Translate this page into:
The inverted Cyclops lesion: A case report
*Corresponding author: Pranav Machchhindra Shejul, DNB ORTHO. MNAMS., Department of Orthopedic Surgery, Ortho One Orthopedic Speciality Centre, Coimbatore, Tamil Nadu, India. pshejul@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shejul PM, Sahanand S, Rajan DV. The inverted Cyclops lesion: A case report. J Arthrosc Surg Sports Med. 2023;4:56-9. doi: 10.25259/JASSM_29_2022
Abstract
We report the first-ever Indian case of an inverted Cyclops lesion limiting knee joint range of motion after anterior cruciate ligament (ACL) reconstruction using a hamstring graft. Till date, only three cases of inverted Cyclops have been reported in the literature following ACL reconstruction. Bone tendon-bone graft was used as a graft in one of these cases, and a hamstring graft was used in the remaining two cases for ACL reconstruction.
Keywords
Anterior cruciate ligament (ACL)
Semitendinosus triple + gracilis triple graft (ST3 + G3)
Posterior cruciate ligament (PCL)
INTRODUCTION
Jackson and Schaefer, in 1990, first described a fibrous lesion at the base of the anterior cruciate ligament (ACL) graft, impinging in full extension on the femoral notch.[1] They coined the term Cyclops lesion as the lesion reminded them of the eye of a Cyclops on arthroscopic examination. Rubin et al. described a similar fibrous lesion but at the femoral insertion site of the bone patellar tendon bone ACL autograft. The investigators coined the term “inverted” Cyclops lesion for this lesion.[2] Kambhampati and Ware described an inverted Cyclops lesion following hamstring autograft ACL reconstruction.[3] Pyrko et al. have recently described a similar lesion two years following ACL reconstruction using a hamstring graft but without any limitation to knee extension.[4]
CASE REPORT
A 31-year-old gentleman sustained a twisting injury to his right knee while playing football three months before presenting himself in the outpatient department. He complained of his knee giving way and locking. On examination, he had a positive Lachman and McMurray test. His magnetic resonance imaging (MRI) showed a chronic ACL tear and a displaced bucket handle medial meniscus tear. He underwent ACL reconstruction using six stranded hamstring graft (ST3 + G3) and subtotal medial meniscectomy for a displaced bucket handle medial meniscus tear. Suspensory fixation was done proximally using Endobutton CL 15 mm, and aperture fixation distally with bioabsorbable interference screw. Patient’s knee range of motion was found to be satisfactory during his 1st month follow-up visit from 0° to 90°.
Subsequent monthly reviews up to 6 months showed limitations to complete extension and flexion despite adequate physiotherapy exercises. Dedicated physiotherapy efforts proved futile when the patient developed a fixed flexion deformity of 10° with further flexion up to 90°. In addition to a restricted range of motion, he also complained of pain during activities such as walking, climbing stairs, and squatting.
Further investigation found his X-ray to be normal. However, the MRI showed a fibrous lesion (1.5 cm × 1.4 cm) in front of the intact ACL graft and femoral tunnel extending up to the notch [Figure 1]. The limitation in the patient’s knee range of motion was attributed to this lesion, and he was scheduled for an arthroscopic debridement of the lesion.
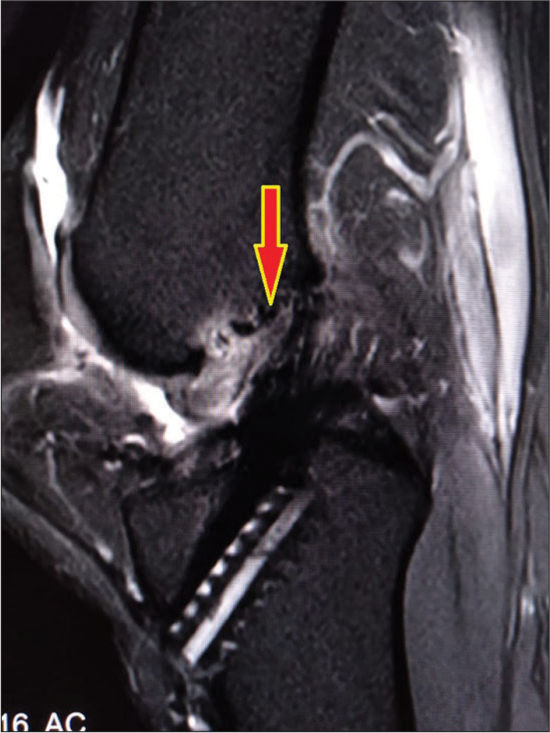
- Magnetic resonance imaging: Sagittal section showing the inverted Cyclops (marked red arrow) arising in front of the anterior cruciate ligament graft.
Examination under anesthesia was unremarkable. The anterior drawer was negative. Lachman’s test had a firm endpoint. Varus and valgus stress test at 0° and 30° was negative. Arthroscopy through standard portals showed ACL graft in excellent condition with proper tension. PCL was normal. It also showed a lesion at the roof of the femoral intercondylar notch – the inverted Cyclops lesion [Figure 2]. This lesion did not appear to have any communication with the femoral tunnel, but it was impinging on the tibial side and limiting the full extension of the knee. It was located in the anterior part of the roof of the notch and extended deeper into the notch toward the ACL graft. This was debrided arthroscopically after adequate peripheral mobilization of the fibrous lesion and protecting the reconstructed ACL [Figure 3]. Notchplasty was done from 8 o’clock to 12 o’clock. Following the arthroscopic debridement, his range of motion improved from 0° to 130° immediately on the operating table [Figures 4a and b]. Prone physiotherapy exercises and range of motion were initiated on the day of surgery. The patient recovered well. Subsequent follow-ups up to a year did not show restriction in the patient’s range of motion. His knee range of motion and pain improved significantly.
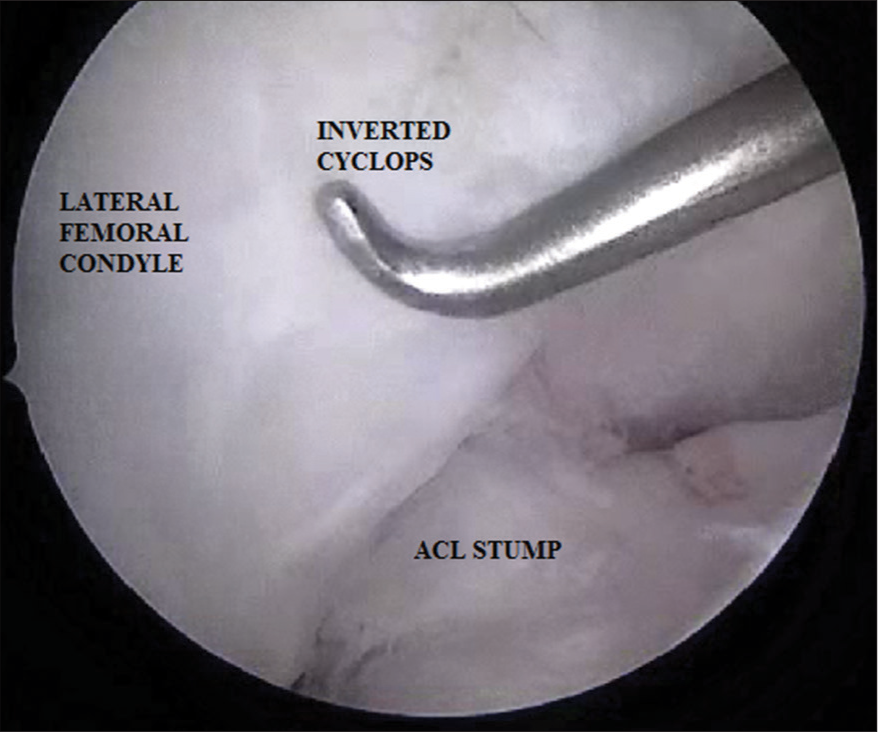
- Arthroscopic location of inverted Cyclops seen through anterolateral viewing portal.
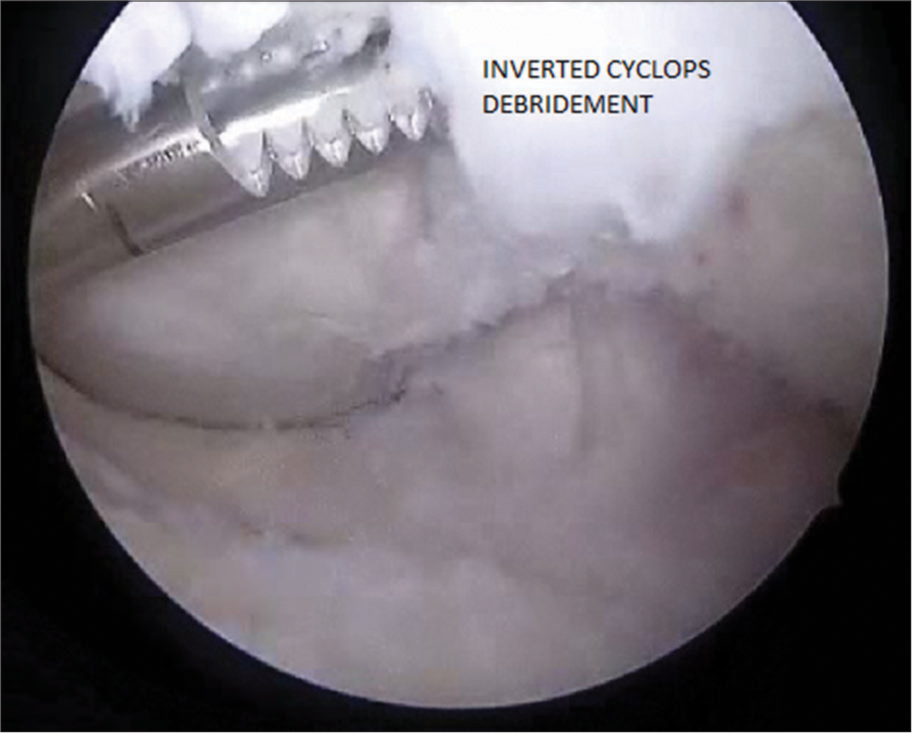
- Debridement of inverted Cyclops with an arthroscopic shaver.

- (a) 130° flexion achieved after arthroscopic debridement of inverted Cyclops. (b) A complete extension was achieved after arthroscopic debridement of the inverted Cyclops.
DISCUSSION
Jackson and Schaefer, in 1990, first coined the term Cyclops lesion. They postulated that the lesion was a result of excess tibial tunnel drilling and preparation. Particularly due to the angle and direction of the drill used to make the tibial tunnel. There is a tendency to create tissue and cartilage overhang anterior and lateral to the drill hole, causing it to stay in the tunnel if not properly irrigated and debrided. The passing of the graft distal to proximal through the tunnel then may push this reaming debris out anterior to the tunnel onto the intra-articular tibial surface, where the tissue then becomes part of the fibroproliferative process that ultimately forms the Cyclops lesion, just anterolateral to the tibial tunnel entrance. They reported in their study that this complication can be minimized by complete debridement at the tibial tunnel and adequate notchplasty.[1]
In another study, Marzo and Bowen suggested that the lesion develops due to repeated impingement of exposed collagen fibers of the graft with the intercondylar notch over time. An injury response develops that progresses from acute inflammation to disorganized scar formation and, eventually, the formation of fibrocartilage.[5]
Watanabe and Howell, in 1995, suggested that cystic lesions arise from injury to the graft caused by either intraoperative manipulation or improper placement of the tunnels, causing impingement.[6]
Delince et al. suggested that the nodules arise from either the drilling debris, remnant of the ACL stump, or broken graft fibers often caused by impingement on the graft secondary to malpositioning of the tunnels. They suggested the use of sequential drills with increasing diameters to minimize large debris fragments, meticulous attention to tunnel positioning, and enlargement of the notch when future impingement is predicted or found on second-look arthroscopy to prevent the formation of the lesion.[7]
Various other theories were later proposed. These included compressive loading, microtrauma, micromotion, partial injury to the ACL graft, and irritation due to impingement. It is now accepted that the origin is multifactorial.
Inverted Cyclops
Hart et al. coined the term “inverted Cyclops lesion” for the case of a 14-year-old boy with a T-shaped intercondylar fracture at the level of the distal physis. He developed a loss of extension secondary to a femoral-sided fibrous nodule.[8]
The first case of an inverted Cyclops following an ACL reconstruction was reported by Rubin et al., in which a bone-patellar tendon-bone graft was used. They have demonstrated a stalk of the Cyclops lesion arising from the outlet of the femoral tunnel in pre-arthroscopy MRI.[2] However, we, like Kambhampati and Ware, could not establish any connection between the lesion and the femoral tunnel on arthroscopy, though it was extending deeper into the notch toward the ACL graft.[3] Following arthroscopic excision of the lesion and notchplasty, our patient regained full range of movement of the knee.
Our case was closely related to that of Kambhampati and Ware with respect to the use of hamstring grafts. It only differed in the strands of the hamstring graft made while preparing the graft. While Kambhampati and Ware had used a four-strand hamstring graft, ours was a six-strand graft. Tonin et al. reported it in patients with ACL injuries without any reconstruction surgery. In the absence of surgery, the origin was thought to be due to the avulsion of pieces of bone from the attachment of the ligament.[9]
CONCLUSION
Cyclops and inverted Cyclops lesions are serious complications following ACL reconstruction. The etiology of Cyclops lesions can be attributed to the remnants of debris coming out of the tibial tunnel while passing the graft, remnants of ACL stump, or the impingement of the ACL graft into the notch.
Strategies to prevent this were first described by Jackson and Schaefer, which included attention to tunnel positioning and notchplasty to avoid impingement, debridement of the tibial tunnel before the graft is advanced, and removal of osteocartilaginous fragments.
Both Cyclops and inverted lesions can be multifactorial in origin. Causative factors leading to the formation of cystic lesions can also be extrapolated to the development of inverted cyclops lesions.
A literature review of previous case reports has shown that the lesion begins to establish between 2 and 3 months following ACL reconstruction surgery. A high degree of suspicion, along with imaging studies like MRI, can help diagnose these lesions.
For the regular Cyclops lesion, the debris is thought to come from the tibial tunnel, while for the inverted Cyclops lesion, it is from the femoral tunnel. Like debridement of the tibial tunnel is done as a standard practice to prevent the formation of a Cyclops lesion, attention should be paid to debridement of the femoral tunnel to prevent an inverted Cyclops.
Both the Cyclops and inverted Cyclops cause mechanical intra-articular block to a range of motion as well as pain. No previous studies have reported the lesion to resolve by itself. Physiotherapy exercises were tried without much benefit to the cause by all authors reporting inverted Cyclops before proceeding to arthroscopic debridement of the lesion. Excision of the lesion has led to satisfactory results in patients by improving the range of motion and pain. Arthroscopic excision of the inverted Cyclops is the standard of care for causing the resolution of symptoms. No previous study, including ours, has reported a recurrence of the lesion.
Ethical Approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Santosh K. Sahanand is on the Editorial Board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cyclops syndrome: Loss of extension following intraarticular anterior cruciate ligament reconstruction. Arthroscopy. 1990;6:171-8.
- [CrossRef] [PubMed] [Google Scholar]
- Extension loss secondary to femoral-sided inverted cyclops lesion after anterior cruciate ligament reconstruction. J Knee Surg. 2009;22:360-3.
- [CrossRef] [PubMed] [Google Scholar]
- Inverted cyclops lesion after anterior cruciate ligament reconstruction. Ann R Coll Surg Engl. 2012;94:e99-100.
- [CrossRef] [PubMed] [Google Scholar]
- Inverted cyclops lesion without extension block: A case report and literature review. Bull Hosp Jt Dis (2013). 2015;73:61-4.
- [Google Scholar]
- Intraarticular fibrous nodule as a cause of loss of extension following anterior cruciate ligament reconstruction. Arthroscopy. 1992;8:10-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic findings associated with roof impingement of an anterior cruciate ligament graft. Am J Sports Med. 1995;23:616-25.
- [CrossRef] [PubMed] [Google Scholar]
- Different aspects of the cyclops lesion following anterior cruciate ligament reconstruction: A multifactorial etiopathogenesis. Arthroscopy. 1998;14:869-76.
- [CrossRef] [PubMed] [Google Scholar]
- Fixed flexion deformity of the knee following femoral physeal fracture: The inverted cyclops lesion. Injury. 2004;35:1330-3.
- [CrossRef] [PubMed] [Google Scholar]
- Progressive loss of knee extension after injury. Cyclops syndrome due to a lesion of the anterior cruciate ligament. Am J Sports Med. 2001;29:545-9.
- [CrossRef] [PubMed] [Google Scholar]






