Translate this page into:
Current concepts on the surgical treatment of ramp, root, and radial meniscal tears
*Corresponding author: Robert F. LaPrade, Department of Orthopedic Surgery, Twin Cities Orthopedics, Edina, United States. laprademdphd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Willner AJ, Sami SL, Tollefson LV, LaPrade CM, LaPrade RF, Current concepts on the surgical treatment of ramp, root, and radial meniscal tears. J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_1_2025
Abstract
Background and Aims
Meniscus tears are among the most common sports medicine knee injuries. Proper diagnosis and treatment of ramp, root, and radial meniscus tears is critical to ultimately help improve patient outcomes. Each type of meniscus tear has unique tear locations and patterns, requiring different surgical repair techniques and rehabilitation protocols. This narrative review aims to discuss the diagnosis, treatment, and rehabilitation for ramp, root, and radial tears.
Materials and Methods
A narrative review was conducted to explore current surgical treatment and protocols for these three types of meniscal tears. A search was conducted on PubMed for all relevant literature.
Results
As the literature advances, there is growing evidence demonstrating improved outcomes for patients undergoing meniscal repairs. Ramp tears are often repaired using inside-out or all-inside techniques, while root tears require a transtibial tunnel or an all-inside repair. Radial tears are repaired using an inside-out, all-inside, or transtibial tunnel repair. Having current concepts on these repair techniques allows for surgeons to remain updated on the best treatment options.
Conclusions
As the important roles of the menisci for both knee biomechanics and joint health are becoming more well known, there is a greater emphasis on meniscus repair. Ramp, root, and radial tears are three common meniscus tears, and all should be repaired when possible. Proper understanding of the meniscus anatomy, tear diagnosis, treatment techniques, and rehabilitation is critical to optimize patient outcomes.
Keywords
All-inside
Inside-out
Radial
Ramp
Root
INTRODUCTION
The menisci are essential to knee function, providing stability, shock absorption, and load distribution.[1] The knee joint endures significant biomechanical demands, including converting axial loads into circumferential “hoop” stresses, allowing even dissipation of forces across the joint.[1,2] Ramp, radial, and root meniscal tears possess distinct anatomic locations and biomechanical implications, necessitating tailored diagnostic and treatment approaches. Meniscal tears contribute to cartilage wear and the development of osteoarthritis.[3,4]
Ramp lesions are commonly associated with anterior cruciate ligament (ACL) injuries.[1] These tears of the posterior medial meniscus involve the meniscocapsular junction of the posterior horn of the medial meniscus. They are often overlooked in imaging and arthroscopic evaluation, so they have been labeled “hidden lesions.”[1] Arthroscopic probing and precise diagnostics are necessary in assessing ACL-injured patients for concomitant ramp lesions, given that they are reported in 9–42% of cases.[5,6]
Meniscal root tears are analogous to total meniscectomies in their functional impact on the menisci.[7] Root tears involve disruptions at the meniscus attachment site and increase loads across the femur and tibia, accelerating cartilage degeneration. Posterior horn lateral meniscus root tears are commonly associated with ACL tears, while posterior horn medial meniscus root tears are commonly associated with degenerative tearing.[8] Emerging advancements, including arthroscopic transtibial pullout repair and suture fixation, have shown promise in restoring knee function following meniscal root tears.[9,10]
Radial tears are defined by a transverse separation of the meniscal circumferential fibers, significantly disturbing the load-bearing function of the menisci.[11] Due to their subtle morphology, conventional magnetic resonance imaging (MRI) often misses these lesions.[11] Their avascularity further complicates management, posing challenges for healing and surgical interventions.[12,13]
This narrative review synthesized recent literature on ramp, root, and radial meniscal tears, focusing on their anatomic features, clinical presentation, imaging modalities, treatment approaches, and rehabilitation protocols.
MATERIALS AND METHODS
This literature review was conducted to explore and summarize current literature on ramp, radial, and root meniscal tears. The primary search for relevant articles was conducted on PubMed, supplemented by additional exploratory searches on related databases, ensuring broad coverage. The search terms included combinations of the following keywords and Medical Subject Headings (MeSH) terms: “meniscus,” “ramp tear,” “radial meniscal tear,” “meniscal root tear,” “knee injuries,” “MRI diagnosis,” “arthroscopic surgery,” “repair techniques,” and “rehabilitation.” Boolean operators (AND, OR) were employed to optimize the retrieval of relevant articles. Articles were included based on their relevance to the review’s objectives, with a focus on peer-reviewed studied that provided insights into the diagnostic, surgical, and rehabilitation practices specific to these tear types.
ANATOMY
Crescent-shaped fibrocartilaginous structures, the menisci predominantly consist of type I collagen fibers, organized circumferentially to withstand tensile forces.[14] They have significant structural integrity for load bearing and are complemented by radially oriented tie fibers.[3,10] The medial meniscus, with its “C”-shape, has rigid attachments contributing to stability, while the smaller lateral meniscus exhibits greater mobility [Figure 1].[9,15]
![Illustration demonstrating the medial and lateral meniscal posterior root attachments and relevant arthroscopically pertinent anatomy (right knee). (a) Superior view and (b) posterior view. ACL: Anterior cruciate ligament, LPRA: Lateral meniscus posterior root attachment, LTE: Lateral tibial eminence, MPRA: Medial meniscus posterior root attachment, MTE: Medial tibial eminence, PCL: Posterior cruciate ligament, SWF: Shiny white fibers. Figure used with permission from Johannsen et al.[15]](/content/115/2025/0/1/img/JASSM-1-2025-g001.png)
- Illustration demonstrating the medial and lateral meniscal posterior root attachments and relevant arthroscopically pertinent anatomy (right knee). (a) Superior view and (b) posterior view. ACL: Anterior cruciate ligament, LPRA: Lateral meniscus posterior root attachment, LTE: Lateral tibial eminence, MPRA: Medial meniscus posterior root attachment, MTE: Medial tibial eminence, PCL: Posterior cruciate ligament, SWF: Shiny white fibers. Figure used with permission from Johannsen et al.[15]
Anatomic precision is essential in surgical approaches to meniscal repairs. The medial meniscus posterior root attachment is 9.6 mm posterior and 0.7 mm lateral to the medial tibial eminence apex, with a total attachment area of 110.4 mm2, including central and supplemental fibers. The lateral meniscus posterior root attachment is located 1.5 mm posterior and 4.2 mm medial to the lateral tibial eminence apex and has a larger footprint of 140.7 mm2.[14]
VASCULAR ZONES AND HEALING POTENTIAL
Meniscal vascularity has significant healing implications, with three zones identified: the red-red zone (outer vascular region), the red-white zone (partially vascular region), and the white-white zone (avascular region).[9] The red zone covers the peripheral portion of the meniscus – 10–30% of it – and extends less than 3 mm from the meniscocapsular junction.[10] The capsular vessels, branches of the genicular artery, perfuse this area, allowing for good healing potential. The red-white zone is 3–5 mm from the meniscocapsular junction and covers the middle third of the meniscus. The white zone lies 5 mm or more from the meniscocapsular junction and is relatively avascular, making healing challenging. Vascularity is vital for healing potential, with red-red zone tears having a higher healing potential when compared to white-white zone tears.[9,10]
BIOMECHANICS
The menisci minimize contact pressures through the even distribution of loads. When axial loads are applied to the knee, the circumferential fibers of the menisci generate “hoop” stresses, which support load transmission.[3] The menisci’s viscoelastic properties enable them to withstand tensile, compressive, and shear stresses.[16]
Functionally, ramp tears occur at the meniscocapsular junction, primarily involving the posterior horn of the medial meniscus or within 3 mm of the meniscus posterior rim [Figure 2]. Ramp tears are often observed in conjunction with ACL tears and can contribute to anteroposterior and rotational instability if left untreated.[5,6] The capsular attachment of the ramp region comprises the shared attachment of the meniscocapsular and meniscotibial ligaments to the PHMM. The posterior meniscocapsular attachment has a length of approximately 20.2 mm and connects at 36.4% of the total posterior meniscal height. The meniscotibial ligament attaches 16.5 mm posterior and 7.7 mm medial to the posterior medial meniscal root and is located 5.9 mm inferior to the articular cartilage of the posterior tibial plateau.[17] A cadaveric analysis revealed nuanced biomechanical implications. Under axial loading, ramp tears and other tears caused significant increases in peak contact pressure and reductions in contact area within the medial tibiofemoral joint, causing abnormal load distribution and a loss of hoop stress resistance.[7,18]
![(a) Sagittal view of a cadaveric dissection of the posterior horn medial meniscus (PHMM) anatomy, showcasing the meniscocapsular and meniscotibial ligament (MTL) attachments as they merge to form a common attachment. The posterior cruciate ligament facet is outlined in methylene blue to illustrate the proximity of its tibial attachment. (b) Illustration of the PHMM and shared common attachment of the meniscocapsular ligament and MTL. The MTL attached 5.9 mm distal to the articular cartilage margin of the posterior medial tibial plateau. Figure used with permission from DePhillipo et al.[17]](/content/115/2025/0/1/img/JASSM-1-2025-g002.png)
- (a) Sagittal view of a cadaveric dissection of the posterior horn medial meniscus (PHMM) anatomy, showcasing the meniscocapsular and meniscotibial ligament (MTL) attachments as they merge to form a common attachment. The posterior cruciate ligament facet is outlined in methylene blue to illustrate the proximity of its tibial attachment. (b) Illustration of the PHMM and shared common attachment of the meniscocapsular ligament and MTL. The MTL attached 5.9 mm distal to the articular cartilage margin of the posterior medial tibial plateau. Figure used with permission from DePhillipo et al.[17]
Root tears are typically located at the posterior horn meniscal attachments. Root tears effectively detach the meniscus from the tibial plateau, creating a condition functionally similar to a complete meniscectomy, resulting in elevated tibiofemoral contact stresses [Figure 3].[19] Morphological characteristics of these tears can be used to classify them, including the extent of the tear, relative location to root attachment, and bony involvement [Figure 4].[20] A finite element analysis highlighted disruption in hoop stresses with root tears, particularly in posterior root tears of the lateral meniscus. Lateral meniscus root tears lead to increased contact pressures and stress on the tibial cartilage (e.g., lateral compartment pressure rising from 3.09 MPa to 3.92 MPa) and a reduced joint contact area (lateral compartment decreasing from 512.286 mm2 to 487.992 mm2).[21,22] A study by Bernard et al. reported on the progression to arthroplasty at an average of 74 months follow-up for non-operative treatment, partial meniscectomy, and root repair for patients with a posterior medial meniscus root tear and found that the meniscus repair group had significantly less progression to osteoarthritis (P = 0.001).[23] Furthermore, they found that the partial meniscectomy group had the highest progression to arthroplasty (9/15 patients), followed by non-operative treatment (4/15 patients), and the root repair group had no progression to arthroplasty (0/15 patients).[23] When indicated, root repairs have become mainstay treatment to preserve the knee joint.[9]
![Posteromedial view photograph of the anatomic attachments to the posterolateral meniscus in a right knee. LC: Lateral capsule, PCL: Posterior cruciate ligament, PFL: Popliteofibular ligament, PHLM: Posterior horn of the lateral meniscus, PIF: Posteroinferior popliteomeniscal fascicle, pMFL: Posterior meniscofemoral ligament, PRLM: Posterior root of the lateral meniscus, PSF: Posterosuperior popliteomeniscal fascicle, PT: Popliteal tendon. Figure used with permission from Aman et al.[12]](/content/115/2025/0/1/img/JASSM-1-2025-g003.png)
- Posteromedial view photograph of the anatomic attachments to the posterolateral meniscus in a right knee. LC: Lateral capsule, PCL: Posterior cruciate ligament, PFL: Popliteofibular ligament, PHLM: Posterior horn of the lateral meniscus, PIF: Posteroinferior popliteomeniscal fascicle, pMFL: Posterior meniscofemoral ligament, PRLM: Posterior root of the lateral meniscus, PSF: Posterosuperior popliteomeniscal fascicle, PT: Popliteal tendon. Figure used with permission from Aman et al.[12]
![Illustrations of the meniscal root tear classification system in five different groups based on tear morphology. All meniscal tears are shown as medial meniscal posterior root tears for consistency in this illustration. The five tear patterns were classified based on morphology: (Type 1) partial stable root tear, (Type 2) complete radial tear within 9 mm from the bony root attachment, (Type 3) bucket-handle tear with complete root detachment, (Type 4) complex oblique or longitudinal tear with complete root detachment, and (Type 5) bony avulsion fracture of the root attachment. Figure used with permission from LaPrade et al.[20]](/content/115/2025/0/1/img/JASSM-1-2025-g004.png)
- Illustrations of the meniscal root tear classification system in five different groups based on tear morphology. All meniscal tears are shown as medial meniscal posterior root tears for consistency in this illustration. The five tear patterns were classified based on morphology: (Type 1) partial stable root tear, (Type 2) complete radial tear within 9 mm from the bony root attachment, (Type 3) bucket-handle tear with complete root detachment, (Type 4) complex oblique or longitudinal tear with complete root detachment, and (Type 5) bony avulsion fracture of the root attachment. Figure used with permission from LaPrade et al.[20]
Radial tears are characterized by disruption of circumferential collagen fibers.[11] Radial tears hinder the meniscus’s ability to absorb and distribute load effectively. Radial tears often occur in the avascular white-white zone. They can progress into the re-white and red-red zones, presenting challenges in healing and increasing the risk of osteoarthritis.[3,12] A finite element musculoskeletal modeling study demonstrated that the burden radial tears have on the menisci’s ability to transmit circumferential hoop stress. Wider tears concentrate the shear stresses at the tear ends, increasing the risk of complete tearing and failure. Despite the minimal increase in tibial cartilage loading – a 9% increase in the most severe cases – disrupting hoop stresses accelerate degenerative processes of the knee.[24]
TREATMENT OPTIONS AND TECHNIQUES
The preferred treatment for meniscal tears has been reevaluated and changed over many years of research. Historically, while it used to be common practice to remove the meniscus tear through a partial meniscectomy, it is now preferable to attempt a meniscal repair when possible due to the risk of early-onset osteoarthritis and very poor outcomes after a total meniscectomy. Of course, the decision to treat some meniscal tears nonoperatively is warranted if the tear is stable and in a well-healing vascularized area. In addition, the choice between a meniscal repair and partial meniscectomy depends on tear type and location. For example, a tear in the red-red vascular zone can allow for an improved chance of healing and may be more amenable to a repair.[25] Regarding the tear type, there are differences in repair techniques and outcomes that should be considered when managing meniscal injuries.[26,27] Meniscal repairs can be performed either arthroscopically or open, but arthroscopic surgeries have been the more popular choice in recent years. Open repair or arthroscopic assisted open repairs can be an option for surgeries where small areas do not allow for the scope to visualize the body tissue, such as for anterior root tears.[28]
RAMP TEARS
Ramp tears are very commonly associated with ACL tears, and they can increase anterior tibial translation instability to the knee following traumatic injury [Figure 5].[29] Diagnosing a ramp tear can often be difficult because they can be missed on both MRI and arthroscopically.[30,31] Treatment of ramp tears depends on their overall stability. If ramp tears are small and stable and have occurred with an ACL tear, reconstruction of the ACL without meniscus repair may be indicated. However, if the ramp tear is unstable to arthroscopic probing, it is important to perform a repair as the tears may worsen or even become bucket-handle tears,[32] and this could lead to ACL reconstruction graft failure.[33] Arthroscopic repair can be performed using several techniques. An all-inside ramp repair technique can be performed using either anterior portals or through a posteromedial portal with suture hooks.[34] This involves using an arthroscopic probe to visualize the meniscal tear and a spinal needle can be used as needed to trephinate the MCL to improve access to the medial compartment. As with many meniscal repairs, an arthroscopic shaver can be used to help improve healing by gently debriding the synovial and tear edges. A curved cannula is used for the suture hook technique to deliver the suture limbs, and vertical sutures are tied for the repair of the ramp lesion.[34] An inside-out technique can also be performed. With this technique, anteromedial and anterolateral portals are made, and an arthroscope is placed in the anterolateral portal. A surgical probe is used to confirm the ramp tear before dissection is used to create the surgical posteromedial or posterolateral incisions. A cannula can then be used to direct sutures above and below the tear.[35] This technique allows the surgeon to place more sutures to ensure a stronger repair, but it does come with an increased risk of neurovascular injury of the knee. Both techniques have had good patient reported outcomes, and the choice between the two techniques depends more on the surgeon’s skill, the size of the tear, and accessibility of the tear itself.[36,37]
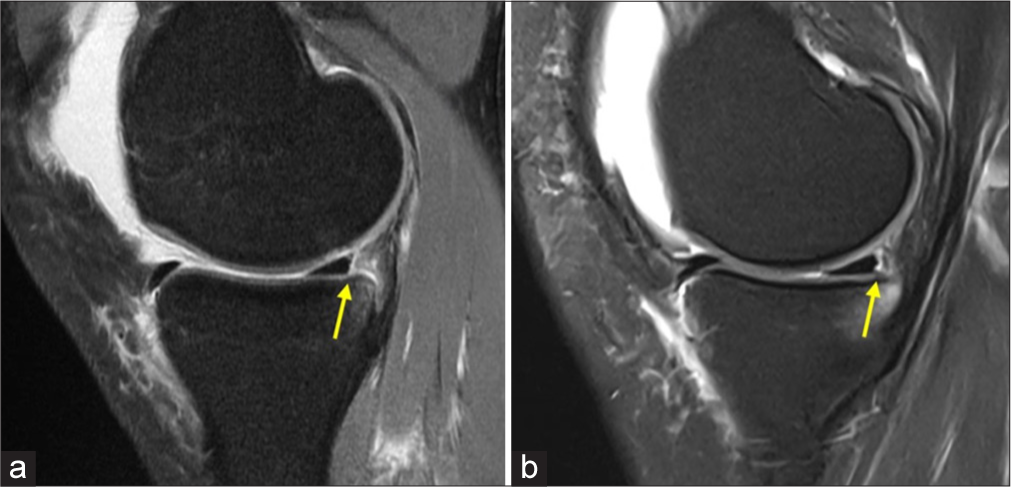
- Magnetic resonance imaging (MRI) (a) sagittal view of a ramp tear in the posteromedial meniscocapsular junction and (b) posteromedial meniscus within 3 mm of the peripheral rim. The ramp tears are marked with yellow arrows. Both MRIs present with posteromedial tibial plateau bruising.
ROOT TEARS
Treatment and outcomes of a root tear can depend heavily on its location and the status of the ipsilateral knee compartment cartilage surfaces. A medial meniscus posterior root tear is more often found in older patients with higher BMIs, while lateral meniscus posterior root tears are typically traumatic, most often concurrent with an ACL tear [Figure 6].[38] In these cases, meniscal repair and transtibial fixation is indicated.[26] Non-operative treatment may be indicated in patients with progressive osteoarthritis or in patients who are unable to follow the post-operative rehabilitation protocol. Meniscectomy is generally not indicated unless the tear is degenerative and causes severe pain or mechanical symptoms.[23] Regarding repair of meniscal root tears, there are two options that are more frequently used: transtibial repair and all-inside repair. The former and more common technique involves using transtibial tunnels to pass sutures through after these sutures are placed into the meniscal root. The transtibial technique is used to pull the meniscus back into its anatomic location. The sutures are then anchored over a surgical button placed on the anterior tibia.[39] The all-inside technique is similar to that performed for ramp tears using two vertical mattress sutures to stabilize the root tear using an anteromedial or anterolateral portal.[40]
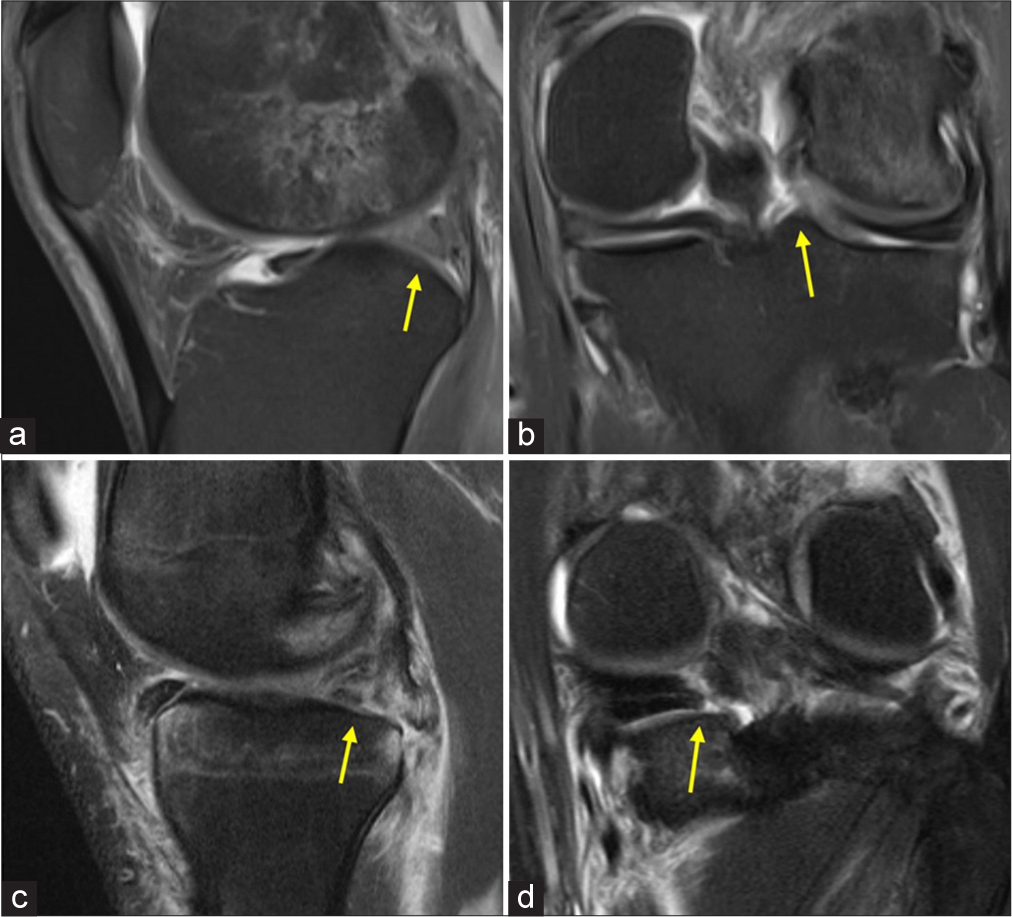
- Magnetic resonance imaging of left knees with signs demonstrating evidence of (a and b) lateral and (c and d) medial posterior meniscal root tear. (a and c) Sagittal view of the left knee showing a ghost sign (yellow arrows) which is a common indicator of (a) lateral and (c) medial posterior meniscus root tear. (b and d) Coronal view of the left knee showing the (b) lateral and (d) medial posterior meniscus root tears (yellow arrows).
RADIAL TEARS
Since radial tears are often found in regions of the meniscus with poor vascularity, they can be especially difficult to heal. Optimally, if possible, a repair is preferred over an arthroscopic partial meniscectomy if the tear extends beyond the white-white zone of the meniscus [Figure 7]. It should be noted that a meniscectomy is an option for patients if a successful repair is unlikely.[28] The “inside-out” meniscus repair approach involves deploying repair sutures along the tear edges without damaging the meniscus. However, this approach uses a posteromedial or posterolateral knee incision that could potentially cause neurovascular injury to the knee.[41] Another option, the “all-inside” technique has become a popular method for repairing radial tears. While this technique allows for the procedure to be completed in less time with fewer technically challenging steps, it does involve placing larger diameter repair sutures which may compromise the radial tear edges. It is an important option for radial meniscal tears when a surgeon may not have a surgical assistant or be familiar with an inside-out radial repair approach.[42] Newer techniques are becoming a more frequent part of operative treatment of meniscal radial tears. The “hashtag” technique involves using vertical mattress near the edges of the radial tear, followed by horizontal mattress sutures resembling the shape of a “hashtag” that are placed to help repair the meniscus tear.[43] Another technique involves using transtibial tunnels to repair the radial tear, especially when the radial tear edges are widely displaced. This technique uses one or two tunnels coursing from the anteromedial or anterolateral tibia to the radial tear at the meniscus. Typically, the first tunnel is made more posteriorly at the radial tear. Self-capture sutures are placed in the meniscus, similar to those placed for root tears, and are passed down the tunnels and tied over buttons on the tibia. Using tibial tunnels allows for the widely separated rims of the radial meniscus tears to be approximated together before the use of a hashtag suture repair technique. Vertical mattress sutures are then placed on each side of the radial tear. Finally, inside-out horizontal mattress sutures are placed at the margins of the vertical mattress sutures to complete the hashtag repair of the radial tear.[44] For radial tear repairs, especially when no tunnels are used, orthobiologic augmentation like bone marrow venting should be considered to augment the healing potential.
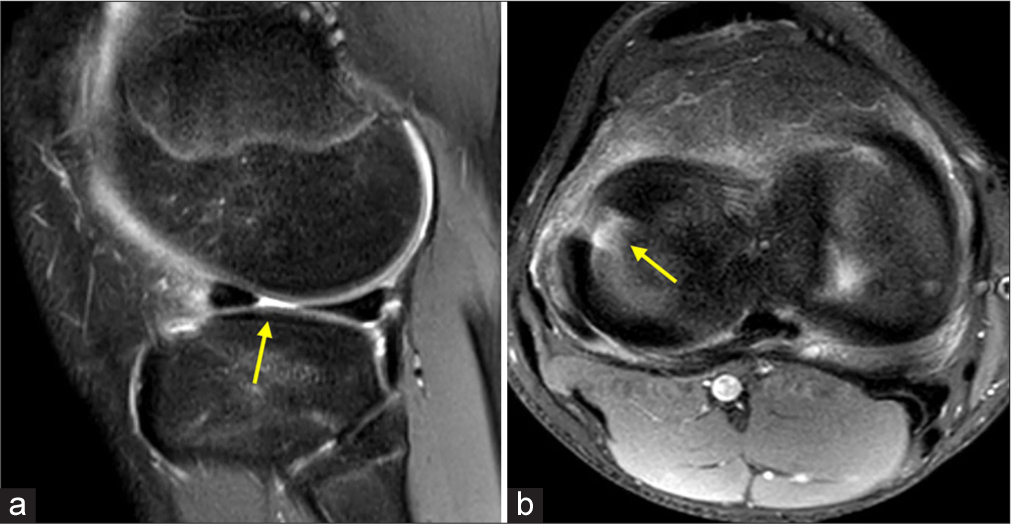
- Magnetic resonance images of a complete radial tear in (a) sagittal view and (b) axial view. Radial tears typically present as a fluid filled break in the meniscus on both sagittal and axial magnetic resonance imaging views. The yellow arrows point to the location of the tears.
In addition, tears located in the anterior horn of the meniscus are often repaired using an “outside-in” technique, usually through an arthroscopic technique. After enlarging the arthroscopic portal over the anterior meniscal tear, a spinal needle is used to enter the capsule and is brought under the medial or lateral meniscus through the anterior horn tear.[45] Using this spinal needle, sutures can be passed into the joint to allow for repair of the meniscal tear.[46] Horizontal or vertical mattress sutures are used for the repair, and it is acceptable to use as many sutures as needed to fully repair the tear.[45]
REHABILITATION AND RECOVERY
For ramp tear repairs performed concurrently with an ACL reconstruction, the recovery and post-operative rehabilitation protocol is the same as the surgeon’s postoperative ACL rehabilitation protocol. This typically involves weight-bearing as tolerated following surgery and transitioning off crutches when one can ambulate without a limp, but some guidelines recommend partial weight-bearing with full extension in the first few weeks after surgery.[47] Clearance for full activities in patients with a ramp tear repair is based on the surgeon’s post-operative ACL rehabilitation protocol and is a minimum of 9 months postoperatively.
Patients with meniscal root and radial repairs are advised to be non weight bearing (NWB) for 6 weeks.[48] Their range of motion (ROM) is typically limited to 0–90° for 2 weeks and can be increased as tolerated afterward. These patients should be careful to avoid deep flexion movements, such as squats and lunges, for approximately 4 months, especially for patients with root tears. For those patients with a medial meniscal root or radial repair and varus alignment or those with an isolated lateral meniscus root or radial repair, the use of a medial or lateral compartment unloader brace, respectively, starting at 6 weeks after surgery when they begin weight-bearing until 4 months after surgery is recommended due to the reported negative effects of malalignment on meniscal root and radial repairs. In patients with severe malalignment, a concurrent realignment osteotomy can be considered. The usual time to be cleared to full activities after a radial or root repair is a minimum of 6 months postoperatively or 9–12 months when concomitant with an ACL reconstruction.[29,49]
Using physical therapy and at-home exercises, patients can begin to increase their ROM and work on progressive strengthening through active recovery. In addition, strength testing for return to athletic competition should be used to monitor patient progress and surgical outcomes. Guidelines regarding return to play for athletes are also provided for patients, and recent studies have shown promising outcomes regarding return to play for athletes who have undergone meniscal repair.[50]
CLINICAL OUTCOMES
For ramp tear repairs, studies have shown good clinical outcomes following repair. Following an all-inside repair of a ramp tear with an ACL reconstruction, second-look arthroscopy in 46 patients showed 86.9% with complete healing, 10.8% with partial healing, and 2.1% with complete failure.[51] In another study, patients who had chosen to nonoperatively treat their stable ramp lesions were followed up at a minimum of 20 years and 28.6% of these patients were found to have meniscal failure, with 21% sustaining a bucket-handle tear.[36] This may highlight the importance of repairing ramp lesions before they worsen, even in patients who have smaller stable tears. Research has shown a greater chance of failure using the all-inside technique for ramp tears in the medial aspect of the ramp area, so a shift toward the inside-out technique or a hybrid procedure may be warranted in these cases.[32]
Outcomes following root repairs have been favorable with a low failure rate around 7% and around 80% of patients having no progression of osteoarthritis.[8] Patients have also had good subjective improvement using patient reports measurements >2 years postoperatively after a root repair.[8] There has also been very little difference in outcomes for patients of different ages or for lateral versus medial root tears.[8] Another study used MRI to evaluate healing rates for patients who had undergone meniscal root repair. They found that 93.3% of patients had evidence of complete healing with an average follow-up period of 46.1 months. Patients who underwent meniscal repair compared to partial meniscectomy were found to have improved Lysholm scores, less arthritic progression, and improved radiological findings.[52]
In a systematic review analyzing patient reported outcomes (Lysholm score and Tegner Activity Scale) from 12 studies who reported on 243 radial meniscal repairs, Milliron et al. found that patients had improved outcomes following surgical repair.[53] The range of Lysholm scores increased from 47–68.9 preoperatively to 86.4–95.6 postoperatively, while the Tegner Activity scaled showed a similar increase postoperatively (2.5–3.1–4.7–6.7). Second-look arthroscopy demonstrated 62% of patients with complete healing, 30% with partial healing, and 9% failure to heal following a two tunnel transtibial pullout technique. This indicates improved outcomes following radial repair with a low chance of failure.[53] In addition, a study using the inside-out repair for radial tears has shown healing of the tear visualized with MRI and patients reporting decreased pain postoperatively.[36]
CONCLUSION
As the important roles of the menisci for both knee biomechanics and joint health are becoming more well known, there is a greater emphasis on meniscus repair. Ramp, root, and radial tears are three common meniscus tears, and all should be repaired when possible. Proper understanding of the meniscus anatomy, tear diagnosis, treatment techniques, and rehabilitation is critical to optimize patient outcomes. This knowledge will enable surgeons and medical staff to better treat patients with ramp, root, and radial meniscus tears, slow the progression of osteoarthritis, and ultimately improve long-term patient outcomes.
Author contributions
LT, RL, AW, SS: Concept and design of the study; AJW, SLS: Literature review, analysis and interpretation of literature. All the authors contributed to drafting of the article or revising, final approval, and all the authors are accountable for all the aspects of the article.
Ethical approval
The Institutional Review Board approval is not required since it is a narrative review with no patient data.
Declaration of patient consent
Patient consent is not required as patient identity is not disclosed or compromised.
Conflicts of interest
Robert F. LaPrade reports a relationship with Ossur Americas that includes: consulting or advisory. Robert F. LaPrade reports a relationship with Smith and Nephew Inc that includes: consulting or advisory. Robert F. LaPrade reports a relationship with Linvatec Europe that includes: consulting or advisory. Robert F. LaPrade reports a relationship with Responsive Arthroscopy that includes: consulting or advisory. Robert F. LaPrade reports a relationship with Ossur Americas Inc that includes: funding grants. Robert F. LaPrade reports a relationship with Smith and Nephew Inc. that includes: funding grants. Robert F. LaPrade reports a relationship with Arthroscopy Association of North America that includes: funding grants. Robert F. LaPrade reports a relationship with American Orthopaedic Society for Sports Medicine that includes: funding grants. Christopher M. LaPrade reports all the same disclosures as Robert F. LaPrade as they are family members. Christopher M. LaPrade reports a relationship with Foundation Medical that includes: speaking and lecture fees. Christopher M. LaPrade reports a relationship with Evolution Surgical that includes: speaking and lecture fees.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Ramp lesion in anterior cruciate ligament injury: A review of the anatomy, biomechanics, epidemiology, and diagnosis. Knee Surg Relat Res. 2023;35:23.
- [CrossRef] [PubMed] [Google Scholar]
- Radial meniscal tears: Significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005;185:1429-34.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and patterns of meniscal tears accompanying the anterior cruciate ligament injury: Possible local and generalized risk factors. Int Orthop. 2018;42:2113-21.
- [CrossRef] [PubMed] [Google Scholar]
- The “Hand as Foot” teaching method in meniscal anatomy. Asian J Surg. 2023;46:4028-30.
- [CrossRef] [PubMed] [Google Scholar]
- MRI of the knee meniscus. Magn Reson Imaging Clin N Am. 2022;30:307-24.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: A biomechanical study. Am J Sports Med. 2018;46:2422-31.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: A decade of research on their relevant anatomy, biomechanics, diagnosis, and treatment. Arch Bone Jt Surg. 2022;10:366-80.
- [Google Scholar]
- Review of meniscus anatomy and biomechanics. Curr Rev Musculoskelet Med. 2022;15:323-35.
- [CrossRef] [PubMed] [Google Scholar]
- Knee MRI: Meniscus roots, ramps, repairs, and repercussions. Radiographics. 2023;43:e220208.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal radial tears: A classification system based on tear morphology. Arthrosc Tech. 2024;13:102888.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative and qualitative assessment of posterolateral meniscal anatomy: Defining the popliteal hiatus, popliteomeniscal fascicles, and the lateral meniscotibial ligament. Am J Sports Med. 2019;47:1797-803.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus anatomy-from basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23:8-14.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of the anterior root attachments of the medial and lateral menisci: A quantitative analysis. Am J Sports Med. 2014;42:2386-92.
- [CrossRef] [PubMed] [Google Scholar]
- Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342-7.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanical properties of human menisci: A systematic review. Acta Biomater. 2024;175:1-26.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative and qualitative assessment of the posterior medial meniscus anatomy: Defining meniscal ramp lesions. Am J Sports Med. 2019;47:372-8.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical impact of meniscal ramp lesions on knee joint contact characteristics in ACL deficient knees: A cadaveric analysis. Eur J Orthop Surg Traumatol. 2024;34:2735-42.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922-31.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363-9.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: Clinical and economic effectiveness. Am J Sports Med. 2019;47:762-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of different repair methods for a posterior root tear of the lateral meniscus on the biomechanics of the knee: A finite element analysis. J Orthop Surg Res. 2021;16:296.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus posterior root tear treatment: A matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med. 2020;48:128-32.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical effects of medial meniscus radial tears on the knee joint during gait: A concurrent finite element musculoskeletal framework investigation. Front Bioeng Biotechnol. 2022;10:957435.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular biology of meniscal healing: A narrative review. Int J Mol Sci. 2024;25:768.
- [CrossRef] [PubMed] [Google Scholar]
- Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017;103:S237-44.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscus tear: Pathology, incidence, and management. Cureus. 2022;14:e25121.
- [CrossRef] [Google Scholar]
- Modern treatment of meniscal tears. EFORT Open Rev. 2018;3:260-8.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus ramp tears: State of the art. J ISAKOS. 2024;10:100380.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2233-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921-6.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscus tears treatment: The good, the bad and the ugly-patterns classification and practical guide. World J Orthop. 2023;14:171-85.
- [CrossRef] [PubMed] [Google Scholar]
- Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: Outcome study with a minimum 2-year follow-up. Arthroscopy. 2016;32:2269-77.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic all-Inside repair of meniscal ramp lesions. J ISAKOS. 2022;7:82-3.
- [CrossRef] [PubMed] [Google Scholar]
- Inside-out repair of medial meniscal ramp lesions in patients undergoing anterior cruciate ligament reconstruction. JBJS Essent Surg Tech. 2024;14:e22.00037.
- [CrossRef] [Google Scholar]
- Meniscal ramp lesions: A lot is known, but a lot is also unknown. Knee Surg Sports Traumatol Arthrosc. 2023;31:2535-9.
- [CrossRef] [PubMed] [Google Scholar]
- Inside-out repair of meniscal ramp lesions. Arthrosc Tech. 2017;6:e1315-20.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment strategies of meniscus root tears: A scoping review. Orthop J Sports Med. 2024;12:23259671241283962.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior meniscal root repair with transtibial double tunnel pullout technique and anchor fixation. Arthrosc Tech. 2023;12:e1133-8.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscal posterior root tear-A current concept review. J Arthrosc Surg Sports Med. 2024;5:107-14.
- [CrossRef] [Google Scholar]
- All-inside meniscus repair. Curr Rev Musculoskelet Med. 2022;15:252-8.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscus radial tears: Current concepts on management and repair techniques. Curr Rev Musculoskelet Med. 2023;16:182-91.
- [CrossRef] [PubMed] [Google Scholar]
- Techniques to treat challenging meniscus tears. J Cartil Joint Preserv. 2023;3:100106.
- [CrossRef] [Google Scholar]
- Two-tunnel transtibial repair of radial meniscus tears produces comparable results to inside-out repair of vertical meniscus tears. Am J Sports Med. 2017;45:2253-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior horn meniscal repair using an outside-in suture technique. Arthrosc Tech. 2016;5:e1111-6.
- [CrossRef] [PubMed] [Google Scholar]
- Outside-in-outside repair technique for anterior horn and body meniscal tear: A modified technique. Arthrosc Tech. 2024;13:103057.
- [CrossRef] [PubMed] [Google Scholar]
- Management of meniscus pathology with concomitant anterior cruciate ligament injury. Curr Rev Musculoskelet Med. 2024;17:321-34.
- [CrossRef] [PubMed] [Google Scholar]
- Rehabilitation following meniscal repair: A systematic review. BMJ Open Sport Exerc Med. 2018;4:e000212.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscus tears in elite athletes: Treatment considerations, clinical outcomes, and return to play. Curr Rev Musculoskelet Med. 2024;17:313-20.
- [CrossRef] [PubMed] [Google Scholar]
- Return-to-play and rehabilitation protocols following isolated meniscal repair-a systematic review. Arthrosc Sports Med Rehabil. 2021;3:e241-7.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal ramp lesion repair using the fast-fix technique: evaluating healing and patient outcomes with second-look arthroscopy. J Knee Surg. 2018;31:710-15.
- [CrossRef] [PubMed] [Google Scholar]
- Repair of radial meniscus tears results in improved patient-reported outcome scores: A systematic review. Arthrosc Sports Med Rehabil. 2021;3:e967-80.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus posterior root tear: A comprehensive review. Knee Surg Relat Res. 2014;26:125-34.
- [CrossRef] [PubMed] [Google Scholar]







