Translate this page into:
Deltoid muscle hernia: An unusual site of myofascial hernia
*Corresponding author: Rajesh Botchu, Department of Musculoskeletal Radiology, Royal Orthopedic Hospital, Birmingham, United Kingdom drrajeshb@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mettu S, Shirodkar K, Iyengar KP, Botchu R. Deltoid muscle hernia: An unusual site of myofascial hernia. J Arthrosc Surg Sports Med. 2025;6:78-81. doi: 10.25259/JASSM_37_2024
Abstract
Muscle hernias are relatively uncommon, with most cases reported in the leg involving the tibialis anterior muscle. However, hernias can affect other muscles in both the upper and lower limbs. Here, we present the first documented case of nontraumatic deltoid muscle hernia. An 80-year-old woman presented to the outpatient department with soft tissue masses on the lateral aspect of her left shoulder, accompanied by mild activity-related pain. Dynamic ultrasonography was done and revealed two discrete transfascial defects through which herniation of outer fibres of deltoid muscle into the subcutaneous plane was noted which was prominent on abduction, features characteristic of muscle hernia. No further investigations were pursued, and the patient was reassured and advised to limit activities involving the affected muscle. This article underscores the importance of considering muscle hernias in the differential diagnosis of soft tissue masses, even when occurring in atypical locations such as the deltoid muscle, and the importance of ultrasound examination in such cases.
Keywords
Deltoid
Muscle hernia
Musculoskeletal
Ultrasonography
Myofascial hernia
INTRODUCTION
A muscle hernia, also known as a myofascial hernia, is defined as a focal protrusion of the muscle belly through an acquired or, less commonly, congenital fascial defect.[1] These hernias are classified as traumatic or constitutional. Constitutional muscle hernias typically result from factors such as vigorous exercise, muscle hypertrophy, or increased intra-compartmental pressure, leading to herniation at points of fascial weakness. Non-traumatic hernias are often painless, with the main concern being the possibility of an underlying benign or malignant neoplasm. However, some cases may become painful during prolonged muscle contraction or exercise due to focal muscle entrapment and ischemia.[2] While the tibialis anterior muscle is most commonly affected, hernias can involve other muscles in both the upper and lower limbs. On review of existing literature, our case appears to be the first documented instance of a deltoid muscle hernia.
CASE REPORT
An 80-year-old female presented to the outpatient department with soft-tissue masses on the lateral aspect of her left shoulder, which were mildly painful during activity. She has no history of trauma. Clinical examination revealed well-defined swelling observed solely on outward abduction of the arm, accompanied by pain during this motion. The lesion was not clearly discerned on palpation, and the overlying skin appeared normal. The rest of the shoulder movements were equal to the opposite side, with intact axillary nerve sensation.
There were no other similar swellings in the ipsilateral limb. Ultrasonography (USG) of the region pinpointed by the patient revealed two discrete defects in the deep fascia, through which the outer muscle fibers of the deltoid muscle protruded into the subcutaneous fat. Dynamic ultrasound examination revealed more pronounced herniation during abduction, measuring 10 mm × 10 mm and 8 mm × 8 mm [Figures 1-4 and Video 1]. The herniated muscle displayed an isoechoic appearance compared to the deeper muscle lying beneath the fascia. Our imaging diagnosis confirmed deltoid muscle hernia, with characteristic ultrasound findings rendering further investigations unnecessary. The patient was reassured and advised to restrict activity involving the affected muscle.
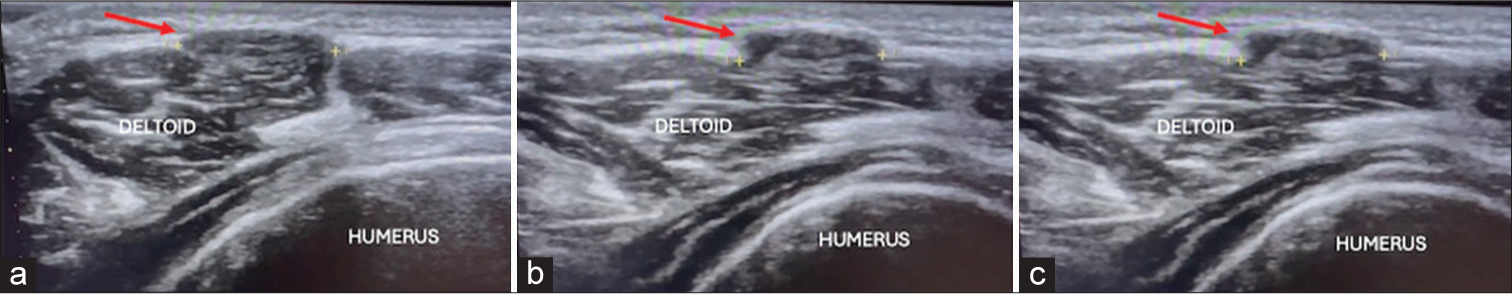
- (a) Short axis ultrasound and (b and c) longitudinal ultrasound image showing herniation of deltoid muscle (red arrows).
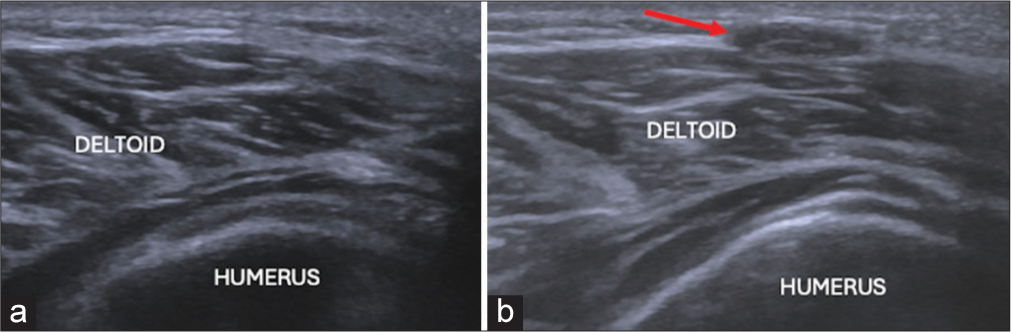
- (a) Short axis ultrasound image and (b) on stressing showing herniation of deltoid through fascial defect (red arrow).
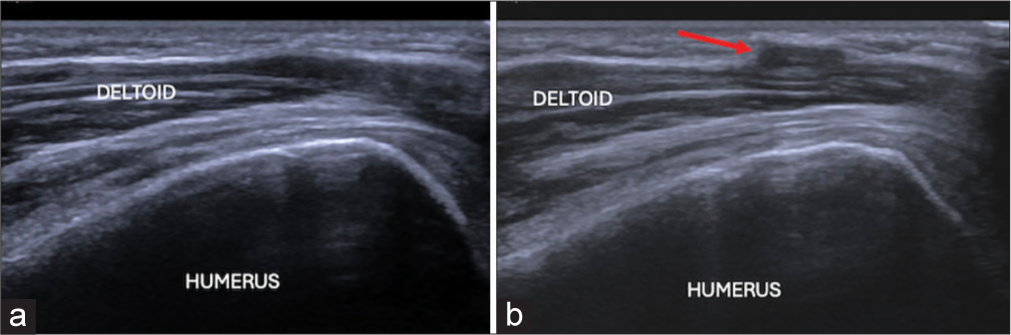
- (a) Longitudinal ultrasound image and (b) on stressing showing herniation of deltoid through fascial defect (red arrow).
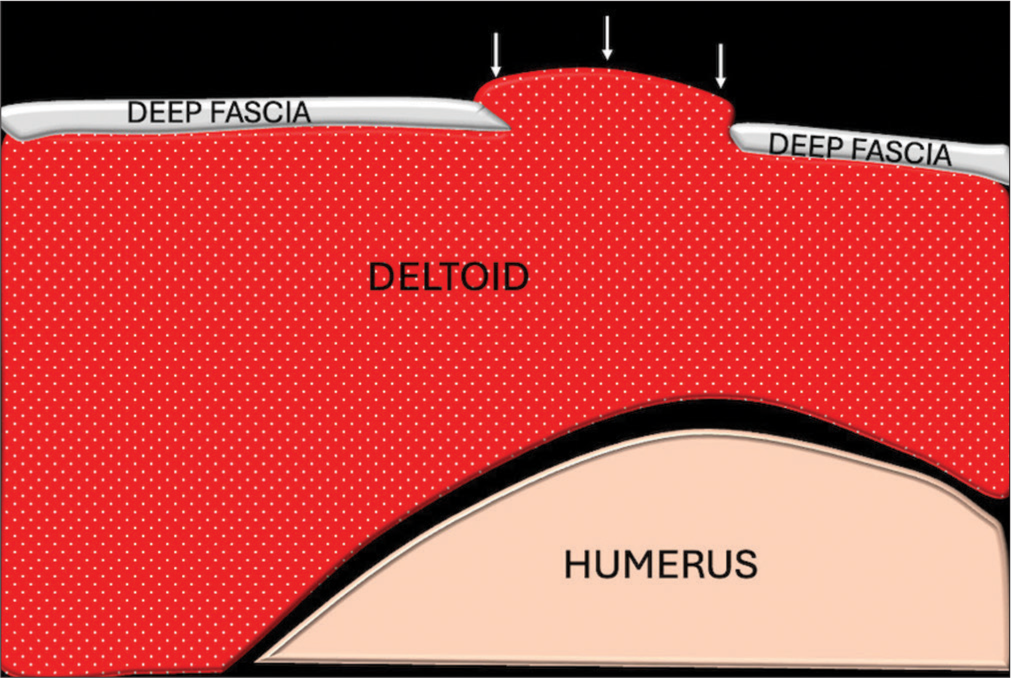
- Schematic representation showing deltoid hernia (white arrows).
Video 1:
Video 1:Video of ultrasound showing herniation of deltoid muscles through defect in deep fascia.DISCUSSION
In myofascial hernias, muscles extend through a fascial defect into the subcutaneous fat, manifesting clinically as a soft-tissue mass.[1] A review of current literature indicates that fewer than 35 reported cases of upper-limb muscle hernias exist, predominantly affecting the volar aspect of the forearm. Most cases result from traumatic causes, such as blunt force or penetrating trauma.[3] Non-traumatic hernias of the upper limb are rare, with only a few documented instances [Table 1].[4-8]
| Authors/Year | Number of cases | Compartment | Muscle | Cause | Treatment |
|---|---|---|---|---|---|
| Khalid et al. (2009)[3] | 1 | Volar forearm | Not mentioned | Strenuous exertion | Fasciorrhaphy |
| Sanders et al. (2011)[4] | 1 | Volar forearm | Not mentioned | Strenuous exercise | Fasciorrhaphy |
| Lim et al. (2015)[5] | 1 | Dorsal forearm | ECU | Strenuous exercise | Fasciorrhaphy |
| Kendi et al. (2003)[6] | 1 | Volar forearm | FDS | Strenuous exertion | Conservative |
| Roberts et al. (1989)[7] | 1 | Extensor forearm | EDC | Strenuous exertion | Fasciorrhaphy |
| Schwartz-Fernandes et al. (2019)[8] | 1 | Volar forearm | FCU | Iatrogenic | Fasciorrhaphy |
ECU: Extensor carpi ulnaris, FDS: Flexor digitorum superficialis, EDC: Extensor digitorum communis, FCU: Flexor carpi ulnaris
A clinical history of soft-tissue mass exhibiting fluctuation in size with physical activity can suggest a diagnosis of muscle hernia. A high index of suspicion is required, especially for muscle hernias in unusual sites. On clinical examination, a focal fascial defect leading to muscle herniation into the subcutaneous fat may present as a palpable bulge, soft-tissue mass, or subcutaneous nodule. These hernias can be solitary or multiple, but palpation alone may not always provide a definitive diagnosis, especially in subtle cases.[9]
Imaging is essential to confirm and evaluate the myofascial defect, rule out soft-tissue masses and other mimics, and guide appropriate treatment. In situations where there is a relevant clinical history, physical examination findings, and a strong suspicion of muscle hernia, USG serves as an appropriate initial imaging modality. In all such instances, it is recommended to conduct a targeted ultrasound examination using a high-frequency linear probe. During ultrasound, the thin superficial layer of the deep fascia, located at the interface of the subcutaneous fat and muscle, can be visualized as a thin, echogenic, and bright line superficial to the muscle. A muscle hernia is identified as a disruption in this echogenic fascia, with muscle protruding into the defect.[10] The hernia becomes more prominent when the muscle is contracted. A pitfall when conducting an ultrasound is to avoid applying excessive pressure with the ultrasound probe, as this may inadvertently reduce the hernia and lead to a false-negative examination. Sonography offers several advantages, including the ability to dynamically examine the patient and demonstrate the nature of the lesion during the examination. Since surgical repair is typically unnecessary in many cases, visualizing the hernia on sonography helps reassure the patient.[11] Magnetic resonance imaging (MRI) becomes necessary when surgical repair is being considered, particularly in cases where severe pain is present. The diagnostic accuracy of MRI and ultrasound for assessing muscle hernia is comparable. MRI offers the advantage of better identifying which muscle is involved and characterizing any identified soft-tissue mass.[9] However, a defect in the fascia is not always visualized on MRI, although it can be inferred from abnormal muscle contour. Subtle muscle hernias may sometimes go undetected on MRI because myofascial hernias may not be apparent without muscle contraction.
Based on the location of the hernia, the possibility of nerve entrapment must be considered.[2] In our case, herniation of the lateral deltoid muscle belly was observed, and it is noteworthy that cutaneous branches of the axillary nerve are present in this area. However, our patient did not have any paresthesia or other symptoms suggestive of nerve entrapment.
The differential diagnosis of deltoid muscle hernia includes other soft-tissue masses such as vascular malformations, hemangiomas, and tumors, including lipomas and peripheral nerve sheath tumors.[12]
Arteriovenous malformations typically present as well-defined solid hypoechoic lesions with small cystic spaces. The lesions often exhibit multiple areas of internal vascularity with mixed arterial and venous flow, and an arterial feeder may be visible.
Intramuscular lipomas typically appear as hyperechoic, well-defined masses with fine internal echoes or a striated appearance due to interdigitations of muscular tissue. While lipomas are usually asymptomatic, they may cause pain and paresthesia due to nerve entrapment.
Intramuscular hemangiomas typically manifest as slow-growing masses, with pain worsening after exercise. On ultrasound, these lesions appear hypoechoic to skeletal muscle, although they can also be isoechoic or hyperechoic. Unlike muscle hernias, which are characterized by their reducibility on the application of pressure from an ultrasound probe, hemangiomas are non-reducible vascular tumors. On Doppler imaging, they exhibit pulsatile arterial waveforms. Benign and malignant peripheral nerve sheath tumors display variable sonographic features. Common characteristics include a hypoechoic and homogeneous appearance, posterior acoustic enhancement, and continuity with peripheral nerves.
Most muscle hernias are managed with reassurance because they typically produce no or few symptoms and do not impact function significantly. For mild symptoms, activity restriction and hand therapy may provide relief. Surgical intervention, such as wide fasciotomy, is reserved for patients with severe symptoms.[13]
CONCLUSION
This case is the first recorded instance of a deltoid muscle herniation in English medical literature. It underscores the importance for radiologists and clinicians to consider muscle hernias when assessing potential soft-tissue masses in the deltoid region. Patients often express concern that the palpable lump may be a tumor; however, characteristic sonographic features of muscle hernias aid in excluding alternative clinical diagnoses. In addition, asymptomatic muscle hernias typically do not require surgical intervention. In such cases, providing reassurance to the patient based on imaging findings becomes a crucial aspect of management.
Author contributions
SM and RB: Conception and design, or acquisition of data, or analysis and interpretation of data, design, or acquisition of data, or analysis and interpretation of data; SM, KS, KPI, RB: Drafting the article or revising it critically for important intellectual content, and final approval of the version to be published.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Superficial peroneal nerve compression due to peroneus brevis muscle herniation. J Radiol Case Rep. 2019;13:10-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of a symptomatic forearm muscle herniation with a wrap-around fascia lata graft. J Hand Microsurg. 2009;1:54-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of a symptomatic forearm muscle herniation with a mesh graft. Sports Health. 2011;3:179-81.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic non-traumatic muscle hernia in the dorsal forearm. JPRAS Open. 2015;3:26-8.
- [CrossRef] [Google Scholar]
- Imaging in the diagnosis of symptomatic forearm muscle herniation. Skeletal Radiol. 2003;32:364-6.
- [CrossRef] [PubMed] [Google Scholar]
- Forearm muscle herniae and their treatment. J Hand Surg Br. 1989;14:319-21.
- [CrossRef] [PubMed] [Google Scholar]
- Repair of forearm muscle herniation using local fascial flap: A case report. Cureus. 2019;11:e4881.
- [CrossRef] [Google Scholar]
- Detection of myofascial herniation on dynamic sonography and magnetic resonance imaging. Case Rep Radiol. 2016;2016:4245189.
- [CrossRef] [PubMed] [Google Scholar]
- Sonography of muscle hernias. AJR Am J Roentgenol. 2003;180:395-9.
- [CrossRef] [PubMed] [Google Scholar]
- A diagnostic approach to deltoid muscle masses. Muscles Ligaments Tendons J. 2019;9:600-5.
- [CrossRef] [Google Scholar]
- Diagnosis and management of symptomatic muscle herniation of the extremities: A retrospective review. Am J Sports Med. 2013;41:2174-80.
- [CrossRef] [PubMed] [Google Scholar]







