Translate this page into:
The HALP – An unusual triad in shoulder instability

*Corresponding author: Saseendar Shanmugasundaram, Consultant Shoulder and Knee Arthroscopy Surgeon, Apollo Hospital, Muscat, Sultanate of Oman. ssaseendar@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Page RS, Gupta G, Shanmugasundaram S. The HALP – An unusual triad in shoulder instability. J Arthrosc Surg Sports Med 2020;1(2):226-9.
Abstract
Humeral avulsion of the glenohumeral ligament (HAGL) and posterior labral tears are less common injuries in comparison to Bankart lesion in traumatic shoulder instability. The association of rotator cuff tears with posterior capsulolabral lesions is even rarer. We present an unreported combination of HAGL with posterior labral tear and partial articular infraspinatus tendon avulsion (PAITA). This combination of shoulder injuries (HALP triad – HAGL + posterior labral tear + PAITA) has not been reported so far in English literature. The mechanism of this rare combination of injuries is discussed. The arthroscopic technique for simultaneous repair of this combination of ligament tears is presented.
Keywords
Bankart lesions
Rotator cuff
Rotator cuff injuries
Shoulder
Shoulder joint
Humerus
Ligaments
Joint Instability
INTRODUCTION
Bankart lesion is the most common ligament injury in traumatic shoulder instability. Humeral-sided capsular avulsions are less common, though there is increasing awareness regarding this injury.[1-3] Posterior capsulolabral lesions are less common and make only 2–5% of all shoulder instability.[4] While rotator cuff tears can be commonly associated with shoulder dislocation in the elderly, they are not common in instability in the young.[5,6] We report an unusual triad of lesions – anterior humeral avulsion of glenohumeral ligament (HAGL), posterior labral tear, and partial articular infraspinatus tendon avulsion (PAITA). The possible mechanism of such a combination of injuries is discussed and the arthroscopic technique for simultaneous repair is presented. To the best of our knowledge, there has been no previous reported case of such an injury pattern – the HALP (HAGL, posterior labrum, and PAITA) triad lesion.
CASE REPORT
A 41-year-old male, construction manager, presented to us 6 months after feeling a sudden sharp pain and something “give” in his dominant shoulder while performing an inclined bench press. He developed persistent ache weeks later with pain superiorly in the shoulder directed laterally and posteriorly into the arm. Pain was worse in extension and abduction – internal rotation. There were no mechanical symptoms. He had been on conservative treatment with analgesics and physiotherapy without improvement. Examination revealed mild tenderness anteriorly and laterally with full range of motion, a painful arc overhead with a negative Neer sign but a mildly positive Hawkins–Kennedy test. Rotator cuff strength was preserved, but with pain on loading in elevation. Apprehension test was negative and no frank instability was detected. His body mass index was 28.4. The Constant score was 60 and the simple shoulder test (SST) score was 8/12. Magnetic resonance arthrogram revealed a HAGL lesion involving the anterior limb of the inferior glenohumeral ligament (IGHL), a generally attenuated labrum and an articular partial thickness rotator cuff tear involving the anterior infraspinatus [Figure 1]. This mixed pathology was discussed and the patient elected to undergo surgery.
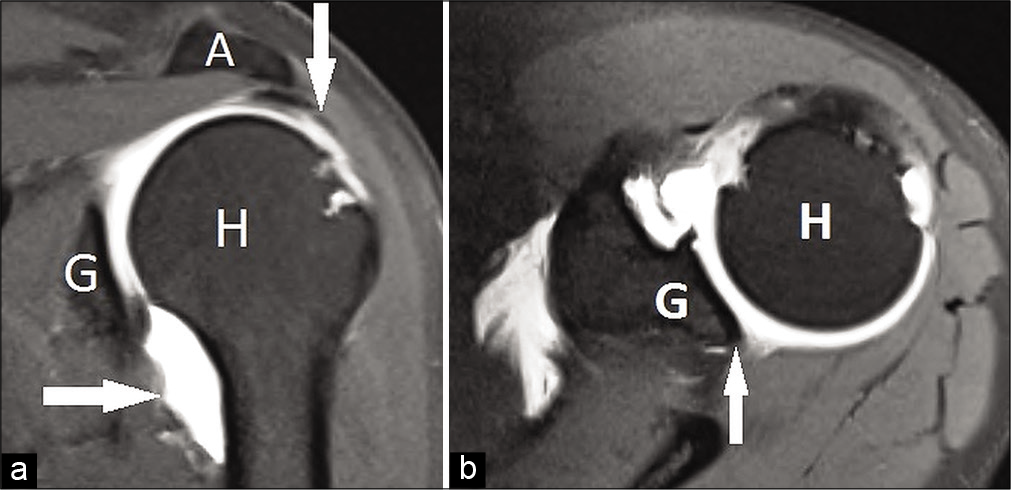
- (a) Pre-operative coronal magnetic resonance imaging (MRI) scan. Rotator cuff lesion is shown with white arrows under the acromion (A). Humeral avulsion of the glenohumeral ligament lesion is shown with white arrow between glenoid (G) and humeral head (H). (b) Pre-operative axial MRI scan. Deficiency of posterior labrum is pointed with white arrow between glenoid (G) and humeral head (H).
In the beach chair position, an EUA revealed Grade II anterior load and shift test and positive posterior labral grind and click. Glenohumeral arthroscopy revealed a deep PAITA extending 15 mm into the anterior infraspinatus [Figure 2]. There was a HAGL lesion involving the anterior half of the humeral capsular attachment [Figure 3]. There was also a posterior inferior labral tear from 7 to 9 o’ clock which had a positive peel back [Figure 4]. The cartilage on the humeral head appeared pristine and no Hill–Sachs lesion was noted.
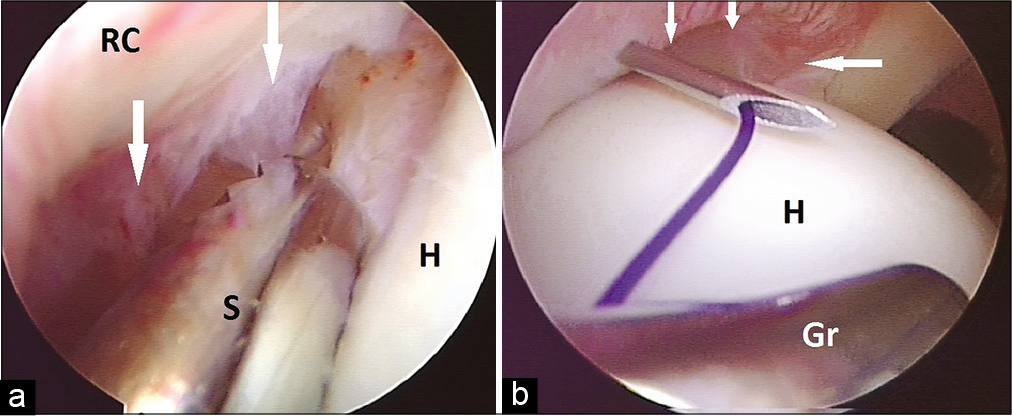
- (a) Partial articular infraspinatus tendon avulsion lesion is shown with white arrows. A shaver (S) is shown preparing the margin of lesion between intact tendon (RC) and humeral head (H). (b) Technique of partial articular infraspinatus tendon avulsion repair. Lesion is shown with white arrows. A transtendinous needle was used to pass PDS suture which was retrieved using grasper (Gr). Later, sutures from the anchor were shuttled over the PDS. Two mattress stitches were thus prepared.
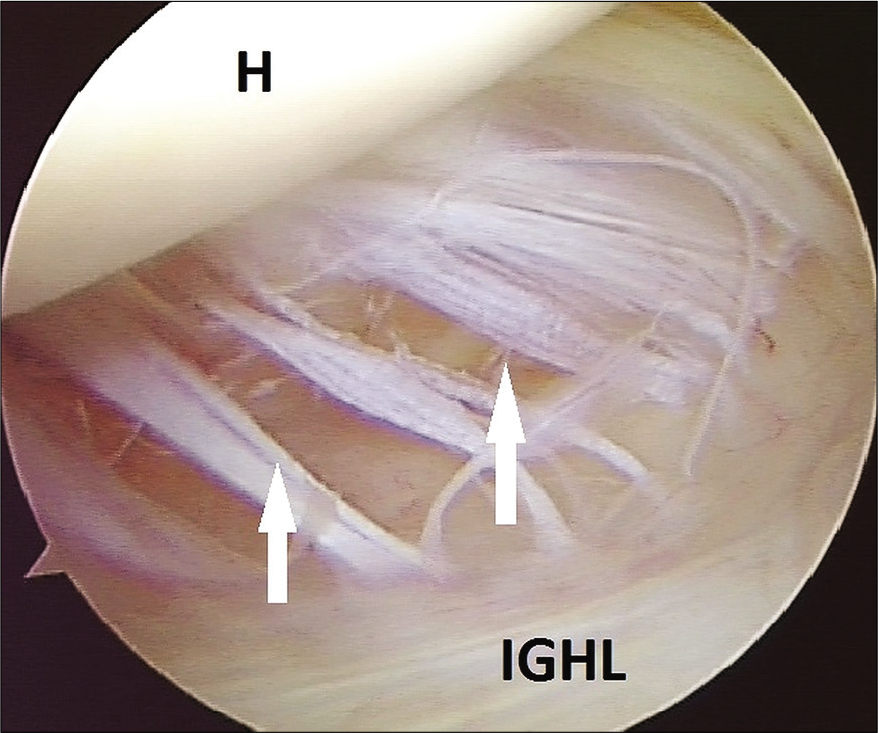
- Humeral avulsion of the glenohumeral ligament lesion is shown with white arrows. Note the humeral head (H) above and the intact part of anterior inferior glenohumeral ligament below. IGHL - Inferior glenohumeral ligament
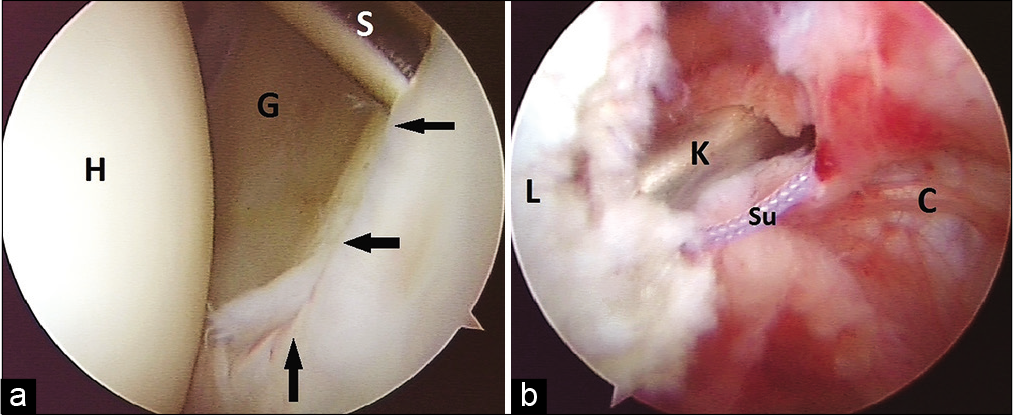
- (a) Posterior labral tear (black arrows) as viewed from the posterior portal. Glenoid (G) and head (H) are marked. Shaver (S) was used to prepare the bed for repair. (b) Posterior labral repair as viewed from the anterior portal. Sutures (Su) are tied over the labrum (L) using a knot pusher (K). The posterior capsule (C) is also seen.
All three lesions were repaired arthroscopically with the HAGL first followed by the PAITA and finally the posterior labral tear. A posterior axillary pouch portal was established and the HAGL lesion was accessed by bringing the limb into extension-internal rotation. The bed of HAGL was prepared in humeral neck using a shaver. A single-loaded Lupine anchor (DePuy Mitek, USA) was inserted and a secure repair along with a capsular shift was achieved using a circumferential plication suture technique previously published.[7] Next, the bed of infraspinatus lesion was prepared from the articular side. Care was taken not to complete the PAITA, but to debride the exposed footprint to bleeding cortical bone. A double-loaded Fastin RC anchor (DePuy Mitek, USA) was inserted and needle localization was used to pass transtendinous 2-0 PDS sutures for shuttling, two stitches were thus prepared but not tied at this stage [Figure 2]. The posterior labrum was then prepared. Poor quality capsulolabral tissues were noted. A single-loaded Lupine (DePuy Mitek, USA) anchor was placed just off the articular margin at 8 o’ clock position. Sutures were shuttled through the capsulolabral tissue and tied [Figure 4]. Subacromial bursoscopy was performed and bursectomy carried out without acromioplasty. Sutures for the PAITA lesion were tied from the bursal side under arthroscopic vision. Portals were closed with subcuticular Monocryl and local ropivacaine was infiltrated. A shoulder immobilizer sling was given in the at-rest position with the elbow by the side and the arm internally rotated to the trunk.
Immobilization was used for first 3 weeks with only wrist and elbow movements allowed. Gentle pendulum exercises were initiated from the 4th week. ROM exercises were started from the 5th week and resistance strengthening began after 10 weeks when he had regained almost full ROM. The strengthening continued until 6 post-operative months. At that stage, he had no pain and full range of flexion, abduction, and internal rotation though external rotation was restricted in the last 15°. Rotator cuff strength had fully returned, there was no apprehension and O’Brien test was negative. Rehabilitation included regular gym with free weights up to 20 kg and push-ups. The SST score had improved to 12/12, Constant score had improved to 94, the Rowe score was 90, Oxford Instability Score 24, and WOSI was 828. Magnetic resonance imaging evaluation at 6 months showed a healed and thickened anteroinferior glenohumeral joint capsule, a healed posterior labrum, and intact and healed rotator cuff [Figure 5]. At 12 months, he was back to normal activities lifting weights at the gym, swimming up to 2 km at a stretch and water skiing though he still lacked terminal 10° of external rotation in abduction. The Constant score was 100, the Rowe score was 95, and SST was 12/12.
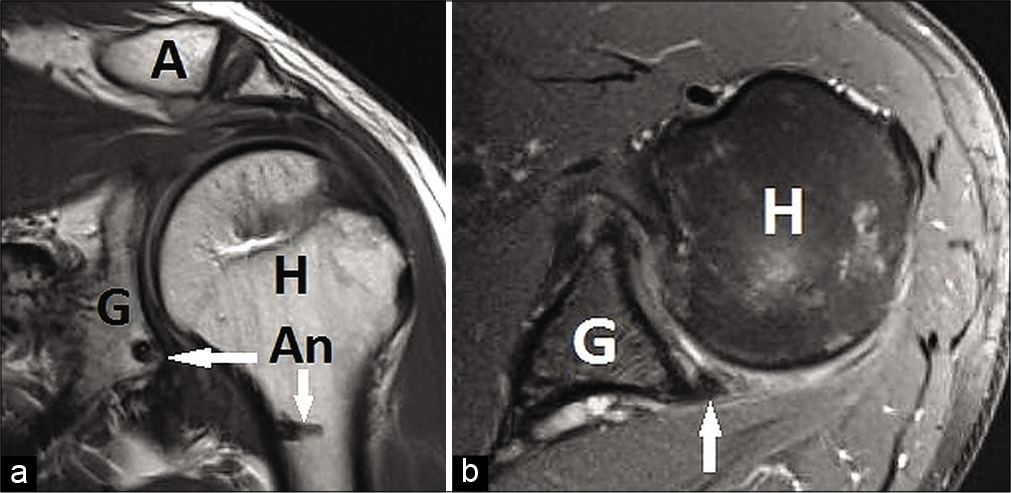
- (a) Six months post-operative coronal magnetic resonance imaging (MRI) scan with white arrows showing two anchors (An) in glenoid (G) and humerus. Healed rotator cuff is seen under acromion (A). Note that the axillary pouch volume is quite reduced as compared to pre-operative (Figure 1a). (b) Six months postoperative axial MRI scan with white arrow showing healed posterior labrum. Glenoid (G) and humeral head (H) are marked.
DISCUSSION
This case report presents the pathoanatomy, surgical technique, and clinical outcome of a previously unreported triad lesion involving an anterior HAGL, posterior labral tear, and a PAITA lesion (HALP triad). Combinations of labral tears with rotator cuff lesions have been previously described.[5,6] Similarly, a combination of anterior Bankart lesion with an anterior HAGL[3] and posterior Bankart lesion with a posterior HAGL has been described.[1] Triad lesions described in literature have involved anterior dislocation with rupture of rotator cuff and injury to the brachial plexus,[8] posterior dislocation with glenohumeral musculoligamentous disruption and neurologic injury,[7] and triple labral lesion involving anterior, posterior, and superior labrum.[9] However, to the best of our knowledge, a triad of lesions involving HAGL, posterior labrum tear, and PAITA has not been reported in the English language literature.
The primary mechanism here was a posteriorly directed shear force during an inclined bench press. This corroborates with the PAITA lesion and posterior labral tear. The presence of a HAGL involving the anterior band of IGHL may be because of a secondary anteriorly directed resultant force vector in the deep press position when the shoulder lies in extension and weights are brought close to the body. It is possible that repetitive microinjury from recreative overhead gym activity caused tear in the cuff and the labrum and was exacerbated by a larger mechanical insult from the bench press. Pouliart and Gagey[10] in their cadaveric study of concomitant rotator cuff and capsuloligamentous lesions found that the humeral head dislocates easily with less extensive capsuloligamentous lesions when rotator cuff lesions are present. This could be the case with our patient, though in contrast to Pouliart and Gagey’s study, our case only sustained a subluxation.
Our patient presented 6 months after injury with pain, but no subjective instability. There were limited clinical signs suggesting mixed impingement and superior labral pathology. In this setting, the magnetic resonance arthrogram revealed pathology in the anterior capsulolabral complex and partial cuff tear. This helped to plan surgery. On arthroscopy, each of the three lesions was significant and could in itself cause the patient’s symptoms. Hence, the decision was taken to repair all the three in the same sitting to restore the anatomy and ensure a complete recovery to full function. Our novel approach to this hitherto undescribed triad lesion has a well-founded basis in literature. However, we stress on anatomical repair to avoid overtightening and post-operative stiffness. Voos et al.[6] have achieved good outcomes with arthroscopic treatment of both cuff and labral lesions in cases where they coexist. Similarly, with concomitant labral tears and HAGL lesions, multiple authors have advocated a simultaneous repair of both.[1,3] A bursectomy was carried out as the last step in the procedure to aid in the visualization of suture tying.
At final follow-up at 1 year, the patient was asymptomatic and had regained almost full movement. He was back to his high level of physical activities. His SST, Constant, and Rowe scores point to an excellent outcome.
CONCLUSION
The HALP triad is a rare combination of HAGL, posterior labral tear, and PAITA lesions in the setting of an episode of shoulder instability. Awareness of this combination will help avoid missed diagnoses. A pathoanatomic approach with concurrent repair of all the three lesions can ensure a good outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Saseendar Shanmugasundaram is on the Editorial Board of the Journal.
References
- Combined posterior Bankart lesion and posterior humeral avulsion of the glenohumeral ligaments associated with recurrent posterior shoulder instability. Arthroscopy. 2007;23:327.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic repair of humeral avulsion of glenohumeral ligament lesion: Anterior and posterior techniques. Tech Hand Up Extrem Surg. 2009;13:98-103.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic shoulder dislocation with combined Bankart lesion and humeral avulsion of the glenohumeral ligament in a professional basketball player: Three-year follow-up of surgical stabilization. Arthroscopy. 2010;26:1404-8.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder instability and related rotator cuff tears: Arthroscopic findings and treatment in patients aged 40 to 60 years. Arthroscopy. 2006;22:270-6.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of combined arthroscopic rotator cuff and labral repair. Am J Sports Med. 2007;35:1174-9.
- [CrossRef] [PubMed] [Google Scholar]
- The reverse terrible triad of the shoulder: Circumferential glenohumeral musculoligamentous disruption and neurologic injury associated with posterior shoulder dislocation. J Shoulder Elbow Surg. 2007;16:e13-7.
- [CrossRef] [PubMed] [Google Scholar]
- The terrible triad: Anterior dislocation of the shoulder associated with rupture of the rotator cuff and injury to the brachial plexus. J Shoulder Elbow Surg. 1995;4:51-3.
- [CrossRef] [Google Scholar]
- Triple labral lesions: Pathology and surgical repair technique-report of seven cases. Arthroscopy. 2005;21:186-93.
- [CrossRef] [PubMed] [Google Scholar]
- Concomitant rotator cuff and capsuloligamentous lesions of the shoulder: A cadaver study. Arthroscopy. 2006;22:728-35.
- [CrossRef] [PubMed] [Google Scholar]






