Translate this page into:
Fluoroscope-assisted arthroscopic retroarticular drilling for osteochondral lesions of talus with bone grafting – Clinical outcome analysis and review of literature

*Corresponding author: Santosh K. Sahanand, Department of Arthroscopy and Sports Medicine, OrthoOne Orthopaedic Speciality Center, Coimbatore, Tamil Nadu, India. sahanand@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ashraf M, Duraiswamy G, Sahanand SK, Rajan DV. Fluoroscope-assisted arthroscopic retroarticular drilling for osteochondral lesions of talus with bone grafting – Clinical outcome analysis and review of literature. J Arthrosc Surg Sports Med 2020;1(2):186-92.
Abstract
Objectives:
Early stages of osteochondral lesions with or without cystic changes are amenable to revitalization and cartilage restoration. In these cases, we assess the outcome using our standard technique and by eliminating the need for malleolar osteotomy.
Materials and Methods:
Seven cases of osteochondral lesion of talus were treated with retroarticular drilling under arthroscopy and fluoroscopy assistance. These cases were followed up for a minimum of 6 months (mean 20 ± 12.53 months). The functional outcome was assessed using American Orthopedic Foot and Ankle Score (AOFAS) hindfoot score.
Results:
The AOFAS increased from 49.28 (±6.7) points to 85 (±9.12) points and was noted to be statistically significant (P < 0.001). 2/7 ankles were lateral sided lesion and had a history of trauma. 6/7 cases had an intact intraoperative cartilage status, whereas one case had Grade C (fissures and fibrillation). However, the location of lesion or the grade of lesion did not influence the results.
Conclusion:
This treatment modality seems to be a feasible option for early lesions and can be considered before alternative cartilage replacement treatment strategies are employed.
Keywords
Osteochondral lesion
Talus
Drilling
Bone grafting
Ankle arthroscopy
INTRODUCTION
A painful ankle is often restricting mobility and is debilitating. Symptomatic osteochondral lesions of talus (OLT) are one such cause of intractable ankle pain. The reported incidence of OLT is 0.09% and a prevalence of 0.002/100,000 person/year.[1] Although the lesion affects every age group, it is frequently seen in the second decade of life.[2] Initially, it was hypothesized to be of traumatic etiology but later it was also associated with atraumatic lesions, the etiology still remains inconclusive. Berndt in 1959 had demonstrated the occurrence of OLT lesion in their experimental study. They had also classified the lesion based on the characteristics of the lesion. This classification is wide popular and still in use.[3] However, with time, better imaging techniques have evolved, and at present, the lesions can be classified based on CT, magnetic resonance imaging (MRI), and also intraoperatively using arthroscope.[4-6] Treatment of these lesions has been reported extensively previously, but as stated by Dahmen et al.; none is superior over the other considering the variety of presentation of these lesions.[7] A lesion-specific approach needs to be tread while treating these cases. In this cases series, we report on the early chondral lesions with and without cystic changes. These cases were operated with retroarticular drilling and autologous bone grafting. Retroarticular drilling is a technique of cartilage repair that avoids damage to the articular cartilage. This is based on the principle of operative technique described by Wagner[8] and Conti and Taranow.[9] We report the clinical outcome analysis of these cases with review of literature pertaining to arthroscope-assisted retroarticular drilling of talus under fluoroscopy guidance. Furthermore, the operative technique employed in our case series is illustratively described.
MATERIALS AND METHODS
Institutional Review Board approval was sought for the study. The study was a review of case records of patients between January 2016 and December 2019 who were diagnosed with osteochondral lesion of the talus and were treated with arthroscope-assisted retroarticular drilling and autologous cancellous bone grafting. The diagnosis of these cases was established preoperatively by plain radiographs and confirmed by MRI. Intraoperatively, the lesions were classified using the arthroscopic classification by Cheng et al. Clinical outcome analysis was performed using the American Orthopedic Foot and Ankle Society-Ankle-Hindfoot Score (AFOS) which was used preoperatively and postoperatively.[10] All cases were followed up for a minimum of 6 months. The exclusion criteria of the study were those patients who had Grade IV Berndt and Harty and prior treatment with cartilage replacement or cartilage regeneration techniques. The review of literature was performed in the following databases PubMed and Google Scholar. The keywords used were retroarticular drilling, osteochondral lesion of talus, and bone grafting.
Statistical analysis
Statistics of descriptive data was calculated by standard formulas (arithmetic mean, standard deviation, range, and frequency). All continuous variables are presented in terms of mean ± standard deviation of the mean. Comparison between paired data and independent groups was performed using the Student’s t-test. P < 0.05 was regarded as statistically significant. Statistical analysis was performed using the SPSS ver 10.0 software package.
Operative technique
Under spinal anesthesia with patient in supine position, the index limb is placed on a well-padded thigh support at an angle 45° and the ankle is placed in a non-invasive external distraction device. Adequate traction will distract the tibia talar joint [Figure 1]
Proper portal placement is critical to perform an accurate diagnostic examination of the ankle. The anteromedial portal which is the viewing portal is established between tibialis anterior and saphenous vein
The anterolateral portal is established between peroneus tertius and lateral malleolus. The superficial peroneal nerve may intervene between the landmarks and can be avoided by directing the light source to illuminate the portal area to trace the nerve before incision
A probe is used to assess the extent, depth of the lesion, and also the status articular cartilage For medial sided lesions, a small stab incision is made over the sinus tarsi and under fluoroscopic guidance a guide wire is passed starting from the non-articular part of the sinus tarsi and directed toward the lesion at the talar dome
For lateral sided lesions, a small stab incision 1 cm below the medial malleoli and parallel to the deltoid fibers is performed and the guide wire is passed toward the lesion
The direction of the guide wire toward the lesion is confirmed with both anteroposterior and lateral view
The guide wire is slowly advanced up to the sclerotic rim of the osteochondral lesion such that it does not perforate the articular cartilage [Figure 2]
This step is vital and needs to be monitored under arthroscopy
In all the cases, 4.5 mm cannulated drill is used over the guide wire and reamed up to the osteochondral lesion [Figure 3]. The reamer is then removed keeping the guide pin in situ
Cancellous bone graft plugs harvested from proximal tibial metaphysis using the OATS donor harvester handle [Figures 4 and 5]. The grafts are then placed through the tunnel and impacted up to the base of the lesion using a long trocar under arthroscopic vision. Two to three cylinders of corticocancellous bone graft were harvested for all the cases
The graft is impacted such that it does not perforate the articular cartilage and does not exceed the base of base of the articular cartilage at the rim of the lesion [Figure 6].
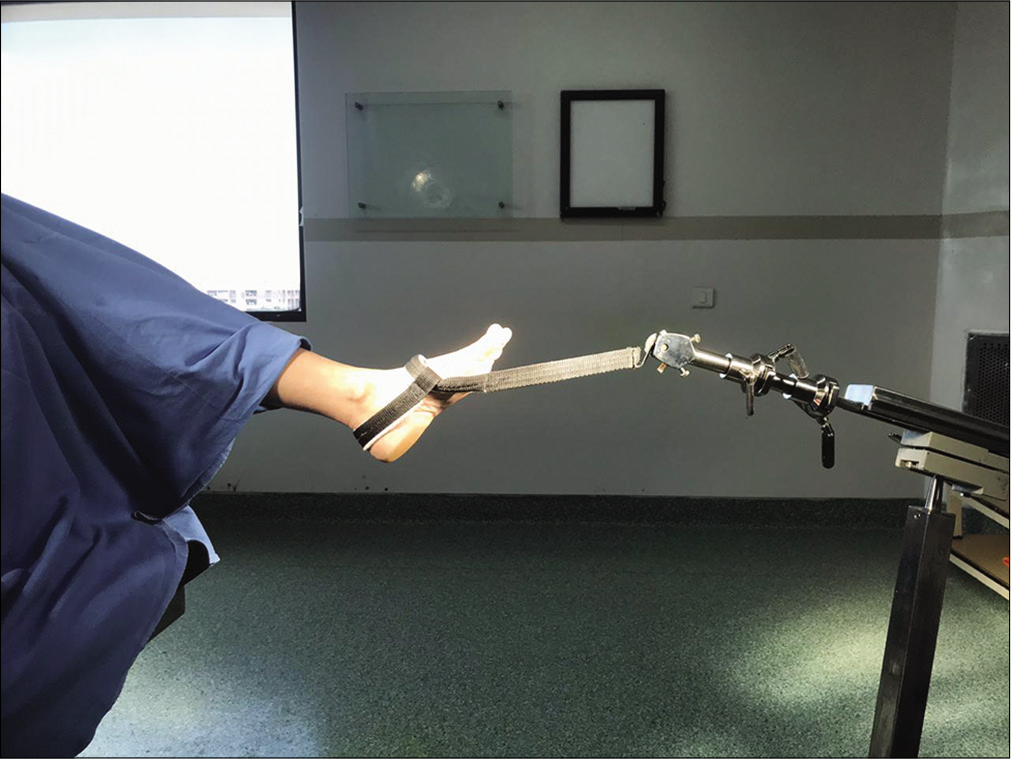
- Ankle distraction for arthroscopy.
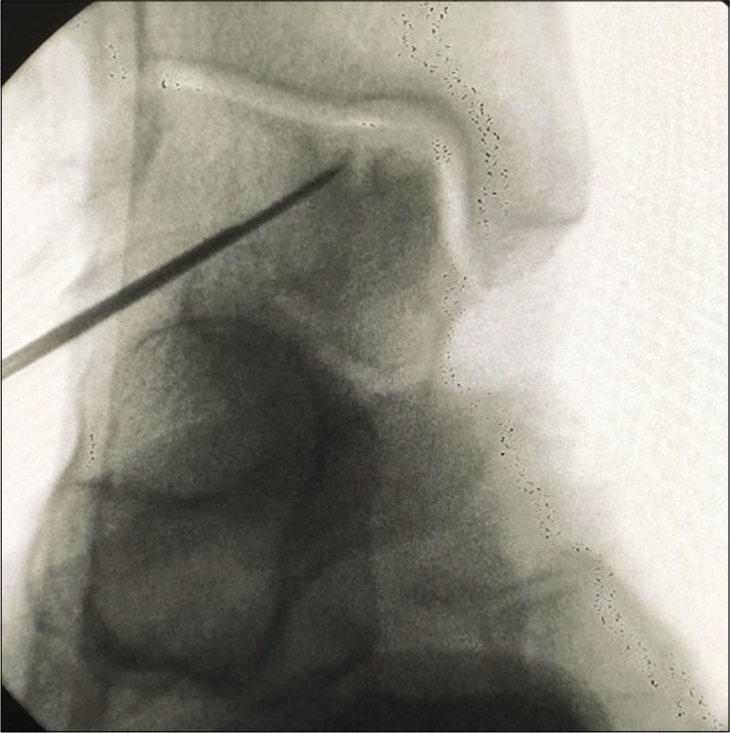
- Guide pin passage toward the lesion under fluoroscopic guidance.
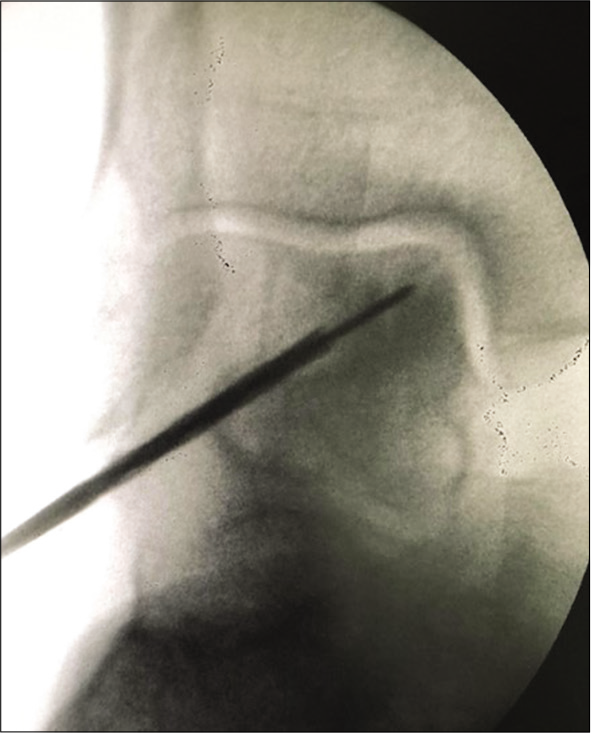
- Six millimeters cannulated drill passed over the guide pinretroarticular drilling.
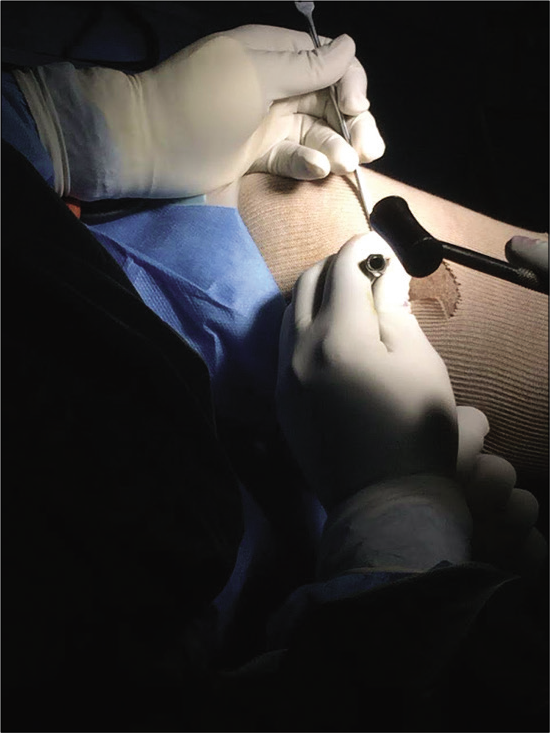
- Harvesting cancellous graft from ipsilateral proximal using OATS bone harvest handle.

- Harvested autologous cancellous bone plugs.

- Impaction of bone graft after retroarticular drilling.
Post-operative rehabilitation
In the immediate post-operative period, the patient is kept non-weight-bearing for 6 weeks
However, range of motion exercises (dorsiflexion and plantar flexion) as tolerated was initiated from day 2 onwards
Inversion and eversion movements were initiated at the end of the 4th week
Encourage to achieve full weight-bearing by 6–8 weeks
As a precaution, the patients were advised to avoid high impact activities for at least 6 weeks.
RESULTS
The mean age at presentation was 48 years (±9.8 years). A total of eight ankles with talar OCD were identified. One case was excluded as it was diagnosed to be Berndt and Harty Stage IV lesion. The mean follow-up duration was for 20 (±12.53) months and all the cases were followed for a minimum of 6 months. Out of the seven cases, four were male and three were female. There was a history of trauma in three out of the seven cases (3/7). Two out of seven (2/7) were lateral sided lesions and five out of seven (5/7) were medial sided lesions. Both the lateral sided lesion had a history of trauma. Pre-operative radiograph classification was performed with Berndt classification. All seven ankles (7/7) were Grade 2 lesions, assessed by two independent orthopedic surgeons. The pre-operative MRI staging was performed using the Hepple’s classification and summarized in [Table 1] along with the intraoperative staging as devised by Cheng et al. The mean pre-operative AOFAS hindfoot score was 49.28 (±6.7) points and the mean post-operative AOFAS hindfoot score at 6 months follow-up was 85 (±9.12) points [Figure 7]. This difference was statistically significant with a P < 0.001 (P < 0.001, t-test). All the patients showed an intact cartilage status preoperatively as well as intraoperatively.
| Pre-operative plain radiographic Berndt and Harty classification[3] | Pre-operative MRI Hepple classification[5] | Intraoperative arthroscopic Cheng classification[6] |
|---|---|---|
| Stage II | Stage IIA | Stage A, smooth, and intact |
| Stage II | Stage II A | Stage A, smooth, and intact |
| Stage II | Stage V | Stage A, smooth, and intact |
| Stage II | Stage V | Stage A, smooth, and intact |
| Stage II | Stage II A | Stage A, smooth, and intact |
| Stage II | Stage III | Stage C fibrillation/fissures |
| Stage II | Stage V | Stage A, smooth, and intact |
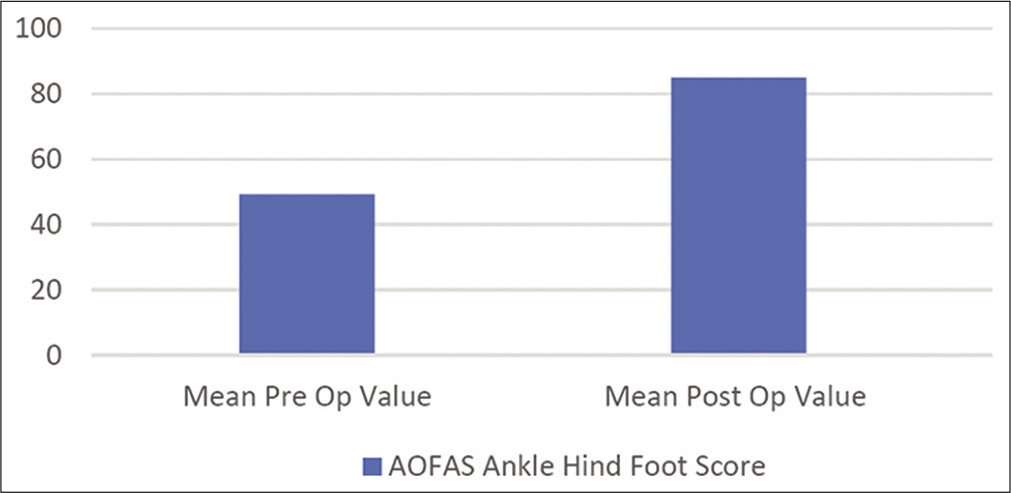
- Mean pre-operative and post-operative AOFAS.
DISCUSSION
The present study shows that retroarticular drilling followed by impaction bone graft yield favorable results which are statistically significant. In such cases, the most vital intraoperative step is being cautious while drilling to avoid chondral breach. In the literature, the talar has OCD which has been extensively reported and various treatment modalities are described.
Osteochondral lesions can occur in the talar head, body, and dome. Talar dome lesions are most common, while talar head lesions are relatively rare.[11] With regard to the side of the lesion, observations have demonstrated consistently that lateral sided lesions are predominantly post-traumatic and the medial lesions are largely due to atraumatic causes, the results in our study also corroborate with the same findings.[12,13]
The mean age at presentation in our study was 48 (±9.8) years. Osteochondral lesions are also reported to have frequent occurring in children and adolescents. Similar treatment with retroarticular drilling was reported by Tis et al.[14]
Non-operative treatment method has a weighed success rate ranging from 45% to 53%, but this varies from the various stages of osteochondral lesions.[15] Often, patients with symptomatic osteochondral lesions require definitive operative procedures.[16] The operative techniques can be categorized as cartilage repair, cartilage restoration, and cartilage replacement [Table 2].
| Cartilage repair | Cartilage regeneration | Cartilage replacement |
|---|---|---|
| A. Microfracture | A. Autologous chondrocyte implantation | A. Osteochondral allograft transfer |
| B. Retroarticular drilling | B. Matrix-induced autologous chondrocyte implantation | B. Osteochondral allograft |
| C. Autologous matrix-induced chondrogenesis | C. Particulated juvenile cartilage allograft transplantation |
Talar drilling is one such of techniques employed for cartilage restoration. The principle involves decompression of the subchondral bone. Essentially, there are two methods to achieve decompression by drilling the talus; they are (a) antegrade drilling or trans talar drilling and (b) retroarticular drilling.
The antegrade or transtalar drilling often breaches the chondral surface, thereby pre-disposing to further articular damage and less favorable outcomes. The retroarticular drilling was popularized by Taranow et al. in 1999 in their case series and was demonstrated to be better than antegrade drilling.[17] In [Table 3], we have summarized the studies with retroarticular drilling and bone grafting and their characteristics.[12,17-23] The retroarticular drilling is performed with arthroscopic assistance under fluoroscopic guidance. However, to minimize radiation and improve accuracy, newer techniques involving navigation systems have been introduced.[24-27] However, the unavailability of these expensive navigation equipment’s limits its use in the developing world. In our study, we used standard fluoroscopy techniques with arthroscopy assistance for the procedure.
| Author | Year | No. of cases | Follow-up period | Staging used | Bone graft | Location of lesion | Scoring used | Clinical outcome |
|---|---|---|---|---|---|---|---|---|
| Taranow et al.[17] | 1999 | 16 | 2 years | Berndt and Harty | Autogenous graft obtained after talar drilling | Medial 16/16 | AOFAS. Ankle-hindfoot score | Improved |
| Nelsonand Haycock[18] | 2005 | 1 | NA | Berndt and Harty | Autogenous calcaneal bone graft | Medial | NA | NA |
| Kilicoglu and Taser[19] | 2005 | 1 | NA | Berndt and Harty | Autogenous ipsilateral lateral femoral condyle | Medial | NA | NA |
| Hyer et al.[20] | 2008 | 8 | 2 years | Berndt and Harty | Synthetic bone graft substitute | Posteromedial 8/8 | AOFAS- ankle-hindfoot score SF 12 score. | Improved |
| Kennedy et al.[21] | 2008 | 1 | NA | NA | Synthetic bone graft | Medial | NA | NA |
| Takao et al.[22] | 2010 | 9/25 | 2 years | MRI Hepple’s staging | Autogenous iliac crest graft | 4 cystic lesions | AOFAS. Ankle-hindfoot score | Improved |
| Anders et al.[23] | 2012 | 41 | 2.5 years | Pritisch staging | Autogenous cancellous | Medial 36/41 Lateral 4/41 Central 1/41 | AOFAS. Ankle-hindfoot score VAS | Improved |
Combination of arthroscopy drilling and bone grafting is usually indicated in early OLT lesions with cystic changes. The bone grafts initially act as scaffold for the overlying cartilage and later osseointegrate into the talus.[18,19] Cancellous bone grafts are harvested either autologous or allograft.[28] Autologous bone graft is harvested from iliac crest,[22] calcaneum,[18] and around the knee.[23] For autologous bone harvesting from donor site, the use of the OATS graft harvest set has been reported and later the same can be used while grafting into the defect post-drilling.[19] A similar method was employed in our case series.
To reduce the donor site morbidity, synthetic bone substitutes have been used to fill the void.[21] However, there have been no comparative studies demonstrating the efficacy synthetic substitutes over bone grafts.
The pre-operative and post-operative AFAOS scores are tabulated in [Figure 7], and the results observed in our study are similar to that in the literature.
MRI is a useful tool to analyze the cartilage status postoperatively. There have been studies with MRI follow-up in the post-operative period and have been associated with favorable outcome with cartilage restoration in majority of the cases studied.[20,23] There have been reports of complete detachment of the OCD lesion following drilling. In our case series, we report no case of complete detachment in the follow-up period.
The limitation for this study includes a small sample size, lack of randomization, and a long-term follow-up. None of the cases in our case series required reoperation. With existing literature and from our experience, we feel that arthroscope-assisted retroarticular drilling with fluoroscopic guidance is a feasible alternative for early lesions of OCD with or without cystic degeneration. However, further research is needed to understand the long-term effects and risk of reoperation in failed cases.
CONCLUSION
Various modalities of treatment have been described previously. However, for the early stages of osteochondral lesions with or without cystic lesions, retroarticular drilling and bone graft application seem to be a viable option. This treatment strategy does not violate the existing intact cartilage and eliminates the need for a malleolar osteotomy, thereby giving a chance for biological restoration and improving post-operative outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Santosh K. Sahanand is on the Editorial Board of the Journal.
References
- Osteochondritis dissecans of the ankle. A 20-year follow-up study. J Bone Joint Surg Br. 1987;69:93-6.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondrosis dissecans of the talus. Arch Orthop Trauma Surg. 1992;112:23-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg. 1959;41:988-1020.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of chronic osteochondral lesions of the talus: Long-term results. Am J Sports Med. 2008;36:1750-62.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondral lesions of the talus: A revised classification. Foot Ankle Int. 1999;20:789-93.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondral Lesions of the Talus: A Radiological and Surgical Comparison New Orleans: Presented at the Annual Meeting of the Academy of Orthopaedic Surgeons; 1995.
- [Google Scholar]
- No superior treatment for primary osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc. 2018;26:2142-57.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of osteochondritis dissecans, a cause of arthritis deformans of the knee. Rev Chir Orthop Reparatrice Appar Mot. 1964;50:335-52.
- [Google Scholar]
- Transtalar retrograde drilling of medial osteochondral lesions of the talar dome. Oper Tech Orthop. 1996;6:226-30.
- [CrossRef] [Google Scholar]
- Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-53.
- [CrossRef] [PubMed] [Google Scholar]
- Retrograde percutaneous drilling for osteochondritis dissecans of the head of the talus: Case report and review of the literature. J Foot Ankle Surg. 2016;55:328-32.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of osteochondral lesions of the talus: Results of drilling and usefulness of magnetic resonance imaging before and after treatment. Arthroscopy. 2000;16:299-304.
- [CrossRef] [Google Scholar]
- Osteochondral lesions of the talus: Current concepts in diagnosis and treatment. Foot Ankle Orthop. 2018;3:3.
- [CrossRef] [Google Scholar]
- Transtalar drilling of osteochondral lesions of the talus in children and adolescents. Tech Foot Ankle Surg. 2004;3:62-7.
- [CrossRef] [Google Scholar]
- Treatment of osteochondral lesions of the talus: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2010;18:238-46.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment principles for osteochondral lesions in foot and ankle. Int Orthop. 2013;37:1697-706.
- [CrossRef] [PubMed] [Google Scholar]
- Retrograde drilling of osteochondral lesions of the medial talar dome. Foot Ankle Int. 1999;20:474-80.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopy-assisted retrograde drilling of osteochondral lesions of the talar dome. J Am Podiatr Med Assoc. 2005;95:91-6.
- [CrossRef] [PubMed] [Google Scholar]
- Retrograde osteochondral grafting for osteochondral lesion of the talus: A new technique eliminating malleolar osteotomy. Acta Orthop Traumatol Turc. 2005;39:274-9.
- [Google Scholar]
- Retrograde drilling of osteochondral lesions of the talus. Foot Ankle Spec. 2008;1:207-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical tips: Retrograde drilling of talar osteochondral defects. Foot Ankle Int. 2008;29:616-9.
- [CrossRef] [PubMed] [Google Scholar]
- Retrograde cancellous bone plug transplantation for the treatment of advanced osteochondral lesions with large subchondral lesions of the ankle. Am J Sports Med. 2010;38:1653-60.
- [CrossRef] [PubMed] [Google Scholar]
- Fluoroscopy-guided retrograde core drilling and cancellous bone grafting in osteochondral defects of the talus. Int Orthop. 2012;36:1635-40.
- [CrossRef] [PubMed] [Google Scholar]
- Fluoro-free navigated retrograde drilling of osteochondral lesions. Knee Surg Sports Traumatol Arthrosc. 2011;19:55-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic-assisted fluoroscopic navigation for retrograde drilling of a talar osteochondral lesion. Foot Ankle Int. 2009;30:70-3.
- [CrossRef] [PubMed] [Google Scholar]
- Computerassistierte minimalinvasive therapie der osteochondrosis dissecans tali. Operative Orthop Traumatol. 2006;18:300-16.
- [CrossRef] [PubMed] [Google Scholar]
- Initial outcomes of 3-dimensional imaging-based computer-assisted retrograde drilling of talar osteochondral lesions. Am J Sports Med. 2009;37:1351-7.
- [CrossRef] [PubMed] [Google Scholar]
- Operative technique and clinical outcome in endoscopic core decompression of osteochondral lesions of the talus: A pilot study. Med Sci Monit. 2016;22:2278-83.
- [CrossRef] [PubMed] [Google Scholar]






