Translate this page into:
Medial meniscal posterior root tear – A current concept review
*Corresponding author: Amit Kumar, Department of Orthopedics, Indraprastha Apollo Hospital, New Delhi, India. achauhan141@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar A, Vijay V, Vaish A. Medial meniscal posterior root tear – A current concept review. J Arthrosc Surg Sports Med. 2024;5:107-14. doi: 10.25259/JASSM_27_2024
Abstract
Menisci are crucial structures in the knee joint for the adequate distribution of hoop stresses. Their significance in preventing early knee osteoarthritis has been acknowledged due to the rapid progression of osteoarthritis in knees following meniscectomy. The anatomy of menisci has been studied in detail with an increased understanding of the importance of meniscal root attachments. This review aims to provide an evaluated summary of the anatomical, biochemical, and functional aspects that are relevant in the clinical context of meniscus root attachments, alongside contemporary strategies for accurately diagnosing and treating common injuries affecting these attachments. We also propose an algorithm for managing medial meniscus root tears which may be beneficial for the readers. We did an up-to-date literature search on PubMed, Scopus, and Google Scholar database, using the keywords ‘meniscus’, ‘meniscal root’, ‘sports injury’, and ‘arthroscopy’ in April 2024 and filtered out the relevant literature for this review on the articles that were published in English. The management of root tears requires a high level of suspicion which is crucial for diagnosis, identifying subtle signs on radiology, and employing specific methods for root repair. The tears or avulsions within one centimeter of the tibial attachment of the medial meniscus posterior root are called medial meniscus posterior root tears. These injuries cause a functional meniscal deficiency, resulting in knee problems unfavorable to biomechanics. Numerous methods have been created to tackle meniscus root tears., with many demonstrating promising outcomes in terms of complete healing.
Keywords
Knee
Meniscus
Medial meniscus root tear
Root repair
Arthroscopy
INTRODUCTION
Meniscal root tears represent a significant and increasingly recognized pathology, posing challenges in diagnosis and management. The menisci have an important function in evenly distributing weight providing stability to the joint and providing shock absorption during movement. Specifically, the menisci are secured to the tibial plateau by the meniscal roots, ensuring their proper function in maintaining joint integrity. A meniscal root tear occurs when the attachment is avulsed or when a full radial tear happens within 1 cm of the meniscus’s anterior or posterior tibial attachment points.[1-3]
The tears lead to meniscal extrusion, increasing pressure on the joint and speeding up the development of joint space narrowing, subchondral insufficiency fractures, and, in rare instances, the distinct characteristics of spontaneous osteonecrosis of the knee (SPONK) as observed in magnetic resonance imaging (MRI).[1]
A tear in the meniscus impairs the anchoring mechanism, putting the knee joint’s structural and biomechanical integrity at risk. Peripheral tears may heal independently, but meniscal root tears often cause the extrusion of the meniscus, altered joint mechanics, and accelerated articular cartilage degradation. Consequently, early detection and adequate care of the meniscal root. Biomechanical studies have demonstrated that injuries to the meniscal root disrupt the integrity of the circumferential fibers, resulting in the inability of the meniscus to distribute axial loads into transverse hoop stresses effectively.[4-8]
Understanding the structural and mechanical differences among the lateral and medial menisci is critical for timely detection and tailored treatment of meniscus root tears, taking into account the distinct biomechanical demands and anatomical features of each meniscus.
This review article discusses the anatomy and biomechanics of meniscal roots, the causes, and categorization of meniscal root tears, diagnostic options, and current trends and techniques for managing them. We have also provided a clinical algorithm for managing meniscus root tears.
ANATOMY AND BIOMECHANICS OF MENISCAL ROOT
Anatomy
The anterior and posterior horns of both the medial and lateral menisci are anchored by four meniscal roots [Figure 1]. These include the anterior root attachments of the medial and lateral menisci and the posterior root attachments of the medial and lateral meniscus. Each of these attachments includes a core group of fibers and additional connecting fibers.
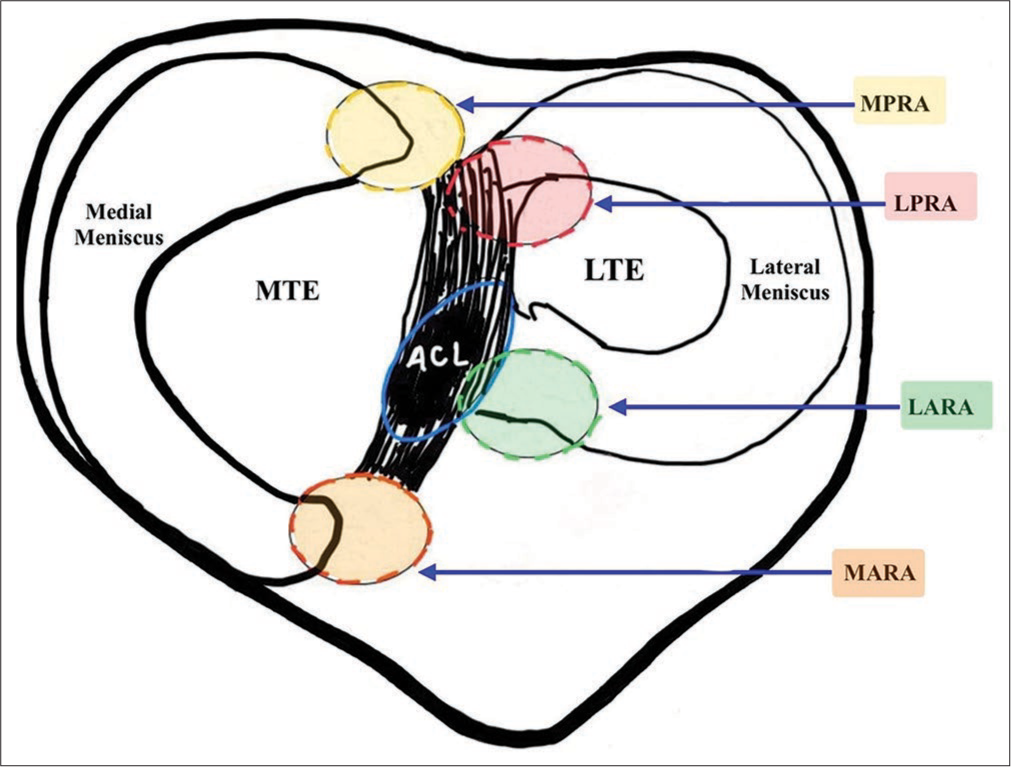
- The top surface of the tibia depicting the attachment of the roots of the menisci. MPRA: Medial posterior root attachment, LPRA: Lateral posterior root attachment, LARA: Lateral anterior root attachment, MARA: Medial anterior root attachment, ACL: Anterior cruciate ligament, MTE: Medial tibial eminence, LTE: Lateral tibial eminence.
The distances from the attachment points of meniscal roots to landmarks such as the lateral tibial eminence (LTE) and medial tibial eminence (MTE) have been established through research on cadavers. They are crucial for correctly repairing meniscal roots. Repairing meniscal roots in a way that does not follow the natural anatomy often leads to outcomes similar to removing the meniscus entirely, increasing the risk of osteoarthritis (OA).
Hence, it is crucial to have a comprehensive grasp of the anatomy of the meniscal root to ensure proper repositioning of the menisci. At times, accomplishing this requires extensive use of arthroscopic tools or similar instruments, particularly when the menisci have become attached in an unnatural location to the adjacent tissue.
Medial anterior root attachment
The point where the medial meniscus anterior root attaches anteriorly to the intercondylar crest of the tibial slope.[9] According to reports, the central location of the anterior root of the medial meniscal is roughly 18.2 mm anterior and medial from the center of the tibial footprint of the anterior cruciate ligament (ACL) and 27.5 mm anterior and lateral from the peak of the MTE.[10]
Lateral anterior root attachment
LaPrade et al. revealed that the anterior lateral meniscal root area averaged 140.7 mm2, indicating significant overlap with the ACL footprint.[11] Furthermore, its location was 5.0 mm anterior and lateral from the center of the ACL footprint, 14.4 mm from the apex of the LTE, and 7.1 mm from the closest edge of the lateral articular cartilage. While reaming the tibial tunnel for an ACL reconstruction, it is crucial to be cautious of possible iatrogenic harm to adjacent structures.[10,11]
Medial posterior root attachment (MPRA)
The medial posterior root attachment of the root is situated 9.6 mm posterior and 0.7 mm lateral to the MTE, considered the most reliable bony reference point.[12] The central point of the MPRA is situated 3.5 mm lateral to the inflection point of the medial cartilage and 8.2 mm anteriorly to the attachment point of the posterior cruciate ligament (PCL).[12]
Lateral posterior root attachment (LPRA)
The position is 1.5 mm behind and 4.2 mm medial to the LTE.[12] The LPRA’s midpoint is positioned 4.3 mm medial to the inflection point of the lateral cartilage and 12.7 mm directly anterior to the most proximal tibial attachment of the PCL.[12]
Biomechanics and significance of meniscal root
The meniscus’s role is essential in knee biomechanics, its integrity depends on secure root attachments, which prevent displacement during movement. Detachment disrupts knee function similar to total meniscectomy. Medial meniscal root tears resemble subtotal meniscectomy, leading to increased contact pressures and reduced area.
PREVALENCE AND AETIOLOGY
Tear in the menisci can be encountered in acute as well as chronic settings. Tear due to frequently encountered by knee injuries involving multiple ligaments or due to trauma from overextension or crouching referred to as acute tears.[13] During knee flexion up to 90°, the posterior attachments of the medial and lateral meniscus bear more weight than the anterior meniscus attachment.[14] The posterior root of the medial meniscus is the least flexible, and the stress on it leads to a higher occurrence of tears compared to other roots. Understanding their incidence and etiology is crucial for effective diagnosis, treatment, and prevention strategies.
Prevalence
Advancements in imaging methods have led to increased recognition of meniscal root tears and greater awareness among clinicians. The incidence of meniscal root tears has been reported to account for 10–21% of all meniscal tears, representing a substantial portion of meniscus-related issues.[1]
Incidence rates vary with age and activity levels. Although they can occur in all age groups, older adults often experience degenerative root tears. At the same time, younger individuals may suffer traumatic injuries during sports or activities involving sudden pivoting or twisting motions.[13] An increased risk of medial root tears has been linked to female sex, increasing age, an elevated body mass index, and a decrease in sports activity levels.[15]
Etiology
These injuries can occur due to traumatic events or more commonly in degenerative knees, with minor movements like squatting also contributing to tears.[16] Among the meniscal roots, the MPRA is particularly susceptible, with an incidence ranging from 10% to 21% of medial meniscus tears.[15] Notably, about 70–80% of individuals diagnosed with SPONK have associated medial meniscus posterior root tears, suggesting a correlation between the tear and this syndrome.
Trauma: Meniscal root tears can be caused by acute trauma, such as twisting or hyperextension of the knee joint, primarily during sports or accidents.
Degeneration: Chronic degenerative changes in the meniscus predispose it to tears, particularly at the root attachment site. Aging, repetitive stress, and underlying conditions like OA significantly contribute to this process.
Predisposing factors
Anatomic variations in meniscal root anatomy, such as root attachment angle or size discrepancies, may increase susceptibility to tears. Abnormalities in knee biomechanics, such as altered joint loading patterns or malalignment, can exert excessive stress on the meniscal root, making it more vulnerable to injury. Genetic factors may play a role in predisposing individuals to meniscal root tears, although specific genetic markers remain to be elucidated.[17] Certain systemic conditions such as rheumatoid arthritis or metabolic disorders may weaken the meniscus and contribute to root tears.[18]
CLASSIFICATION OF MENISCAL ROOT TEARS
As per LaPrade, the meniscal root tears are classified [Figure 2].[3]
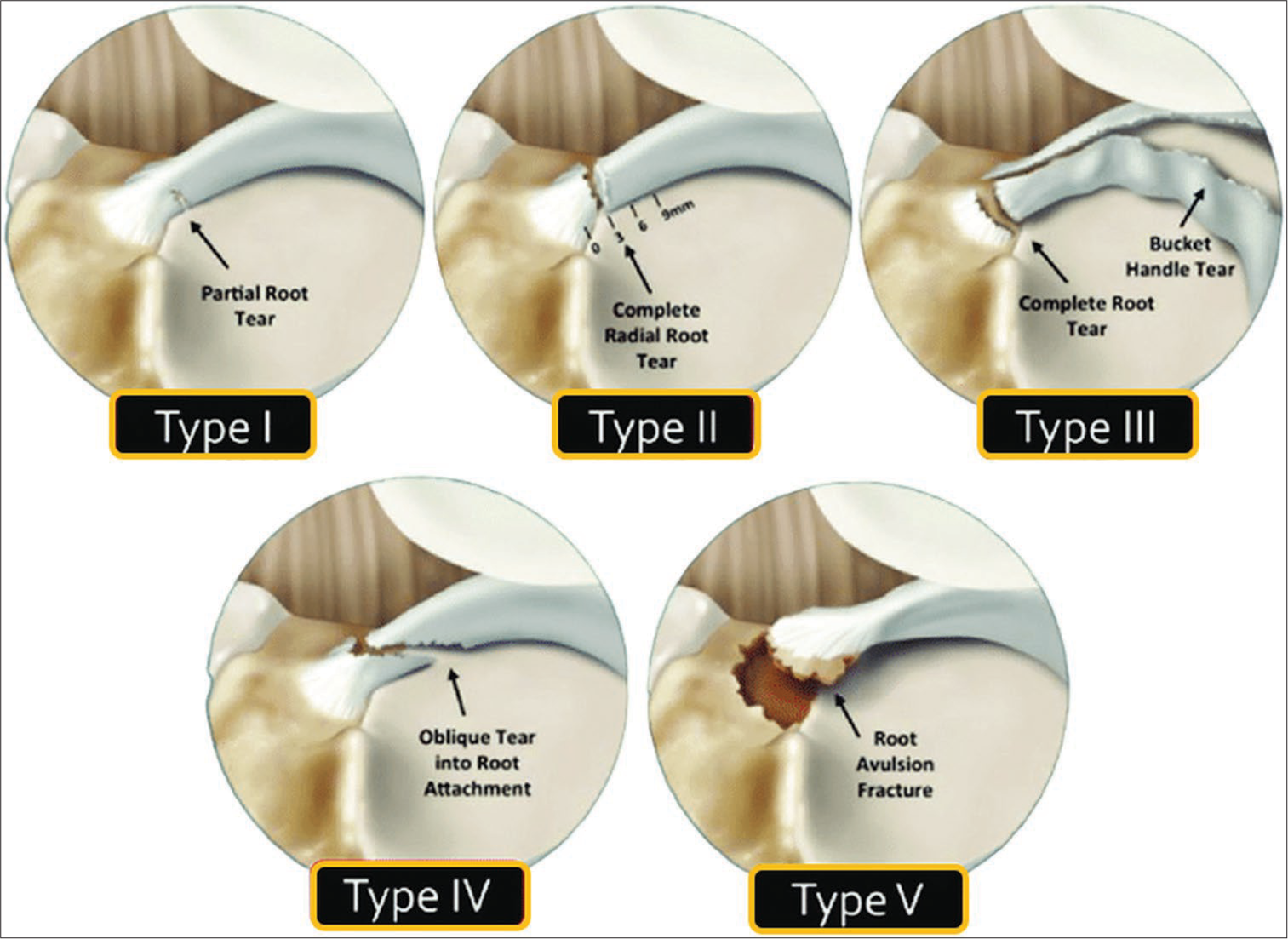
- Classification of meniscal root tears (LaPrade’s system, 2014).
To categorize posterior root tears based on their morphology through arthroscopic evaluation, there is a classification as follows:
Type 1: Incomplete tears with stable root conditions
-
Type 2: Most prevalent, complete radial tears occurring adjacent to the root attachment
They are further classified into subtypes depending on their proximity to the center of attachment:
Type 2A: <3 mm
Type 2B: 3–6 mm
Type 2C: 6–9 mm
Type 3: Bucket-handle tears with complete root detachment
Type 4: Oblique tears up to the root attachment
Type 5: Bony avulsions can cause long-term issues by turning into meniscal ossicles over time.
Recent studies show the association of meniscus root tears with the medial meniscosynovial or meniscal-capsular junction, known as a RAMP lesion within the same meniscus. This particular meniscal injury pattern is classified as Type 6 in addition to LaPrade classification.[19]
DIAGNOSIS
Effectively counseling and planning further management for patients requires the essential diagnosis of meniscal root injuries.
Physical examination
During a physical examination, commonly observed indicators include posterior knee discomfort during deep flexion and sensitivity along the joint line.[20] McMurray testing yielded positive results in only 57.1% of cases, while effusion was evident in merely 14.3%.[19] A new varus stress examination helped identify the avulsion of the posterior root of the medial meniscus. In this examination, the patient should be completely relaxed with the knee extended. When conducting the varus stress test, meniscal extrusion can be detected through palpation along the anteromedial joint line. The extrusion diminishes on restoring the knee to its normal alignment.[21] Despite limited data to provide quantitative sensitivity or specificity, they advocated for its utility in diagnosis and clinical monitoring.[21]
Imaging
The preferred imaging technique for diagnosing meniscal root tears and associated pathologies is MRI, which has high reported sensitivity and specificity, particularly with T2-weighted sequences [Figure 3]. Key MRI signs suggestive of root tears include root discontinuity, extrusion, and the ghost sign, which together enhance diagnostic accuracy. Extrusions larger than 3 mm on mid-coronal imaging have a strong correlation with degenerative changes, highlighting their importance for diagnosis.[22]
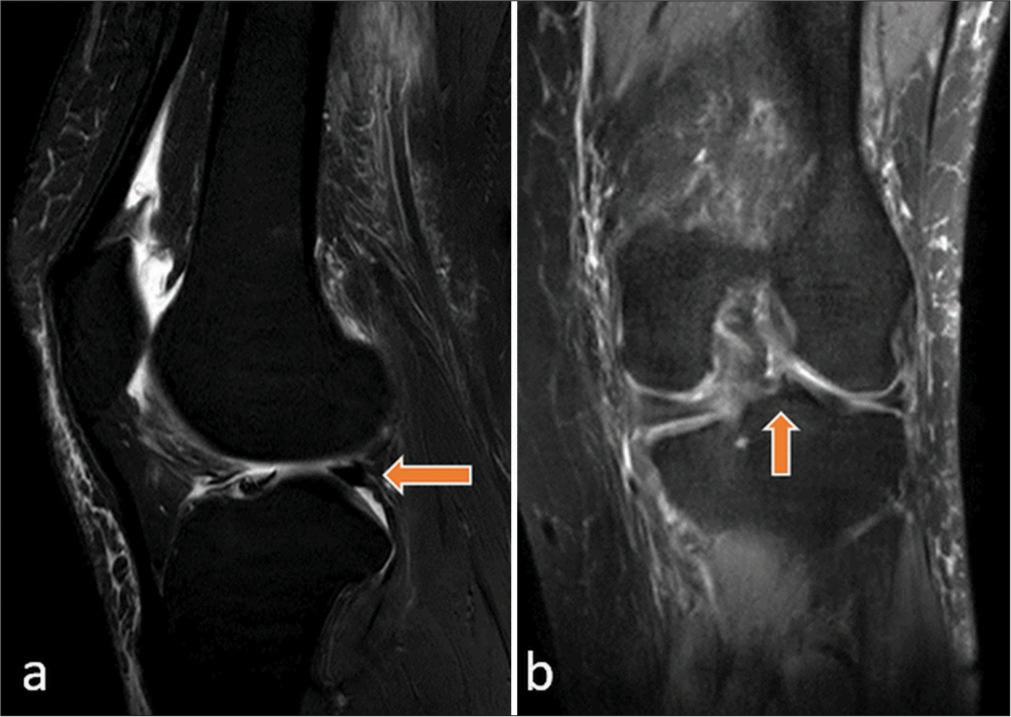
- Fast spin echo T2-weighted fat suppression images (a) sagittal section shows the oblique tear of the posterior horn of the medial meniscus extending into the root attachment (left arrow) and (b) coronal image with a change in signal intensity (right arrow).
While challenges persist in visualizing the posterior medial meniscus root on MRI, efforts are focused on improving detection methods. Differentiating true medial meniscal root tears from other tear types is vital for determining appropriate treatment strategies. In addition, standard MRI protocols can detect lateral meniscal root tears, but the accuracy of MRI in identifying these tears has not been fully determined.
TREATMENT
The management of meniscal root tears can be classified into three primary methods: (A) Non-operative treatment, (B) partial meniscectomy, and (C) meniscal root repair.[23] In the past, individuals with root injuries have often chosen one of the initial two options. In specific situations, non-surgical treatment may still be suitable, especially for patients who are unsuitable candidates for surgery due to numerous additional health conditions, old age, and established advanced arthritis. In such instances, a preliminary trial of conservative therapy is the chosen treatment method. The primary goal of surgical intervention is to restore normal articular surface loads and biomechanics to normal, which also aims to delay the advancement of OA. Therefore, in patients with diffuse Outerbridge Grades 3–4 cartilage injury, surgical restoration might not be advised. To relieve symptoms, it might be taken into consideration for those with specific chondral deficiencies.
The surgical management of meniscal root tears is usually only considered for individuals with high-quality cartilage and relatively recent meniscal root injuries. It is crucial to carefully consider appropriate indications for surgical intervention to optimize treatment outcomes.
Non-operative treatment
The approach to meniscal root tear management is determined by the severity of the injury, the timing of surgical intervention for the injury, and the clinical status of the articular surface area. Surgery aims to restore normal articular load and knee joint motion, hence delaying the onset of OA. As a result, surgical management is usually not suggested for individuals with extensive and advanced cartilage degradation; however, it could be taken into account for individuals with specific cartilage deficiencies to help relieve symptoms.
The recommended approach is to avoid surgery for individuals with major additional health issues and advanced OA (Kellgren–Lawrence grade ≥3) as shown on radiographs. Patients in this category may find relief from symptoms using pain relievers and an off-loader brace that unloads the medial compartment. If non-operative treatment fails and patients progress to knee OA, partial or total knee replacement may be considered as a further option.
Meniscectomy
Meniscectomy has been linked to a greater likelihood of developing arthritis when compared to non-surgical treatment, while meniscal root repair has been an economically efficient procedure. Non-surgical treatment or meniscectomy for meniscal root tears may lead to unfavorable clinical results and require a transition to total knee arthroplasty, as suggested by various studies. Meniscal removal is now seldom recommended, except in cases of degenerative tears that are advanced or cause significant physical symptoms for the patient, despite the expected arthritic progression.
Root repair
Anatomic repair-transtibial pull-out repair
The method outlined includes sutures being passed through the meniscus root, brought back through tunnels created in the proximal tibia, and then anchored across an attachment, button, or anterior tibia bone bridge [Figure 4]. There are various variations in meniscal suture configurations, including two basic sutures, the horizontal mattress stitch, modified Mason-Allen (MMA), and two customized loop stitches. Studies have shown that two simple sutures minimize root displacement, exhibit higher stiffness, and supposedly show no significant variance from the more complex MMA suture. The anatomical footprint can be better replicated and biological healing can be improved through the use of single-tunnel and double-tunnel techniques.[24] Fixation with a button is preferred because it is less intrusive and provides a reduced risk of soft-tissue damage than screw and washer fixation. This technique aims to provide stability and function with minimal complications and maximize the healing process.
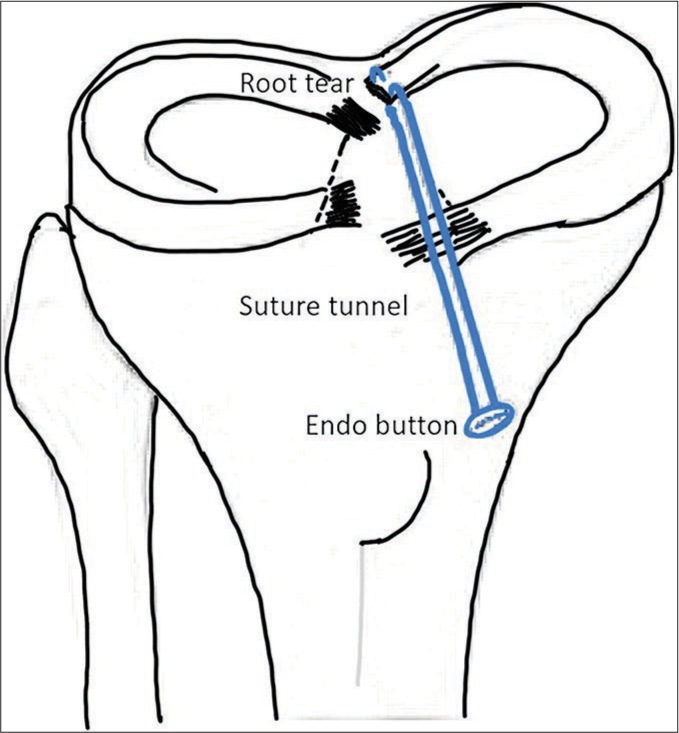
- Transtibial pull-out repair of a medial meniscal posterior root tear in a right knee.
Non-anatomical root repair (all inside suture repair technique)
The evaluation of a tear in the posterior root of the medial meniscus involves the use of a probe inserted through an anteromedial portal. If the exposure of the posterior root of the medial meniscus is obstructed and if there is tightness in the medial compartment, an outside-in percutaneous release of the medial collateral ligament will be performed. Medial meniscus posterior root fixation will be done in a cerclage fashion superiorly and inferiorly to the capsular margins. There will be two vertical mattress sutures used to secure the posterior root tear of the medial meniscus through the anteromedial portal.
To avoid over-penetration, which may lead to neurovascular injury, the depth penetration is limited to 12–14 mm to prevent over-penetration to the posterior joint capsule. Thorough probing medial meniscus tightness ensured with posterior capsular attachment in cerclage configurations. A procedure will be carried out to vent the bone marrow in the intercondylar notch to enhance healing, through the introduction of bone marrow elements, such as mesenchymal stem cells, to migrate to the surface of the damaged cartilage. A hinged knee brace will be applied for the post-operative course. A proposed algorithm is presented in Table 1 for managing medial meniscal root tears.
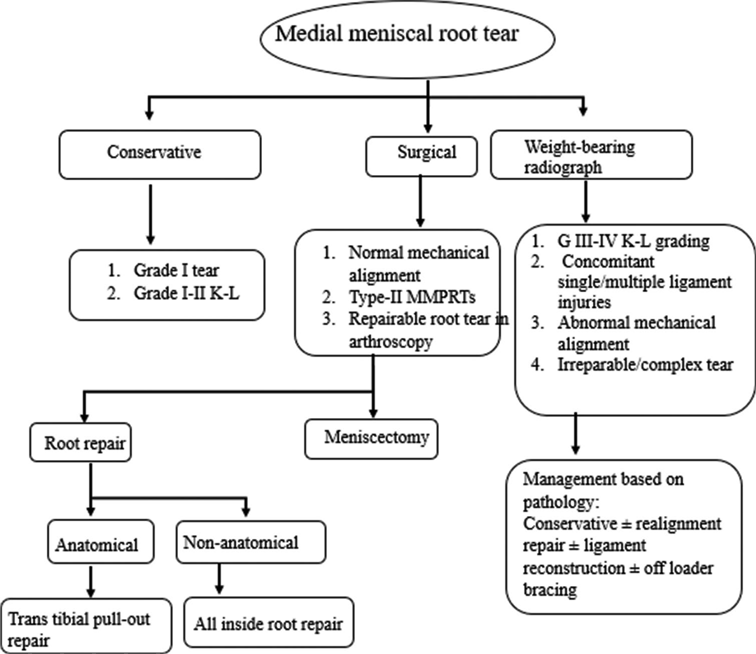 |
MMPRTs: Medial meniscus posterior root tears; K-L grading: Kellgren and lawrence grading
Post-operative rehabilitation
The operated knee will be restrained in a brace with the knee extended for 4 weeks. The patient will be allowed closed chain range of motion exercises. Active or passive range of motion will be allowed up to 90° starting on day 1 for 6 weeks. The patient will be kept non-weight bearing for four weeks followed by partial weight bearing with progression to complete weight bearing and a full range of motion by 8–10 weeks post-surgery. After the surgery, deep squatting and strenuous activity like running will be allowed at 4 months and 6 months, respectively.
To optimize conditions for healing after meniscal root repair, patients undergo a carefully structured rehabilitation protocol.
The rehabilitation program aims to promote healing while gradually restoring mobility and strength. Deep knee flexion exercises are integrated into the regimen to enhance flexibility and functionality.[25]
Outcomes
As per treatment protocols, meniscal root tears have evolved significantly. Recent literature-based analysis has shown debatable outcomes following non-operative management versus operative management including meniscectomy and repair. Until 2005, there was a consistent increase in publications; from 2005 to 2022, there was an almost fourfold increase.[26]
The transtibial pullout technique is reported to effectively restore knee joint motion in the vast majority of individuals when repairing meniscal root tear injuries. LaPrade et al. undertook a study that included 45 knees. They noted improvements in Lysholm scores and observed no substantial variations in operational result ratings between patients younger than 50 and those aged 50 and above.[27]
Ozkoc et al.[15] defined the clinical outcomes of patients who underwent partial meniscectomy, with a Level 4 retrospective study (67 patients, 56.7 months), comparing post-operative MRI and surgical outcomes. The clinical results were evaluated by Kellgren–Lawrence grading, Lysholm scoring, and radiological investigations which revealed that the average Lysholm score increased from 53 to 67. Pre-operative Kellgren–Lawrence Grade 2 (range 0–3) raised to 3 (range 2–4). Hence, they concluded that the arthroscopic partial meniscectomy for posterior root medial meniscus tears reduces symptoms but does not stop the progression of OA. Kim et al.[28] investigated the outcomes of patients in two groups (28 with partial meniscectomy and 30 with arthroscopic transtibial pullout repair) and found that arthroscopic transtibial pullout surgery produced improved functional and radiological outcomes. The repair group achieved significantly higher International Knee Documentation Committee (IKDC) and Lysholm scores, with less joint space narrowing and less advancement to Kellgren–Lawrence grading.
Surgical repair, particularly a transtibial tunnel pull-out technique, has yielded excellent outcomes, ensuring anatomical reduction and fixation on the anterior tibia.[29]
Jung et al.[30] investigated the subjective and objective outcomes of all inside root repair of a posterior root medial meniscus tear in 21 knees over a 24–48-month period. Clinical evaluation was performed utilizing tenderness over the joint line, the McMurray test, and radiographic examinations. They concluded that no patients experienced joint line discomfort, effusion, or a positive McMurray test result after surgery. Significant improvements were observed in both Tegner activity level and Lysholm scores. The average medial meniscus extrusion was 3.9 mm preoperatively and 3.5 mm postoperatively (P > 0.05). Choi et al.[31] proposed an arthroscopic all-inside approach to maintain the structural vitality and biomechanics of the meniscus instead of resorting to meniscectomy. A curette is used to remove the attachment of the posterior horn.
The posteromedial portal had two fiber wires and a metal anchor inserted through it. An anatomic insertion of the posterior meniscus root was done using a polydioxanone suture.
Zhu et al.[32] in the study discussed a new arthroscopic repair technique for individuals more than 45–50-year-old patients with tears in the posterior root of the medial meniscus and assessed the outcomes of this procedure throughout 3–6 months of follow-up. The mean Lysholm score improved significantly, the median Tegner activity score improved, and the mean IKDC score improved.
As previously mentioned, research in the literature has shown that meniscal root tears are better treated with a variety of repair techniques than meniscectomy, provided that the root tear is amenable to repair. Stem cells and other biological treatments, such as platelet-rich plasma (PRP), are utilized to enhance the healing process for tears.[33] Meniscal root tear repair may be a viable option to improve objective and subjective outcomes in clinical and radiological settings.
CONCLUSION
Meniscal root tears have garnered attention as a silent epidemic. Significant steps have been taken since meniscectomy was the go-to treatment, with the realization that non-operative management and non-anatomic repairs fail to restore joint kinematics and halt OA progression. While awareness of root tears has improved, detection remains imperfect. It is advisable to repair these tears whenever feasible. However, despite anatomical fixation, extrusion persists as a concern, prompting further exploration into the viability of additional stabilization sutures for long-term resolution. Post-surgery, adherence to a well-structured rehabilitation program is imperative for optimal recovery. Surgical techniques for meniscal tear repair have improved significantly, and there is a greater focus on repairing meniscal tears rather than removing them when possible. The presence of menisci is now widely accepted as essential for knee health in the long term.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Meniscal root tears: A silent epidemic. Br J Sports Med. 2018;52:872-6.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43:912-20.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363-9.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922-31.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42:699-707.
- [CrossRef] [PubMed] [Google Scholar]
- Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37:124-9.
- [CrossRef] [PubMed] [Google Scholar]
- Repair of lateral meniscus posterior horn detachment lesions: A biomechanical evaluation. Am J Sports Med. 2012;40:2604-9.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: Diagnosis and treatment. Arthroscopy. 2009;25:1025-32.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of the anterior root attachments of the medial and lateral menisci: A quantitative analysis. Am J Sport Med. 2014;42:2386-92.
- [CrossRef] [PubMed] [Google Scholar]
- Consequences of tibial tunnel reaming on the meniscal roots during cruciate ligament reconstruction in a cadaveric model, Part 2: The posterior cruciate ligament. Am J Sports Med. 2015;43:207-12.
- [CrossRef] [Google Scholar]
- Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sport Med. 2012;40:2342-7.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior meniscus root tears: Associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23:3127-31.
- [CrossRef] [PubMed] [Google Scholar]
- The basic science of human knee menisci: Structure, composition, and function. Sports Health. 2012;4:340-51.
- [CrossRef] [PubMed] [Google Scholar]
- Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16:849-54.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior root tear of the medial meniscus in multiple knee ligament injuries. Knee. 2010;17:324-8.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: Comparing medial and lateral meniscal root tears is like comparing apples and oranges. Arthroscopy. 2020;36:1142-4.
- [CrossRef] [PubMed] [Google Scholar]
- A new entity of ramp lesion combined with posterior root tear of the medial meniscus: A case report. JBJS Case Connect. 2024;14:e2300439.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: Radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25:951-8.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2011;19:2072-5.
- [CrossRef] [PubMed] [Google Scholar]
- The MRI findings of meniscal root tear of the medial meniscus: Emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc. 2012;20:2098-103.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016-30.
- [CrossRef] [PubMed] [Google Scholar]
- Avulsion of the anterior medial meniscus root: Case report and surgical technique. Knee Surg Sports Traumatol Arthrosc. 2013;23:146-51.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus posterior root tear: How far have we come and what remains? Medicina (Kaunas). 2023;59:1181.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in Meniscus-related publications in PubMed since 1928: A bibliometric study. Orthop J Sports Med. 2024;12:23259671231226326.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884-91.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus root tear refixation: Comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27:346-54.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: Solving the silent epidemic. J Arthrosc Surg Sports Med. 2021;2:47-57.
- [CrossRef] [Google Scholar]
- All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40:1406-11.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: A technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16:891-3.
- [CrossRef] [PubMed] [Google Scholar]
- Non-anatomic repair of medial meniscus posterior root tears to the posterior capsule provided favourable outcomes in middle-aged and older patients. Knee Surg Sports Traumatol Arthrosc. 2021;29:4261-9.
- [CrossRef] [PubMed] [Google Scholar]
- A minimally invasive revolution: The future of arthroscopy and sports medicine. J Arthrosc Surg Sports Med. 2023;4:27-9.
- [CrossRef] [Google Scholar]






