Translate this page into:
The role of in-office needle arthroscopy in orthopedic practice: A review
*Corresponding author: Vineet Thomas Abraham, Department of Orthopaedics, All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh, India. abrahamvineet@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abraham VT, Kambhampati SBS, D’Ambrosi R. The role of in-office needle arthroscopy in orthopedic practice: A review. J Arthrosc Surg Sports Med. 2025;6:16-23. doi: 10.25259/JASSM_48_2024
Abstract
Background and Aims:
In-office needle arthroscopy (IONA) has emerged as a valuable diagnostic and therapeutic tool in orthopedic practice. It offers a minimally invasive approach to evaluating and treating various joint conditions. This review aims to explore the clinical applications, benefits, and challenges of IONA in orthopedic practice.
Materials and Methods:
A comprehensive literature search was conducted to identify relevant studies on IONA. The included articles were analyzed to extract information on the clinical applications, techniques, outcomes, and limitations of this procedure.
Results:
IONA has been successfully applied to a wide range of joints, including the knee, shoulder, ankle, wrist, elbow, and hip. It has demonstrated superior diagnostic accuracy compared to traditional imaging techniques, particularly for intra-articular pathologies. IONA can be used for both diagnostic purposes and therapeutic interventions, such as meniscus repair, rotator cuff repair, labral repair, and synovial biopsy.
Conclusion:
IONA offers a minimally invasive and cost-effective approach for diagnosing and treating various orthopedic conditions. It provides accurate visualization, reduces the need for traditional surgical procedures, and improves patient outcomes. However, further research is needed to establish its long-term efficacy and identify its optimal applications.
Keywords
In-office needle arthroscopy
Orthopedics
Minimally invasive surgery
Arthroscopy
Sports medicine
Joint disorders
INTRODUCTION
In-office needle arthroscopy (IONA) was first described in the early 1990s,[1] but its usage has increased recently because of improvements in instruments, image quality, and technique.[2,3] The needle arthroscope is typically used as an office procedure; the advantages of the needle arthroscope include a more miniature, lightweight 2 mm camera, allowing for a minimally invasive approach with even smaller incisions than standard arthroscopy. The sheath of the camera is also smaller, resulting in decreased requirement of arthroscopy fluid and decreased postoperative swelling.[4]
IONA is gaining traction as a minimally invasive alternative to conventional arthroscopy, which is performed in an operation theater. IONA procedures can be conducted in outpatient department rooms, similar to nanoscopy or gastroscopy procedures, providing orthopedic surgeons with valuable diagnostic and therapeutic tools. It also allows better pre-operative planning and thus reduced operative time during subsequent arthroscopic procedures. IONA facilitates the diagnosis and treatment of various conditions affecting both the upper and lower limbs under local anesthesia, circumventing the potential adverse effects associated with general anesthesia and spinal/epidural anesthesia.
Historically, IONA has been in use for many years but has faced challenges such as inadequate visualization and a lack of suitable instruments for interventions. However, the introduction of chip-on-tip technology has significantly enhanced the visual capabilities of the arthroscope. In addition, the availability of specialized micro-instruments now allows for intricate intra-articular procedures, transforming the arthroscope from a purely diagnostic tool into a therapeutic one.
This article will explore the diverse applications of the in-office needle arthroscope, beginning with diagnostic arthroscopy.
MATERIALS AND METHODS
A PubMed search for in-office needle arthroscopy (IONA) revealed 473 articles; of these, 374 had been published in the past 10 years. A search in the Cochrane Library “in-office needle arthroscopy” provided two search results, of which one was relevant.
Exclusion criteria were articles in languages other than English and articles that discussed arthroscopy with the regular arthroscope. The reference lists of these articles were searched for further relevant studies. Since we were covering a large number of joints, we included review articles and more recent articles describing needle arthroscopy of a particular joint. After we accounted for the duplication of the articles and the overlap of search results, we included a total of 31 articles in this narrative review.
RESULTS AND DISCUSSION
Clinical applications, benefits, and challenges
Clinical applications
There are multiple clinical applications of IONA. Starting with the knee, all the applications are discussed in this review [Table 1].
| Joint | Diagnostic applications | Therapeutic applications |
|---|---|---|
| Knee | Meniscus evaluation, ligamentous tears, cartilage damage, synovial inflammation | Meniscus repair, meniscectomy, synovial biopsy, patellofemoral release, Osgood-Schlatter disease, debridement following infections |
| Shoulder | Partial rotator cuff tear, complete rotator cuff tears, labral tears, impingement | Rotator cuff repair, labral repair, subacromial decompression, biceps tenotomy, biopsy |
| Ankle | Osteochondral lesions, impingement, ligament injuries | Ankle ligament repair, tendon releases, loose body removal, bone marrow stimulation |
| Wrist | Carpal tunnel syndrome, TFCC tears | TFCC repair, distal radius fracture fixation |
| Elbow | Loose bodies, osteochondral lesions | Loose body removal, osteocapsular arthroplasty, fracture fixation |
| Hip | Labral tears, femoroacetabular impingement | Labral repair, hip joint debridement |
IONA: In-office needle arthroscopy, TFCC: Triangular fibrocartilage complex
Diagnostic arthroscopy
Diagnostic arthroscopy offers numerous advantages over traditional magnetic resonance imaging (MRI), which has been the gold-standard diagnostic tool. Arthroscopy is invaluable across various joints where MRI alone may not suffice for planning management strategies.
According to Zhang et al., IONA can lead to cost savings and enhanced diagnostic accuracy, particularly for intra-articular issues such as meniscal, ligamentous, and chondral defects in the knee.[3] Unlike MRI, which requires interpretation by a skilled musculoskeletal radiologist or a surgeon proficient in MRI analysis, IONA provides direct visualization, increasing diagnostic precision. Their meta-analysis, reviewing five studies involving 226 patients, highlighted that the sensitivity of IONA ranged from 90.5% to 100%, while MRI ranged from 59.5% to 91.4%. IONA’s specificity was between 93.1% and 100%, compared to MRI’s 82.9–100%. In addition, the positive and negative predictive values for IONA were reported as high as 100% and 93.2%, respectively, surpassing those of MRI.[3]
Further studies, such as those by Krakowski et al. from 2014 to 2017, evaluated MRI’s effectiveness in diagnosing medial meniscus (MM), lateral meniscus, and anterior cruciate ligament (ACL) tears, demonstrating varying levels of sensitivity and specificity across different conditions.[4] Phelan et al. corroborated these findings, emphasizing MRI’s distinct accuracy metrics for different tears.[5]
Despite the affordability and accessibility of MRI in regions like India, where cost and wait times are minimal, IONA provides additional diagnostic benefits. It allows surgeons not only to visualize but also physically probe the tissue, offering insights into the extent of damage, such as in partial ACL tears or differentiating between degenerative and traumatic meniscal tears. This tactile feedback is crucial in deciding surgical approaches for ACL reconstructions or meniscal repairs, also aiding in assessing the severity of cartilage damage.
IONA proves invaluable as a diagnostic tool, particularly in planning interventions such as high-tibial osteotomy for osteoarthritis in the knee. By assessing the involved compartments, IONA enables precise surgical decisions.
For the shoulder, IONA’s capabilities extend to conditions where MRI may fall short. In cases of partial rotator cuff tears, where MRI is inconclusive regarding the need for surgery, IONA allows surgeons to visualize and probe the tear directly, facilitating a more informed decision-making process. Similarly, IONA is instrumental in assessing shoulder instability issues, such as the quality of labral tissue, the extent of glenoid bone loss, and the size of Hill-Sachs lesions. This information is crucial for determining whether to proceed with labral repair procedures, with or without remplissage or a Latarjet operation.
IONA for synovial biopsy in inflammatory arthritis
Andreozzi et al. have explored the application of knee IONA for synovial biopsies in inflammatory arthritis cases.[6] Utilizing IONA, they assessed the pathological characteristics and inflammation grade from synovial biopsies, which then guided adjustments in treatment strategies for drug-resistant monoarticular inflammatory arthritis. This technique, involving up to three synovial tissue samples per procedure, has proven to be an effective and tolerable approach, enhancing treatment precision for conditions such as rheumatoid and psoriatic arthritis.[7]
Limitations of IONA
While IONA is a robust intra-articular diagnostic tool, it does not assess extra-articular ligament injury or subchondral bone changes, which can be associated with osteochondral lesions, as highlighted by Zhang et al.[3] In addition, Mc Intyre cautioned against using IONA in acute knee injuries and hemarthrosis, where it may not be indicated.[8]
Patient experience and satisfaction
The awake arthroscopy approach of IONA has significantly enhanced patient satisfaction, as noted by Labib and Hanna, 2022.[8] This method allows surgeons to narrate the procedure in real time, fostering transparency and trust. Studies by Neal et al. and Kirschner et al. further confirm high patient satisfaction, with many patients appreciating the opportunity to view the arthroscopic feed alongside the surgeon, thereby enhancing their understanding and comfort during the procedure.[9,10] On comparing IONA to traditional arthroscopy, there are quite a few advantages that have been listed in Table 2.
| Feature | IONA | Traditional arthroscopy |
|---|---|---|
| Invasiveness | Minimally invasive | More invasive |
| Procedure setting |
Outpatient setting | Operating room |
| Anesthesia | Local anesthesia | General or regional anesthesia |
| Recovery time | Shorter recovery time | Longer recovery time |
| Cost | Generally less expensive | More expensive |
IONA: In-office needle arthroscopy
Knee
Meniscal injury and IONA
When comparing IONA to traditional operating room arthroscopy, Abbas et al. concluded that IONA is a cost-saving option for patients undergoing partial media meniscectomy.[11] This approach not only reduces healthcare costs associated with meniscal injuries but also prompts further evaluation into patient perceptions of IONA versus traditional arthroscopy. Future clinical trials are necessary to determine IONA’s efficacy, patient-reported outcomes, and potential complications.
Partial meniscectomy
Partial meniscectomy, a procedure often performed using a Nanoscope, benefits from advancements in miniature surgical instruments. Lavender et al. employed nano-biters and nanoshavers to execute partial medial meniscectomies, providing an incisionless option that requires no cuts larger than 2 mm when using 2 mm meniscal biter and shaver (Arthrex).[12] This technique utilizes cannulas of various lengths to facilitate the easy passage of instruments and, if necessary, the dilation of portals to accommodate instrumentation. To compensate for fluid loss to suction, increasing the pressure of the pump to 30 mmHg may be advantageous. The specifics of working portals will depend on the tear’s location and pattern. In 2020, Quinn et al. described a similar approach using nano instruments to perform medial meniscectomy of the posterior horn and body, which they completed in an average of 15 min with around 250 mL of arthroscopy fluid.[13]
Meniscus repair
Lavender et al., in their 2021 study, highlighted the benefits of using a Nanoscope for meniscus repair, which includes less fluid introduced into the joint, smaller portal sizes, and reduced trauma to the knee.[14] However, they also noted disadvantages such as the technical demands and steep learning curve associated with using a 0° scope. In addition, the cost of single-use scopes compared to standard reusable scopes poses a financial consideration.
They also described the pearls and pitfalls of this procedure in their article [Table 3].
| Pearls | Pitfalls |
|---|---|
| Familiarization with the 0° optic before surgery will improve the surgeon’s experience using the Nanoscope. | The camera uses a 0° view that has an initial learning curve for surgeons. |
| IONA favors a straight or an in-line approach, and sweeping motions should be avoided. | IONA instruments are more delicate and malleable than the standard arthroscopic equipment because of their small size, which can thus result in bending or even breakage. |
| The use of an inflow on a separate sheath from the camera may improve visualization because of the reduced flow restriction. | During diagnostic NA, a surgeon may find an indication to use the standard arthroscopy versus NA, leading to potential increased cost. |
| The usage of far medial and lateral portals permits open access to the standard portals for instrumentation, such as shavers, probes, or punches. | During the learning curve of IONA, there is an increased risk of iatrogenic chondral damage. |
IONA: In-office needle arthroscopy, NA: Needle arthroscopy
Cyclops lesion excision
Cyclops lesions, as discussed by Kambhampati et al. in the Orthopaedic Journal of Sports Medicine, are accessible and removable using a Nanoscope.[15] Lavender et al. (2022) highlighted that the Nanoscope technique results in reduced post-operative pain and even swelling, thus reducing the recovery time. The recommended approach is to view the cyclops through a medial portal with the Nanoscope and excise it through a lateral portal using a 3.5 mm shaver.[16]
Lateral release
Patients experiencing persistent pain in the patellofemoral joint after conservative treatment may benefit from diagnostic arthroscopy of the patellofemoral joint and the surrounding soft tissue. This standard orthopedic procedure provides diagnostic and therapeutic insights into the parapatellar envelope. IONA is utilized to treat patellofemoral pain and lateral patellar maltracking by doing a lateral parapatellar retinacula release, as described by Neal et al. (2023).[9] Diagnostic arthroscopy is done first using the lateral portal, and the medial portal is then created and becomes the viewing portal. A 90° ablator is then inserted into the lateral portal. The procedure starts at the superior aspect of the trochlea, and then, the ablator moves laterally over the anterior edge of the lateral femoral condyle. IONA provides excellent visualization and enables sequential incision of the deep layers, moving more superficially with each pass. Care is taken to avoid injuring the superior and inferior lateral genicular arteries during the procedure.
Osgood-Schlatter disease
Kamiya et al. utilized IONA with ultrasound guidance for the excision of Osgood-Schlatter disease.[17] The needle arthroscope is inserted lateral to the proximal patellar tendon and is maneuvered between the ossicle and the anterior surface of the tibia under the guidance of ultrasound. Another working portal is created on the medial side of the proximal patellar tendon. Bursectomy is done, and the proximal border of the ossicle is visualized. The ossicle is then removed using a 2 mm punch in fragments. Any remnant is confirmed using the ultrasound and excised. The patient is allowed full weight-bearing mobilization and full range of motion. The advantage of the procedure is that it minimizes the damage to the patellar tendon and facilitates an early recovery.[17]
Biopsy techniques
Synovial and bone biopsy for total knee arthroplasty pain
Lavender et al. (2021) used the IONA to perform synovial and bone biopsy in patients experiencing pain following total knee replacement without utilizing the standard arthroscopy portals.[18] They highlighted several advantages of this method, including its potential for tissue diagnosis, reduced risk of contamination compared to open approaches, and its utility in intensive care settings. This less invasive technique also allows for the inspection of prosthetic components and is considered particularly useful in diagnosing unexplained pain post-surgery.[18]
Assessment of inflammatory monoarthritis
Andreozzi et al. conducted a study to evaluate the safety, tolerability, and diagnostic accuracy of IONA for assessing knee inflammatory monoarthritis and refining treatment options.[6] Using a 2.75-mm grasper, biopsies were obtained through accessory working portals, located 1 cm medial and lateral to the standard AM and AL portals, respectively. In their study of 12 patients, where three biopsies were taken from each, they achieved a success rate of 97% in obtaining useful diagnostic tissue.
Shoulder
Subacromial decompression technique
Owusu-Sarpong et al. described a technique for performing IONA-based subacromial decompression, which includes both bursectomy and acromioplasty.[19] After positioning the patient in a 70–80° beach chair position, the procedure begins by marking the relevant surface anatomy and portal sites. LA is administered with a mixture of 1% lidocaine and 0.5% bupivacaine. Using a standard posterior portal, diagnostic arthroscopy is conducted. A 90° radiofrequency ablator and a 2 mm shaver are then used for the subacromial bursectomy to expose the undersurface of the acromion. The acromial branch of the thoracoacromial artery is cauterized. Acromioplasty is performed using a 3 mm nano resection burr, from lateral to medial, gradually resecting the anterior and lateral bony spurs.[19] The authors further outlined several benefits of IONA, including reduced costs, decreased surgical morbidity, lower anesthesia risks, and expedited post-procedural recovery. The method boasts higher diagnostic accuracy, sensitivity, and specificity compared to MRI and offers a decreased risk of both chondral damage and nerve injury. Patients typically experience less pain and often avoid narcotic post-surgery, favoring over-the-counter pain management like acetaminophen and NSAIDs.[19]
Rotator cuff tear
Diagnostic and treatment advantages with IONA
IONA proves especially beneficial for managing partial rotator cuff tears, providing precise details about the tear’s size and location, which aids in deciding between surgical and conservative treatments. Lavendar C described a technique that involves using a reduced number of portals, typically a single lateral standard portal for rotator cuff repair, minimizing shoulder swelling post-operation. The Nanoscope, used during the procedure, minimizes injury to the capsule and the infraspinatus.[20]
Clinical applications and limitations
Indications: Partial thickness rotator cuff tears (bursal or articular-sided), small minimally retracted full-thickness tears, and anterior or posterior labral tears.
Contraindications: Large or retracted rotator cuff tears or repairs, which will require additional procedures such as biceps tenodesis or distal clavicle excision.
Pitfalls: Due to its small size, the Nanoscope can be fragile and may only sometimes clearly display the pathology, in which cases switching to a standard arthroscope is recommended.
Innovative techniques for rotator cuff repair
Lavender et al. (2022) described a minimally invasive repair technique using a double-lumen cannula that allows both direct visualization and access to instruments to treat the rotator cuff tear.[21] A standard posterior portal with a smaller incision is made. The Nanoscope is passed. A spinal needle is passed, and the location of the lateral portal is marked. A Passport Dual Lumen Cannula (Arthrex) is inserted using a hemostat. This portal is used both as a working and viewing portal. After clearing the subacromial space and identifying the tear, the site of the medial anchors is identified using a needle, and the anchors are then inserted. The IONA is passed through the auxiliary lumen of the cannula. The suture retriever passed through the other lumen is used to retrieve the suture tape coming out of the anterior-most anchor. The suture tape is then loaded into a suture passing device, and the passer is then used through the main lumen of the cannula to pass the anterior and posterior respective sutures through the rotator cuff. The sutures are retrieved superiorly before pulling the entire suture out the lateral portal to prevent knots. If a double row repair is planned, then 1 anterior suture and 1 posterior suture are retrieved from lateral while still viewing with the Nanoscope through the auxiliary lumen. These are then placed through a Knotless SwiveLock anchor, and the lateral row anchor is punched laterally in standard fashion. Hence, the repair is completed using just 2 portals.[21]
Adhesive capsulitis: Minimally invasive treatment
Yadoji et al. (2023) reported on an arthroscopic capsular release using the Nanoscope.[22] This procedure includes a diagnostic arthroscopy followed by targeted cuts within the rotator interval capsule using a nano punch, resembling a piecrusting technique. Subsequent anteroinferior capsulotomy and debris removal are performed with a 2.5 mm shaver. This technique, potentially developed as an outpatient procedure with minimal infrastructure, underscores the need for careful patient selection and further studies to compare its effectiveness against conventional methods.[22]
Wrist arthroscopy
Munaretto et al. (2022) examined the proximity of neurovascular structures and tendons during wrist arthroscopy using a 1.9 mm Nanoscope.[23] This smaller scope size may enhance safety when establishing dorsal wrist arthroscopy portals. Notably, the 1–2 portal was found to be an average of 3 mm from the superficial branch of the radial nerve and about 2.1 mm and 1.4 mm from the extensor pollicis brevis tendon and radial artery, respectively.[23]
Dittman et al. also conducted a study and found that the Nanoscope did not pierce any neurovascular structures and was away from critical structures except for the radial artery.[24] Choke A et al. described the arthroscopic-assisted distal radius fracture fixation using the Nanoscope.[25] Using the trans-FCR approach, the fracture site is exposed, gross extra-articular fracture reduction is done under fluoroscopy control, and fracture is fixed provisionally with K-wires. Arthroscopy is used to fine-tune the intra-articular fragment reduction. Dry scope with intermittent irrigation is preferred. The portal, which is placed over the ulnar head, optimally visualizes the intra-articular distal radius fixation and minimizes interference with the fracture fragments. 1.2 mm K-wire can be used as a joystick for easy manipulation while reducing the fracture. Ulnar fragments are stabilized as a priority before stabilizing the radial fragment; this is useful, especially when reducing the comminuted AO C3 fractures. The authors concluded that the procedure has a steep learning curve and will require additional operative time initially. This technique is a valuable adjunct to achieve precise anatomical fracture reduction in comminuted fractures of the distal radius.[25]
Ankle arthroscopy
Duenes ML et al. mentioned in their article that IONA has revolutionized the management of ankle and foot disorders.[26] IONA can be used to manage a variety of disorders, including osteochondral lesions of the Talus, anterior ankle impingement, posterior ankle impingement, hallux rigidus, repair of lateral ankle ligaments, and treatment of Achilles, peroneal and posterior tibial tendon pathologies. 96% of the talus surface and 85% of the tibia plafond can be reached with IONA. Excellent outcomes have been reported in terms of return to sport, clinical sores, and reduced complications following IONA for these pathologies.
Technique of IONA for anterior ankle impingement
The patient is positioned comfortably in the supine position with the operative foot free and off the table. The surface anatomy is marked along with the portals. The anteromedial and anterolateral portals are established, and diagnostic arthroscopy is performed. Using A 2.0-mm shaver soft-tissue synovial hyperplasia, scar tissue is removed to visualize the anterior aspect of the joint. The tibia and talar neck are then visualized. Any exostoses that may potentially cause impingement are resected using a 2.0-mm shaver or a 3-mm burr. After adequate resection and confirmation that no impingement has been seen, the portals are closed.[26]
IONA is being used in both the assessment and management of ankle sprains. Butler et al., in their article, have concluded that repair of the anterior talofibular ligament using the IONA provides a minimally invasive approach both to the diagnosis and treatment of chronic lateral ankle instability.[27] The technique results in limited soft-tissue trauma, thus facilitating a rapid return to daily work and sports.
Elbow arthroscopy
Rapariz JM et al. did a cadaveric study where they studied the anterior transbrachial portal, which is made just lateral to the biceps tendon, and the scope is inserted through the brachialis muscle and the anterior capsule.[28] Arthroscopy is then performed. When dissection was done on the cadaver, they found that the cannula was an average of 12.92 mm away from the radial nerve, 22.27 mm from the median nerve, and 16.8 mm from the brachial artery. They found that this portal is useful and allows complete visualization of the anterior compartment of the elbow. Furthermore, it allows direct visualization of the posterolateral compartment of the elbow.[28] Peters M et al. described the portals and techniques for elbow arthroscopy. They described multiple portals, both anterior and posterior, for access to all the regions of the elbow with the Nanoscope.[29] The technique described by them and portals can be used to do various procedures such as osteocapsular arthroplasty and fracture fixation.
Hip arthroscopy
McMillan S et al. have described arthroscopic hip labral repair using IONA. Hip arthroscopy cases have increased by over 600% over the past decade.[30] The advantage of a Nanoscope is that it has a 120° field of view and can be percutaneously repositioned. The authors use a postless traction system in a lateral decubitus position. After preparation, needle arthroscopy is performed using the standard anterolateral (AL) and the mid-anterior (MA) portal. Distal anterolateral accessory portals are placed as needed for the placement of the anchor.
First, the AL portal is localized with an 18G spinal needle under fluoroscopy control. The suction seal is released, creating more potential space for the Nanoscope to be inserted. 160 mm 0 deg scope is used; however, in thinner patients, 95 mm 0 deg scope may also be used. First, acetabuloplasty is performed using a burr which is inserted using the MA portal. The labral repair is then carried out using anchors. The Nanoscope, because of its low profile, minimizes iatrogenic cartilage and labral damage on entry into the central compartment. It has the advantage of good visualization across the central and peripheral compartments during femoral osteoplasty and anchor placement. It saves on surgical fluid. Typically, for a labral repair using the traditional arthroscope, the amount of fluid used is 12000– 15000 mL, but with the Nanoscope, the usage is only between 1200 and 1600 mL. The drawbacks include the fact that not all Nanoscopes are designed for a hip length of 160 mm. Furthermore, it is difficult to manipulate the Nanoscope in more muscular or heavier patients.[30]
General procedure and setup for nanoscopy
The procedure room is set up similarly to an operating theater. The patient is positioned on an appropriate table, and part is prepared with a solution of povidone-iodine and draped in a sterile manner. An arthroscopy pump with an inflow of 1 L of 0.9% normal saline mixed with 5 cc of epinephrine to promote hemostasis is used. Optionally, the fluid can also be administered through a syringe connected to the handpiece.
The needle arthroscopy set includes a needle scope, obturators, and cannulas, with additional instrumentation selected based on the specific case [Figure 1]. Local anesthesia typically involves a mix of lidocaine and bupivacaine, with concentrations varying by surgical site and procedure duration. A scrub technician and an additional staff member assist with equipment during the procedure. The IONA can demonstrate the intra-articular structures of the joint clearly [Figure 2].

- Needle arthroscope set and portal marking for surgery. (a) Equipment used for nanoscopy. (b) Portals used for Nanoscopy. Reproduced from Quinn et al. Copyright © The Author(s). 2020, Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/).
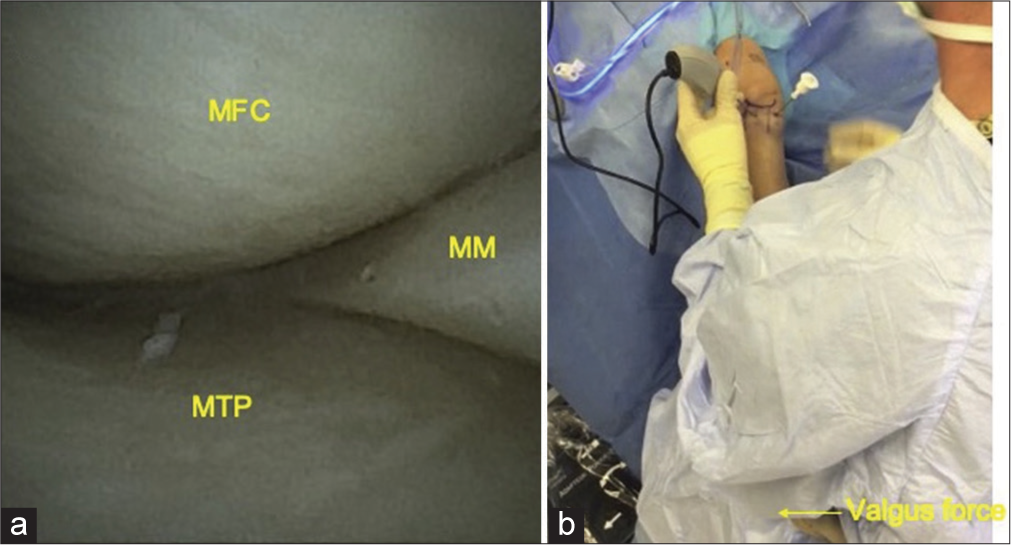
- (a) The medial compartment of the knee - Medial femoral condyle (MFC), medial tibial plateau (MTP) and medial meniscus (MM). (b) External picture - Needle arthrosocope in the central portal and cannula in the medial portal. Reproduced from Quinn et al. Copyright © The Author(s). 2020, Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/).
Arthroscopy portal sites are then anesthetized with 10 cc of 1% lidocaine, followed by an injection of 20cc of 1% lignocaine and 0.5% bupivacaine through the portals into the joint. Portal incisions are made with an 11-blade and closed post-procedure using Steri-Strip adhesive wound closure strips.
The advantages and disadvantages of IONA are listed in Table 4.
| Advantages | Disadvantages |
|---|---|
| Minimally invasive | Requires specialized equipment and training |
| Outpatient setting | May not be suitable for complex procedures |
| Shorter recovery time | Limited visualization compared to traditional arthroscopy |
| Cost-effective | Potential for iatrogenic injuries |
| Improved patient outcomes | Not suitable for all joint conditions |
IONA: In-office needle arthroscopy
HIGHLIGHTS
IONA offers superior diagnostic accuracy compared to traditional imaging techniques, particularly for intraarticular pathologies.
IONA can be used to diagnose and treat various joint conditions, including the knee, shoulder, ankle, wrist, elbow, and hip.
IONA is a less invasive procedure compared to traditional open surgery, reducing patient discomfort and recovery time.
IONA can be performed in an outpatient setting, reducing health-care costs associated with traditional surgical procedures.
IONA has been shown to improve patient outcomes by providing accurate diagnoses and effective treatments.
Limitations of the review
Most of the current evidence on IONA is in the form of case reports, technique articles, and reviews. Hence, the quality of evidence needs to improve. Future studies with a more significant number of patients or even randomized control trials comparing it to arthroscopy in certain conditions will further define and establish the role of IONA.
CONCLUSION
IONA using the Nanoscope is an invaluable, affordable, and accurate diagnostic tool for various joints. In many conditions across joints, it is found to be more accurate than the MRI. However, the benefit is restricted to identifying intra-articular pathologies. Its application has expanded to minor procedures across various joints, thus saving operation theater time for more complex cases. It also reduces saline usage and saves on cost overall.
Author contributions
VTA: Concepts, design, definition of intellectual content, literature search, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis, manuscript preparation, and manuscript editing and review; SBSK: Design, definition of intellectual content, literature search, clinical studies, and manuscript editing and review; RD: Concepts, manuscript editing and review, definition of intellectual content, and design.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Office arthroscopy: A diagnostic alternative. Arthroscopy. 1992;8:320-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic evaluation of the knee in the office setting using small-bore needle arthroscopy. Arthrosc Tech. 2018;7:e17-21.
- [CrossRef] [PubMed] [Google Scholar]
- In-office needle arthroscopy: A systematic review of indications and clinical utility. Arthroscopy. 2019;35:2709-21.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the diagnostic accuracy of MRI in detection of knee cartilage lesions using Receiver Operating Characteristic curves. J Phys Conf Ser. 2021;1736:12028.
- [CrossRef] [Google Scholar]
- A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1525-39.
- [CrossRef] [PubMed] [Google Scholar]
- In-office needle arthroscopic synovial biopsy is an effective diagnostic tool in patients with inflammatory arthritis. Arthrosc Sports Med Rehabil. 2022;4:e2099-106.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: What you see is what you getis in-office needle arthroscopy ready for prime time? Arthroscopy. 2019;35:2722-3.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: In-office needle ankle arthroscopy may be better, simpler, and less expensive. Arthroscopy. 2022;38:1312-4.
- [CrossRef] [PubMed] [Google Scholar]
- In-office needle arthroscopy of the knee with lateral parapatellar retinacular release. Arthrosc Tech. 2023;12:e1809-13.
- [CrossRef] [PubMed] [Google Scholar]
- In-office needle arthroscopy with meniscal repair for meniscal lesions of the knee. Arthrosc Tech. 2023;12:e1821-6.
- [CrossRef] [PubMed] [Google Scholar]
- In-office needle arthroscopy is a cost-effective alternative for operating room diversion in medial meniscectomy: A financial analysis. J Orthop Surg Res. 2023;18:435.
- [CrossRef] [PubMed] [Google Scholar]
- Incisionless partial medial meniscectomy. Arthrosc Tech. 2020;9:e375-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic needle arthroscopy and partial medial meniscectomy using small bore needle arthroscopy. Arthrosc Tech. 2020;9:e645-50.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoscopic medial meniscus repair. Arthrosc Tech. 2021;10:e1943-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cyclops lesions of the knee: A narrative review of the literature. Orthop J Sports Med. 2020;8(8) Doi: 10.1177/2325967120945671
- [CrossRef] [PubMed] [Google Scholar]
- Excision of a knee cyclops lesion using a needle arthroscope. Arthrosc Tech. 2022;11:e563-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nano-arthroscopic ultrasound-guided excision of unresolved osgoodschlatter disease. Arthrosc Tech. 2021;10:e1581-7.
- [CrossRef] [PubMed] [Google Scholar]
- Incisionless synovium and bone biopsy of a painful total knee arthroplasty. Arthrosc Tech. 2021;10:e475-9.
- [CrossRef] [PubMed] [Google Scholar]
- In-office nano-arthroscopy of the shoulder with acromioplasty. Arthrosc Tech. 2023;12:e1423-8.
- [CrossRef] [PubMed] [Google Scholar]
- Single-incision rotator cuff repair with a needle arthroscope. Arthrosc Tech. 2020;9:e419-23.
- [CrossRef] [PubMed] [Google Scholar]
- Rotator cuff repair using a needle arthroscope through a dual-lumen flexible cannula. Arthrosc Tech. 2022;11:e2119-23.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous capsule release in adhesive capsulitis with nanoscope under local anesthesia-Case Report. J Orthop Case Rep. 2023;13:126-9.
- [CrossRef] [PubMed] [Google Scholar]
- Is wrist arthroscopy safer with the nanoscope? J Wrist Surg. 2022;11:450-5.
- [CrossRef] [PubMed] [Google Scholar]
- Volar wrist arthroscopy portals using the nanoscope are safer than traditional arthroscopy. Hand. 2024;18 Doi: 10.1177/15589447231221168
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic-assisted distal radius fracture fixation using the nanoscope system. Arthrosc Tech. 2024;13:103033.
- [CrossRef] [PubMed] [Google Scholar]
- In-office needle arthroscopy for the foot and ankle. Arthroscopy. 2023;39:1129-30.
- [CrossRef] [PubMed] [Google Scholar]
- The role of needle arthroscopy in the assessment and treatment of ankle sprains. Foot Ankle Clin. 2023;28:345-54.
- [CrossRef] [PubMed] [Google Scholar]
- Needle arthroscopy of the elbow through an anterior transbrachial portal. JSES Int. 2023;7:673-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic and therapeutic elbow arthroscopy using small-bore needle arthroscopy. Arthrosc Tech. 2020;9:e1703-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic hip labral repair using needle arthroscopic visualization. Arthrosc Tech. 2024;13:102819.
- [CrossRef] [PubMed] [Google Scholar]







