Translate this page into:
Radiological evaluation of glenoid bone reaction following arthroscopic Bankart repair using all-soft suture anchors
*Corresponding author: V Nagendra, Department of Orthopaedics, Maulana Azad Medical College, New Delhi, India. nagendrav7NAYAK@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nagendra V, Kumar V, Sabat D. Radiological evaluation of glenoid bone reaction following arthroscopic Bankart repair using all-soft suture anchors. J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_40_2024
Abstract
Objectives
Glenohumeral instability is one of the most common orthopedic problems encountered in the clinical practice. Anterior shoulder instability accounts for 90% of total cases of shoulder instability. Bankart lesion (Avulsion of anteroinferior glenoid labrum) occurs as a sequela to anterior dislocation in the majority of cases, which, in turn, predisposes to recurrent shoulder instability. Arthroscopic Bankart repair using all-soft suture anchors is currently being considered as an advanced method in the management of Bankart lesions due to the better understanding of pathology behind the recurrent instability and greater experience among surgeons regarding the usage of suture anchors. Our study focused on assessing radiological outcomes following the implantation of all-soft suture anchors using advanced radiological imaging (computed tomography [CT]) in the post-operative period.
Materials and Methods
We used 43 all-soft suture anchors (24 single-loaded and 19 double-loaded) in 15 patients managed by arthroscopic Bankart repair. The suture anchors were assessed radiologically using CT at regular intervals (6 and 12 months). The peri-implant changes (Glenoid Bone reactions) in the post-operative period were assessed as per the study conducted by Tompane et al. and Ruiz Ibán et al.
Results
In our study, none of the anchors showed complete resorption or grade 0 changes. Partial bony defect or erosions were identified in 14 out of 43 anchors and 21 out of 43 anchors in the first and second CT, respectively. We found tunnel dilation or grade 2 changes in 26 anchors in first CT which reduced to 19 in the second CT. Three peri-anchor cystic lesions were identified in the first CT which remained the same on subsequent serial imaging.
Conclusion
Overall performance of all-soft suture anchors in arthroscopic Bankart repair is comparable to that of previous generation suture anchors in terms of clinical and functional outcomes. Serial radiological assessment (CT-based) of all-soft suture anchors following implantation showed some changes in the glenoid bone following insertion, which showed a tendency toward healing on serial evaluation in the majority of cases.
Keywords
All-soft suture anchors
Arthroscopic Bankart lesion
Bankart lesion
Glenoid bone reaction
Radiological outcomes
INTRODUCTION
Glenohumeral joint instability is one of the most common orthopedic problems encountered in the current population especially among young males, athletes, and those involved in contact sports.[1] Anterior dislocation is the most frequent type of shoulder instability accounting for about 90% of the total cases.[1] Bankart lesion paves the way for recurrent anterior shoulder instability by creating a pocket in front of the glenoid bone of the scapula, allowing the humeral head to frequently dislocate into it.[2] The surgical management techniques for the repair of the lesion have been constantly evolving since the last century. With the advancement in arthroscopic techniques and instrumentation, minimal invasiveness and increasing scientific evidence revealing similar clinical outcomes between patients undergoing open versus arthroscopic techniques, there has been a significant shift toward the arthroscopic Bankart repair with suture anchors being utilized as the first line of surgical management in recent times. The most significant advantage of the suture anchor method is that the glenohumeral ligament-labrum complex is directly sutured to the glenoid rim, inducing very good healing between the bone and ligament-labrum complex while also allowing detailed evaluation of coexistent intra-articular pathologies.[3]
There have been many developments in the structure and composition of these glenoid anchors.[4] Initially, metallic and bio-absorbable anchors were used but soon fell out of practice due to complications arising following their usage. Complications such as chondral damage, articular protrusion, anchor migration, foreign body reactions, and osteolysis which led to decreased bone stock and increased incidence of post-operative glenoid rim fractures paved way for the emergence of a newer type of suture anchor system – “all-soft suture anchors.”
These all-soft suture anchors (ASSAs) offer reduced bone resection due to smaller drill hole compared to classical suture anchors (1.4 mm vs. 3 mm), equivalent clinical results and ultimate load-to-failure as that of solid anchor systems.[5,6] Some recent researches have shown increasing evidence of osteolysis following the usage of ASSAs with majority being animal studies.[7] Although all-soft suture anchors offer a wide range of favorable advantages when compared to its counterparts, there are limited sequential studies executed to check for the incidence, prevalence, and time dependence of glenoid bone reactions following the implantation of all-soft suture anchors.
Aims and objectives
The aim of our clinical study was to evaluate the glenoid bone reactions following the usage of all-soft suture anchors at different post-operative time periods using radiological imaging techniques (Non-contrast-enhanced computed tomography [NCCT]).
MATERIALS AND METHODS
Eligibility criteria and clinical evaluation
The study was conducted after taking the appropriate approval of the Institutional Ethical Board. The study type was prospective observational study. All eligible patients with shoulder instability who underwent arthroscopic Bankart repair in our institution using all-soft suture anchors with at least 6 months follow-up post-surgery were recruited. These patients were followed up for a period of 1 year after informing regarding the purpose of study and potential risks and benefits associated with it. All patients who underwent revision surgery, sustained re-trauma or infection and those who refrained from giving their consent were excluded promptly.
A total of 15 patients with 43 anchors, meeting the inclusion and exclusion criteria were prospectively enrolled for our study. Relevant clinical history was obtained regarding the demographic details and chief complaints at the time of presentation such as pain, instability, subluxation, and dislocation. Relevant details regarding the surgical procedures, such as date of surgery, operated site, technique used (biodegradable/all-soft suture anchors), number of anchors, and anchor positions, were obtained from the patient’s case files. Relevant physical examination in the form of anterior apprehension and assessment of anterior translation clinically followed by functional assessment using Rowe and Western Ontario shoulder instability index (WOSI) scoring system were done at the 6th and 12th month follow-up.
Radiological evaluation
All patients were advised to undergo NCCT using 128 slice multidetector computed tomography scanner, of their operated glenohumeral region in supine position. The scan was limited to 6–8 cm distance spanning the glenohumeral joint with 1 mm slice thickness. The scan data were displayed through picture archive and communication system and the measurements were standardized to reduce the inter- and intraobserver variability. The DICOM format was imported to RadiAnt DICOM viewer software 2020.2 version and later evaluated for the presence and absence of glenoid bone reactions and further quantified if present.
Tunnel diameter was defined as “the average of the greatest width of the hole measured perpendicular to the direction of suture anchor insertion in axial, sagittal, and oblique coronal planes.” The largest diameter (D) on the axial, oblique coronal, and sagittal image was measured perpendicular to the direction of the anchor and the average of all three diameters was recorded as the width of the tunnel [Figure 1]. Quantification of glenoid bone reactions [Table 1] was graded based on Ruiz Ibán et al.[8]
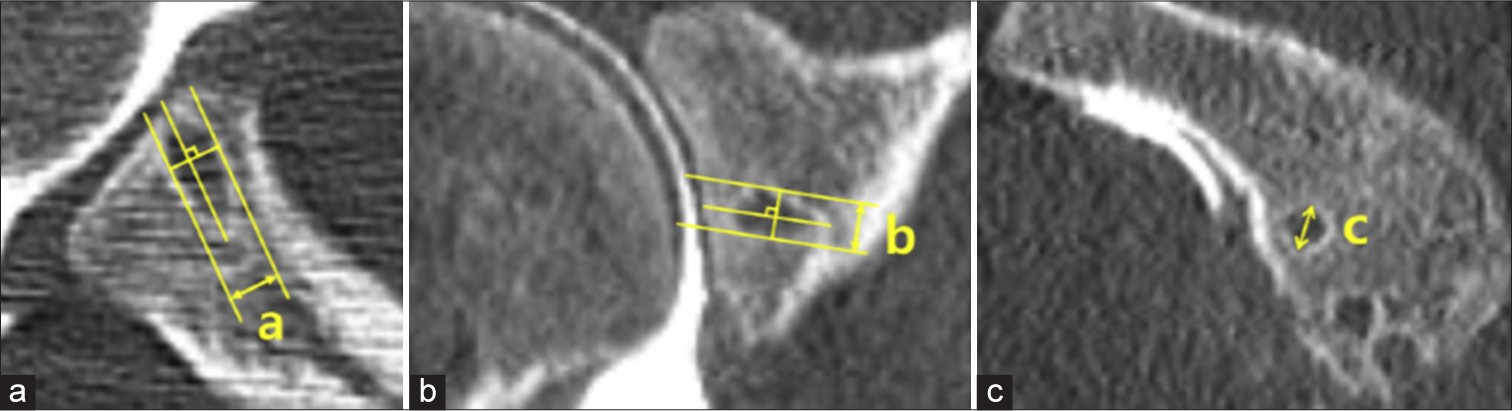
- Morphology of tunnel in different views on computed tomography. (a) Tunnel diameter in the axial plane, (b) Tunnel diameter in the coronal plane, and (c) Tunnel diameter in the sagittal plane.
| Grade 0 | Complete resorption |
| Grade 1 | Partial bony defects (or) erosions (Tunnel diameter < original tunnel diameter) |
| Grade 2 | Tunnel dilation (original tunnel diameter < Tunnel diameter < 2 x original tunnel diameter) |
| Grade 3 | Peri anchor cyst formation (tunnel diameter > 2 x original tunnel diameter) |
Data entry and statistical analysis
The collected data were transformed into variables, coded, and entered in Microsoft Excel. Data were analyzed and statistically evaluated using the Statistical Package for the Social Sciences-PC-25 version. Normal distribution of different parameters was tested by the Shapiro–Wilk normality test. Qualitative data were expressed in mean ± standard deviation or median with interquartile range. Normality difference between pre-post data was compared by paired t-test. Qualitative data were expressed in frequency and percentage and statistical difference between the pre-post proportions were tested by McNemar test. P < 0.05 was considered statistically significant.
RESULTS
All 15 patients were available for follow-up. There were 12 males and three females patients. Maximum number of patients was observed to be in the early half of third decade of life at the time of follow-up. The mean number of dislocations before surgery was 6 ranging from a minimum of 2 to a maximum of 10. Out of 15 patients, 11 were participating in some sort of sporting activities before surgery [Table 2].
| Mean age | 25.13±8.36 |
| Gender | |
| Male | 12 |
| Female | 3 |
| Dominant side | 12 |
| Mean number of dislocations | 6.06 |
| Nature of sport | |
| Contact | 4 |
| Non-contact | 7 |
| None | 4 |
In our study, 6 patients (40%) had Bankart lesion, 4 (26.67%) had bony Bankart, and 5 (33.33%) had Bankart lesion with significant Hill Sachs defect in the pre-operative period. None of the patients had bony Bankart with Hill Sachs defect in our study. A total of 43 all-soft suture anchors (24 single-loaded and 19 double-loaded) were used with three anchors being used for repair in 13 patients and two in two patients. Anterior apprehension test was positive in five patients at the time of first follow-up and positive in two patients at the time of second follow-up visit. Load and shift test was suggestive of normal laxity in 10, grade 1 laxity in 4 and grade 2 laxity in one patient in comparison to contralateral normal shoulder during the first follow-up. None had grade 2 laxity during the second follow-up at the end of 12 months. There was significant improvement in the functional scores (WOSI and ROWE scores) of all patients at the end of our study [Table 3]. All suture anchors were inserted along the 2’o clock to 7’o clock arc for the right (R) side and the 5’o clock to 10’o clock arc on the left (L) side. Tunnel visualized between (R) 2–3’o clock position (L) 10–9’o clock (superior) was assigned tunnel 1, tunnel 2 between (R) 3–5’o clock (L) 9–7’o clock (middle) and tunnel 3 between (R) 5–7’o clock (L) 7–5’o clock (inferior). The mean diameters of tunnels 1, 2, and 3 were calculated to be 1.85, 2.44, and 2.94, respectively, with a standard deviation of 0.91, 1.31, and 1.24, respectively [Table 4]. There was a statistically significant reduction in the diameters of tunnels 1 and 2 in the 2nd computed tomography (CT) with P-value 0.01 and 0.02, respectively, with P < 0.005 considered statistically significant. No significant difference was found between the diameters of 3rd tunnel on serial evaluation.
| 1st follow-up (6th month) | 2nd follow-up (12th month) | P-value | |
|---|---|---|---|
| Apprehension | 0.24 | ||
| No | 10 (66.7%) | 13 (86.7%) | |
| Yes | 5 (33.3%) | 2 (13.3%) | |
| Median WOSI score | 14 (8.3–33.1) | 9.6 (5.9–33.38) | 0.08 |
| ROWE score | 82.33±24.48 | 84.0±21.31 | 0.20 |
WOSI: Western Ontario shoulder instability index.
| Tunnel 1 | Tunnel 2 | Tunnel 3 | |
|---|---|---|---|
| Mean±standard deviation | 1.85±0.91 | 2.44±1.31 | 2.94±1.24 |
NCCT: Non-contrast-enhanced computed tomography
We evaluated the glenoid bone reactions and graded them as per Ruiz Ibán et al.[8] None of the anchors showed complete resorption, partial erosions were noticed in 14 out of 43 anchors at the first CT evaluation which increased to 21 at the end of 12 months. Tunnel dilation decreased from 26 to 19 at the end of our study. Two peri-anchor cystic changes were identified in the first follow-up which remained the same on subsequent serial imaging [Table 5]. Bone volume remained stable in 2, increased in 12, and decreased in 1 shoulder. A significant improvement (reduction) in the size of the drilled tunnel was observed in both tunnels 1 and 2, but similar results could not be reflected in tunnel 3, which showed a reduction in size on serial imaging but was not statistically significant.
| First CT | Second CT | |
|---|---|---|
| CR | 0 | 0 |
| PE | 14 | 21 |
| TD | 26 | 19 |
| Peri-anchor CC | 3 | 3 |
NCCT: Non-contrast-enhanced computed tomography, CT: Computed tomography, CR: Complete resorption, PE: Partial bony erosions, TD: Tunnel dilation, CC: Cyst changes
DISCUSSION
The number of patients opting for shoulder surgeries has drastically increased in the past two decades due to the increase in the number of overhead sporting activities, better patient education, and improved diagnostic and surgical techniques. With the advent of shoulder arthroscopy, arthroscopic Bankart repair is considered by many surgeons all over the world to be the preferred method of management of anterior instability. It is minimally invasive, avoids splitting the subscapularis muscle, and provides a detailed evaluation of intra-articular anatomy and pathology, maximal preservation of external rotation and statistically significant reduction in post-operative instability and a higher rate of return to sports and other daily activities.
Arthroscopic repair of recurrent glenohumeral instability by anatomical repair techniques has been shown to be clinically equivalent to open techniques in the long term.[9,10] Improvement in the surgical instruments, implants, and techniques has paved the way for the increase in the consideration of these procedures as the first-line management in patients presenting with recurrent anterior instability with non-significant glenohumeral bone loss.
Arthroscopic techniques have evolved from the usage of metallic staples and bio-degradable tacks to the recent introduction of suture anchors. All-soft suture anchors are less invasive than standard implants. These are based on ultra-high molecular weight polyethylene.[11] They minimize hardware-related complications and reduce the incidence of suture-induced arthritic changes. The tunnel drilled in the glenoid bone for anchor insertion is significantly smaller than that required for a classical suture anchor (1.4 mm vs. 3 mm), thereby reducing the risk of glenoid rim fractures and anchor pull-out.[12]
We evaluated a total of 43 all-soft suture anchors in 15 patients. No anchor showed complete resorption in both the 1st and 2nd CT studies. There was an increased conversion rate from grade 2 (tunnel dilatation) to grade 1 (partial erosion) at the end of our follow-up study, as visualized in the 2nd CT study at the end of 12 months. A total of three anchors in three patients showed grade 3 reaction (cystic change) at the time of 1st CT scan (6th month) which remained constant at the end of our 2nd CT study. Two out of these three patients reported a recurrence of instability after the study period and had to undergo a revision bone block procedure (Latarjet procedure) for the same.
No anchor inserted on the anterior aspect (2–3’o clock) position showed grade 3 changes. One anchor in the anteroinferior (3–5’o clock) and two anchors in the posteroinferior (5–7’o clock) position showed grade 3 changes. Out of these three, two were single-loaded, and one was double-loaded. Lee et al.[7] demonstrated the effect of position and angle of insertion on bio-mechanical effects of all-soft suture anchors in arthroscopic Bankart repair. He reported increased stiffness and greater ultimate to-load failure for anchors implanted at the 2:30’ o clock position in comparison to the 4 and 5:30’ o clock positions regardless of the angle of suture anchor insertion. The micromotion resulting during anchor deployment while insertion and lower ultimate load to failure in the inferiorly placed anchors can explain the increased incidence of grade 3 changes in this position. Persistent micromotion may lead to tunnel dilation and peri-anchor cyst formation, further increasing the stress on other anchors, thereby influencing similar bone reactions in them, eventually resulting in failure of the repair.
Glenoid bone loss increased in one patient and remained stable in two other patients on subsequent follow-ups. Out of which, two patients showed grade 1 instability and positive apprehension during their clinical evaluation. Yamamoto et al.,[13] showed a decrease in glenoid bone width following arthroscopic repair, more so in patients with soft-tissue Bankart (57%) as compared to Bony Bankart (15%) which was further validated by Hirose et al.[14] Shaha et al.[15] reported a bone loss of more than 13.5% corresponded to sub-critical bone loss that influenced post-operative outcomes. One patient in our study had a bone loss more than the critical limit and reported persistent instability before and after surgery (grade 3 in pre-operative and grade1 in post-operative period). All-soft suture anchors were associated with some changes in the glenoid bone following insertion but showed a tendency toward healing on serial evaluation in majority of cases and were associated with lower hardware-related complications than previous generation anchors. The results of our study could be compared to that of Ruiz Ibán et al.,[8] Tompane et al.,[16] and Willemot et al.,[17] who reported an increased incidence of tunnel dilation following the usage of ASSAs [Table 6]. The incidence of grade 3 cystic changes in the glenoid bone was less but their occurrence could not be ruled out. None of the above-mentioned studies performed a serial follow-up radiological evaluation of glenoid bone reactions.
| S. No. | Authors | Number of suture anchors | Glenoid bone reactions | |||
|---|---|---|---|---|---|---|
| CR/NBL | PE | TD | CC | |||
| 1. | Ruiz Ibán et al.[8] | 55 | 2 | 8 | 35 | 10 |
| 2. | Tompane et al.[16] | 33 | 0 | 4 | 28 | 1 |
| 3. | Willemot et al.[17] | 58 | 45 | 13 | 3 | 2 |
| 4. | Present study | 43 | 0 | 21 | 19 | 3 |
CR: Complete resorption, NBL: No bony lesion, PE: Partial bony
Limitations of the study
First being the relatively small sample sizes, whose results cannot be reflected on the normal population on a grand scale. Second is the lack of a comparison group comprising previous generation anchors. Third, the duration of follow-up was relatively short, which did not allow evaluation of all patients with peri-anchor cystic changes and their functional outcomes. Finally, higher radiological investigations like MRI (Magnetic resonance imaging) would have provided a more comprehensive evaluation of healing.
CONCLUSION
We observed that the overall performance of all-soft suture anchors in arthroscopic Bankart repair was comparable to previous generation suture anchors in terms of clinical and functional outcomes and was associated with a lower complication rate than metallic and bio-degradable anchors. However, we would advocate for further long-term follow-up studies of these anchors in the future with a larger non-randomized cohort of patients.
Acknowledgment
We thank all the individuals included in this study and the anonymous reviewers for their valuable suggestions.
Author contributions
All the authors were involved in conceptualization, literature search, design, data analysis, manuscript writing and final approval.
Ethical approval
The research/study approved by the Institutional Review Board at Maulana Azad Medical college, number F.1/IEC/MAMC/(82/10/2020/No.182, dated January 14, 2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Shoulder girdle In: McRae’s orthopaedic trauma and emergency fracture management (3rd ed). Poland: Elsevier; 2016. p. :146-57.
- [Google Scholar]
- Arthroscopic approach to acute bony Bankart lesion. Arthroscopy. 2002;18:764-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic Bankart repair with knotless suture anchor for traumatic anterior shoulder instability: Results of short-term follow-up. Arthroscopy. 2006;22:620-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between metal and biodegradable suture anchors in the arthroscopic treatment of traumatic anterior shoulder instability: A prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2010;18:1785-91.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term degradation of a polylactide co-glycolide/β-tricalcium phosphate biocomposite interference screw. Arthroscopy. 2011;27:637-43.
- [CrossRef] [PubMed] [Google Scholar]
- Bone replacement of fast-absorbing biocomposite anchors in arthroscopic shoulder labral repairs. Am J sports Med. 2012;40:1392-401.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of clinical outcomes and Computed tomography analysis for Tunnel diameter after arthroscopic Bankart repair with the all-suture anchor and the biodegradable suture anchor. Arthroscopy. 2019;35:1351-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic Bankart repair with all-suture anchors does not cause important glenoid bone osteolysis: A volumetric CT study of 143 anchors. Knee Surg Sports Traumatol Arthrosc. 2021;29:2152-8.
- [CrossRef] [Google Scholar]
- Arthroscopic versus open reconstruction of the shoulder in patients with isolated Bankart lesions. Am J Sports Med. 1996;24:144-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic Bankart repair in traumatic anterior shoulder instability using a suture anchor technique. Arthroscopy. 2006;22:931-6.
- [CrossRef] [PubMed] [Google Scholar]
- The history of suture anchors in orthopaedic surgery. Clin Biomech (Bristol Avon). 2019;61:70-8.
- [CrossRef] [PubMed] [Google Scholar]
- Triple labrum tears repaired with the JuggerknotTM soft anchor: Technique and results. Int J Shoulder Surg. 2015;9:81-9.
- [CrossRef] [PubMed] [Google Scholar]
- Morphological changes in glenoid after arthroscopic Bankart repair. Shoulder Joint. 2016;40:857-60.
- [Google Scholar]
- Progression of erosive changes of glenoid rim after arthroscopic Bankart repair. Arthroscopy. 2020;36:44-53.
- [CrossRef] [PubMed] [Google Scholar]
- Redefining “critical” bone loss in shoulder instability: Functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43:1719-25.
- [CrossRef] [PubMed] [Google Scholar]
- Glenoid bone reaction to all-soft suture anchors used for shoulder labral repairs. J Bone Joint Surg Am. 2018;100:1223-9.
- [CrossRef] [PubMed] [Google Scholar]
- Radiological and clinical outcome of arthroscopic labral repair with all-suture anchors. Acta Orthop Belg. 2016;82:174-8.
- [Google Scholar]






