Translate this page into:
Single-stage capsular release and rotator cuff repair for patients with rotator cuff tear
*Corresponding author: Prashanth Pandian, Department of Orthopaedics, Chettinad Academy of Research and Education, Chennai, Tamil Nadu, India. drprashanth.sayee@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thavasianantham K, Pandian P, Pandian H. Single-stage capsular release and rotator cuff repair for patients with rotator cuff tear. J Arthrosc Surg Sports Med 2023;4:10-5.
Abstract
Objectives:
Shoulder stiffness is often an associated symptom in patients with rotator cuff (RC) tear. With an ongoing debate on the timing and staging of procedures, there seems to be no clear consensus about managing these patients. In this study, we aimed to ascertain if performing a single-stage rotator cuff repair (RCR) along with concomitant capsular release (CR) has any advantage over performing RCR alone and whether it has any impact on the functional outcome of the patients.
Materials and Methods:
Retrospective study was conducted with 23 patients who received arthroscopic RCR under a single surgeon from 2017 to 2022. From 2017 to 2019, patients underwent only RCR without any CR; from 2020 to 2022, concomitant CR was done along with all RCR. A total of 12 patients were identified under the CR group and 11 patients under the no-CR group. Range of motion (ROM) and functional outcomes were recorded and assessed pre- and post-operatively for 2 years.
Results:
There was no significant variation in gender distribution, age, and cuff tear size between the two groups. Postoperatively, there was a substantial variation between the two groups in the recovery period (6 months post-operative) of ROM. Postoperatively, patients in both groups reported lesser pain and improved ROM compared to pre-operation. However, there was no substantial variation in functional outcome scores and ROM between both groups at the final follow-up.
Conclusion:
Combined single-stage RCR along with CR significantly reduces the recovery period compared to those who underwent repair without CR.
Keywords
Shoulder
Rotator cuff tear
Arthroscopic repair
Capsular release
Stiffness
INTRODUCTION
Rotator cuff tear (RCT) is common shoulder pathology, with a global incidence of about 40% in asymptomatic individuals and 65% in symptomatic individuals.[1] Due to resultant muscular weakness and altered biomechanics, a ruptured rotator cuff (RC) can severely restrict the active range of motion (ROM) of the shoulder joint. It is not uncommon for these lesions to cause excruciating, protracted pain, eventually resulting in progressive capsular contracture developing over time, restricting both active and passive ROM, and leading to secondary stiffness. There is debate regarding the best timing to do an RC surgery on individuals who have both concurrent stiffness and RCT.[2] Conventionally, several authors have recommended a phased treatment, first to recover passive ROM, and then proceed with surgery for RCT.[3] Pre-operative physical therapy may sometimes be ineffective due to discomfort or the risk of causing more RC damage.[4] Patients who have preserved scapulothoracic mobility but minimal glenohumeral joint motion may consider manipulation since non-operative therapy alone cannot reduce shoulder stiffness.[5-7] Furthermore, deferring RC treatment in favor of pre-operative physical therapy might lead to tendon retraction, muscle atrophy, and tear propagation making rotator cuff repair (RCR) more difficult or perhaps impossible.[8,9] The other possibility is to do an arthroscopic capsular release (ACR) first, followed by an RCR later. Before RC surgery, this helps to increase ROM, but it exposes patients to the danger and expense of multiple procedures. With improved surgical techniques and a better understanding of the disease pathophysiology, attempts to perform a single-stage capsular release (CR) along with RCR have been made and claimed to have promising results.[10,11]
In this study, individuals who simultaneously underwent RCR and ACR surgery are compared to patients who underwent only RCR. We hypothesized that patients who underwent concomitant anteroinferior CR along with RCR would have better functional outcomes compared to those patients who underwent RCR alone.
Procedure
All patients received subacromial decompression, acromioplasty, and RCR with or without concomitant anteroinferior CR. For the patients positioned in a lateral decubitus position, a radiofrequency wand was used to release the inferior-capsule, rotator-interval, middle glenohumeral ligament, and anterior capsule when concomitant CR was carried out. All patients had bursectomy and acromioplasty through the lateral-portal using an arthroscopic shaver and burr. Cuff integrity was assessed intraoperatively using an arthroscope. The long head of the biceps tendon and its attachment status was checked and addressed accordingly if need be. Before starting the repair, the torn edges were debrided and the osseous bed on the greater tuberosity of the humerus was prepped.[12] Adequate release and marginal convergence were done if necessary to facilitate a tension-free repair of the RC. Single-row repair with PEEK anchors was used to complete the repair in all patients. No intra-articular or subacromial injections were administered following surgery.
Following surgery, both groups adhered to the same rehabilitation plan. All patients received the same postoperative care, which included post-operative arm slings for pain management and the proper oral analgesics. On the 1st post-operative day, all patients were permitted to perform mild wrist and elbow ROM exercises. Physical therapy was divided into three phases. Exercises to increase passive shoulder ROM were started in weeks 2–4. Therapy from weeks 4 to 12 concentrated on enhancing active ROM. After week 12, the post-operative rehabilitation program included active resistance and strengthening activities. To check for recovery and surgical problems, the operating surgeon followed up every patient for 2 years following the procedure.
A dedicated data-gathering facility managed by independent specialists collected both subjective and objective data. Using standardized survey questionnaires, age, sex, and medical comorbidities were gathered. Two qualified examiners used an inclinometer to measure the active ROM in flexion, abduction (Abd), and internal and external rotation (IR and ER) of both shoulders sequentially. Simple shoulder scores, the American Shoulder and Elbow Surgeons Shoulder Score, and the University of California Los Angeles Shoulder Score were compiled.
MATERIALS AND METHODS
A retrospective study with 23 patients who underwent arthroscopic RCR under a single surgeon at a single center from 2017 to 2022 was conducted. From 2017 to 2019, patients did not undergo any CR and from the year 2020 to 2022, concomitant CR was done along with all RCR. Twelve patients belonged to the CR group and 11 patients belonged to the no-CR group. ROM and functional outcomes were recorded pre- and post-operatively for 2 years. Inclusion criteria were pre-operative radiological evidence of RCT along with symptoms for at least 3 months and postoperative follow for 2 years. Exclusion criteria were age >65 years, grade IV glenohumeral arthritis, massive irreparable RCT, acute traumatic cuff tears, and severe osteoporosis.
Statistical analysis
The variation in gender distribution within groups was compared using the Chi-square test and expressed as mean (±standard deviation). Using an independent t-test, the RCT size and age were compared between the case and control groups. A group of patients was compared using the Mann– Whitney U-test. All statistical tests were two-tailed, and significance was set at P < 0.05. Statistical Package for the Social Sciences (SPSS) Version 26 was used for all statistical analyses (IBM, SPSS Statistics, Armonk NY, USA).
RESULTS
We did not observe any substantial variation in demographic data (gender, age, and size of cuff tear) between the groups. DeOrio and Cofield classification[13] was used to classify the RCT size, which is defined as small (0–1 cm), medium (1–3 cm), large (3–5 cm), and massive (>5 cm) [Table 1]. Postoperatively, we found that there was substantial variation in the ROM recovery period between the two groups [Table 2 and Figure 1]. IR was the first to recover, with a statistical difference at 3 months post-operative. The difference between the groups in forward flexion elevation, Abd, and ER was statistically significant at 6 months of follow-up. During the follow-up, both patient groups reported improved ROM and lesser pain compared to pre-operation levels. At the end of the 2-year follow-up, patients who underwent CR had marginally better Abd and ER but were found to be statistically insignificant. However, the functional outcomes between the two groups at the final follow-up showed no significant variation [Table 3 and Figure 2]. Within the time frame of the follow-up, no patients in either group needed revision surgery.
| Capsular release (Cr) | No capsular release (Nr) | |
|---|---|---|
| Gender | ||
| Male | 6 | 6 |
| Female | 6 | 5 |
| Age (Mean years ± SD) | 59.5±4.77 | 60.6±5.95 |
| Cuff Tear Size* | ||
| Partial | 2 | 3 |
| Small | 4 | 3 |
| Medium | 5 | 4 |
| Large | 1 | 1 |
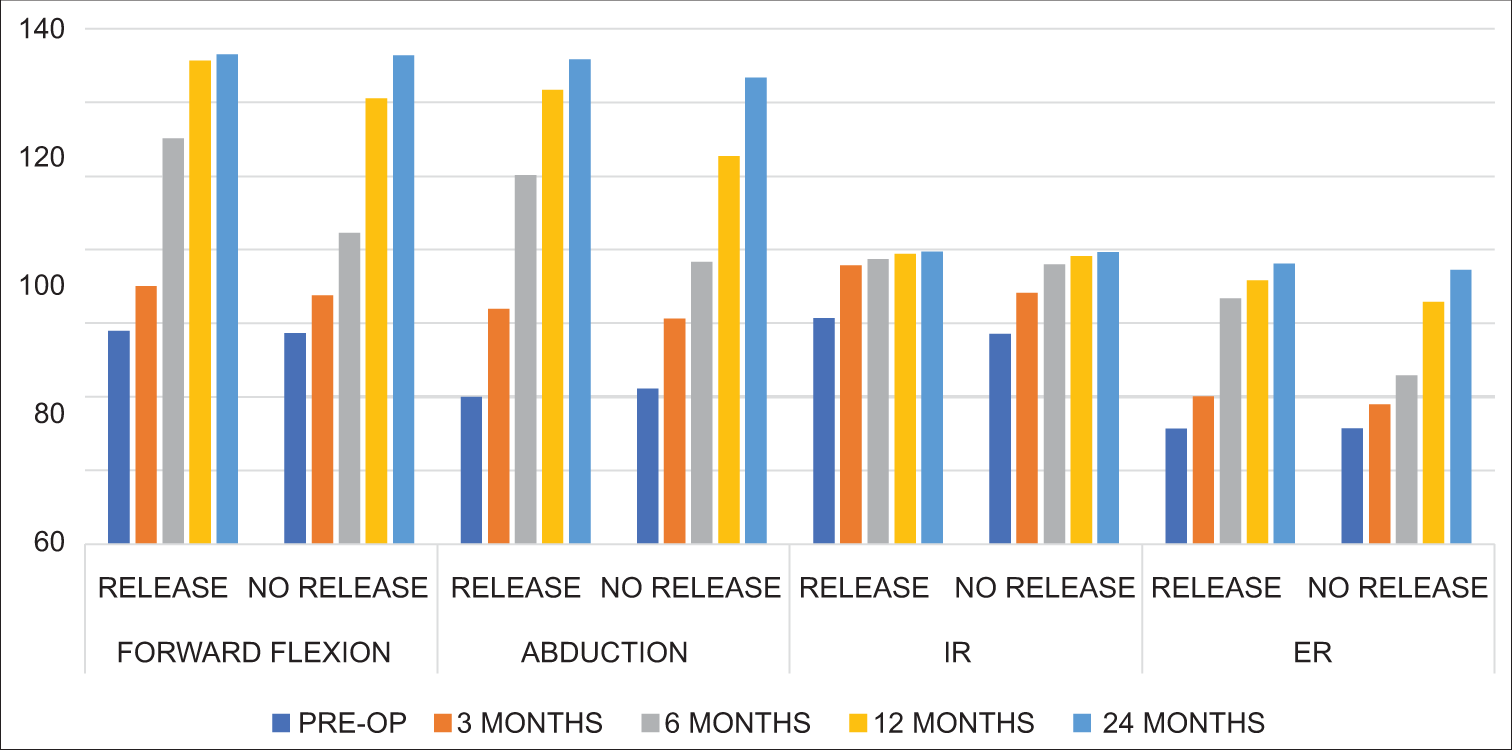
- Mean value of the range of motion. IR: Internal rotation, ER: External rotation, PRE-OP: Pre-operative
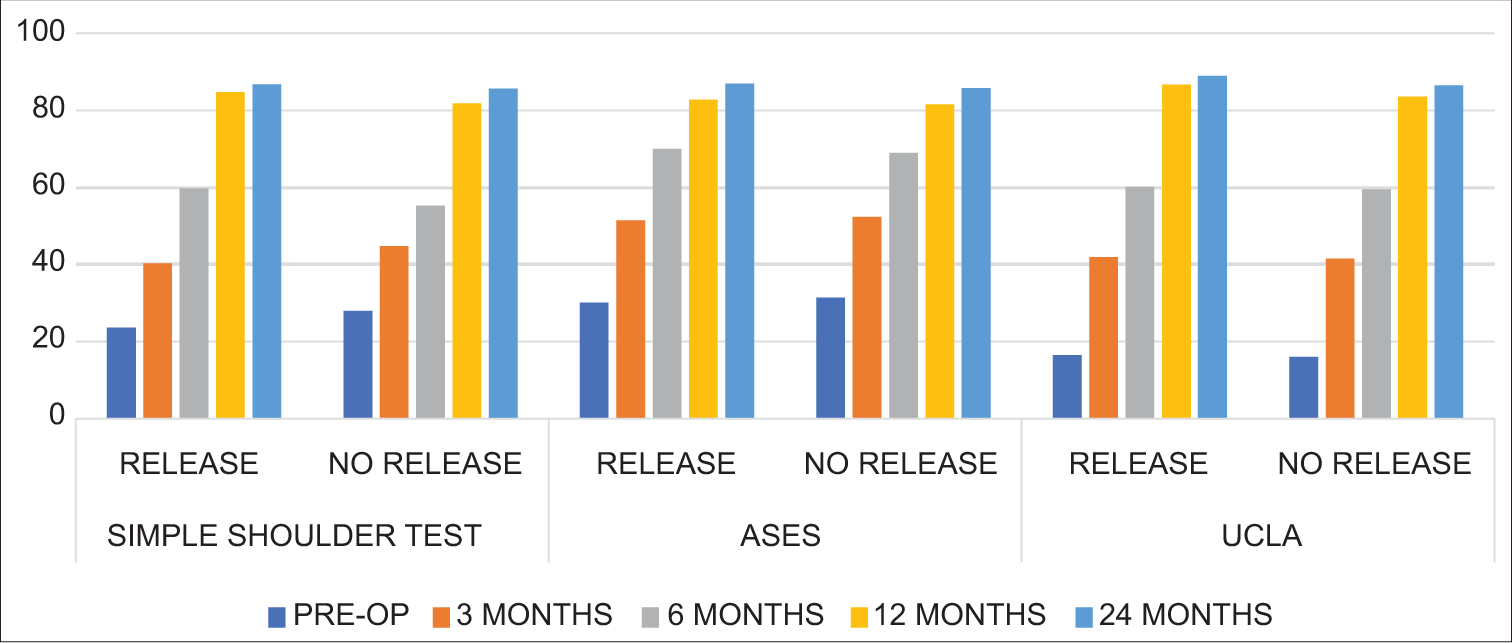
- Mean value of the functional score. ASES: American shoulder and elbow surgeons (ASES) score, UCLA: University of california-Los angeles (UCLA) shoulder scale, PRE-OP: Pre-operative
| ROM (Range of motion) | Preop | 3 Months | 6 Months | 12 Months | 24 Months |
|---|---|---|---|---|---|
| Forward flexion | |||||
| Capsular release | 57.83±4.54 | 70±2.95 | 110.16±5.85 | 131.33±5.39 | 133±4.13 |
| No capsular release | 57.27±4.92 | 67.45±3.35 | 84.54±2.59 | 121±1 | 132.72±4.49 |
| P value | >0.05 | >0.05 | <0.05* | <0.05* | >0.05 |
| Abduction | |||||
| Capsular release | 40±2.41 | 63.83±3.01 | 100.16±3.01 | 123.33±6.28 | 131.66±5.64 |
| No capsular release | 42.18±2.60 | 61.27±3.32 | 76.63±6.83 | 105.36±6.26 | 126.72±2.86 |
| P value | >0.05 | >0.05 | <0.05* | <0.05* | >0.05 |
| Internal rotation | |||||
| Capsular release | 61.33±3.55 | 75.75±3.76 | 77.41±2.77 | 78.83±3.01 | 79.5±2.71 |
| No capsular release | 57.09±4.84 | 68.18±3.15 | 76±2.82 | 78.18±2.60 | 79.27±2.24 |
| P value | >0.05 | <0.05* | >0.05 | >0.05 | >0.05 |
| External rotation | |||||
| Capsular release | 31.33±1.96 | 40.16±3.66 | 66.83±4.21 | 71.66±2.09 | 76.16±1.99 |
| No capsular release | 31.45±2.01 | 38±2.19 | 45.81±3.28 | 65.81±4.51 | 74.54±2.54 |
| P value | >0.05 | >0.05 | <0.05* | <0.05* | >0.05 |
| Functional score | Preop | 3 Months | 6 Months | 12 Months | 24 Months |
|---|---|---|---|---|---|
| Simple shoulder test | |||||
| Capsular release | 23.57 ± 11.16 | 40.24 ± 9.93 | 59.68 ± 8.58 | 84.68 ± 4.79 | 86.75 ± 4.27 |
| No capsular release | 27.99 ± 12.50 | 44.68 ± 11.94 | 55.26 ± 11.33 | 81.78 ± 8.16 | 85.56 ± 6.52 |
| P value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
| ASES | |||||
| Capsular release | 30.08 ± 6.89 | 51.41 ± 4.73 | 70 ± 6.41 | 82.83 ± 6.65 | 86.83 ± 4.44 |
| No capsular release | 31.36 ± 9.18 | 52.36 ± 4.29 | 68.90 ± 6.77 | 81.54 ± 4.76 | 85.72 ± 4.31 |
| P value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
| UCLA | |||||
| Capsular release | 16.42 ± 5.46 | 41.87 ± 9.84 | 60.21 ± 5.79 | 86.62 ± 6.21 | 88.98 ± 4.34 |
| No capsular release | 16.09 ± 5.75 | 41.54 ± 12.12 | 59.46 ± 8.47 | 83.60 ± 7.31 | 86.44 ± 5.55 |
| P value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
Preop: Pre-operative, ASES: American shoulder and elbow surgeons (ASES) score, UCLA: University of california-Los angeles (UCLA) shoulder scale
DISCUSSION
Patients are frequently present with an RCT and concurrent stiff shoulders. The appropriate degree of stiffness which requires intervention at the time of RC surgery is still up for debate.[14,15] The disabling illness of shoulder stiffness has a significant impact on a patient’s everyday activities. Pre-operative shoulder stiffness is thought to increase the likelihood of developing post-operative stiffness which affects patient satisfaction following surgery.[16,17] Determining the best course of treatment for this particular patient population is crucial. According to Tauro, patients with mild-to-moderate pre-operative stiffness often have resolution with early passive ROM therapy following RCR. However, individuals who had arthroscopy-confirmed adhesive capsulitis and substantial pre-operative stiffness did not have an improvement in their ROM following surgery.[14] Regarding the treatment of these individuals, shoulder surgeons differ; some propose a one-stage procedure while others carry out two-stage procedures.[3,11,18,19] Kim et al. observed no benefit in postponing RCR and advocated concurrent CR and RCR for pre-operative rehab to alleviate stiff shoulders.[20] McGrath et al. observed that patients who underwent simultaneous RC surgery and CR had no re-tear as opposed to a twenty percent retear rate for patients without stiffness who underwent repair alone.[11]
Cho presented a different one-stage treatment in which manipulation and RCR were used in place of CR.[19] Patients with stiff shoulders achieved comparable results to those without stiffness in their case–control study after 2 years, although the recovery in ROM was delayed in patients with a stiff shoulders. According to our research, patients who underwent concomitant CR with RCR had a lesser recovery period compared to those who did not have a CR. However, the results of our research were comparable between the two groups.
Grant conducted a systematic analysis comparing ACR and manipulation for adhesive capsulitis, and the results revealed that ACR improved Abd and ER more effectively. This could be because manipulation is a crude way to deal with stiffness. The ACR, on the other hand, enables fine visual control to release only certain tight structures. However, the grant revealed that there was not any apparent difference in the median change in constant score between the two modalities. Due to the lack of arthroscopy equipment, manipulation is simpler and easier than ACR. However, manipulation can result in a number of significant issues.[21-24] When done by skilled surgeons, ACR may be safer than manipulation. In addition, ACR is practical for patients with subsequent stiffness and RCT.[25] To avoid the problems discussed with manipulation, ACR followed by manipulation would be preferable to manipulation followed by ACR. On the other hand, numerous investigations have revealed that manipulation offers no benefits above conventional therapy.[26-28] ACR has demonstrated promising outcomes and is growing in popularity.[29-31] According to Cvetanovich et al.,[29] ACR for idiopathic stiffness had excellent functional outcomes, considerable early and persistent improvements in ROM, and minimal revision and complication rates.
To restore normal ROM, previously, several authors have advocated 360° CR. Recent evidence has shown that partial CR (anterior-inferior capsule)[29,32] along with coracohumeral ligament and rotator interval release is adequate[29,33-35] and, hence, was adapted in our study population.
The study has several limitations. First, the number of patients involved in the study is less than ideal for arriving at any conclusive evidence. Second, before 2020, all patients underwent only RCR and those who presented after 2020 had a concomitant anterior CR irrespective of the pre-operative shoulder ROM. Not taking into account the pre-operative stiffness can result in skewed data. However, this limitation has been overcome by standardizing the procedure over definite periods of time and offering it to all subjects undergoing intervention. The retrospective nature of the study itself results in inherent weakness. Furthermore, arthroscopic anteroinferior CR, when done by inexperienced surgeons, can result in inadvertent axillary nerve injury. Finally, the role of medical comorbidities such as diabetes, smoking, obesity, and thyroid disorder, which might have an impact on the outcome, was not taken into account. The strength of the study is that a single surgeon performed all the procedures, which aids in ensuring uniformity in pre-operative evaluation and surgical procedures. The homogeneity of the data was further guaranteed by assessing the patient’s outcome using standard questionnaires, evaluation methods, and specified temporal time frames.
CONCLUSION
Our findings add to the expanding body of research showing that patients with symptomatic RC injuries and shoulder stiffness need not require postponing surgery. Single-stage surgery combining CR and RCR was found beneficial as the recovery period was significantly reduced without any added risk to the patient. However, we found no substantial variation in functional outcome and ROM between the two groups at the end of the study period.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Outcomes of single-row versus double-row arthroscopic rotator cuff repair: A systematic review and meta-analysis of current evidence. Arthroscopy. 2013;29:1437-49.
- [CrossRef] [PubMed] [Google Scholar]
- Complications associated with arthroscopic shoulder surgery. Arthroscopy. 2002;18:88-95.
- [CrossRef] [PubMed] [Google Scholar]
- Practical evaluation and management of the shoulder Philadelphia, PA: WB Saunders; 1994.
- [Google Scholar]
- Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg. 2005;14:16-21.
- [CrossRef] [PubMed] [Google Scholar]
- Manipulation in the treatment of frozen shoulder. Orthopedics. 1988;11:1255-60.
- [CrossRef] [PubMed] [Google Scholar]
- The frozen shoulder. Diagnosis and management. Clin Orthop Relat Res. 1987;223:59-64.
- [CrossRef] [Google Scholar]
- Frozen shoulder. Part II: Treatment by manipulation under anesthesia. Orthopedics. 1989;12:989-90.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550-4.
- [CrossRef] [PubMed] [Google Scholar]
- The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505-15.
- [CrossRef] [PubMed] [Google Scholar]
- One-stage arthroscopic repair of rotator cuff tears with shoulder stiffness. Arthroscopy. 2013;29:1283-91.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of concomitant glenohumeral joint capsule release during rotator cuff repair--a comparative study. J Shoulder Elbow Surg. 2016;25:714-22.
- [CrossRef] [PubMed] [Google Scholar]
- Is single stage capsular release and rotator cuff repair suitable for rotator tears with concomitant stiffness? J Orthop. 2020;21:496-9.
- [CrossRef] [PubMed] [Google Scholar]
- Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563-7.
- [CrossRef] [Google Scholar]
- Stiffness and rotator cuff tears: Incidence, arthroscopic findings, and treatment results. Arthroscopy. 2006;22:581-6.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of shoulder stiffness after rotator cuff repair. Clin Orthop Relat Res. 2005;430:94-9.
- [CrossRef] [PubMed] [Google Scholar]
- Range of motion limitation after rotator cuff repair. J Shoulder Elbow Surg. 2010;19:290-6.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of patient satisfaction with outcome after rotator cuff surgery. J Bone Joint Surg Am. 2005;87:121-6.
- [CrossRef] [PubMed] [Google Scholar]
- Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008;24:983-91.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcome of arthroscopic repair with concomitant manipulation in rotator cuff tears with stiff shoulder. Am J Sports Med. 2008;36:1323-9.
- [CrossRef] [PubMed] [Google Scholar]
- Are delayed operations effective for patients with rotator cuff tears and concomitant stiffness? An analysis of immediate versus delayed surgery on outcomes. Arthroscopy. 2015;31:197-204.
- [CrossRef] [PubMed] [Google Scholar]
- Early clinical outcomes of manipulation under anesthesia for refractory adhesive capsulitis: Comparison with arthroscopic capsular release. Clin Orthop Surg. 2020;12:217-23.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of manipulation and arthroscopic capsular release for adhesive capsulitis: A systematic review. J Shoulder Elbow Surg. 2013;22:1135-45.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcome after arthroscopic capsular release for adhesive capsulitis of the shoulder. Clin Shoulder Elb. 2018;21:127-33.
- [CrossRef] [PubMed] [Google Scholar]
- Glenoid fracture during manipulation under anesthesia for adhesive capsulitis: A case report. J Shoulder Elbow Surg. 2011;20:e23-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes of rotator cuff repair with arthroscopic capsular release and manipulation for rotator cuff tear with stiffness: A matched-pair comparative study between patients with and without stiffness. Arthroscopy. 2015;31:482-7.
- [CrossRef] [PubMed] [Google Scholar]
- Manipulation or intraarticular steroids in the management of adhesive capsulitis of the shoulder? A prospective randomized trial. J Shoulder Elbow Surg. 2009;18:348-53.
- [CrossRef] [PubMed] [Google Scholar]
- Manipulation under anesthesia with home exercises versus home exercises alone in the treatment of frozen shoulder: A randomized, controlled trial with 125 patients. J Shoulder Elbow Surg. 2007;16:722-6.
- [CrossRef] [PubMed] [Google Scholar]
- Thawing the frozen shoulder. A randomised trial comparing manipulation under anaesthesia with hydrodilatation. J Bone Joint Surg Br. 2007;89:1197-200.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes of arthroscopic 360° capsular release for idiopathic adhesive capsulitis in the lateral decubitus position. Arthroscopy. 2018;34:764-70.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized controlled trial of arthroscopic capsular release versus hydrodilatation in the treatment of primary frozen shoulder. J Shoulder Elbow Surg. 2018;27:1401-6.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder adhesive capsulitis: Manipulation and arthroscopic arthrolysis or intra-articular steroid injections? Int Orthop. 2012;36:101-6.
- [CrossRef] [PubMed] [Google Scholar]
- Essential surgical technique for arthroscopic capsular release in the treatment of shoulder stiffness. JBJS Essent Surg Tech. 2015;5:e14.
- [CrossRef] [PubMed] [Google Scholar]
- Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am J Sports Med. 2012;40:815-21.
- [CrossRef] [PubMed] [Google Scholar]
- Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am. 1989;71:1511-5.
- [CrossRef] [PubMed] [Google Scholar]
- Variations in the superior capsuloligamentous complex and description of a new ligament. J Shoulder Elbow Surg. 2007;16:821-36.
- [CrossRef] [PubMed] [Google Scholar]






