Translate this page into:
Ochronotic arthropathy knee-arthroscopic diagnosis and treatment – A case report
*Corresponding author: Dr. Sumit Jain Sethia, Department of Orthopedics, Calcutta Medical Research Institute (CMRI) Hospital, Kolkata, West Bengal, India. sumitjain41@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Narvekar A, Jain Sethia S. Ochronotic arthropathy knee-arthroscopic diagnosis and treatment – A case report. J Arthrosc Surg Sports Med. 2023;4:48-52. doi: 10.25259/JASSM_31_2022
Abstract
Ochronotic arthropathy is a rare hereditary disorder found in patients with Alkaptonuria due to a deficiency of Homogentisic acid oxidase. It is associated with the deposition of homogentisic acid derivatives in various connective tissues, causing characteristic pigmentation known as ochronosis. Due to its clinical resemblance to that of a degenerative disorder, the diagnosis of ochronotic arthropathy usually occurs intraoperatively. This case report is of a 56-year-old male who presented with complaints of pain and swelling in the right knee. Clinical examination and MRI findings were correlated to reveal a tear of the lateral meniscus. On arthroscopy, the blackish-brown pigmentation of the meniscus and the articular cartilage led to a diagnosis of ochronotic arthropathy. The pathology and biochemistry studies further support this. Arthroscopy plays an important tool in terms of the management of patients with ochronosis. The characteristic findings, in this case, report may help in establishing the diagnosis of ochronotic arthropathy without other systemic presentations. It can help in delaying inevitable progression and allow patients to be pain-free for longer periods. Arthroscopy delays the need for arthroplasty.
Keywords
Arthroscopy
Alkaptonuria
Ochronosis
Ochronotic arthropathy
INTRODUCTION
Alkaptonuria is a rare autosomal recessive disorder due to a deficiency of the enzyme homogentisic acid oxidase (HGAO), which is involved in the metabolism of amino acids such as phenylalanine and tyrosine. Due to partial or total deficiency of HGAO, homogentisic acid accumulates in the blood, and part is excreted in the urine.[1] The incidence of alkaptonuria is estimated to be 1:250,000–1:1,000,000 live births.[2]
On exposure to the atmosphere, urine containing homogentisic acid gradually darkens to a black color. Homogentisic acid and its oxidation products accumulate, especially in the cartilage and tendons. It is also reported to be deposited extra-articularly in the skin, tympanic membrane, heart valves, sclera, cartilages of nose and ears, kidneys, pancreas, and large vessels.[3] Due to the high affinity for fibrillar collagen, this pigment affects the hyaline cartilage of the larger peripheral joints. This results in decreased cross-linkage of collagen, thereby making it more susceptible to mechanical stress.[4] This causes the cartilage to become brittle and fragmented, which loads the subchondral bone, leading to inflamed synovium, thereby resulting in “ochronotic arthropathy.”[5] The development of degenerative arthritis with accompanying brownish-black pigmentation of the tissues and dark discoloration of the urine is called “ochronosis.” Ochronosis was first described in 1866 by Virchow during a necropsy; he found pigmentation of the tissues caused by the deposition of ochre-colored granules.[6] Gross and Allard (1907) noted the overwhelming incidence of arthritic changes in some patients with alkaptonuria, and the pigmentation of joint cartilage was described by Clemens (1907).
The manifestation of clinical symptoms of ochronotic arthropathy is revealed after the fourth decade of life. Clinical diagnosis is made on the basis of skeletal manifestations, including low back pain, stiffness, degenerative arthropathy of the large joints, ochronotic pigmentation of the tissues, and blackish urine. The definitive diagnosis of alkaptonuria is confirmed with several biochemical tests for the quantitative presence of homogentisic acid in urine and enzyme analysis. To date, there is no effective medical treatment available for alkaptonuria. Symptomatic treatment at present is by local heat, physiotherapy, analgesics, external support, and surgical treatment in the form of synovectomy, arthroscopic debridement, fusion, or arthroplasty as indicated regarding the affected joint.[7,8]
In this article, our purpose is to present a patient who was diagnosed to have alkaptonuria during further laboratory tests after observing initial ochronotic brownish-black pigmentation of the menisci and femoral-tibial cartilage during arthroscopy of the knee. This hastens his diagnosis, improves his lifestyle by reducing pain, and delays any further complications.
CASE REPORT
A 56-year-old male who is known as diabetic and hypertensive presented with long-lasting dull, aching low back pain with small joint pain of hand and morning stiffness for ten years and concurrent bilateral knee pain over a period of two years. His symptoms necessitated the use of nonsteroid anti-inflammatory drugs (NSAID) on a daily basis, but his right knee pain gradually worsened, restricting his daily activities, and he decided to have arthroscopy. In the past, he was operated on for intertrochanteric femur fracture in 2010 and oral carcinoma in 2017.
Clinical findings
His physical examination revealed right knee crepitation and swelling. There was lateral joint line tenderness, McMurray tested positive for lateral meniscus, and Lachmann was clinically negative. Terminal flexion is painful and restricted. Neurological examination was normal.
Diagnostic assessment
Orthoscangram [Figure 1a] shows lateral compartment Osteoarthritis. Plain Radiograph of Knee [Figure 1b] showed grade-2 osteoarthritis with osteopenia.

- (a) Orthoscanogram showing lateral compartment osteoarthritis of the right knee and (b) radiograph knee showing grade 2 osteoarthritis changes with osteopenia.
Magnetic resonance imaging [Figures 2a and b] revealed minimal effusion, bone edema, degenerative complex grade-3 tear of the lateral meniscus along with mucoid degeneration in the anterior cruciate ligament/posterior cruciate ligament, and degenerative cartilage lesion in the right knee joint. The patient was planned for arthroscopic synovectomy with partial Meniscectomy and debulking of Lateral Meniscus done.
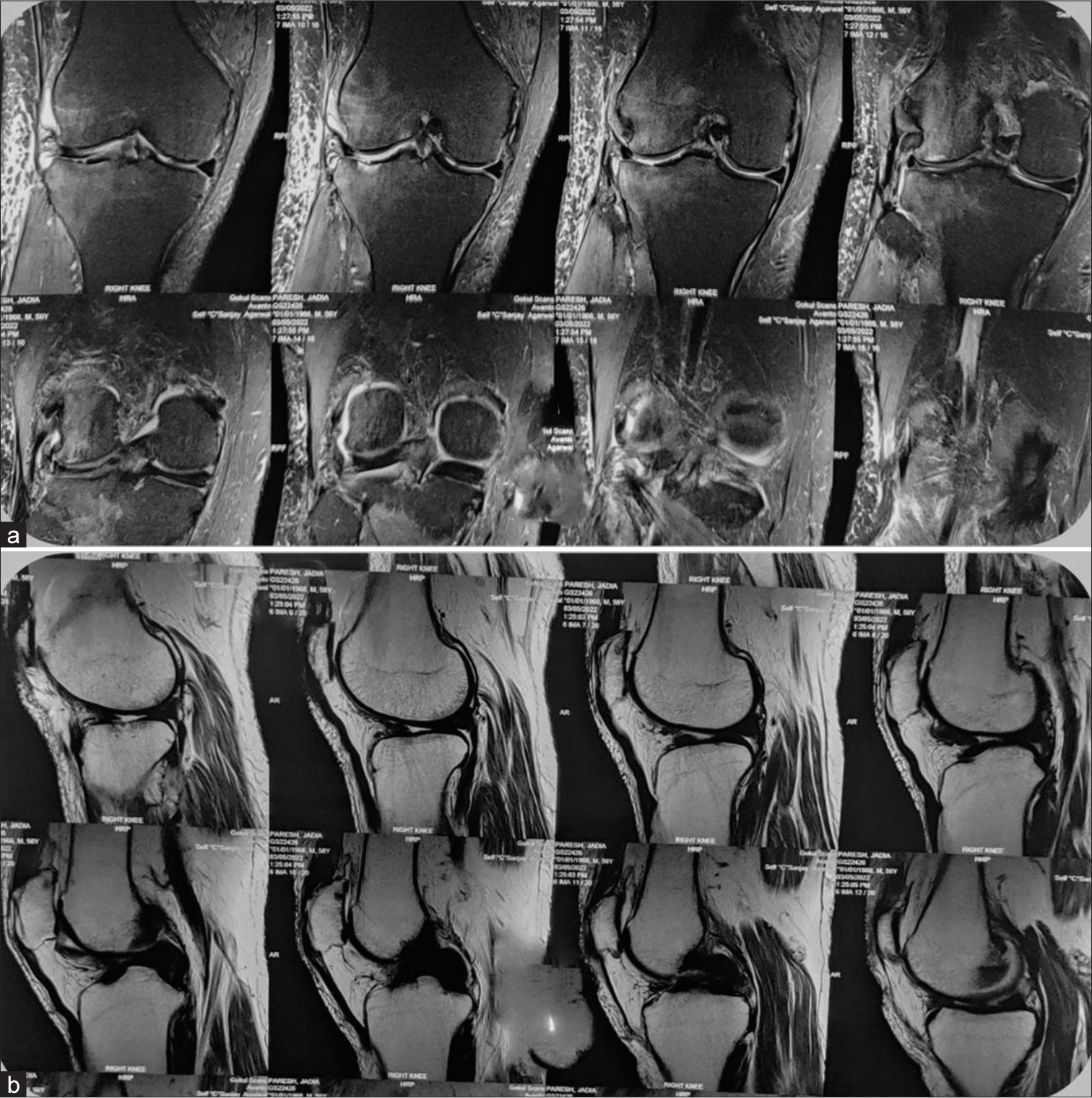
- (a) Magnetic resonance imaging of coronal section showing cartilage degeneration of both compartments. (b) Sagittal section showing grade 3 complex tear of lateral meniscus with mucoid changes of cruciate.
Differential diagnosis
Pigmentary disorder of the knee, like hemochromatosis.
Therapeutic intervention
The arthroscopic findings were astonishing and revealed synovial hypertrophy with blackish-pigmented synovium [Figure 3]. There were chondral defects of size 2 × 3 cm over the lateral condyle and 0.5 × 0.5 cm over the medial condyle. There were pigmented loose bodies with sizes varying from 0.5 mm to 5 mm. ICRS Grade IV cartilage changes in the lateral femoral condyle and Grade 3b changes in the medial femoral condyle were observed with grayish-black discoloration. Both the menisci were discolored with tears in the lateral meniscus [Figure 4]. Although the integrity of all the ligaments was maintained, there was evident discoloration and mucoid changes present. Arthroscopic partial lateral meniscectomy with balancing, removal of loose body, and debridement of hypertrophied discolored synovium was done. With the suspicion of ochronotic arthropathy due to such incidental arthroscopic finding, the specimen [Figure 5] was sent for histopathological examination, and further examination and investigations were planned.
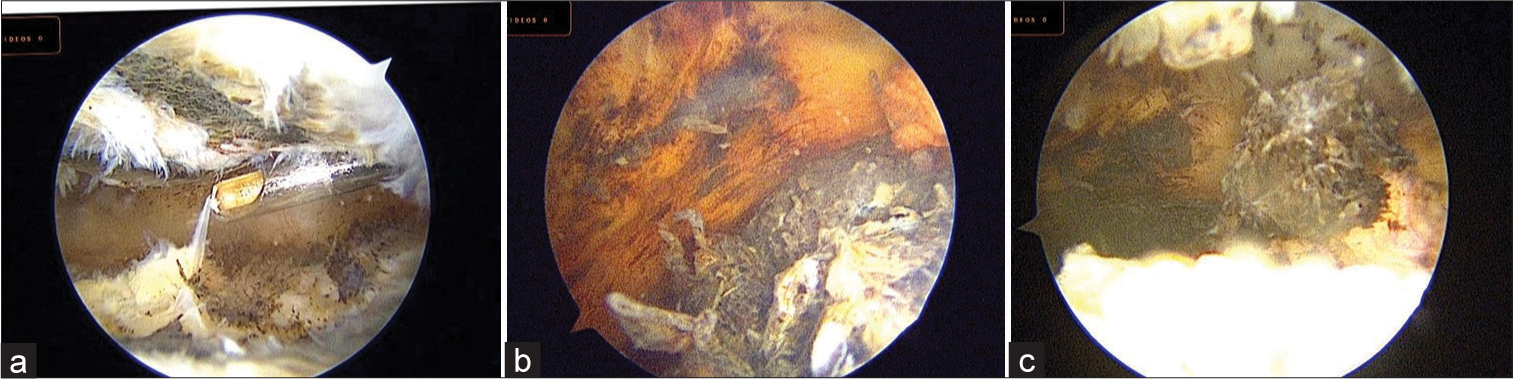
- (a-c) Arthroscopic image of a knee joint showing synovial hypertrophy with blackish-brown pigmentation with loose body.
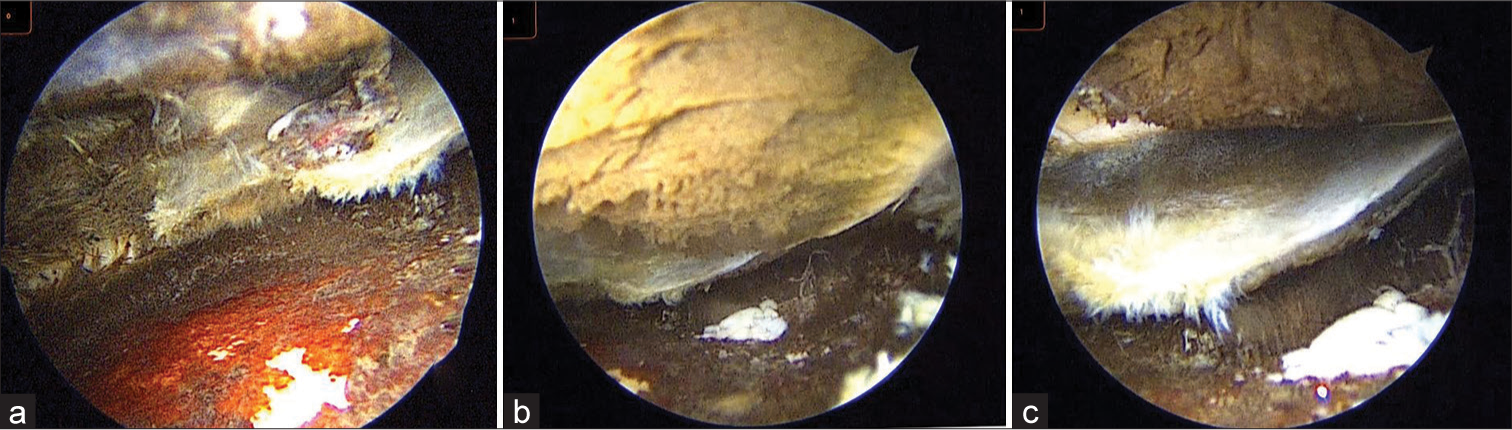
- Arthroscopic image (a-c) of a knee joint showing (a) blackish-brown discoloration with degenerated lateral meniscus, (b) cartilage loss at femoral condyle, and (c) torn cartilage flap floating in the knee joint.

- Intraoperative specimen of blackish-brown tissue.
Serum ferritin and transferrin saturation were within range, and it ruled out hemochromatosis. Urine was normal in color but turned dark brown when tested with sodium hydroxide and Iron(III) chloride test was positive. Urine showed high levels of homogentisic acid. Histopathological reports revealed irregular bits of deep brown colored cartilage embedded in the synovium suggestive of ochronosis. Later, detailed examination of the skin, sclera, eye, and ear showed blackish discoloration of eye and ear lobule. Patient achieved immediate pain relief after the arthroscopic intervention. Treatment was initiated by administering Vitamin C and NSAID, and he was discharged consequently.
Follow-up and outcomes
Postoperatively, a physical therapy rehabilitation program was started, and his complaints in the subsequent follow-up diminished, and his lifestyle improved.
DISCUSSION
Ochronotic arthropathy is a rare disorder found in patients with alkaptonuria. Only a few reports of arthroscopic diagnosis and treatment of ochronosis have been found in the literature.[9-12] Alkaptonuria was one of the diseases described by Sir Archibald Edward Garrod as being the result of the accumulation of intermediates due to metabolic deficiencies. He linked ochronosis with the accumulation of alkaptans in 1902.[13] At present, no cure has been found for ochronosis or alkaptonuria. The rare prevalence of the disease makes it difficult to form a consensus on surgical treatment options. The literature highlights the arthroscopic findings of ochronosis observed in the knee and some in the hip and shoulder.[3,9,11] Case reported by Thacker et al.[11] described the arthroscopic findings in a 40-year-old male with multiple joint involvement.
The findings revealed pigmented hypertrophic synovium with loose bodies in the knee joint. The patient did exhibit grayishblackish discoloration of the meniscus and articular surface; similar findings were observed in our case. During arthroscopy, brownish-black discoloration of the articular cartilage and menisci desired us to do further research and investigate the patient for ochronosis. The findings of pigmented hypertrophic synovium with loose bodies and lack of involvement of ligamentous structures, though less pliable than normal, were similar in our case.[11] The involvement of the lateral meniscus in our case was ochronotic arthropathy. Our arthroscopic findings were consistent with those of other cases in the literature. Generalized synovial hypertrophy accompanying brownish-black discoloration of articular cartilage and menisci were our common arthroscopic finding, which is consistent with the findings reported by Chen et al.,[9] Kural et al., [14] and Raaijmaaker et al.[8] where the patient had a degenerative tear of the menisci for which partial meniscectomy was performed. Generalized cartilage degeneration found in our case has also been reported consistently in the literature.[9,13] Calcification with narrowing of intervertebral discs [Figure 6] and Generalized Osteophyte in x-ray is correlated with similar cases in literature.[15] Ochronosis is one of the clinical manifestations of alkaptonuria. Approximately 50% of patients with alkaptonuria in their 40s show ochronosis. They present with ochronotic sclera pigmentation, degenerative joints, and characteristic urinary changes.[16,17] Diagnosis can be made during childhood by observing the dark coloration of diapers or urine when left in the air. Ochronotic discoloration of the cartilage of the ears and nose may be observed at the age of 30. Other less common extra-articular manifestations are ochronosis of the heart with valve stenosis and urinary tract obstruction by ochronotic calculi. In our patient, there was blackish discoloration of the eye and ear lobule. No curative treatment for this disease exists. Treatment with a high dose of ascorbic acid proved to lower the levels of homogentisic acid in excreted urine[8] but did not prevent the occurrence of arthropathy. Nitisinone is shown to have significantly altered the excretion of homogentisic acid in urine in both human and rat studies.[18] Since there is no effective treatment to replace the deficient enzyme, symptomatic treatment is initiated with NSAIDs, intra-articular steroid injection, and ascorbic acid. Arthroscopic debridement, synovectomy, partial or total joint arthroplasties, and fusion are the surgical treatment options.[7,8,10] Arthroplasty seems to be the best choice for patients whose symptoms persist despite conservative treatment. Raaijmaakers et al.[8] reported to provide symptomatic relief by administering 400 mg/day chondroitin sulfate and 1500 mg/day glucosamine for four months.

- Radiograph of spine showing intervertebral joint calcification with degenerative changes.
Arthroscopy in ochronotic arthropathy is recommended for diagnostic and therapeutic purposes. It helps to reduce pain and swelling and also improves range of motion. Removal of loose bodies and debridement of the frayed tissue can further reduce the insult to the articular cartilage. This helps in slowing down the rate of cartilage degeneration, thereby delaying the need for arthroplasty.
CONCLUSION
Arthroscopy plays an important tool in terms of therapeutic and diagnostic in the management of patients with ochronosis. The characteristic incidental findings in this case report may help in establishing the diagnosis of ochronotic arthropathy without other systemic presentations.
Interesting case; why?
Initial clinicoradiological presentation mimicked degenerative lateral meniscus tear with synovitis . On arthroscopy, it was incidentally diagnosed as a black pigmented knee, which, in literature, is termed as OCHRONOSIS. Later biochemical and pathological investigations confirmed it to be ALKAPTONURIA.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Use of nitisinone in patients with alkaptonuria. Metabolism. 2005;54:719-28.
- [CrossRef] [PubMed] [Google Scholar]
- Natural history of alkaptonuria. N Engl J Med. 2002;347:2111-21.
- [CrossRef] [PubMed] [Google Scholar]
- Ochronotic arthropathy: The black hip. Case report and review of the literature. Acta Orthop Belg. 1997;63:122-5.
- [Google Scholar]
- The role of calcified cartilage and subchondral bone in the initiation and progression of ochronotic arthropathy in alkaptonuria. Arthritis Rheum. 2011;63:3887-96.
- [CrossRef] [PubMed] [Google Scholar]
- Ochronotic arthropathy: Case report and review of the literature. Int Orthop. 1999;23:122-5.
- [CrossRef] [PubMed] [Google Scholar]
- A case of general ochronosis of the cartilage and cartilage-like parts. Arch Path Anat. 1866;37:212-9.
- [CrossRef] [Google Scholar]
- Ochronotic arthropathy. A review with four case reports. J Bone Joint Surg Br. 1970;52:653-66.
- [CrossRef] [Google Scholar]
- Ochronosis, arthroscopy of a black knee: A case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2008;16:182-4.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic diagnosis and management of ochronotic arthropathy of the knee. Arthroscopy. 2001;17:869-73.
- [CrossRef] [PubMed] [Google Scholar]
- Alkaptonuria and ochronotic arthropathy. Arthroscopic and intraoperative findings in implantation of a knee joint surface replacing prosthesis. Chirurg. 1994;65:1061-5.
- [Google Scholar]
- Ochronotic arthropathy: Arthroscopic findings in the shoulder and the knee. Arthroscopy. 2003;19:E14-7.
- [CrossRef] [PubMed] [Google Scholar]
- Knee arthroscopy in a case of ochronotic arthropathy. Ital J Orthop Traumatol. 1992;18:107-10.
- [Google Scholar]
- The incidence of alkaptonuria: A study in chemical individuality. Lancet. 1902;2:1616-20.
- [CrossRef] [Google Scholar]
- Knee ochronotic arthropathy and arthroscopic findings. Acta Orthop Traumatol Turc. 2009;43:67-71.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic and MRI findings in ochronosis. Radiol Med. 2005;110:349-58. English, Italian
- [Google Scholar]
- The pathology of alkaptonuric ochronosis. Hum Pathol. 1989;20:40-6.
- [CrossRef] [PubMed] [Google Scholar]
- Alkaptonuria--a review of surgical and autopsy pathology. Histopathology. 2008;53:503-12.
- [CrossRef] [PubMed] [Google Scholar]
- A 3-year randomized therapeutic trial of nitisinone in alkaptonuria. Mol Genet Metab. 2011;103:30714.
- [CrossRef] [PubMed] [Google Scholar]






