Translate this page into:
Enhancing stability and outcomes in young Indian footballers: The synergistic effect of anterior cruciate ligament reconstruction with lateral extra-articular tenodesis – A prospective observational cohort study
*Corresponding author: Aravind Elango Shanthini, Department of Arthroscopy and Sports Medicine, Sri Ramachandra Institute of Higher Education and Research, Ramachandra Medical College, Chennai, Tamil Nadu, India. airwind67@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Elango Shanthini A, Perumal S, Jeganathan P, Sanjay AK, Rohit KR, Mekkamannil AH, et al. Enhancing stability and outcomes in young Indian footballers: The synergistic effect of anterior cruciate ligament reconstruction with lateral extra-articular tenodesis – A prospective observational cohort study. J Arthrosc Surg Sports Med. 2025;6:58-64. doi: 10.25259/JASSM_38_2024
Abstract
Objectives:
Anterior cruciate ligament (ACL) tears are frequently seen injuries in young footballers that can contribute to chronic knee instability, meniscal injuries, and increased risk of early-onset osteoarthritis if not properly treated.
Materials and Methods:
This study evaluated the clinical findings of combined ACL reconstruction and lateral extra-articular tenodesis (LET) in 22 male footballers aged 20–30. ACL reconstruction was carried out using hamstring autografts and LET was done utilizing a modified Lemaire procedure with iliotibial band autograft. Clinical findings were studied preoperatively and at six months and one year postoperatively utilizing the International Knee Documentation Committee (IKDC) and Tegner–Lysholm scores.
Results:
Mean IKDC and Tegner-Lysholm scores were similar or slightly improved at six months compared to pre-operative baselines and further increased at one year follow-up, with the improvements being statistically significant. There are no cases of graft failure occurred.
Conclusion:
A combination of ACL reconstruction and LET is a safe and effective treatment for ACL tears in young footballers, which can restore knee stability and allow them to go back to sports. Adding LET to ACL reconstruction may help lower the likelihood of graft failure in this high-risk population.
Keywords
Anterior cruciate ligament injuries
Lateral extra-articular tenodesis
Young
Knee injury
Soccer
INTRODUCTION
Football involves multidirectional movements such as cutting, pivoting, decelerating, and rapid changes in direction, which place high translational and rotational loads on the knee.[1] The anterior cruciate ligament (ACL) is crucial for knee stability during these movements, providing restraint against anterior tibia displacement and rotational instability.[1] Disruption of the ACL can lead to knee instability, compromising the capacity of the player to perform pivoting maneuvers and increasing the chances of secondary injuries.[2]
ACL tears are one of the most frequently occurring knee injuries in footballers, with an incidence of approximately 0.15–3.7 injuries/1000 h of exposure. Young footballers are at particularly high risk, with peak incidence occurring in the second and third decades of life.[3] ACL injuries can cause significant time lost from sports participation and, if not properly treated, persistent knee instability and increased risk of osteoarthritis.[4,5] Delaying operative management for more than 12 months in ACL injuries has a very high risk of leading to medial meniscus tears.[6] Optimal management of ACL tears in young footballers is important to allow a safe return to sports and minimize knee disability in the future.[7] Reconstruction of ACL is the standard treatment option for ACL tears in active individuals.[8] However, concerns exist regarding the possibility of graft failure, especially in young patients going back to high-demand sports such as football, where a lot of pivoting activities are involved. Rates of graft failure and contralateral ACL tears of up to 20–40% have been reported in athletes under 20 years old.[9] Persistent rotatory knee laxity is thought to be a major contributor to graft failure risk. Anterolateral knee soft-tissue structures assist in restricting tibial internal rotation, and injury to these structures is usually associated with ACL rupture.[10] However, isolated ACL reconstruction fails to completely address this rotatory laxity.[11]
Lateral extra-articular tenodesis (LET) methods were developed to treat the anterolateral rotatory laxity that may exist following ACL reconstruction.[12] By providing an extra-articular constraint to tibial internal rotation, LET can unload the ACL graft and lower the likelihood of graft failure.[13] While the role of LET has been debated, recent studies have demonstrated significantly reduced graft failure rates when LET is combined with ACL reconstruction in young patients who are engaged in pivoting sports.[14] However, further studies are needed to establish the clinical findings and return to sports post-combined ACL reconstruction with LET in young footballers. The objective of this study was to assess the clinical results, return to sports, and graft failure rates in young Indian footballers undergoing combined ACL reconstruction and LET. We hypothesized that this combined reconstructive method would result in improved knee stability and function, high rates of return to football, and low graft failure rates.
MATERIALS AND METHODS
A prospective study was conducted of 22 male footballers aged 20–30 years old undergoing primary ACL reconstruction with concomitant LET from January 2020 to January 2023. All patients underwent a standardized surgical technique, post-operative rehabilitation protocol, and clinical follow-up. Pre-operative sports activity level and knee function were determined retrospectively [Figures 1-3]. The inclusion and exclusion criteria are listed in the Box below.

- Pre-operative X-ray of the right knee in standing antero-posterior view.

- (a-f) Pre-operative magnetic resonance imaging, short tau inversion recovery and T2-weighted images sagittal section showing complete tear of the anterior cruciate ligament.

- Post-operative right knee X-ray antero-posterior view of the patient showing post-anterior cruciate ligament reconstruction with lateral extra-articular tenodesis.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
ACL: Anterior cruciate ligament, PCL: Posterior cruciate ligament
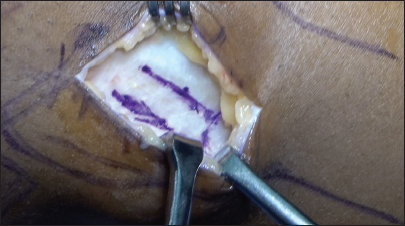
Reconstruction of ACL was done using five-strand semitendinosus-gracilis (STG) autografts. Tunnels in the femoral side were reamed through the anteromedial portal technique and tibial tunnels through a standard technique. Grafts were tensioned and fixed with extracortical endo button fixation on the femoral side and interference screw fixation on the tibial side. Post-fixation of the ACL graft LET was performed using a modified Lemaire method with a central strip of iliotibial band autograft. The graft was guided deep to the fibular collateral ligament (FCL) and proximally at the distal femoral metaphysis with suture anchors [Figure 1].[15]
Postoperatively, patients followed a structured rehabilitation plan, including early weight-bearing and range of motion as tolerated. Patients who met their rehabilitation goals were allowed to return to sports at least nine months after surgery. Clinical findings were studied preoperatively, after six months, and after one year postoperatively using the International Knee Documentation Committee (IKDC) Subjective Knee Form[16] and Tegner–Lysholm Knee Scoring Scale.[17] Graft failure and contralateral ACL tears were recorded. Paired t-tests were used to compare pre-operative and post-operative scores. Significance was set at P < 0.05. Ethical approval for the study was obtained from the Institutional Ethics Committee Review Board.
Surgical technique
Reconstruction of ACL with LET was done under general anesthesia with the patient in the supine position and a tourniquet tied around the operative thigh. Standard anterolateral and anteromedial arthroscopic portals were made. Any meniscus or cartilage injuries were addressed. After confirming the ACL tear, the ACL stump was debrided while preserving femoral and tibial footprints for anatomic tunnel placement.
STG tendons were collected through an oblique incision over the pes anserinus using an open-ended tendon stripper. The tibial insertions were left intact for eventual hamstring tendon regeneration. Tendons were quintupled and pretensioned on the graft preparation board.
An anteromedial portal approach was utilized to drill the femoral tunnel. A guidewire was positioned 5 mm anterior to the posterior wall, located between the posterolateral and anteromedial bundle imprints, with the knee in the hyper-flexed position. Once the tunnel’s length was determined, the femoral cortex was breached using a drill with a 4.5 mm diameter. Next, a reamer with the proper graft size was drilled to a depth of 25 mm. For femoral fixation, an extracortical suspensory fixation device was employed [Figures 4 and 5]. The IT band graft was left attached distally at Gerdy’s tubercle after a 1 cm wide central strip of the IT band was taken for the LET graft. To tubularize the graft, a high-strength suture was used.
- From the lateral view on the left knee, the procedure is begun with a posterolateral hockey stick incision on the left knee and exposure of the iliotibial band is performed before harvest of the graft.
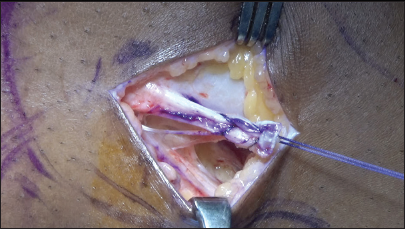
- From the lateral view on the left knee, harvest of the lateral extra-articular tenodesis graft from the iliotibial band is performed on the operative leg (left knee).
A standard ACL tibial guide, adjusted to 55°, was used to drill the tibial tunnel. After positioning a guidewire in the middle of the ACL footprint, the entire tunnel was drilled using a reamer fitted for the graft size. Using an interference screw that was 1 mm larger than the graft diameter, the ACL graft was passed through and secured in the tibial tunnel.
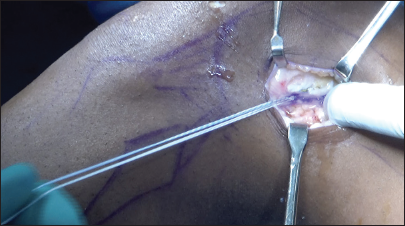
The graft was routed superficially to the lateral capsule and deeply to the FCL to facilitate LET graft transit and fixation [Figure 6]. A 5 mm suture anchor was used to secure the proximal end at the distal lateral femoral metaphysis, which is about 30 mm proximal to the lateral epicondyle [Figure 7]. The distal end was left attached to Gerdy’s tubercle. The knee was kept at 30° of flexion and neutral rotation while the fixation was performed [Figure 8].
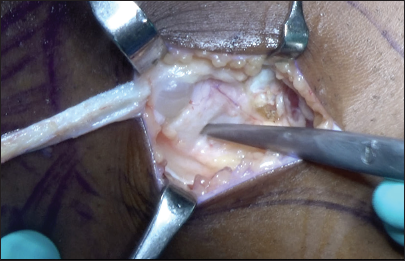
- From the lateral view on the left knee, the fibular collateral ligament has been identified and the iliotibial band graft should be passed beneath it.
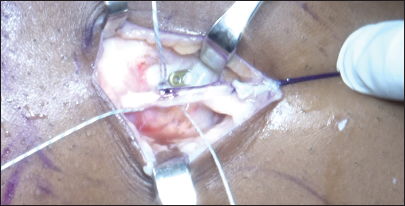
- From the lateral view on the left knee, proximal fixation of the iliotibial band graft is performed with a 2.8 mm double-loaded all-suture anchor with knee kept in neutral rotation and flexed to 20 and tension pulled on the graft, completing the lateral extra-articular tenodesis procedure.
- From the lateral view on the left knee, image shows post-anterior cruciate ligament reconstruction with lateral extra-articular tenodesis.
RESULTS
The average age of the 22 male football players in the study was 22.4 ± 3.1 years. All patients had a pre-operative diagnosis of ACL tear confirmed by magnetic resonance imaging. Meniscal repair or partial meniscectomy was used to treat six medial and five lateral meniscus tears that were concurrent injuries.
The mean pre-operative IKDC score was 48.2 ± 12.4, and the mean pre-operative Tegner–Lysholm score was 46.7 ± 10.6. At the 6-month follow-up, the mean IKDC score was 74.6 ± 9.2, and the mean Tegner–Lysholm score was 81.5 ± 8.4, representing statistically significant improvements compared to pre-operative scores (P < 0.001). Further improvements were seen at a follow-up period of one year, with a mean IKDC score of 86.2 ± 6.8 and a mean Tegner–Lysholm score of 89.4 ± 5.7 (P < 0.001 compared to preoperative and six-month scores).
By a year after surgery, all patients had regained their complete range of motion and were back playing sports [Figures 9-11]. 18/22 (82%) were able to resume playing football, similar to their pre-injury level. There were no instances of contralateral ACL tears or graft failure. Six of them had rehab-related challenges like mild stiffness and they regained their ROM a bit delayed.

- Post-operative photograph of the athlete showing achievement of full range of motion.

- Post-operative photograph of the athlete showing his ability to squat fully.

- Picture of a young footballer successfully returning to sport after undergoing anterior cruciate ligament reconstruction with lateral extra-articular tenodesis.
Paired t-tests were used in the statistical analysis to compare the pre-operative, six-month, and one year postoperative scores. The Shapiro–Wilk test was used to determine that the data were normal. At P < 0.05, statistical significance was established.
DISCUSSION
This study shows that, during one year follow-up, young football players who received both ACL reconstruction and LET had outstanding clinical outcomes. High rates of return to football and no instances of graft failure were observed, along with notable improvements in knee function and sports activity level.
With rates of graft rupture and contralateral ACL tear of 20–40% in athletes under 20, treating ACL tears in young athletes is difficult since this population is at high risk for recurrent instability and graft failure.[18] The cause of this high failure rate is likely multifactorial, with contributing factors including higher activity level, stronger quadriceps, narrower intercondylar notch, and increased joint laxity.[19] However, persistent rotatory instability due to concomitant anterolateral soft-tissue injury is increasingly recognized as an important factor.[9]
Historically, the gold standard for treating ACL rupture was thought to be isolated intra-articular reconstruction.[20] Nevertheless, new research indicates that, particularly in individuals with high-grade rotatory laxity, ACL restoration alone might not be adequate to return knee kinematics to normal and shield the knee from recurrent bouts of instability [Table 1].[21,22] LET helps treat the rotational component of instability and safeguards the ACL graft by supplying an extra-articular constraint to tibial internal rotation.[17]
| Procedure | Advantages | Disadvantages |
|---|---|---|
| Isolated ACL reconstruction | Well-established and widely accepted technique | Does not address rotational stability and increased strain on the graft |
| ACL reconstruction with LET | Allows for anatomic graft placement Avoids additional surgical dissection and hardware Provides additional rotational stability Reduced risk of residual pivot-shift phenomenon Decreased strain on the ACL graft Theoretical reduced risk of graft failure and re-rupture |
Higher risk of residual pivot-shift phenomenon Potential for graft failure and re-rupture More invasive and technically demanding procedure Potential for over-constraint and loss of knee range of motion Increased surgical time and complications Additional hardware (e.g., bone staples, screws) required |
ACL: Anterior cruciate ligament, LET: Lateral extra-articular tenodesis
When LET is used with ACL restoration in young patients who play pivoting sports, there is a lower rate of graft failure, according to several clinical studies. According to a comprehensive study by Hewison et al., individuals under 30 who underwent ACL surgery with LET in addition had a 2.5 times reduced risk of graft rupture than those who underwent ACL reconstruction alone.[23] At a two-year follow-up, the STABILITY research, which randomized 624 patients to ACL reconstruction with or without LET, discovered a substantial decrease in graft failure (4% vs. 11%) in the LET group.[14]
The current study’s results, which show great outcomes with combined ACL restoration and LET in a high-risk cohort of young male football players, are consistent with these earlier reports. Within a year after surgery, 82% of patients had recovered to their pre-injury football level, with no occurrences of graft failure.
This study’s prospective design, standardized surgical method, established rehabilitation plan, and utilization of verified patient-reported outcome measures are its strong points. Some of the limitations are the relatively brief one year follow-up period and the absence of a control group undergoing isolated ACL reconstruction. To find if adding LET to isolated ACL surgery leads to better clinical outcomes and lower graft failure rates, larger comparative studies with more long-term follow-up are required.
Limitations
The main limitation of the study is a smaller sample size because the participants included in the study were only elite footballers playing in the state and national leagues. Hence, its findings cannot be generalized to other population groups.
CONCLUSION
ACL reconstruction, along with LET, is a safe and effective treatment for tears of the ACL in young footballers, resulting in excellent clinical findings, higher rates of return to sports and low rates of graft failure at 1-year follow-up.
The addition of LET helps address rotational knee laxity and may protect the ACL graft from excessive forces during the ligamentization process and reduce the chances of graft failure or retear in athletes participating in pivoting sports.
Author contributions
AES, SP, PJ, AKS, AS, KRR, AHM: Contributed significantly to the study and preparation, review, and final approval of this manuscript.
Ethical approval
The research/study was approved by the Institutional Ethics Committee at Sri Ramachandra Institute of Higher Education and Research, Ramachandra Medical College, number 78/24, dated October 15, 2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573-8.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2016;44:1861-76.
- [CrossRef] [PubMed] [Google Scholar]
- ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139:e20161877.
- [CrossRef] [PubMed] [Google Scholar]
- The role of ACL injury in the development of posttraumatic knee osteoarthritis. Clin Sports Med. 2013;32:1-12.
- [CrossRef] [PubMed] [Google Scholar]
- Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: Is there harm in delay of treatment? Am J Sports Med. 2011;39:2582-7.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for meniscal tears: A systematic review including meta-analysis. J Orthop Sports Phys Ther. 2013;43:352-67.
- [CrossRef] [PubMed] [Google Scholar]
- Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis. Arthrosc Tech. 2019;8:e855-9.
- [CrossRef] [PubMed] [Google Scholar]
- 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42:675-80.
- [CrossRef] [PubMed] [Google Scholar]
- Complications after pediatric ACL reconstruction: A meta-analysis. J Pediatr Orthop. 2019;39:e566-71.
- [CrossRef] [PubMed] [Google Scholar]
- The anterolateral ligament: An anatomic, radiographic, and biomechanical analysis. Am J Sports Med. 2015;43:1606-15.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical comparison of anterolateral ligament anatomical reconstruction with a semi-anatomical lateral extra-articular tenodesis. A cadaveric study. Knee. 2019;26:1003-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of rotatory knee instability. J Exp Orthop. 2019;6:48.
- [CrossRef] [PubMed] [Google Scholar]
- Anterolateral knee extra-articular stabilizers: A robotic study comparing anterolateral ligament reconstruction and modified lemaire lateral extra-articular tenodesis. Am J Sports Med. 2018;46:607-16.
- [CrossRef] [Google Scholar]
- Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med. 2020;48:285-97.
- [CrossRef] [PubMed] [Google Scholar]
- Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis in skeletally immature patients: Surgical technique. Arthrosc Tech. 2020;9:e897-903.
- [CrossRef] [PubMed] [Google Scholar]
- The International Knee Documentation Committee (IKDC) subjective short form: A validity and reliability study. Knee Surg Sports Traumatol Arthrosc. 2015;23:3163-7.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for early ACL reconstruction failure in pediatric and adolescent patients: A review of 561 cases. J Pediatr Orthop. 2018;38:388-92.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for anterior cruciate ligament graft failure in professional athletes: An analysis of 342 patients with a mean follow-up of 100 months from the SANTI study group. Am J Sports Med. 2022;50:3218-27.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction in skeletally immature patients: Early results using a hybrid physeal-sparing technique. Orthop J Sports Med. 2018;6:23-25.
- [CrossRef] [PubMed] [Google Scholar]
- Allograft and autograft transphyseal anterior cruciate ligament reconstruction in skeletally immature patients: Outcomes and complications. Arthroscopy. 2016;32:860-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament-deficient knee. J Orthop Traumatol. 2017;18:91-106.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: A systematic review of the literature. Arthroscopy. 2015;31:2022-34.
- [CrossRef] [PubMed] [Google Scholar]







