Translate this page into:
Non-operative and operative management of posterior tibialis tendon dysfunction – A systematic review and meta-analysis
*Corresponding author: Rishi Trivedi, Department of Trauma and Orthopaedics, Leicester Royal Infirmary, Leicester, United Kingdom. rishijtrivedi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Adukia V, Trivedi R, Houchen-Wolloff L, Mangwani J, O’Neill S, Divall P, et al. Non-operative and operative management of posterior tibialis tendon dysfunction – A systematic review and meta-analysis. J Arthrosc Surg Sports Med. 2025;6:3-15. doi: 10.25259/JASSM_43_2024
Abstract
Background and Aims:
Posterior tibial tendon dysfunction (PTTD) is the most common cause of adult-acquired flatfoot deformity. Both non-operative and operative treatment modalities exist; however, there is no consensus on the optimal treatment. The aim was to systematically review the literature for outcomes following the treatment of PTTD.
Materials and Methods:
Medline, Embase, and the Cochrane Library were searched between August 2020 and August 2021. Studies on the management of PTTD were identified and included those that explored non-operative modalities, such as physiotherapy, or operative modalities, such as flexor digitorum longus (FDL) transfer or the Cobb procedure. Only studies that reported pre- and post-operative functional and/or radiological outcome measures were included. The studies were analyzed for quality using the modified Coleman Methodology Score. A random effects model was used to evaluate the pooled outcome data.
Results:
The search yielded 1795 and 129 studies for the non-operative and operative management of PTTD, respectively, of which 3/1795 and 15/129 studies were included. All 3 studies for the non-operative management of PTTD reported different orthotics and physiotherapy regimens. Orthoses along with stretching and strengthening exercises had more favorable outcomes (P < 0.0001) than orthoses and stretching alone (P = 0.02). 12/15 studies for the operative management of PTTD involved an FDL transfer, of which only one was a randomized controlled trial. The pooled mean difference (MD) was found to be significant for all assessed outcomes – American Orthopaedic Foot and Ankle Society (AOFAS) scores (MD = 41, P < 0.00001), talonavicular coverage angle (MD = 12.66, P < 0.001), lateral talometatarsal angle (MD = 7.17, P < 0.00001), and calcaneal pitch (MD = 4.09, P < 0.00001).
Conclusion:
Orthoses with stretching and strengthening exercises have more favorable outcomes than orthoses and stretching alone. Both FDL transfer and the Cobb procedure improve functional and radiological outcomes and are viable options for the surgical management of PTTD. However, there is a lack of data, meaning that the superiority of one method over the other cannot be proven.
Keywords
Posterior tibialis tendon dysfunction
Adult acquired flatfoot deformity
Flexor digitorum longus tendon transfer
Cobb procedure
Orthoses
Talonavicular coverage angle
INTRODUCTION
Posterior tibialis tendon dysfunction (PTTD) is a degenerative condition characterized by pathological changes in the posterior tibialis tendon (PTT). This results in the collapse of the medial longitudinal arch, a valgus deformity of the hindfoot, and forefoot abduction.[1] It is one of the most common causes of adult-acquired flatfoot deformity, and it is thought to affect at least 3% of the general population over the age of 40.[2] Patients with PTTD often describe a history of trauma and present with progressive pain over the medial side of their foot and ankle. Clinical examination typically demonstrates tenderness over the PTT, inability to perform a single heel raise, and weakness on testing the power of the PTT.[3]
The Myerson modification of the Johnson and Strom classification is the most widely used system to classify the disease into four stages. Each stage represents a progressive deformity of the foot. In stage I, patients have PTTD with an intact medial longitudinal arch, whereas stage II includes patients with a flatfoot deformity and a flexible hindfoot deformity. In stage III, the hindfoot deformity becomes rigid. Stage IV involves deltoid ligament compromise, resulting in lateral tibiotalar arthritis in addition to the subtalar arthritis seen in stage III.[4]
Management consists of anti-inflammatories, physiotherapy, and orthotics for patients with Stage I disease, whereas surgery is recommended for Stages II-IV. Surgery typically involves tendon transfers using the flexor digitorum longus (FDL) or anterior tibialis tendon and calcaneal osteotomies (medial displacement calcaneal osteotomy [MDCO], lateral column lengthening [LCL]) and other adjunctive procedures. Later stages of the disease require joint arthrodesis. There is, however, no consensus as to the most appropriate physiotherapy regimen, optimal orthotic, or most favorable surgical treatment, as evidenced by the multitude of options available.[5]
We therefore performed a systematic review and meta-analysis of the available literature to evaluate the outcomes following various physiotherapy regimens, use of orthotics, and surgical procedures in patients with PTTD. Our aim was to determine if a particular physiotherapy regimen, orthotic, or surgical procedure was superior to the other.
MATERIALS AND METHODS
The systematic review and meta-analysis were conducted and reported in accordance with the standards set by the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [Appendix 1 – PRISMA checklist].
A systematic literature search was conducted by an experienced clinical librarian. PubMed, Embase, Medline, CINAHL, and the Cochrane Central Register of Controlled Trials were searched from the inception of the databases until January 1st, 2022. The search terms included “posterior tibial tendon dysfunction,” “adult acquired flatfoot deformity,” “posterior tibial tendon insufficiency” AND “surgical” OR “physiotherapy,” “orthotic,” “brace,” as separate terms. The papers were restricted to the English language as we did not have the means to translate papers written in other languages. Reference lists of all included studies were also examined to identify any potential studies that may have been missed in the search results.
Eligibility criteria
All clinical studies that assessed 20 or more patients with PTTD treated either operatively or non-operatively and reported radiological and/or patient-reported outcome measures (PROMs) pre- and post-intervention were included. Studies with fewer than 20 patients, case reports, cadaveric studies, review articles, technique tips, and expert opinions were excluded. Any studies which included patients under the age of 18 were also excluded.
Outcome measures
Radiological outcomes included calcaneal pitch, anteroposterior talonavicular coverage angle (TNCA), and lateral talus-first metatarsal angle, also known as Meary’s angle. PROMs were in the form of the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scores or the foot function index (FFI).
Study selection
All titles and abstracts from the search results were independently reviewed by two authors (VA and RT) for inclusion in the study. Full texts of articles that met the eligibility criteria were then assessed by them for quality using the Modified Coleman Methodology Score [Appendix 2]. Data extracted included the number of patients treated, mean follow-up time, AOFAS scores, radiological outcomes, other PROMs, complications following treatment, and postoperative regimen.
Statistical analysis
Review Manager 5.4 by the Cochrane collaboration was used for data synthesis and analysis. Standardized mean differences were used to assess changes in the radiological outcomes and PROMs following either operative or non-operative management. The I2 statistic was used to calculate heterogeneity in the studies, and a fixed-effects model was used unless the I2 was >50%, in which case a random effects model was employed instead.
RESULTS
Non-operative management
For the non-operative management of PTTD, 1795 records were screened of which only 3 were identified as being suitable [Figure 1]. The study by Augustin et al.[6] utilized only orthotics in the form of Arizona braces for patients with PTTD stages I–III, whereas the other 2 studies by Houck et al.[7] and Kulig et al.[8] incorporated stretching exercises and/or physiotherapy in addition to either ankle stirrups or a custom-made foot orthosis, respectively [Table 1].
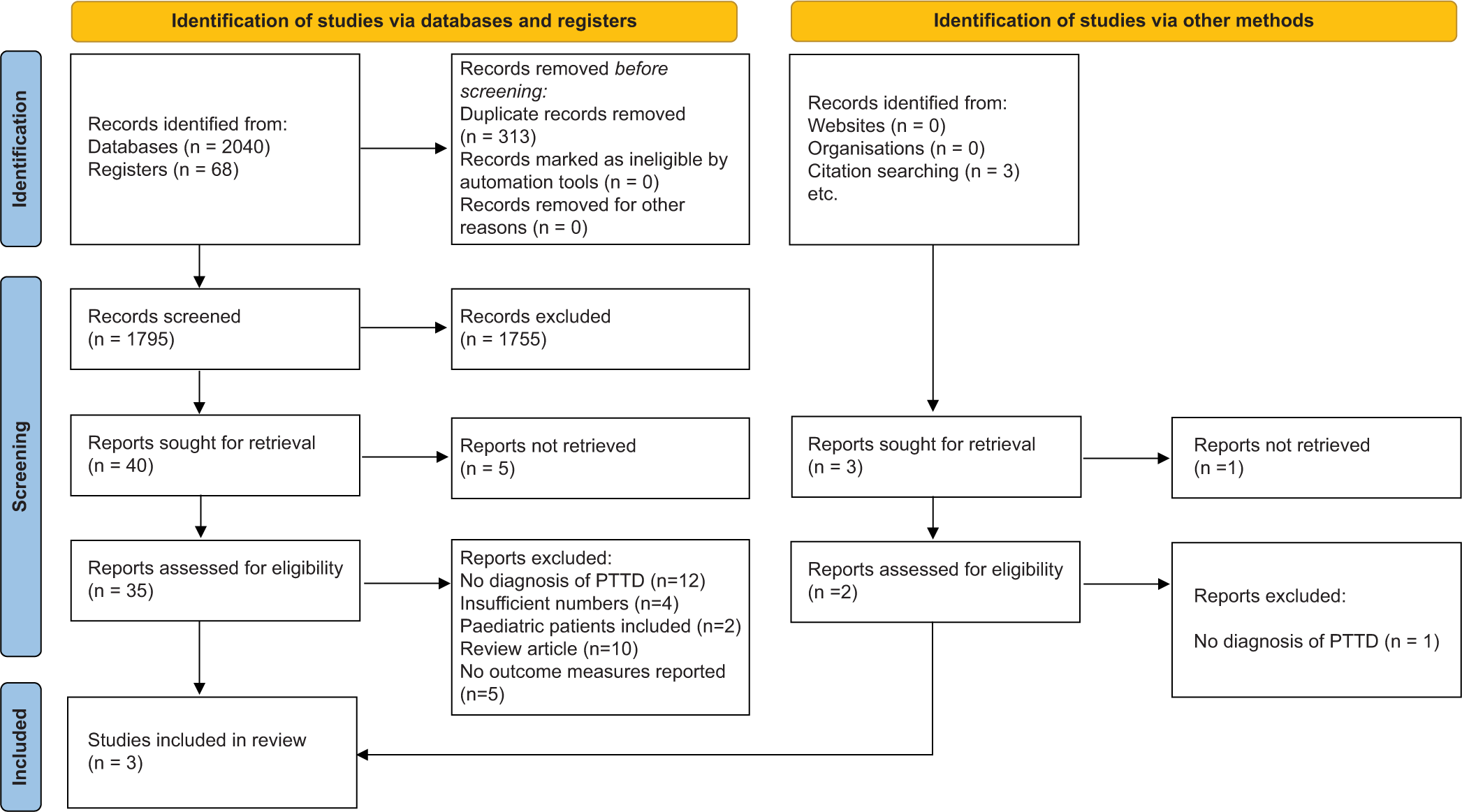
- PRISMA 2020 flow diagram for new systematic reviews evaluating the non-operative management of posterior tibialis tendon dysfunction (PTTD).
| Reference | Study type | No of patients (feet) | M : F | PTTD Stage | Additional inclusion criteria | Exclusion criteria | Intervention (no. of feet) | Mean follow up | Outcome measures | MCMS |
|---|---|---|---|---|---|---|---|---|---|---|
| Augustin JF 2003 | Case series | 21 (27) | 3 : 18 | I, II, III | No other concomitant pathology e.g., Osteoarthritis | Arizona brace (27) | 12 months | FFI SF36 AOFAS hindfoot score |
49 | |
| Houck J 2015 | RCT | 36 (36) | 8 : 28 | II | Age >40 years Able to walk 15 m |
Bilateral disease Inflammatory arthritis Other foot conditions (e.g. hallux rigidus, plantar fasciitis) Peripheral neuropathy |
Ankle stirrup and medial longitudinal arch support+stretching exercises (17) Ankle stirrup and medial longitudinal arch support+stretching and strengthening exercises (19) |
12 weeks | FFI | 77 |
| Kulig K 2009 | RCT | 36 (36) | 8 : 28 | I, II | Fixed foot deformities Previous foot or ankle surgery Cardiovascular or neuromuscular disease |
Custom made FO+stretching (12) Custom made FO+ stretching+concentric exercises (12) Custom made FO+stretching+eccentric exercises (12) |
12 weeks | FFI | 72 |
RCT: Randomised controlled trial, SF-36: 36 item short form survey, MCMS: Modified Coleman Methodology Score, PTTD: Posterior tibialis tendon dysfunction, AOFAS: American orthopedic foot and ankle society, FO: Foot orthosis, FFI: Foot function index
While all three studies demonstrated an improvement in FFI scores in all domains (pain, disability, activity), direct comparisons were not possible as each study focused on a different orthotic and/or physiotherapy regimen. However, a greater treatment effect was seen for those patients who were given strengthening exercises, in particular eccentric exercises, in addition to wearing orthotics and/or stretching [Figures 2 and 3].
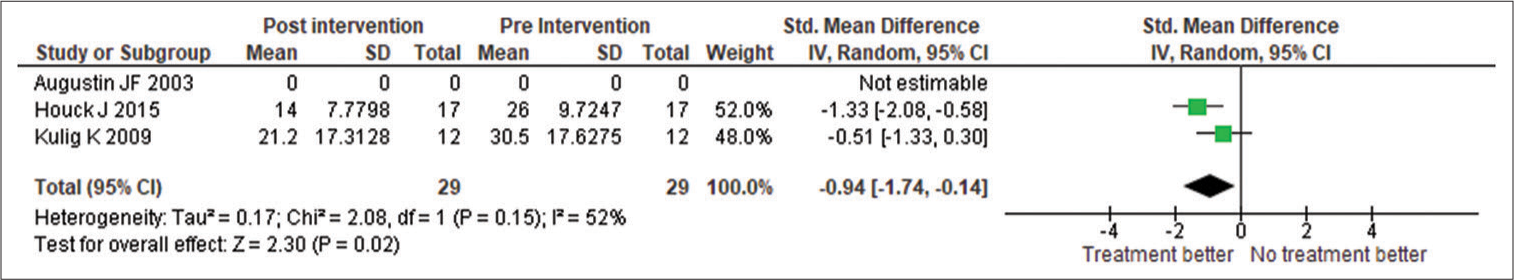
- Orthotics and stretching show some improvement in foot function index scores. SD: Standard deviation; Std.: Standard, CI: Confidence interval, IV: Inverse variance, df: Degrees of freedom, Z: Z score.

- Orthotics, stretching and strengthening show a greater treatment effect in FFI scores, most markedly in those who did eccentric exercises. SD: Standard deviation; Std.: Standard, CI: Confidence interval, IV: Inverse variance, df: Degrees of freedom, Z: Z score.
Operative management
For the surgical management of PTTD, 112 records were identified, of which 15 were included in the review [Figure 4]. All studies[9-23] were case series except the one by Osman et al.[23] which was a randomized controlled trial comparing MDCO with LCL in addition to an FDL tendon transfer. Twelve studies utilized FDL tendon transfers, while the remaining 3 used the Cobb procedure [Table 2]. In addition, all but 2 carried out additional soft tissue procedures (spring ligament plication [n = 6] and/or Achilles lengthening [n = 5]). The most commonly carried out bony procedure was an MDCO, followed by LCL. Post-operative regimens varied considerably in the studies, with patients being kept non-weight bearing between 2 and 6 weeks, with the leg either in a cast or a boot [Table 3].
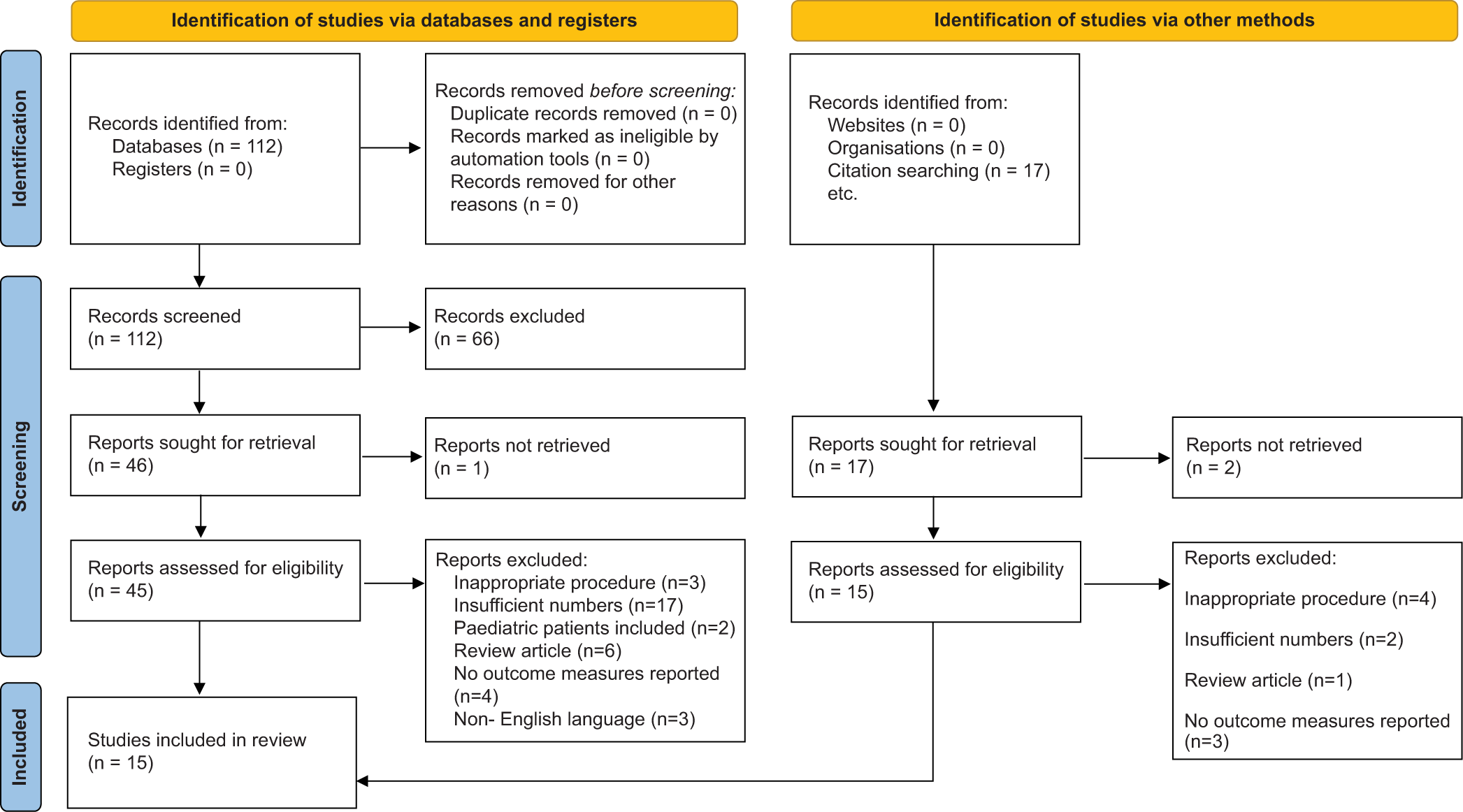
- PRISMA 2020 flow diagram for new systematic reviews evaluating the operative management of posterior tibialis tendon dysfunction.
| Reference | No of patients (feet) |
Male/female | Mean age (range) yrs |
PTTD stage | Other inclusion criteria | Exclusion criteria | Main soft tissue procedure | Additional soft tissue procedure (s) | Bony procedure | MCMS |
|---|---|---|---|---|---|---|---|---|---|---|
| Robberecht J et al. | 24 (25) | 6/18 | 54 | II | Failed conservative treatment Flexible hindfoot deformity No significant hindfoot arthrosis |
None stated | FDL tendon transfer (n=25) | Spring ligament reefing (n=5) | MDCO (n=25) Accessory navicular bone excision (n=2) |
42 |
| Usuelli FG et al. | 42 (42) | 17/25 | 41 (19–74) |
II | Failed conservative treatment MRI significant for PTTD Lack of severe deformity |
Active infection Diabetes, RA, haemophilia, neurological, metabolic or autoimmune disease Previous surgery on affected foot |
FDL transfer (n=42) | MDCO (n=42) Cotton osteotomy (n=1) |
58 | |
| Schuh R et al. | 49 (51) | 59.9 (43–79) | II | Failed conservative treatment | None stated | FDL transfer (n=51) | MDCO (n=51) | 64 | ||
| Niki H et al. | 25 (26) | 1/24 | 55.2 (42–71) | II | Failed conservative treatment MRI confirmation for PTT pathology |
Infection Diabetes Arthropathy or neuroarthropathy |
FDL transfer (n=26) | Spring ligament plication (n=10) | MDCO (n=26) | 21 |
| Chadwick C et al. | 31 (31) | 10/21 | 54.3 (42–70) | II | Failed conservative treatment | None stated | FDL transfer (n=31) | MDCO (n=31) | 60 | |
| Silva MG et al. | 40 (43) | 11/32 (feet) | 46.3 (18.9–73.5) | IIb | Flexible hindfoot deformity | None stated | FDL transfer (n=43) | Achilles lengthening (n=43) | MDCO (n=43) Lateral column lengthening (n=43) |
70 |
| Marks RM et al. | 20 (20) | 3/17 | 52.4 | II, IIb | Failed conservative treatment | PTTD stage III Prior flatfoot corrective surgery Ankle or hindfoot arthritis or fusion Angular deformity involving hip, knee or ankle DM, Inflammatory arthritis |
FDL transfer | - | MDCO (n=20) Lateral column lengthening (n=6) |
28 |
| Myerson MS et al. | 129 | 12/117 | 53 (34–75) | II | Failed conservative treatment Flexible subtalar joint with less than 15 degrees of fixed forefoot varus deformity |
Infection, diabetes, arthropathy, neuroarthropathy, seropositive arthritis | FDL transfer (n=129) | Achilles lengthening (n=26) Repair of spring ligament/deltoid ligament, talonavicular capsule (n=46) |
MDCO (n=129) 1stTMTJ fusion (n=4) Hallux valgus correction (n=5) |
63 |
| Fayazi AH et al. | 23 (23) | 6/17 | 56 (33–81) | II | Failed conservative treatment | None stated | FDL transfer (n=23) | Achilles lengthening (n=16) | MDCO (n=23) | 35 |
| Wacker JT et al. | 48 (48) | 18/30 | 61.3 (38–80) | II | Failed conservative treatment | None stated | FDL transfer | MDCO | 64 | |
| Toolan BC et al. | 36 (41) | 15/21 | 54 (23–81) | II | Failed conservative treatment | No previous hindfoot surgery | FDL transfer (n=41) | Achilles lengthening (n=41) Young’s suspension (n=9) |
MDCO (n=2) Lateral column lengthening (n=41) 1stTMTJ fusion (n=29) Naviculo- cuneiform arthrodesis (n=6) |
54 |
| Madhav RT et al. | 43 (43) | 6/37 | 57 (27–75) | II | Failed conservative treatment | Fixed foot deformities Degenerate subtalar joint Nueromuscular disorders Poor soft tissue quality |
Cobb procedure (n=43) | Rose calcaneal osteotomy (n=43) 1stTMTJ fusion (n=2) |
59 | |
| Osman AE et al. | 42 (42) | 21/21 | 49.6 (43–55) | II | Failed conservative treatment | Previous hindfoot surgery Subtalar or midfoot OA Neurological disease Patients who declined to participate in study, those who were lost to follow up, or those with missing data |
FDL transfer (n=42) | Achilles lengthening (n=42) Spring ligament plication (n=42) |
MDCO (n=22) Lateral column lengthening (n=20) |
73 |
| Knupp M et al. | 22 (22) | 10/12 | 49 (29–64) | II | Flexible flatfoot deformity | Fixed foot deformity Neuromuscular, connective tissue disorders or OA |
Cobb procedure (n=22) | Deltoid ligament reconstruction (n=17) Spring ligament repair (n=3) |
Medial sliding osteotomy (n=11) Calcaneal lengthening osteotomy (n=3) |
47 |
| Parsons S et al. | 32 (32) | 4/28 | (44–66) | II | Failed conservative treatment Flexible hindfoot deformity with forefoot supination less than 15 degrees |
Ankle or midfoot OA | Cobb procedure (n=32) | Spring ligament repair (n=2) | Medial displacement calcaneal osteotomy (n=32) | 57 |
PTTD: Posterior tibialis tendon dysfunction, MCMS: Modified Coleman Methodology Score, FDL: Flexor digitorum longus, MDCO: Medial displacement calcaneal osteotomy, RA: Rheumatoid arthritis, MRI: Magnetic resonance imaging, PTT: Posterior tibial tendon, DM: Diabetes mellitus, TMTJ: Tarsometatarsal joint, OA: Osteoarthritis
| Reference | No. of patients (feet) | Post-operative regime |
|---|---|---|
| Robberecht J et al. | 24 (25) | NWB 6 weeks in below knee cast WBAT in boot for 4-6 weeks |
| Usuelli FG et al. | 42 (42) | NWB 4 weeks in short leg cast Progressive WB from 6 weeks onwards |
| Schuh R et al. | 49 (51) | NWB in equinovarus cast 2 weeks PWB for 4 weeks in a neutral cast |
| Niki H et al. | 25 (26) | Not stated |
| Chadwick C et al. | 31 (31) | Not stated |
| Silva MG et al. | 40 (43) | NWB 2 weeks in plantigrade position WBAT in boot from 2 weeks onwards |
| Marks RM et al. | 20 (20) | Not stated |
| Myerson MS et al. | 129 | First 52 patients : NWB in equinovarus cast 4 weeks Plantigrade cast or boot 4 weeks WBAT from 6 weeks onwards Next 77 patients: Cast for 2 weeks ROM exercises and WBAT in walker boot from 2 weeks onwards |
| Fayazi AH et al. | 23 (23) | NWB 6 weeks WBAT following radiographic evidence of consolidation |
| Wacker JT et al. | NWB in equinovarus cast for 2 weeks NWB in below knee cast in neutral position for 4 weeks WBAT from 6 weeks onwards |
|
| Toolan BC et al. | 36 (41) | NWB in below knee cast 6 weeks WBAT from 6 weeks onwards |
| Madhav RT et al. | 43 (43) | NWB in below knee cast with plantigrade foot and hindfoot inversion for 2 weeks, changing to a more neutral NWB cast at 2 weeks, and then at 4 weeks WB cast from 6 weeks onwards for a further 2 weeks |
| Knupp M et al. | 22 (22) | NWB cast for 2 weeks FWB in neutral foot position cast from 2 weeks for 4 weeks |
| Parsons S et al. | 32 (32) | TWB in below knee cast in slight equinus and hindfoot inversion for 4 weeks WBAT in neutral cast for 4 weeks |
| Osman AE et al. | 42 (42) | NWB in splint for 2 weeks, following by a short leg cast for 4 weeks WBAT in walker boot from 6 weeks onwards |
WB: Weightbearing, NWB: Non-weightbearing, PWB: Partial weightbearing, TBW: Total weightbearing, WBAT: Weightbearing as tolerated, ROM: Range of motion
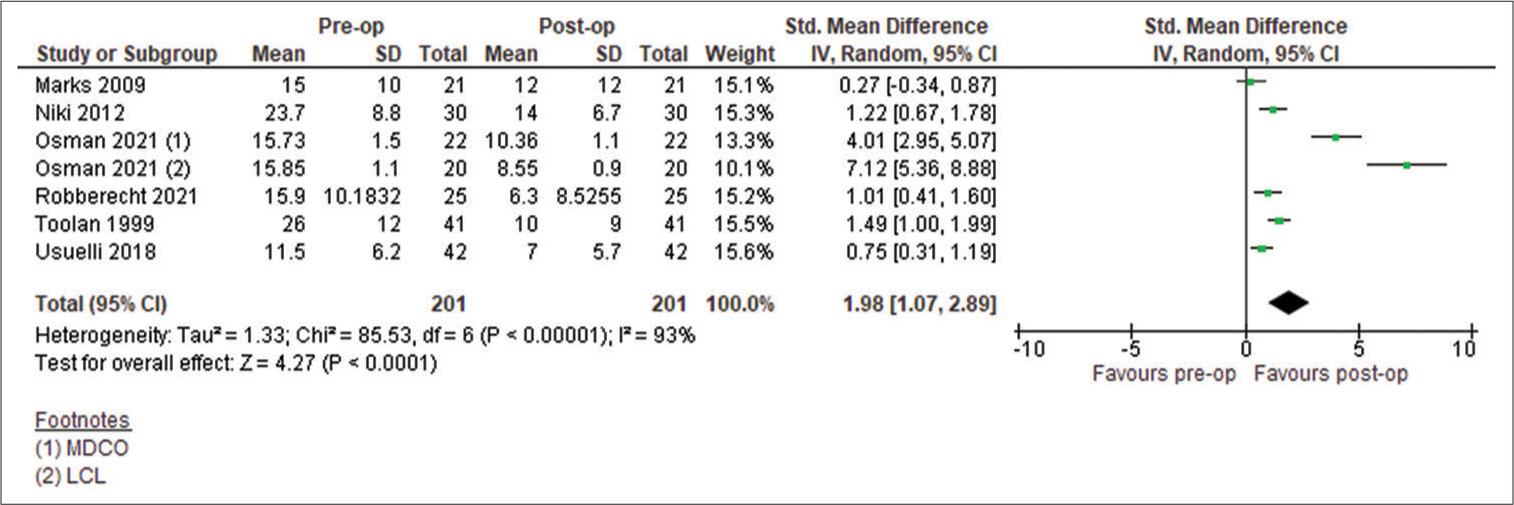
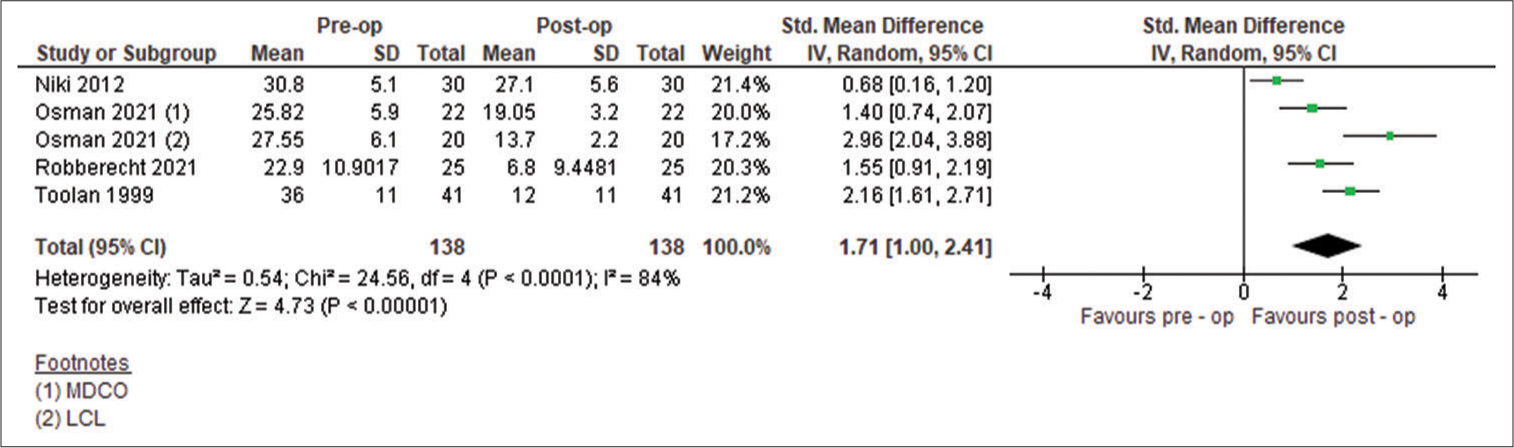
All studies demonstrated significant improvements in AOFAS scores and/or radiological outcomes (calcaneal pitch, Meary’s angle, TNCA) [Table 4]. 12 studies reported significant improvements in AOFAS total scores, of which only 3 could be used for meta-analysis purposes, as the others did not report their standard deviations or standard errors of the mean [Figure 5]. Papers that used the Cobb procedure only provided the mean changes in the AOFAS hindfoot scores seen, without any information on their standard deviations or their standard errors of the mean, and therefore, a comparison could not be made between the Cobb procedure and FDL tendon transfer.

- American Orthopaedic Foot and Ankle Society hindfoot scores pre-operatively versus postoperatively. MDCO: Medial displacement calcaneal osteotomy, LCL: Lateral column lengthening, SD: Standard deviation; Std.: Standard, CI: Confidence interval, IV: Inverse variance, Z: Z score, df: Degrees of freedom.
| Reference | No of patients (feet) | Mean follow-up (range) months | AOFAS | Radiological outcomes | Complications | ||
|---|---|---|---|---|---|---|---|
| Calcaneal pitch (degrees) | LTMA (degrees) | TNCA (degrees) | |||||
| Robberecht J et al. | 24 (25) | 26.4 (20.3–32.6) | Pre-op 44.8 (29.6–60.0) Post-op 67.8 (49.9–85.7)P=0.031 |
Pre-op 15.8 (13.0–18.6) Post-op 17.5 (15.0–20.0) P=0.001 |
Pre-op 15.9 (11.6–20.1) Post-op 6.3 (2.7–9.9) P<0.001 |
Pre-op 22.9 (18.4–27.3) Post-op 6.8 (2.9–10.7) P<0.001 |
Superficial wound infection (n=3) Surgery for removal of hardware (n=5) Other joint arthrosis (n=2) |
| Usuelli FG et al. | 42 (42) | 24 (18–31) | Pre-op 16.5 +/-4.6 Post-op 19.1 +/-5.0 P<0.01 |
Pre-op 11.5 +/-6.2 Post-op 7.0 +/-5.7 P<0.01 |
Superficial wound infection (n=1) Lateral heel paraesthesia (n=4) |
||
| Schuh R et al. | 49 (51) | 48 (12–146) | Pre-op 39.0 (25.0–78.0) Post-op 91.0 (77.0–100.0) P<0.001 |
Superficial wound infection (n=1) Sural nerve lesion (n=2) Reoperation due to hindfoot varus development (n=1) |
|||
| Niki H et al. | 25 (26) | Pre-op 13.3 +/-4.1 Post-op 16.9 +/-4.2 P=Not stated |
Pre-op 23.7 +/-8.8 Post-op 14.0 +/-6.7 P<0.005 |
Pre-op 30.8 +/-5.1 Post-op 27.1 +/-5.6 P=Not stated |
Superficial wound infection (n=2) Lateral heel paresthesia (n=4) |
||
| Chadwick C et al. | 31 (31) | 182.4 (136.8–198) | Pre-op 48.8 Post-op 90.3 (54–100) P<0.001 |
Revision surgery (n=2) Pain around metalwork (n=5) Superficial wound infection (n=3) DVT/PE (n=2) Sural nerve lesion (n=1) |
|||
| Silva MGAN et al. | 40 (43) | 24 | Pre-op 47.2 Post-op 83.1 P<0.001 |
Pre-op 8.4 Post-op 18.7 P=Not stated |
Pre-op 14.0 Post-op 1.3 P=Not stated |
Pre-op 35.6 Post-op 9.6 P=Not stated |
Deep wound infection (n=1) Sural nerve lesion (n=1) |
| Marks RM et al. | 20 (20) | 14.4 +/- 6.5 | Pre-op 14 +/-5 Post-op 20 +/-5.0 P<0.05 |
Pre-op 15.0 +/-10.0 Post-op 12.0 +/-12.0 P<0.05 |
Not stated | ||
| Myerson MS et al. | 129 (129) | 62.4 (36–146) | Pre-op 27 (9–45) Post-op 12 (0–33) P<0.05 |
Pre-op 37 (7–57) Post-op 16 (0–45) P=0.017 |
Revision surgery (n=3) Sural nerve lesion (n=3) Superficial wound infection (n=5) Medial plantar numbness (n=5) |
||
| Fayazi AH et al. | 23 (23) | 35 +/- 7 | Pre-op 50.0 (27.0–85.0) Post-op 89.0 (70.0–100.0) P<0.001 |
DVT (n=1) | |||
| Wacker JT et al. | 48 (48) | 51 (38–62) | Pre-op 48.8 Post-op 88.5 P=Not stated |
Revision surgery (n=2) Pain due to metalwork requiring removal (n=5) Superficial wound infections (n=3) Sural nerve lesion (n=1) Numbness around scars (n=6) DVT/PE (n=3) |
|||
| Toolan BC et al. | 36 (41) | 34 (24–50) | Pre-op 13 +/-6 Post-op 21 +/-6 P<0.0001 |
Pre-op 23 +/-14 Post-op 8 +/-8 P<0.0001 |
Pre-op 36 +/-11 Post-op 12 +/-11 P<0.0001 |
Non-union (n=8) Further procedures including removal of metalwork, revision surgery for non-union, loss of correction (n=29) |
|
| Madhav RT et al. | 43 (43) | 51.4 (10–83) | Pre-op 58.0 Post-op 85.0 P<0.0001 |
Partial nerve injuries (n=2) Minor oozing from wounds (n=4) Removal of metalwork (n=6) Subtalar joint OA development (n=2) |
|||
| Knupp M et al. | 22 (22) | 24 (12–46) | Pre-op 53.2 (40.0–68.0) Post-op 88.5 (78.0–94.0) P=Not stated |
Wound healing problems (n=1) Loss of sensation medial aspect of foot (n=1) Revision surgery (n=2) |
|||
| Parsons S et al. | 32 (32) | 61.2 (36–86.4) | Pre-op 52.2 (38.0–70.0) Post-op 89.0 (76.0–94.0) P=Not stated |
Superficial wound infection (n=1) Medial plantar nerve dysesthesia (n=1) |
|||
| Osman AE et al. | 42 (42) | 12 | Pre-op 42.73 and 44.80 for MDCO and LCL respectively Post-op 88.68 and 85.95 for MDCO and LCL respectively P<0.001 |
Pre-op 12.36 and 11.65 for MDCO and LCL respectively Post-op 13.95 and 17.0 for MDCO and LCL respectively P=0.006 and<0.001 respectively |
Pre-op 15.73 and 15.85 for MDCO and LCL respectively Post-op 10.36 and 8.55 for MDCO and LCL respectively P=0.001 and<0.001 respectively |
Pre-op 25.82 and 27.55 for MDCO and LCL respectively Post-op 19.05 and 13.70 for MDCO and LCL respectively P<0.001 |
Metalwork removal surgery (n=11) Wound dehiscence (n=1) |
AOFAS: American Orthopaedic Foot and Ankle Society, LTMA: Lateral talometatarsal angle, TNCA: Talonavicular coverage angle, DVT: Deep vein thrombosis, PE: Pulmonary embolism, MDCO: Medial displacement calcaneal osteotomy, LCL: Lateral column lengthening, OA: Osteoarthritis
Seven papers reported Meary’s angle and calcaneal pitch, whereas 6 described changes in the TNCA [Figures 6-8].
- Calcaneal pitch angles pre-operatively versus post-operatively. MDCO: Medial displacement calcaneal osteotomy, LCL: Lateral column lengthening, SD: Standard deviation; Std.: Standard, CI: Confidence interval, IV: Inverse variance, Z: Z score, df: Degrees of freedom.

- Lateral talometatarsal angles pre-operatively versus post-operatively. MDCO: Medial displacement calcaneal osteotomy, LCL: Lateral column lengthening, SD: Standard deviation; Std.: Standard, CI: Confidence interval, IV: Inverse variance, Z: Z score, df: Degrees of freedom.
- Talonavicular coverage angles pre-operatively versus post-operatively. MDCO: Medial displacement calcaneal osteotomy, LCL: Lateral column lengthening, SD: Standard deviation; Std.: Standard, CI: Confidence interval, IV: Inverse variance, Z: Z score, df: Degrees of freedom.
DISCUSSION
We performed a systematic review and meta-analysis on the outcomes following non-operative management and operative management (using either FDL tendon transfer or the Cobb procedure) for patients with PTTD. Our analysis suggests that both orthotics and physiotherapy can be used to treat early stages of PTTD, and surgical options involving either an FDL transfer or the Cobb procedure are viable options in combination with other soft tissue and/or bony procedures for later stages of the disease.
Despite the high prevalence of PTTD, few guidelines exist for the non-surgical management of stage I and II disease. The pathogenesis behind acquired flat foot deformity was thought to involve an inflammatory process around the PTT, resulting in tendinitis or tenosynovitis. However, recent studies suggest that the changes are secondary to a degenerative process.[8] Considering this, the non-operative management of PTTD has historically consisted of pain management while correcting the progressive deformity. Multiple orthotics exist for flatfeet, including the University of California Biomechanics Laboratory foot orthosis, solid ankle foot orthosis (AFO), and ankle braces; however, Augustin et al.[6] described the successful use of the Arizona AFO brace in the non-operative management of PTTD. The Arizona AFO brace is designed to slide into patients’ shoes and extends from the midshaft of the tibia to the metatarsal heads. In the study, 21 patients with PTTD were fitted with custom-made Arizona AFOs and evaluated over a two-year period.
Approximately 90% of patients reported decreased pain and increased function, which was similar to the findings by Lin JL et al.[24] who demonstrated that surgery was avoided in 69.7% of individuals with PTTD who wore a custom-designed AFO. Our study suggests that eccentric exercises appear to have a bigger impact on alleviating symptoms and improving quality of life when compared with stretching and/or concentric exercises in the non-operative management of PTTD. In concentric contraction, muscle fibers shorten under load while they elongate in eccentric contraction.[25] Eccentric calf muscle training is a well-established technique for improving muscle strength and power, with the theory being that progressive eccentric loading causes a stress reaction on muscle tissue, which in turn improves tolerance and helps avoid future injury,[26,27] a principle that was utilized by Kulig et al.[8] when they carried out a randomized controlled trial in patients with PTTD. The first arm of the trial had patients wearing custom orthoses and performing stretching exercises. Patients in the second arm additionally carried out concentric exercises, with those in the third arm doing eccentric exercises on top of stretching and wearing an orthosis. Their results showed that while the FFI improved in all 3 groups, the largest improvement was seen in patients carrying out eccentric tibialis posterior tendon exercises.
Unfortunately, a large part of any physiotherapy or orthotic regimen is patient compliance, which ultimately determines the effectiveness of the treatment program. Houck et al.[7] examined PTT force production in plantar flexion and forefoot adduction at baseline and at 6 and 12 weeks following isotonic strengthening exercises against band resistance. This was in comparison to a group who participated in tendon stretching exercises only. Both groups wore orthotics in conjunction, and both exercise programs were home-based. Although improvements were seen in both pain and function, minimal differences were noted between treatment groups. The results identify the importance of patient adherence to a specific exercise program. Without close supervision, actual load may not be adequate to elicit changes in musculotendinous strength.[28]
In our study, 12 of the 15 studies for the surgical management of PTTD involved transfer of the FDL tendon, of which only 1 study was a randomized controlled trial. In the majority of cases, patients underwent an MDCO followed by harvesting of the FDL tendon and transferring it to the navicular. Other procedures carried out at the same sitting included LCL, cotton osteotomy, Achilles tendon lengthening, spring ligament repair, and deltoid ligament reconstruction.[9-19,23] The variety of soft tissue and bony procedures that can be carried out to correct a flatfoot deformity indicates not only how complex the disease process is but also demonstrates that surgery for planovalgus foot correction has to be customized for each individual patient. The decision to add additional soft tissue and bony procedures depends on the degree of correction that is achieved following the initial calcaneal osteotomy and FDL transfer.
The Cobb procedure offers an alternative to the FDL tendon transfer using the tibialis anterior tendon instead, which is split, with the lateral half of the tendon being harvested and utilized to either reinforce or reconstruct the PTT. This, too is often combined with additional soft tissue and bony procedures to correct the planovalgus foot deformity. The studies included in this review demonstrate that the results in terms of improvement in PROMs and radiological outcomes are equivalent to those of patients undergoing an FDL tendon transfer. The advantage of the Cobb procedure over the FDL transfer is that it involves making a bony tunnel in the medial cuneiform and passing the harvested split tibialis anterior tendon to the plantar aspect through it, after which it is sutured to the remnant of the PTT. This avoids having to drill through the navicular, which is routinely done when using the FDL tendon, which, in theory, allows the surgeon to carry out a spring ligament repair or reconstruction without any limitations if needed.[29] Furthermore, Knupp and Hintermann[21] tested the power of the tibialis anterior tendon in the 22 patients included in their study and found that none had decreased tibialis anterior power compared to the contralateral foot. The main drawback of the procedure, however, is that the peroneal tendons can overcome the stabilization provided by the harvested tibialis anterior tendon, causing a recurrence of the planovalgus deformity of the foot.[30]
The biggest limitation of this review is the heterogeneity of the included studies, starting from the patient population (age ranging from 18.9 to 81 years), surgical technique, postoperative rehabilitation, and follow-up duration. Moreover, a large number of patients had additional soft tissue and bony procedures performed concurrently (spring ligament plication, Achilles tendon lengthening), and it is difficult to quantify the effect that those procedures may have had on the PROMs and radiological outcomes.
CONCLUSION
This study demonstrates that the non-operative treatment of PTTD with orthoses along with stretching and strengthening exercises has more favorable outcomes than orthoses and stretching alone. Both FDL transfer and the Cobb procedure improve functional and radiological outcomes and are viable options for the surgical management of PTTD. However, this study identifies the lack of data available, especially for the Cobb procedure. Few large-scale randomized controlled trials exist, meaning the superiority of one method over the other cannot be proven. Ultimately, the goal of surgery is to correct the deformity to allow patients to have a shoe-able, pain-free foot, and the decision as to whether the Cobb procedure or FDL tendon transfer is performed must be determined by the surgeon, depending on each individual patient. This study highlights the lack of high-quality published literature on the management of PTTD and the need for randomized controlled trials in the future.
Author contributions:
VA and RT: Writing of the paper and data analysis; LHW and SO'N: Data analysis and methodology; JM: Design of the paper and overall lead; PD: Literature review and data analysis; RV: Design of paper. All the authors were involved in conceptualization, literature search, design, data analysis, manuscript writing, editing, and final approval.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- Adult-acquired flatfoot deformity: Etiology, diagnosis, and management. JBJS Rev. 2017;5:e7.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of symptomatic posterior tibialis tendon dysfunction in women over the age of 40 in England. Foot Ankle Surg. 2009;15:75-81.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior tibial tendon dysfunction. Treatment by flexor digitorum longus transfer. Foot Ankle Clin. 2001;6:77-87.
- [CrossRef] [PubMed] [Google Scholar]
- Tendon transfer options in managing the adult flexible flatfoot. Foot Ankle Clin. 2012;17:205-26.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of posterior tibial tendon dysfunction without flexor digitorum tendon transfer: A retrospective study of 34 patients. J Foot Ankle Surg. 2011;50:293-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nonoperative treatment of adult acquired flat foot with the Arizona brace. Foot Ankle Clin. 2003;8:491-502.
- [CrossRef] [PubMed] [Google Scholar]
- Randomised controlled trial comparing orthosis augmented by either stretching or stretching and strengthening for stage II tibialis posterior tendon dysfunction. Foot Ankle Int. 2015;36:1006-16.
- [CrossRef] [PubMed] [Google Scholar]
- Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: A randomised controlled trial. Phys Ther. 2009;89:26-37.
- [CrossRef] [PubMed] [Google Scholar]
- Limited plantar incision for flexor digitorum longus tendon harvest in surgical treatment of tibialis posterior tendon insufficiency. Foot Ankle Surg. 2021;27:15-9.
- [CrossRef] [PubMed] [Google Scholar]
- Return to sport activities after medial displacement calcaneal osteotomy and flexor digitorum longus transfer. Knee Surg Sports Traumatol Arthrosc. 2018;26:892-6.
- [CrossRef] [PubMed] [Google Scholar]
- Flexor digitorum longus transfer and medial displacement calcaneal osteotomy for the treatment of stage II posterior tibial tendon dysfunction: Kinematic and functional results of fifty one feet. Int Orthop. 2013;37:1815-20.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of medial displacement calcaneal osteotomy for correction of adult-acquired flatfoot. Foot Ankle Int. 2012;33:940-6.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term follow up of flexor digitorum longus transfer and calcaneal osteotomy for stage II posterior tibial tendon dysfunction. Bone Joint J. 2015;97:346-52.
- [CrossRef] [PubMed] [Google Scholar]
- Results of operative correction of grade IIB tibialis posterior tendon dysfunction. Foot Ankle Int. 2015;36:165-71.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical reconstruction of posterior tibial tendon dysfunction: Prospective comparison of flexor digitorum longus substitution combined with lateral column lengthening or medial displacement calcaneal osteotomy. Gait Posture. 2009;29:17-22.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot Ankle Int. 2004;25:445-50.
- [CrossRef] [PubMed] [Google Scholar]
- Intermediate term follow-up of calcaneal osteotomy and flexor digitorum longus transfer for treatment of posterior tibial tendon dysfunction. Foot Ankle Int. 2002;23:1107-11.
- [CrossRef] [PubMed] [Google Scholar]
- Calcaneal osteotomy and transfer of the tendon of flexor digitorum longus for stage II dysfunction of tibialis posterior. Three to five year results. J Bone Joint Surg Br. 2002;84:54-8.
- [CrossRef] [PubMed] [Google Scholar]
- Complex reconstruction for the treatment of dorsolateral peritalar subluxation of the foot. Early results after distraction arthrodesis of the calcaneocuboid joint in conjunction with stabilisation of, and transfer of the flexor digitorum longus tendon to, the midfoot to treat acquired pes planovalgus in adults. J Bone Joint Surg Am. 1999;81:1545-60.
- [CrossRef] [PubMed] [Google Scholar]
- Cobb procedure and Rose calcaneal osteotomy for the treatment of tibialis posterior tendon dysfunction. Acta Orthop Belg. 2009;75:64-9.
- [Google Scholar]
- The Cobb procedure for treatment of acquired flatfoot deformity associated with stage II insufficiency of the posterior tibial tendon. Foot Ankle Int. 2007;28:416-21.
- [CrossRef] [PubMed] [Google Scholar]
- Correction and prevention of deformity in type II tibialis posterior dysfunction. Clin Orthop Relat Res. 2010;468:1025-32.
- [CrossRef] [PubMed] [Google Scholar]
- Medial displacement calcaneal osteotomy versus lateral column lengthening to treat stage II tibialis posterior tendon dysfunction, a prospective randomised controlled study. Foot (Edinb). 2021;47:101798.
- [CrossRef] [PubMed] [Google Scholar]
- Results of non-surgical treatment of Stage II posterior tibial tendon dysfunction: A 7-to 10-year followup. Foot Ankle Int. 2008;29:781-6.
- [CrossRef] [PubMed] [Google Scholar]
- Concentric and eccentric: Muscle contraction or exercise? Sports Health. 2013;5:306.
- [CrossRef] [PubMed] [Google Scholar]
- Autoregulation in resistance training for lower limb tendinopathy: A potential method for addressing individual factors, intervention issues, and inadequate outcomes. Front Physiol. 2021;12:704306.
- [CrossRef] [PubMed] [Google Scholar]
- Eccentric muscle contractions: Risks and benefits. Front Physiol. 2019;10:536.
- [CrossRef] [PubMed] [Google Scholar]
- Exercise for posterior tibial tendon dysfunction: A systematic review of randomised clinical trials and clinical guidelines. BMJ Open Sport Exerc Med. 2018;4:e000430.
- [CrossRef] [PubMed] [Google Scholar]
- The Cobb procedure for stage II posterior tibial tendon dysfunction. Clin Podiatr Med Surg. 1999;16:471-7.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the Cobb procedure in the treatment of posterior tibial tendon dysfunction. Clin Podiatr Med Surg. 2002;19:371-89.
- [CrossRef] [PubMed] [Google Scholar]







