Translate this page into:
Femoral notch and proximal tibial morphology and their relationship with an anterior cruciate ligament injury in the Indian population: A magnetic resonance imaging-based study

*Corresponding author: K. Yogesh, Department of Orthopaedics, Tejasvini Hospital, Kadri, Mangalore, Karnataka, India. yogiortho@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Huggi V, Yogesh K, Jacob G, Pai S, Kumar A, Arya S. Femoral notch and proximal tibial morphology and their relationship with an anterior cruciate ligament injury in the Indian population: A magnetic resonance imaging-based study. J Arthrosc Surg Sports Med 2020;1(2):193-8.
Abstract
Objectives:
We aim to study the incidence of anterior cruciate ligament (ACL) injury to proximal tibia bone morphology in Indian patients.
Materials and Methods:
Forty male subjects who sustained non-contact ACL injury who presented to our center between October 2015 and December 2016 studied and compared to 40 non-ACL injury knee magnetic resonance imaging scans. Notch morphology and both medial and lateral posterior tibial slope measurements were performed and studied.
Results:
We noted that the difference in notch depth and notch angle between the two groups was not significant. There was a statistically significant higher incidence of ACL injury in patients with smaller notch widths. Both an increased medial and lateral posterior tibial slope did not demonstrate a statistically significant incidence in ACL injury.
Conclusion:
Notch width is a major contributing risk factor for ACL injury in Indian patients. This is in agreement with previously published literature.
Keywords
Anterior cruciate ligament injury
Tibia morphology
Tibial slope
Tibial notch
Anterior cruciate ligament
INTRODUCTION
The anterior cruciate ligament (ACL) is a key stabilizer of the knee joint which opposes anterior tibial translation and internal rotation. ACL injuries are most common ligament injuries in the knee joint and cause significant disability in both the athletic and the general population. These injuries have also been known to predispose to early knee joint osteoarthritis in spite of reconstructive surgery.[1-3] For this reason, considerable literature and research have focused on determining the several possible risk factors that predispose a patients toward an ACL injury.[4-6]
Research has revealed that ACL injuries have numerous possible risk factors ranging from the nature of sports, limb alignment, hormonal variation, neuromuscular variations, and anatomic variations in knee joint morphology.[7,8] The aim of such research is to identify high-risk patients to develop preventative strategies reducing the occurrence or recurrence of an ACL injury. Our study focuses on the measurements of the femoral and tibial bony morphology in ACL injured patients in the Indian population to identify any anatomic bony variables and its variations with published literature.
MATERIALS AND METHODS
With ethical committee clearance, we performed a prospective case–control study to assess the bony knee morphology of patients who sustained an ACL injury. The inclusion criteria of our study were male patients between the ages of 20 and 50 years old who sustained non-contact ACL injury with a body mass index under 25 kg/m2 proven by magnetic resonance imaging (MRI). All subjects in the study were not sports persons and participated only in occasional recreational activities. We included patients who presented to our center between October 2015 and December 2016. The bony measurements of these patients were compared against 40 control MRI scans. Control MRI scans were those performed in patients with knee joint pathologies not associated with a ligamentous injury such as meniscal lesions, osteochondral lesions, or injuries which on MRI were not detected. Patients with contact injuries, mucoid degeneration of the ACL, or osteotomies around the knee were not excluded from the study.
MRI technique
According to standard procedure at our institution, the MRI scan was performed with the knee join in 10 degrees of flexion. The section of the notch, seen at the level of the popliteal groove in the lateral femoral condyle, was identified in the axial images to measure the notch morphology parameters. The sagittal knee sequence was used to measure the posterior medial tibial slope (PTMS) and posterior lateral tibial slope (PTLS) was measured. The MRI examinations were performed on Siemens 1.5 T using a quad coil.
Notch morphology
The axial image which demonstrated the largest area of the popliteal groove was used to measure the notch morphologic parameters. Notch outlines were divided into three types as described by Van Eck et al.[9]
Type A: Tapering apex
Type U: Less tapered notch with a larger angle when compared to Type A
Type W: Notch has two apices.
Notch measurement
The notch morphological measurements were performed, as described by Stein et al.[10] [Figure 1] illustrates the methodology we used for measuring the femoral notch morphology.
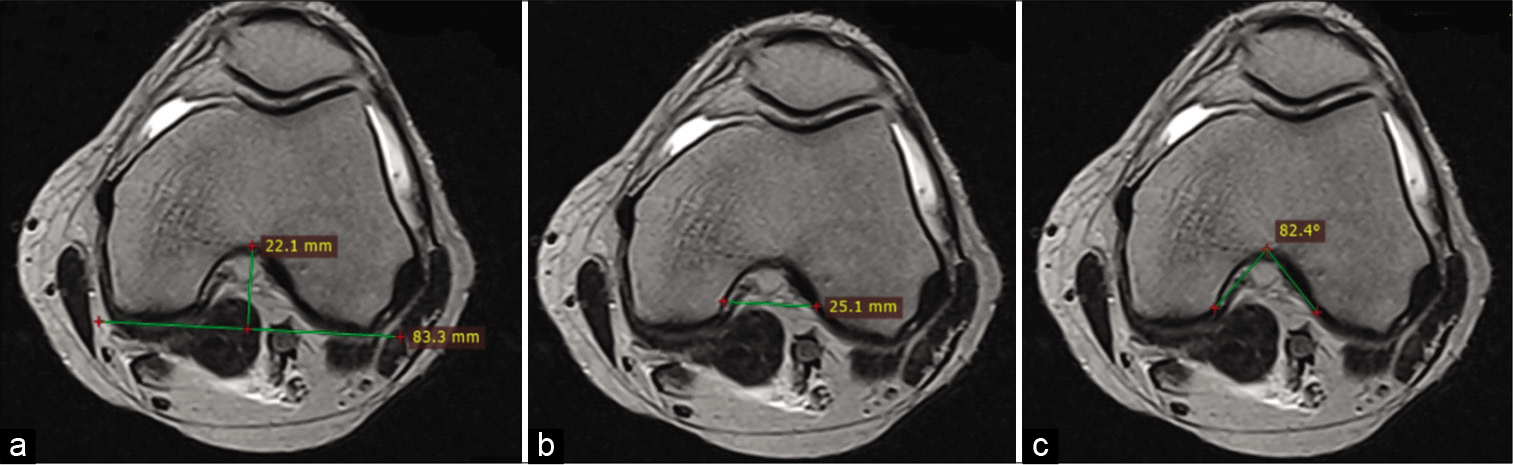
- Illustrating the method used to measure (a) notch depth, (b) notch width, (c) notch.
Notch depth was measured between the highest point of the notch apex to the posterior bicondylar line of the distal femur
Notch width was determined between the medial projection of lateral condyle and lateral projection of medial condyle at two-third of the notch depth
The notch angle was determined in the axial sequence by a line drawn from the superior most aspect of the notch to the inferior most aspect of the notch on the medial and lateral condyle.
Measurement of posterior tibial slopes
We developed our own technique for measuring the posterior tibial slope on MRI as determining the long axis of the limb was not possible in the regular MRI sequence window, which is possible in a computer tomography (CT) scan. To overcome this, we performed our measurements in the following sequence. In the axial view, the sequence demonstrating the largest femoral popliteal groove was utilized as the scout image, next the corresponding coronal MRI image was used to define the midpoint of the medial and lateral articular surface. This was measured from the medial most point of the medial femoral condyle to the medial most part of the medial tibial spine and similarly in the lateral compartment, the lateral most aspect of the lateral tibial plateau to the lateral most point of the lateral tibial spine. Next, the corresponding sagittal image of both the mid articulating points of the medial and lateral compartments was used to measure the posterior tibial slope. Next, the posterior tibial slope was determined by drawing a vertical line over the anterior most part of the tibial cortex and then a second line connecting the peak anterior and posterior points on the tibial plateau in both the medial and lateral compartments. The angle formed between the two lines was determined and recorded is the tibial slope. [Figure 2] illustrates the methodology we used for determining the posterior tibial slope.
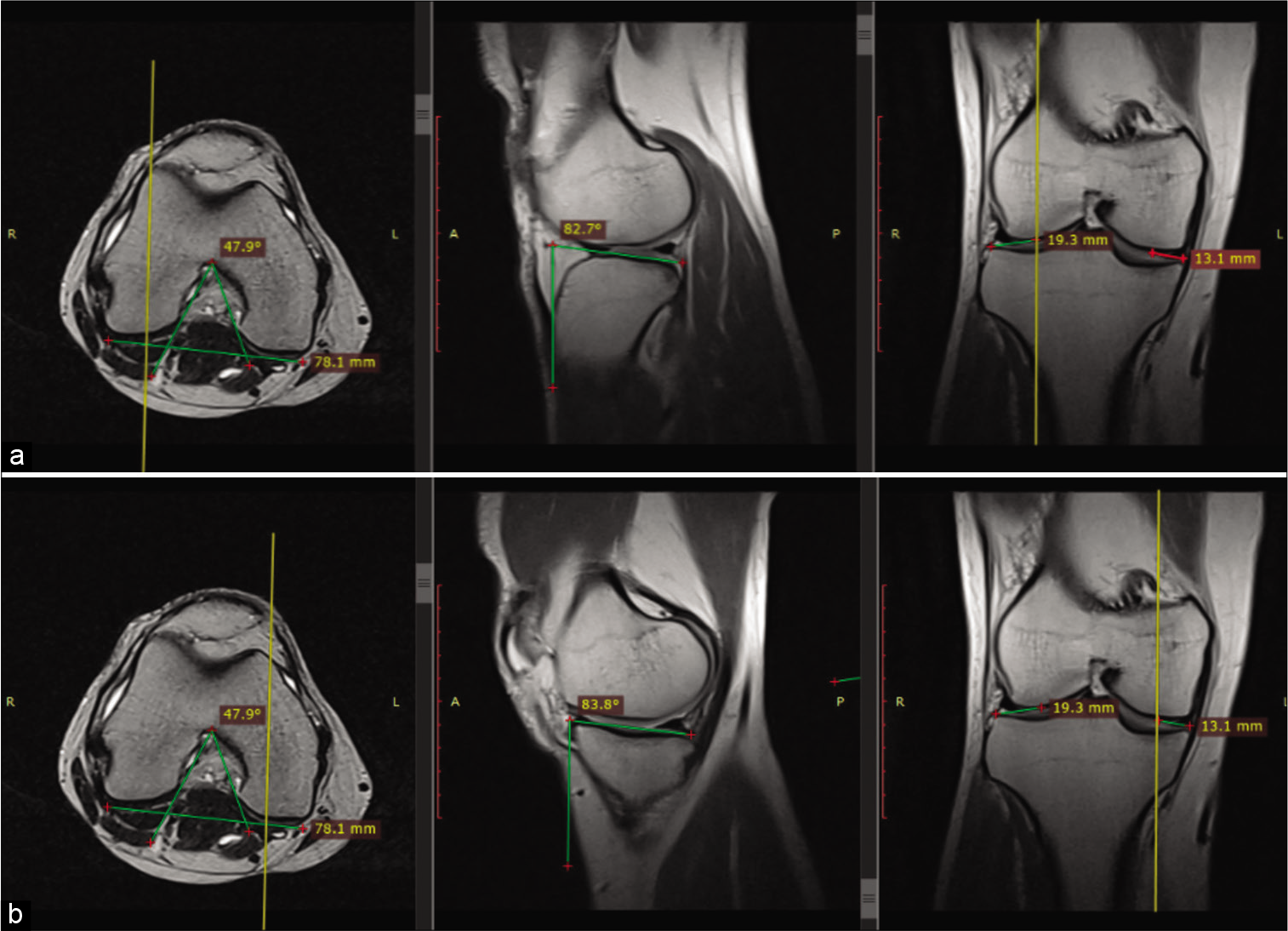
- Illustrating the method used to measure (a) posterior tibial slope in the lateral compartment (b) posterior tibial slope in the medial compartment.
Statistical methods
All the measurements were performed 3 times by a single observer using RadiAnt DICOM viewer 3.4.1. Statistical analysis was done using Student’s unpaired t-test using SSPS software.
RESULTS
A total of 80 male patients (40 ACL injury and 40 nonACL injury) MRI scans were analyzed and the notch morphology and tibial slopes measured in each case. The mean age of ACL injured group was 32.98 (range 20–50) years and the non-ACL injured group was 34.23 (range 20–49) years [Table 1].
| ACL injury | n | Mean | Std. deviation | t | DF | P-value | |
|---|---|---|---|---|---|---|---|
| Age | Present | 40 | 32.98 | 8.16 | –0.692 | 78 | 0.491* |
| Absent | 40 | 34.23 | 7.995 | ||||
| Depth | Present | 40 | 35.51 | 6.155373 | 1.917 | 78 | 0.059* |
| Absent | 40 | 33.3825 | 3.375469 | ||||
| ngle | Present | 40 | 46.8875 | 6.087406 | –0.903 | 78 | 0.369* |
| Absent | 40 | 48.335 | 8.112243 | ||||
| Width | Present | 40 | 22.335 | 2.87737 | –2.241 | 78 | 0.028** |
| Absent | 40 | 23.7525 | 2.779134 | ||||
| PTMS | Present | 40 | 8.4875 | 3.856276 | 1.048 | 78 | 0.298* |
| Absent | 40 | 7.54 | 4.219053 | ||||
| PTLS | Present | 40 | 8.2475 | 3.906273 | 1.07 | 78 | 0.288* |
| Absent | 40 | 7.3075 | 3.953991 |
Notch shape
There were 35 Type A, 33 Type U, and 12 Type W notches in the total 80 studied patients [Figure 3]. Out of 40 patients in ACL injured group, 19 patients had a type A notch, 15 a type U, and 6 a Type W. There was a higher incidence of type U notches in the control group of patients when compared to the ACL injury group.
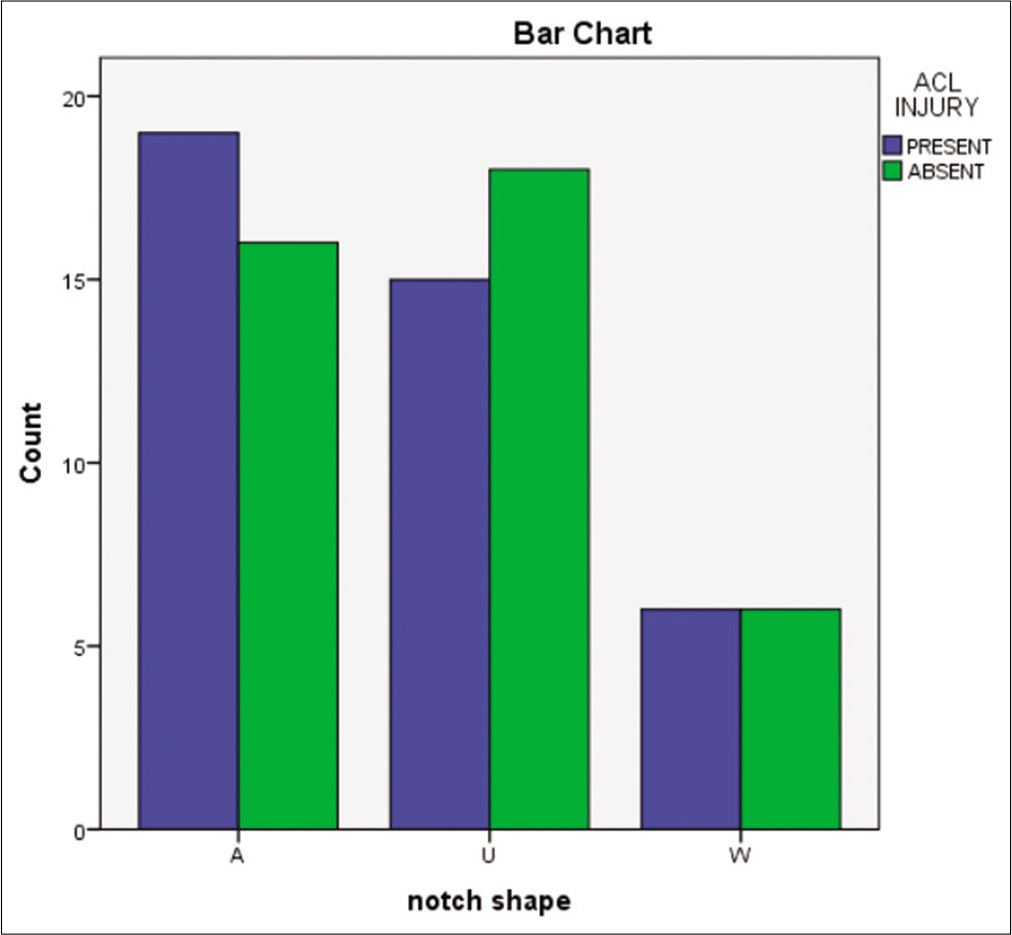
- Graph demonstrating the number of each notch shape included in our study.
Notch depth
In the ACL injury group, the average notch depth was measured to be 35.51 ± 6.1 mm and the non-injured group was 33.38 ± 3.37 mm. The difference in notch depth between the two groups was not found to be significant (P > 0.05).
Notch angle
The mean measured notch angle in the ACL injury group was 46.88 ± 6° in the ACL injury and 48.35 ± 8.11° in the non-injury group. There was no statistical significance when comparing both groups (P > 0.05).
Notch width
The mean notch width was 22.33 ± 2.8 mm in the study group and 23.77 ± 2.77 mm in the non-injured group. When comparing the two groups, there was a statistically significant difference in that the ACL injured groups had smaller notch widths (P < 0.05).
PTMS
The mean PTMS in the ACL injured group was 8.48±3.8° and non-injured group was 7.54 ± 4.2°. On comparison, though the mean PTMS was higher in the study group, it was not found to be statistically significant (P > 0.298).
PTLS
The mean PTLS in the ACL injured group was 8.24 ± 3.9°, whereas in the non-ACL injured group, the mean PTLS was 7.3 ± 3.95° in the non-injury group. The mean PTLS was higher in the ACL injured group however was not found to be statistically significant (P > 0.288).
DISCUSSION
As ACL injuries are common injuries causing considerable disability with a high socioeconomic burden in all parts of the population,[11] it is well worth studying the risk factors that predispose patients to an ACL injury. Multiple risk factors have been reported, for example, female sex, ligament laxity, hormonal changes, and even specified sporting activities.[7,12] Arthroscopy and ACL reconstructive techniques have improved significantly overtime with various implants and techniques being developed for an improved ligament reconstruction, however, due bone morphology some patients result in retears of the reconstructed graft.[13] Therefore, it is important to note the bony morphologies that predispose to a primary ACL injury as well as more importantly identifying patients who are susceptible for another tear which would make our observations more clinically applicable.
In our study, we noted that the mean femoral notch width in the ACL injury group was smaller than that of the non-ACL injury group and the difference between the two groups was statistically significant. This indicates that narrower notch width could be the principal risk factor for an ACL injury. This is a well-studied parameter and our results are comparable with published literature.[14-17] It is thought that a narrower notch results in greater degrees of impingement of the ACL along with a higher incidence of a mucoid hypertrophy. Both the notch width and depth did not correlate a higher incidence of ACL injury. Literature has reported that a notch angle <50° was a significant risk factor for ACL injury.[18,19] We did not note similar findings and found that despite measuring a lower mean notch angle in the ACL injury group, it was not significantly reduced when compared to the non-injured group. Studies have classified femoral notches into different shapes. These include Type A, U and W of which Type A was found to be the most common type of femoral notch morphology. Reports suggested that Type A notches had a higher incidence of ACL injury, however, in our study results, we did not a statistically significant incidence of Type A notches in the ACL injury group.[20] Notch morphology and shape have also been thought to affect surgical technique where visualization of the lateral aspect notch through a standard anteromedial arthroscopy portal may be difficult in tapering stenotic notches as seen in Type A.[21]
Posterior tibial slope angles have also been considered a significant risk factor for ACL injury, especially during compressive axial loading, where it results in increased anterior tibial translation.[22] More recently, studies have evaluated medial and lateral posterior tibial slopes to determine which of the two contributes to increase ACL injury predisposition. Our results suggested that there was no significant relationship between the medial and lateral posterior tibial slope and ACL injury. Our findings are in agreement with other literature[16,23] but also contrary to a few studies that have shown significance in the medial posterior tibial slope and others in the lateral posterior tibial slope and ACL injury.[24-26] Since the results of posterior tibial slope angle and ACL injury are not uniform, it is worth considering the variations in measurement techniques in each study. Defining the midpoint of the medial and lateral compartment is challenging as well as determining which MRI sequence to use. Standardization techniques using fixed bony landmarks to define image sequences or sections for subsequent measurements are used and therefore there is a vast amount of possible interobserver variability. This could be the reason for many different study outcomes. There is enough biomechanical evidence and sound theory in that an increased posterior tibial slope would allow for further anterior tibial translation adding more stress on the ACL.[27,28]
The importance of these measurements in patients with an ACL injury is the increased risk factors predisposing the patient for a reinjury of the ACL. It also gives an indication to the surgeon and patient for the chance of a contralateral knee ACL injury in view of similar bony knee morphology. MRI is also the preferred radiographic investigation for knee pathologies therefore using MRI for measurement reduces the need for an additional investigation therefore more economical.
We do recognize that our study has limitations, and this may affect our findings. We only had one observer perform measurements and our sample size was limited. In addition, the use of CT scan would have allowed for the accurate determination of the long axis of the tibia, however. We wanted to avoid the additional cost and radiation to the patient.
CONCLUSION
Femoral notch width is the most significant risk factor for ACL injury in the Indian population. Though our results did not show increased proximal tibial slope angles to be a significant risk factor, we did note higher slope angles in the ACL injury group and an increased sample size may have resulted in a significant finding.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Anterior cruciate ligament injuries in young athletes, Recommendations for treatment and rehabilitation. Sport Med. 1995;20:117-27.
- [CrossRef] [PubMed] [Google Scholar]
- Fate of the ACL-injured patient: A prospective outcome study. In: Classic Papers in Orthopaedics. London: Springer; 2014. p. :149-52.
- [CrossRef] [Google Scholar]
- Osteoarthritis after anterior cruciate ligament reconstruction: The importance of regaining and maintaining full range of motion. Sports Health. 2012;4:79-85.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of ACL injury, Part I: Injury characteristics, risk factors, and loading mechanism. Res Sports Med. 2012;20:180-97.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;41:i47-51.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part. 2 A review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17:859-79.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for anterior cruciate ligament injury: A review of the literature-Part 1: Neuromuscular and anatomic risk. Sports Health. 2012;4:69-78.
- [CrossRef] [Google Scholar]
- The influence of tibial and femoral bone morphology on knee kinematics in the anterior cruciate ligament injured knee. Clin Sports Med. 2018;37:127-36.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral intercondylar notch shape and dimensions in ACL-injured patients. Knee Surg Sports Traumatol Arthrosc. 2010;18:1257-62.
- [CrossRef] [PubMed] [Google Scholar]
- The relation of femoral notch stenosis to ACL tears in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2010;18:192-9.
- [CrossRef] [PubMed] [Google Scholar]
- Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95:1751-9.
- [CrossRef] [PubMed] [Google Scholar]
- Management of anterior cruciate ligament injury: What's in and what's out? Indian J Orthop. 2017;51:563-75.
- [CrossRef] [PubMed] [Google Scholar]
- Underappreciated factors to consider in revision anterior cruciate ligament reconstruction: A current concepts review. Orthop J Sports Med. 2018;6:2325967117751689.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. J Bone Joint Surg Br. 2011;93:1475-8.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for anterior cruciate ligament injury in skeletally immature patients: Analysis of intercondylar notch width using magnetic resonance imaging. Int Orthop. 2010;34:703-7.
- [CrossRef] [PubMed] [Google Scholar]
- A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43:1702-7.
- [CrossRef] [PubMed] [Google Scholar]
- The importance of the intercondylar notch in anterior cruciate ligament tears. Orthop J Sports Med. 2015;3:2325967115597882.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of the intercondylar notch by computed tomography. Am J Sports Med. 1987;15:547-52.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between mucoid hypertrophy of the anterior cruciate ligament (ACL) and morphologic change of the intercondylar notch: MRI and arthroscopy correlation. Skeletal Radiol. 2008;37:821-6.
- [CrossRef] [PubMed] [Google Scholar]
- Association of femoral intercondylar notch morphology, width index and the risk of anterior cruciate ligament injury. Knee Surg Sport Traumatol Arthrosc. 2013;21:678-82.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of intercondylar notch shape and size on the treatment algorithm for anatomic anterior cruciate ligament reconstruction. Oper Tech Orthop. 2017;27:27-32.
- [CrossRef] [Google Scholar]
- Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br. 1994;76:745-9.
- [CrossRef] [PubMed] [Google Scholar]
- Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467:2066-72.
- [CrossRef] [PubMed] [Google Scholar]
- Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16:112-7.
- [CrossRef] [PubMed] [Google Scholar]
- Shallow medial tibial plateau and steep medial and lateral tibial slopes: New risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38:54-62.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for anterior cruciate ligament injury: Assessment of tibial plateau anatomic variables on conventional MRI using a new combined method. Int Orthop. 2011;35:1251-6.
- [CrossRef] [PubMed] [Google Scholar]
- Noncontact anterior cruciate ligament injuries: Mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18:520-7.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376-82.
- [CrossRef] [PubMed] [Google Scholar]






