measures included the Visual Analog Scale (VAS) for pain; Quick disabilities of the arm, shoulder, and hand (QuickDASH) score for functional disability; and Constant-Murley score (CMS) for shoulder function.
Results:
Significant improvement (P <0.005) in VAS, QuickDASH, and CMS scores was found in the MPSSEs group compared to the control group. Furthermore, a greater number of patients in the MPSSEs group returned to their pre-injury sport level.
Conclusion:
This study suggests that MPSSEs are a valuable addition to standard rehabilitation for SAIS, facilitating pain reduction, improved function, injury prevention, and earlier return to sport. Further research with biomechanical and radiological outcomes is recommended.
Keywords
Racquet sports
Return to sports
Shoulder impingement syndrome
Shoulder pain
Sports medicine
INTRODUCTION
Shoulder pain has been reported to rank as the third most common complaint. Its lifetime prevalence is as high as 67%. In Northern India, its prevalence was noted to be 22.9%.[1] Despite such a high prevalence, its treatment outcome is quite unfavorable.[2] This leads to substantial impairment in work performance, causing absence from work, early retirement, or job loss.[3] Sleep disturbances due to Shoulder pain also lead to poor quality of life.[4]
Shoulder impingement syndrome (SIS) is the most frequently reported cause of shoulder pain, the most common type of SIS being subacromial impingement syndrome (SAIS).[5] SAIS is commonly seen in sportspersons engaged in repeated overhead activities such as handball, volleyball, swimming, and badminton. In a survey conducted during the Badminton Sudirman Cup in 2003 (Netherlands), it was found that shoulder pain was a common troublesome problem even for world-class badminton players. Swimmers who do freestyle are reported to have more risk of SAIS due to overuse of their shoulders, which causes microtrauma during the cyclic-overhead motion.[6]
Subacromial impingement of the shoulder is a syndrome in which the soft tissues in the subacromial space become entrapped and cause pain. The patients then present with the chief complaint of pain on raising the arm overhead or sleeping on the affected side.[7] In recent years, the definition of impingement syndrome has changed, and now, it is more accurately considered as a clinical sign[8] which points us toward an entire spectrum of pathology of the subacromial space, including rotator cuff pathologies and subacromial bursitis.[9]
The initial management of choice for SIS without any major structural damage is conservative multimodal treatment, which is for a duration of 3-6 months. The initial goals of rehabilitation are (1) pain relief (including intervention – injection steroid), (2) regaining range of motion (ROM), and (3) promoting scapulothoracic and rotator cuff neuromuscular control.[10] The Jacksin Program for shoulder impingement is a five-step exercise program which is a set of simple exercises given to the patient to perform throughout the day.[7]
Treatment of shoulder pain and subsequent return to sports (RTS) has undergone a paradigm shift with the recent introduction of the following therapies. One of them is Capacitive and Resistive Electric Transfer Therapy.[11] It is a diathermy device using a frequency of 448 kHz imparting effective deep heat for amelioration of shoulder pain.[12] The other one is a modification to the traditional posterior shoulder stretching exercises. These new exercises are (1) modified cross-body stretch and (2) modified sleeper’s stretch. Recent studies have shown that including modified posterior shoulder stretching exercises (MPSSEs) in this rehabilitation program produces significantly better results.[13] In a meta-analysis, it was concluded that in SAIS, there was significant improvement in the shoulder function and pain on doing MPSSEs.[14] In another study, it was observed that there was significant improvement in the shoulder internal rotation and horizontal adduction after four weeks of intervention with MPSSEs.[15]
Eccentric strengthening of the external rotators is also recommended during rehabilitation and injury prevention in overhead athletes.[16]
MATERIALS AND METHODS
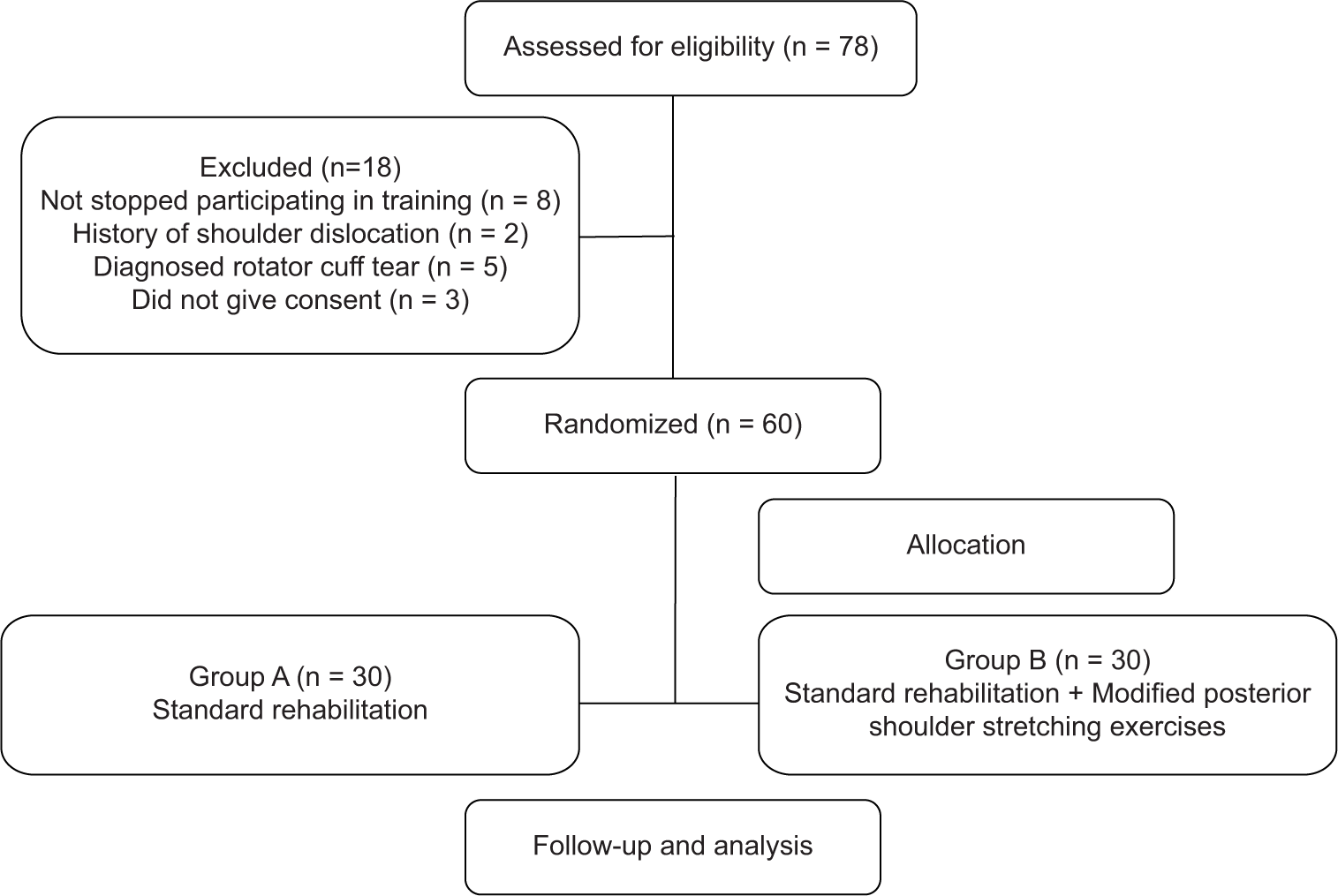
The study was a randomized controlled trial approved by the institutional ethics review board in 2020 [Figure 1]. After a detailed scrutinization, discussion, and assessment of the research project/thesis, the members of the Institutional Protocol Review Committee (IPRC) arrived at a unanimous resolution approving this thesis. Patients with shoulder pain attending the outpatient department were screened by a Sports Medicine resident. Consenting adults within the age group 20 and 55 years, having symptoms consistent with a diagnosis of SIS (more than 3 out of 5 tests positive, that is Neers, Hawkins Kennedy, Jobe’s empty can, painful arc, and external rotation resistance test)[17] and a pain score on the numerical pain rating score (NPRS) of <6 out of 10 were included in the study. Patients with a history of trauma or surgery to the upper limb, full rotator cuff tears, limitation of passive ROM >50% of contra-lateral side in more than 2 planes (suggestive of adhesive capsulitis), other musculoskeletal, or systemic inflammatory diseases affecting uncontrolled diabetes mellitus were excluded from the study. The sample size was estimated based on the work of Tahran and Yeşilyaprak.[13] to find a difference of 15 units and pooled standard deviation (SD) of 13.4, alpha of 95%, and power of 85%. It was estimated to be 14 in each group. Expecting loss to follow-up, 30 patients were included in each group. The randomization was done with a simple randomization method by a nurse not part of the study. As the patients were recruited, she allotted a random number to each patient from 1 to 60. Numbers 1-30 were allocated to Group A (control), and 31-60 (MPSSEs) were allocated to Group B. Both groups received medical (non-steroidal anti-inflammatory drugs) and conventional physical therapy management.[18-20] However, the intervention group was taught a modified version of the traditional posterior capsule stretch, which has been explained in Table 1 (Groups A - Standard Rehabilitation and B - Standard Rehabilitation + Modified Posterior Capsule Stretching Exercises). The session was 30 min long, twice a day. The exercises were instructed by a blinded physical therapist initially. It included exercises as described in Table 2. Outcome measure for objective evaluation of the functioning of the shoulder was done using patient-reported outcome measure questionnaire forms for constant Murley score (CMS) and quick disabilities of the arm, shoulder, and hand (QuickDASH) score on the first and twelfth weeks. Subjective evaluation of pain was done using the Visual Analog Scale (VAS) on the first and twelfth weeks. Radiological evaluation was done using an X-ray (True AP view). In this, the acromiohumeral distance (AHD) was defined as the distance between the undersurface of the acromion and the humeral head. All patients underwent baseline and follow-up measurements of pain using NPRS, function using the CMS, and QuickDASH questionnaire score by a sports medicine physician blinded to group allocation.
- Methodology.
| Traditional posterior shoulder stretching exercises | Modified posterior shoulder stretching exercises | Problem faced by patients |
|---|---|---|
| Sleeper stretch -Position Patient -Side-lying on the throwing side Shoulder -90° abduction, elbow -90° flexed In this position, passive IR is applied to the dominant arm by using the opposite hand. |
MSS - Position Patient -Side-lying position, trunk rolled posteriorly 20°-30° Shoulder -90° abduction Elbow -90° flexion In this position, passive internal rotation is applied at the affected arm using the opposite arm. A towel roll can be placed under the arm (humerus) to better isolate the stretch. |
Traditional stretches -Pain when the shoulder is at 90° due to which patients avoid doing the stretch. It works best with NSAIDs. However, with the modification, the patients were more compliant with the stretch and they avoided taking NSAIDs |
| Cross-body stretch -Position Patient -Standing Using the opposite hand to horizontally adduct the targeted shoulder. |
MCS -Position Patient -Side-lying position, trunk rolled posteriorly 20°-30° Shoulder -90° abduction Elbow -90° flexion Passively adduct shoulder using the opposite arm. |
Traditional method does not provide scapula stabilization, hence accessory abduction occurs at the scapula which prevents the intended stretch to the posterior capsule. |
IR: Internal rotation, NSAIDs: Non-steroidal anti-inflammatory drugs, MSS: Modified sleeper stretch, MCS: Modified cross-body stretch
| Exercise | Dose | Note/Comment |
|---|---|---|
| Warm up -Cycling | 5-10 min | Depending on the environment, humidity, etc. |
| Dynamic stretching -Neck, shoulder, and back mobility exercises | 5-10 slow repetitions per side | It helps in increasing blood flow and prevents injury by giving time to muscles to be well activated |
| Strengthening -Rhomboids, mid and lower trapezius, serratus anterior, rotator cuff, deltoid | Resistance band based or machine weight-based workout (tailored as per patient) | Patients were taught isometrics. After they became pain free, concentric strengthening exercises followed by eccentric strengthening exercises were added. Machine-based workouts were done only 2-3 days/week. |
| Static stretching (SS) -Pectoralis minor, latissimus dorsi, upper trapezius, sleeper stretch, cross body stretch (CBS), biceps and triceps stretch | 30 s hold, 3-5 reps SS, CBS, and their modifications - 30-60 s hold (as tolerable), 5-10 repetitions (as tolerable) |
Group A did traditional posterior capsular stretches Group B did modified posterior shoulder stretching exercises |
| Cool down -Cycling | 5-10 min |
The resistive exercises were calibrated according to subject capability and tolerance. All patients performed exercises for 12 weeks and maintained exercise logs. Once the athletes had returned to participation, they were asked to complete the thrower’s 10 program[21] and pain-free Derby’s shoulder instability program.[22] Return to participation was defined as “The athlete may be participating in rehabilitation, training (modified or unrestricted), or in sport, but at a level lower than his or her RTS goal.”[23] The athletes continued to perform static stretching for the posterior capsule as part of injury prevention, even after complete resolution of glenohumeral internal rotation deficit (GIRD) as part of injury prevention in their training. The dose of the exercises (volume, intensity, frequency) for a patient was tailored after monitoring for morning stiffness post-exercise and pain of more than 2 out of 10 in an NPRS while exercising. The modifications were done in the exercise regimen explained in Table 2. Hence, optimal loading was done in all cases and controls. Exercises were changed based on the improvement of the patient.
The dependent variables were reassessed at the end of the first and twelfth week by the blinded assessor. The pain and function scores were checked for normality. Descriptive data were presented in number, percentage, mean, median, range (min-max) and mean ± SD, variance. The independent t-test was used to compare the means between the two groups. The Chi-square test was used to assess the relationship between two categorical variables. The confidence interval (CI) was considered to be 95%. A P < 0.05 was considered statistically significant. A P < 0.05 was considered significant for all tests.
RESULTS
The demographic details of the included patients are described in Table 3. There were 60 patients out of the 78 who were assessed in the study. Most patients were overhead athletes who had difficulty adhering to their training regimen in view of shoulder pain or those engaged in contact sports. A total of 35 patients were engaged in active sports, and all of them had a GIRD of more than 20° in their affected shoulder during enrollment. Two overhead athletes also had GIRD in both shoulders, while seven had GIRD in their nondominant/left shoulder.
| S No | Variable | Group A Rehabilitation exercises (n=30) |
Group B Rehabilitation exercises+Modified posterior capsule stretching exercises (n=30) |
|---|---|---|---|
| 1 | Mean age | 38 | 37.36 |
| 2 | Gender | 19 males, 11females | 23 males, 7 females |
| 3 | Side involved | 3 both, 19 right, 8 left | 19 right, 11 left |
| 4 | Mean duration of symptoms (months) | 6.76 | 6.75 |
| 5 | Overhead athletes | 15 patients | 12 patients |
| 6 | Contact sports athletes | 4 patients | 4 patients |
The results of the study are described in Table 4. The groups were not different at baseline for any outcome variable. Group B had a significantly lower score at 12 weeks post-intervention as compared to Group A (mean difference [MD] - 1.8; 95% CI- 1.5, 2.1). Group B also had a significantly improved QuickDASH score (MD- 10.3; 95% CI - 6.1, 14.4) and CMS (MD- 10.3; 95% CI - 6.7, 13.8), as mentioned in Table 4.
| S. No. | Outcome variable | Group A | Group B | P-value (1st week) (12th week) | ||||
|---|---|---|---|---|---|---|---|---|
| Standard rehabilitation (n=30) | Standard rehabilitation+Modified posterior capsule stretching exercises (n=30) | |||||||
| Baseline | Post- intervention (1st week) | Post- intervention (12th week) | Baseline | Post- intervention (1st week) | Post- intervention (12th week) | |||
| 1 | Visual Analog Scale | 4.6±0.7 | 4.1±0.5 | 3.3±0.6* | 4.7±0.6 | 3.7±0.5 | 1.4±0.7* | 0.004; 0.000* |
| 2 | Constant-Murley score | 51.7±7.4 | 56.9±7.7 | 61.4±7.5* | 51.4±7.3 | 60.93±6.9 | 71.6±6.1* | 0.039; 0.000* |
| 3 | QuickDASH | 49.7±8.1 | 43.6±8.1 | 36.3±7.4* | 49.5±10.8 | 39.5±9.3 | 26.1±8.7* | 0.073; 0.000* |
| 4 | Acromio-humeral distance (mm) | 6.67±0.959 | - | 6.63±0.890 | 6.80±0.887 | - | 6.83±0.874 | 0.889 (baseline); 0.884 (12thweek) |
In 35 patients who were engaged in active sports, 27 players returned to sports at their respective pre-treatment levels of sports after treatment. Out of the 8 remaining players, 7 were in group A and only 1 in group B.
DISCUSSION
SIS is a common cause of shoulder pain for which specific exercise therapy with emphasis on making posterior soft tissue more flexible and treating GIRD is chosen as the first line of management.
In our study, 45% of patients were overhead athletes. Some boxers also had GIRD in both the shoulders, while some had GIRD in their non-dominant/left shoulder. It was found that the boxers had pain in the dominant shoulder earlier, and to prevent further injury in that shoulder, they changed their dominant arm for punching and now presented with GIRD in their previously non-dominant shoulder as well.
VAS for pain showed a significant difference in the 1st and 12th weeks with the MPSSEs group showing better improvement. This reduction in VAS could be due to the stabilization of the scapula in the modified stretches, which further led to improved compliance in our study.
There was a falling trend in the QuickDASH score in our study; the scores were 36.33 ± 7.392 in the control group (CG) and 26.07 ± 8.686 in the MPSSEs group. There was a significant increase in the CMS score in our MPSSEs group. The mean CMS score in the twelfth week was 61.37 ± 7.453 and 71.60 ± 6.179 for CG and MPSSEs groups, respectively. The MPSSEs reduced the inflexibility of the posterior capsule and decreased the negative biomechanical changes that were causing the symptoms of impingement, thereby improving the symptoms. Further, the MPSSEs can possibly be used for a longer duration to prevent posterior shoulder tightness (PST), GIRD, and impingement. GIRD was corrected in all the athletes in group B in a span of a maximum of 2-3 weeks; however, such was not the case in the control group.
In contrast, the traditional posterior shoulder stretching exercises (PSSEs) required assistance and, therefore were difficult to perform at home individually. We found that modifications by Wilk et al.[24] that were used in our study had an added additional advantage of stabilizing the scapula thereby excluding the need for assistance. These MPSSEs not only provide accelerated relief of pain but also functional improvement and are an indispensable tool for the rehabilitation of SAIS.
AHD, which is normally reduced in patients of SAIS, was found to be 6.67 ± 0.959 and 6.63 ± 0.890 for the CG and MPSSEs group, respectively, at baseline. The normal ADH is between 7 and 14 mm. Post-treatment, the mean AHD after 12 weeks was 6.80 ± 0.887 and 6.83 ± 0.874 for CG and MPSSEs groups, respectively. We found that there was no significant difference between or within the groups. Park et al.[25] demonstrated that there was no relationship or, rather, no linear correlation between AHD and the outcome measures of patients with respect to pain and function. They did not find any improvement in symptoms with an increase in AHD over time. However, dynamic ultrasound could have been a better way to assess this change in AHD instead of plain radiographs, as shown by Maenhout et al.[26] and Yamauchi et al.[27]
We had only one patient in group B who did not improve as he was not compliant with exercises. He was taken up for arthroscopic evaluation/decompression, but per-operatively, there was adequate subacromial space, superior labrum anterior-posterior type I, so a simple washout, debridement of frayed labral end was done, and intra-articular steroid was injected only. Patients returning to sports were significantly more in group B as calculated using the Chi-square test, and the P-value was 0.031785, which is significant (P < 0.05) [Tables 5 and 6]. This shows the effectiveness of MPSSEs in reducing the additional intervention need while not compromising the return to pre-exercise sport level. All patients returned to pre-exercise level sports, and six even returned to competitive sports in the MPSSE group. MPSSEs are associated with an earlier return to performance in sports as compared to the traditional stretches.
| Return to Sports | International level (number of sports patients) | National level (number of sports patients) | State/district level (number of sports patients) | Total (number of sports patients) | ||||
|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | Before | After | |
| Group A | 0 | 0 | 1 | 0 | 18 | 12 | 19 | 12 |
| Group B | 1 | 1 | 3 | 3 | 12 | 11 | 16 | 15 |
| Patients that returned to sport | Patients that did not return to sport | P-value | |
|---|---|---|---|
| Group A | 12 | 7 | |
| Group B | 15 | 1 | |
| Total | 27 | 8 | 0.031785 |
The MPSSEs should be included in the cool-down routine of the athletes for injury prevention. The cool-down program should be performed after every upper body strengthening or plyometric session, and they should be incorporated into the cool-down post-training and competition as well. They should be instructed that the stretches should be done in pain-free range; however, the aim should be to achieve adequate stretch and to hold the stretch for 30-60 s and perform 3-5 repetitions with 1-2 min rest in between each repetition.
The strength of this study is that the exercises were home-based, easy to perform, and did not need assistance. The modifications possibly helped in stabilizing the scapula and, therefore in reducing pain and impingement even in a short duration.
The limitations of this study include a lack of long-term follow-up and a lack of dynamic shoulder ultrasound imaging for the measurement of AHD. The stretches were given as part of treatment; hence, their efficacy as part of the injury prevention program was not assessed. For better quantitative comparison, more studies need to be done with biomechanical and radiological outcomes. A standardized return to performance criteria needs to be devised to better assess the outcomes more objectively.
Further research should be conducted focusing on biomechanical analysis and dynamic radiological measurement of subacromial space while comparing the effectiveness of traditional versus modified PSSEs in patients with SAIS. This is the first study on the effectiveness of MPSSEs as an additional treatment modality for SAIS in India, to the best of our knowledge.
CONCLUSION
The addition of MPSSEs resulted in better clinical outcomes than the standard rehabilitation exercises alone, leading to a decreasing trend of VAS and QuickDASH along with a significantly increasing trend of CMS scores in the MPSSEs group. Patients returning to sports were significantly more in the MPSSEs group. The modified stretches reduce the need for surgery and increase the chances of patients returning to pre-exercise levels of sports, even competitive sports. Hence, these modified stretches should be made an indispensable part of rehabilitation for SAIS.
Acknowledgment:
The authors would like to thank Dr. C. R. Constant (Inventor of CMS) for his permission to use Constant-Murley score as an outcome measure.
Author contributions:
SM: Concepts, design, definition of intellectual content, literature search, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing and review; HL: Concepts, design, definition of intellectual content, manuscript preparation, manuscript editing and review, data acquisition, data analysis; JK: Data acquisition; KV: Data acquisition and statistical analysis; AS: Data acquisition, statistical analysis, and manuscript preparation.
Ethical approval:
The research/study was approved by the Institutional Review Board at Vardhman Mahavir Medical College and Safdarjung Hospital, number 2020-11/CC-305, dated December 10, 2020.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- The painful shoulder: An update on assessment, treatment, and referral. Br J Gen Pract. 2014;64:e593-5.
- [CrossRef] [PubMed] [Google Scholar]
- A prediction rule for shoulder pain related sick leave: A prospective cohort study. BMC Musculoskelet Disord. 2006;7:97.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between shoulder impingement syndrome and sleep quality. Eur Rev Med Pharmacol Sci. 2013;17:370-4.
- [Google Scholar]
- Shoulder disorders in general practice: Incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54:959-64.
- [CrossRef] [PubMed] [Google Scholar]
- Management options for shoulder impingement syndrome in athletes: Insights and future directions. Open Access J Sports Med. 2021;12:43-53.
- [CrossRef] [PubMed] [Google Scholar]
- Impingement syndrome of the shoulder. Deutsch Ärztebl Int. 2017;114:765-76.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder impingement syndrome: From pathology to treatment. SSRN Electronic J [Preprint] 2020 Available from https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3676373
- [CrossRef] [Google Scholar]
- Impingement syndrome: A review of the literature. Austin J Clin Pathol. 2020;7:1067.
- [Google Scholar]
- Impingement syndrome In: Giangarra CE, Manske RC, eds. Clinical orthopedic rehabilitation a team approach (4th ed). Philadelphia, PA: Elsevier; 2018. p. :210-20.
- [CrossRef] [Google Scholar]
- Effects of capacitive and resistive electric transfer therapy in patients with painful shoulder impingement syndrome: A comparative study. J Int Med Res. 2019;48 Available from: http://dx.doi.org/10.1177/0300060519883090
- [CrossRef] [PubMed] [Google Scholar]
- Repressive effects of a capacitive-resistive electric transfer (CRet) hyperthermic apparatus combined with provitamin C on intracellular lipid-droplets formation in adipocytes. Int J Hyperthermia. 2013;29:30-7.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of transfer energy capacitive and resistive on musculoskeletal pain: A systematic review and meta-analysis. Galen Med J. 2022;11:e2407.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of modified posterior shoulder stretching exercises on shoulder mobility, pain, and dysfunction in patients with subacromial impingement syndrome. Sports Health. 2020;12:139-48.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of modified posterior shoulder stretching exercises on shoulder function in subacromial impingement syndrome: A comprehensive meta-analysis. Medicine (Baltimore). 2025;104:e41117.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative analysis of acromiohumeral distances according to the locations of the arms and humeral rotation. J Phys Ther Sci. 2014;26:97-100.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder terminal range eccentric antagonist/concentric agonist strength ratios in overhead athletes. Scand J Med Sci Sports. 2006;16:174-80.
- [CrossRef] [PubMed] [Google Scholar]
- Screening the athlete's shoulder for impingement symptoms: A clinical reasoning algorithm for early detection of shoulder pathology. Br J Sports Med. 2008;42:628-35.
- [CrossRef] [PubMed] [Google Scholar]
- Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: An evidence-based review. Br J Sports Med. 2010;44:319-27.
- [CrossRef] [PubMed] [Google Scholar]
- Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: Effect of a 6-week training program on muscle recruitment and functional outcome. Am J Sports Med. 2012;40:1906-15.
- [CrossRef] [PubMed] [Google Scholar]
- Stretching the posterior shoulder structures in subjects with internal rotation deficit: Comparison of two stretching techniques. Shoulder Elbow. 2012;4:56-63.
- [CrossRef] [Google Scholar]
- Evidence based arm care: The throwers 10 revisited. Int J Sports Phys Ther. 2021;16:1379-86.
- [CrossRef] [PubMed] [Google Scholar]
- Physiotherapy treatment for atraumatic recurrent shoulder instability: Early results of a specific exercise protocol using pathology-specific outcome measures. Shoulder Elbow. 2015;7:282-8.
- [CrossRef] [PubMed] [Google Scholar]
- Defining return to sport: A systematic review. Orthop J Sports Med. 2021;9 Available from: http://dx.doi.org/10.1177/23259671211009589
- [CrossRef] [PubMed] [Google Scholar]
- The modified sleeper stretch and modified cross-body stretch to increase shoulder internal rotation range of motion in the overhead throwing athlete. J Orthop Sports Phys Ther. 2013;43:891-4.
- [CrossRef] [PubMed] [Google Scholar]
- No relationship between the acromiohumeral distance and pain in adults with subacromial pain syndrome: A systematic review and meta-analysis. Sci Rep. 2020;10:20611.
- [CrossRef] [PubMed] [Google Scholar]
- Quantifying acromiohumeral distance in overhead athletes with glenohumeral internal rotation loss and the influence of a stretching program. Am J Sports Med. 2012;40:2105-12.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of two stretching methods on shoulder range of motion and muscle stiffness in baseball players with posterior shoulder tightness: A randomized controlled trial. J Shoulder Elbow Surg. 2016;25:1395-403.
- [CrossRef] [PubMed] [Google Scholar]






