Translate this page into:
The straight head of rectus femoris: An underdiagnosed cause of chronic pain post hip replacement
*Corresponding author: Rajesh Botchu, Department of Musculoskeletal Radiology, Royal Orthopaedic Hospital, Birmingham, United Kingdom. drrajeshb@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Hussein M, Ariyaratne S, Iyengar KP, Sharma GK, Botchu R. The straight head of rectus femoris: An underdiagnosed cause of chronic pain post hip replacement. J Arthrosc Surg Sports Med. 2024;5:115-8. doi: 10.25259/JASSM_26_2024
Abstract
Groin pain following hip arthroplasty has a spectrum of aetiologies. Although mild post-operative pain at six months to a year is common, other causative factors should be considered where pain is severe or persistent. The rectus femoris (RF) muscle is the most common of the quadriceps tendons to be injured or strained. Pathologies are known to occur in athletic adults and children and include tendinopathy, tear, and avulsion, but the RF is rarely attributed to hip pain post-arthroplasty. However, tendinopathy may occur as a result of altered biomechanics and muscle loading. We performed a retrospective analysis of 100 patients, at our tertiary orthopedic hospital, who presented with chronic pain post hip arthroplasty. We identified three patients with RF straight (direct) head tendinopathy and one patient with RF straight (direct) head calcific tendinopathy. Established causes of chronic post-operative pain include septic/aseptic loosening, pseudotumor, iliopsoas bursitis/impingement, and bursitis. In this report, we describe the scanning technique, sonographic appearances, and our institutional experience of post-arthroplasty pathologies of the RF straight (direct) head which is an underreported cause of chronic pain following hip replacement. We also recommend including the RF straight (direct) head in routine US protocols of the post-operative hip.
Keywords
Groin
Arthroplasty
Replacement
Hip
Pain
Tendinopathy
INTRODUCTION
Groin pain following hip arthroplasty has a spectrum of etiologies. Although mild post-operative pain at six months to a year is common, other causative factors should be considered where pain is severe or persistent. Established causes of chronic pain may be joint centered such as septic/aseptic loosening, pseudotumor or osteolysis, or soft tissue centered which include iliopsoas bursitis/impingement, gluteal muscle tendinopathy, and trochanteric bursitis.[1-4] Pathologies of the rectus femoris (RF) including tendinopathy, tears, and avulsions are known to occur in both children and athletic individuals. To the best of author’s knowledge, no such case reports being attributed to chronic pain post-arthroplasty exist. In this article, we report the scanning technique, sonographic appearances, and our institutional experience of post-arthroplasty pathologies of the RF straight (direct) head which may represent an underreported cause of chronic pain following hip replacement.
ANATOMY AND SCANNING TECHNIQUE OF THE RF
Methods
Local search
Following local institutional approval, we performed a retrospective analysis of 100 patients, at our tertiary orthopedic hospital, who presented to our institution for an ultrasound (US) scan of the hip, with chronic pain post hip arthroplasty. The computerized radiology information system was used to search for patients and picture archiving and communication system to review images.
Scanning technique
The RF is the most superficial of the quadriceps femoris muscle group located in the anterior thigh. It functions to flex the hip joint and extend the knee joint. The proximal RF consists of two tendinous origins; the straight (direct) head originating from the anterior inferior iliac spine (AIIS) and reflected (indirect) head originating from a broader attachment at the anterolateral acetabular ridge and hip joint capsule. The two heads form a conjoined tendon a few centimeters below the origin. As described by Hasselman et al., the tendons do retain a significant anatomic independence; distally the straight (direct) head blends with the anterior muscular fascia and the reflected (indirect) head continues as the central tendon (aponeurosis).[5] The distal tendon is formed from a broad posterior aponeurosis and becomes the superficial portion of the quadriceps tendon.
A standard protocol in scanning the post-operative hip was utilized. This included scanning the anterior joint recess, surrounding tendons and the femoral neurovascular bundle.[6] A linear 15–6 MHz probe was suitable in the majority of patients. In those with periprosthetic collections or in obese patients, a lower frequency 5–1 MHz probe was more suitable.
The RF is located in the anterior compartment. First, the transducer was placed craniocaudally in the sagittal plane over the AIIS. On this long-axis view, the normal straight (direct) head of the RF tendon returned a homogenous fibrillar echogenic pattern [Figure 1]. Approximately 2–3 cm proximal to its origin, the reflected (indirect) head was identified as an area of posterior acoustic shadowing, due to an abrupt change in orientation of tendon fibers as it passes from the superolateral acetabular groove, to join the straight head, form the conjoint tendon [Figure 1]. Consequently, sonographic assessment of the reflected head is limited.
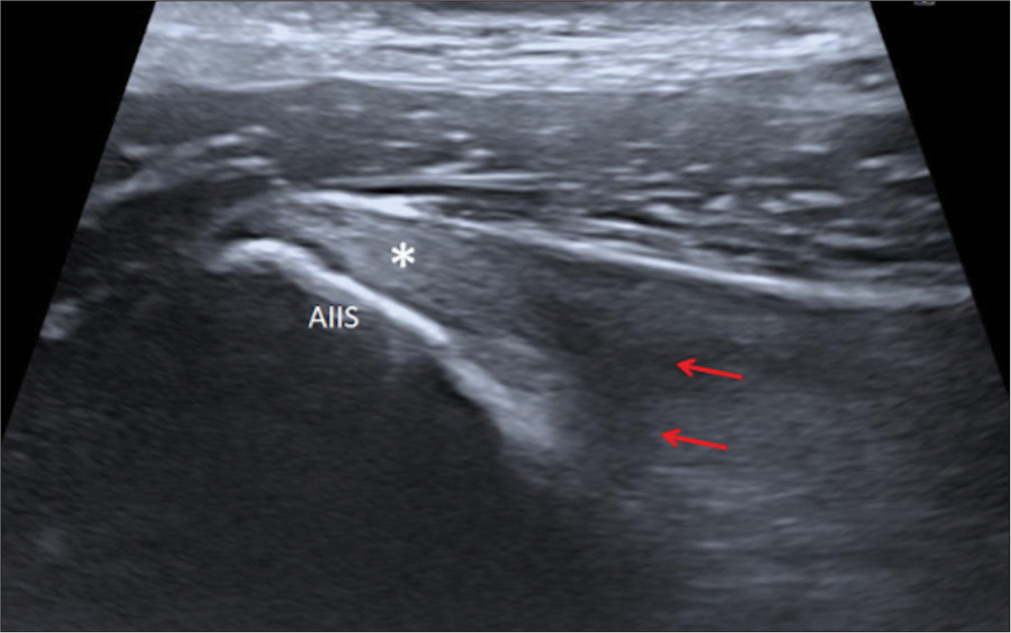
- Normal longitudinal (sagittal) ultrasound image of the rectus femoris (RF) muscle. Longitudinal fibrillar pattern of the normal straight (direct) head (asterisk) origin at the anterior inferior iliac spine (AIIS). RF reflected (indirect) head (red arrows) is visualized as an area of acoustic shadowing due to changing caliber of fibers which attach to the superior acetabular ridge.
The RF straight head was identified in a similar fashion on the transverse plane at the level of the AIIS. The reflected head is visualized as an area of acoustic shadowing laterally [Figure 2a and b]. Moving inferiorly, the myotendinous junction appears at the lateral aspect of the tendon with the Sartorius (superiorly), iliopsoas (medially), and tensor fascia lata (laterally) within the field of view. Further inferiorly, the reflected head continues predominantly as the central tendon (aponeurosis), identified at the anteromedial aspect of the muscle; the straight head blends with the anterior fascia and is not distinctly visualized [Figure 2c and d].
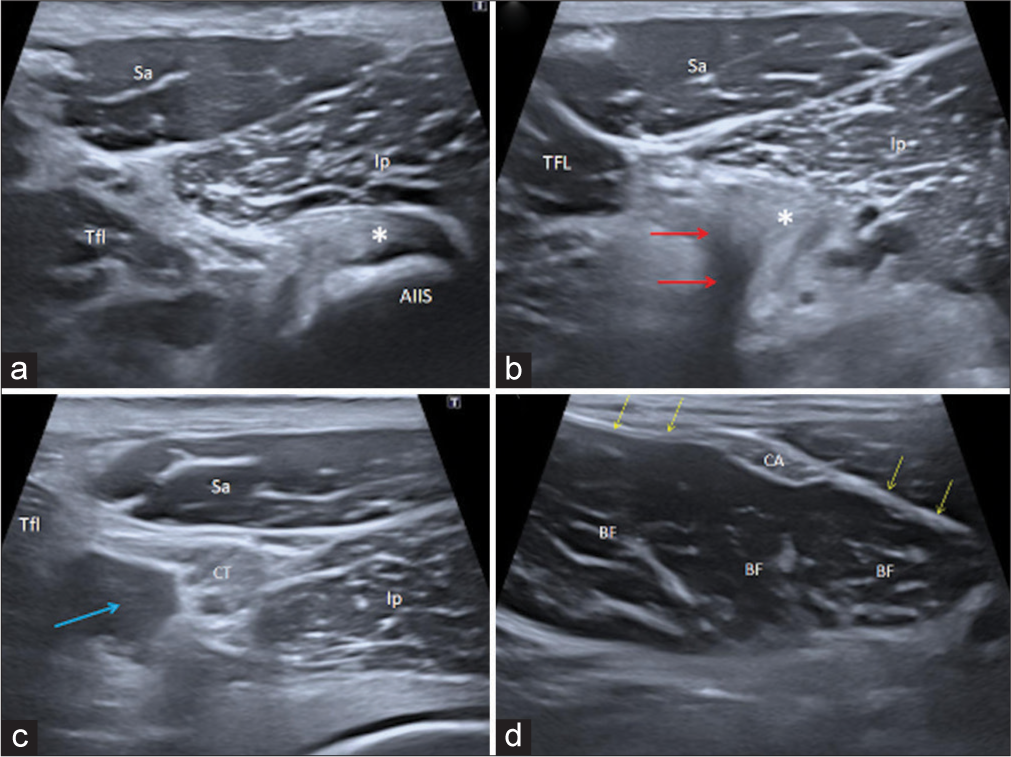
- Sequential cranial to caudal transverse ultrasound images (left column) with corroborative axial MRI images (right column) of a normal right RF muscle and surrounding structures. (a) RF straight (direct) head origin (asterisk) at the AIIS. (b) RF reflected (indirect) head (red arrows) is visualized as an area of acoustic shadowing due to changing caliber of fibers which attach to the superior acetabular ridge; the corroborative MRI depicts this clearly. The straight (direct) head (asterisk) is seen adjacent to this. (c) Conjoint tendon of the RF at the myotendinous junction with the muscle belly forming at the lateral margin (blue arrow). (d) RF muscle belly. CA formed by the reflected (indirect) head and an indistinct anterior aponeurosis (yellow arrows) formed by the straight (direct) head. RF: Rectus femoris muscle belly, asterisk: RF straight (direct) head, red arrows: RF reflected (indirect) head, CT: Conjoint tendon, CA: Central aponeurosis, Sa: Sartorius, Tfl: Tensor fascia lata, Ip: Iliopsoas, Gl: Gluteal muscles, Cap: Anterior hip capsule, Fe: Femoral head, AIIS: Anterior inferior iliac spine, MRI: Magnetic resonance imaging.
RESULTS
Four patients demonstrated heterogeneity within the RF straight (direct) head origin [Figure 3] and one out of these patients demonstrated calcification within the RF straight (direct) head origin [Figure 4]. The remaining 96 demonstrated iliopsoas tendinopathy, gluteal muscle tendinopathy, impingement at the acetabular cup, or trochanteric/subgluteal bursitis. Of the four patients with RF findings, all had tenderness on probe pressure over the focus of heterogeneity/calcification at the origin of the RF straight head with no other attributable cause of groin pain identified. Consequently, these four patients were diagnosed with RF tendinopathy. Three patients were managed conservatively with non-steroidal anti-inflammatory drugs (NSAIDs) and physiotherapy with resolution of pain over the next few months. One patient had an US-guided injection of local anesthetic and steroid in conjunction with physiotherapy with significant improvement in symptoms.
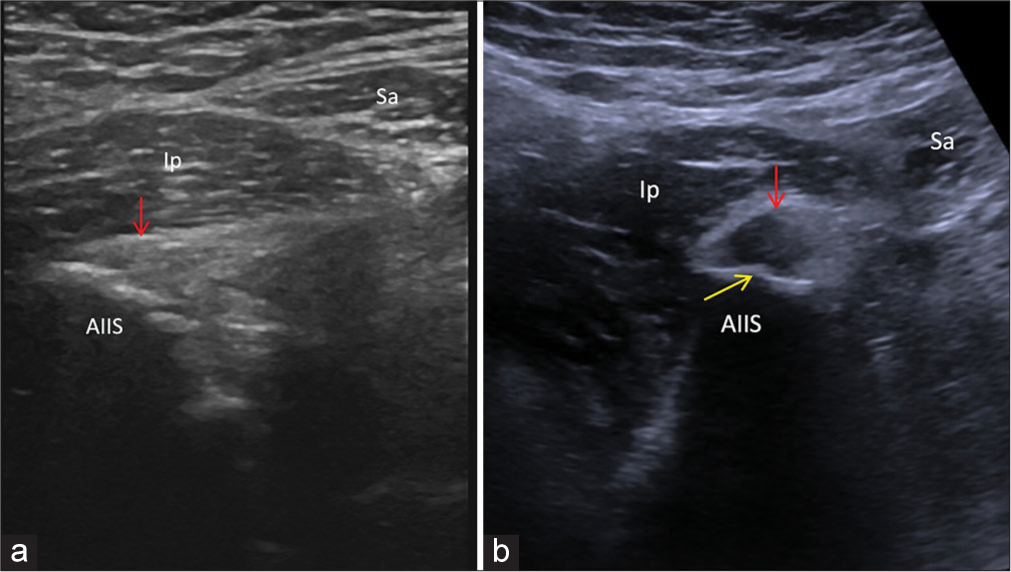
- RF straight (direct) head tendinopathy. (a) Short axis ultrasound image demonstrates mild heterogeneous echotexture (red arrow) of the RF origin with irregularity (yellow arrows) of the AIIS enthesis. (b) Short axis ultrasound image in a different patient showing more marked tendinopathy (red arrow) with a prominent enthesophyte at the AIIS (yellow arrow). RF: Rectus femoris, AIIS: Anterior inferior iliac spine, Ip: Iliopsoas, Sa: Sartorius.
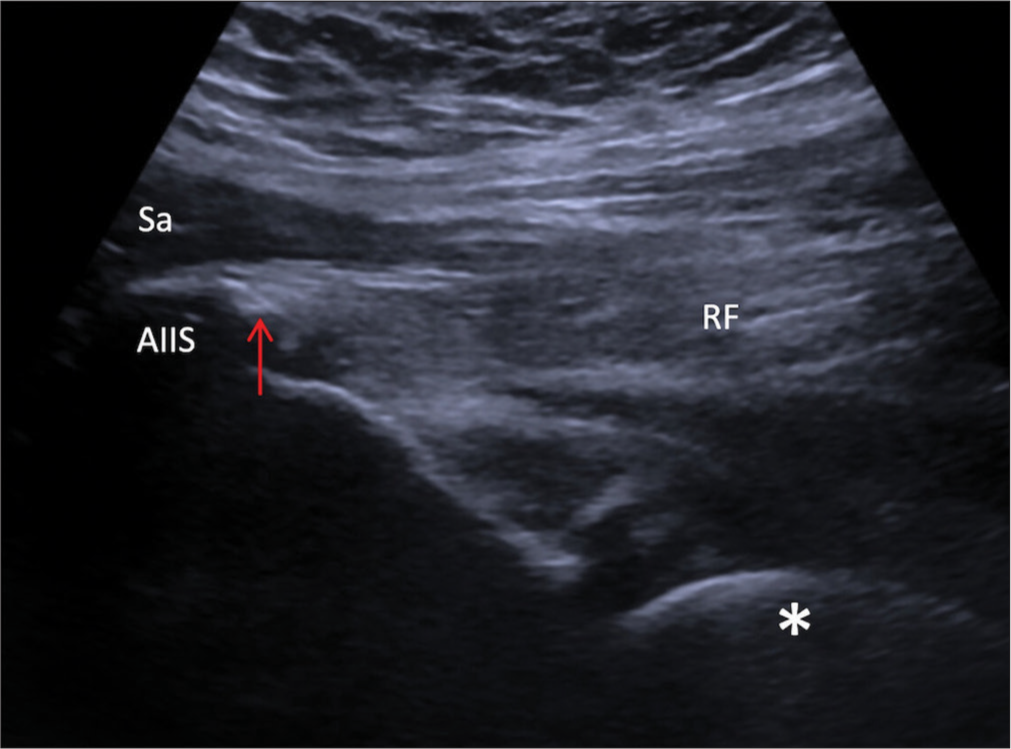
- RF straight (direct) calcific tendinopathy. Long axis ultrasound image demonstrates a prominent calcification (red arrow) and heterogenous echotexture of the RF straight head origin. AIIS: Anterior inferior iliac spine, RF: Rectus femoris, Sa: Sartorius, Asterisk: Femoral head arthroplasty.
DISCUSSION
Hip arthroplasty is the second most common joint-replacement operation performed within the United Kingdom. It is one of the most cost-effective orthopedic surgeries and carries relatively low major complication rates.[7] Although routine radiographs may reveal causes of chronic pain secondary to aseptic loosening, pseudotumor, osteolysis, and heterotopic ossifications, US is a superior study to evaluate soft tissues. It provides excellent soft-tissue resolution to assess echotexture of tendon entheses and joint recesses. Images are not limited by arthroplasty-related streak and susceptibility artifacts which may be observed in computed tomography and magnetic resonance imaging, respectively. US is limited in assessing deep structures, such as the reflected head of the RF, high-density material (such as calcification), and patients with a large body habitus. The operator must take care to differentiate the iliopsoas tendon from the RF as both are imaged in close proximity on the sagittal plane.
The RF is the most common of the quadriceps muscles to be strained/injured due to its elongated shape, extension across two joints and high proportion of type II muscle fibers.[8] In adults, pathologies are most commonly calcific tendinopathy and traumatic tears, whereas in children, avulsion injuries of the straight (direct) head at the AIIS predominate.[9-11] RF tendinopathy is a well-known cause of pain in football players and is thought to occur from repetitive hip flexion performed during sprinting and kicking. Patients present with sharp pain or stiffness localized to the anterior aspect of the hip or groin which is exacerbated during hip flexion and knee extension against resistance. Outside of overuse injuries, it is also observed in spondylarthritis or hydroxyapatite deposition.[12] It is possible that the tendinopathy found in our cohort may be the result of altered biomechanics and muscle loading, which may occur following hip arthroplasty, which imposes strain beyond physiological limits across the straight head. An anterior (Smith-Peterson) surgical approach is reported to have a higher incidence of RF injury; although its propensity to cause chronic pain is not documented, this may also be a contributing factor.[13] Other documented risk factors of RF injury such as decreased flexibility, high body weight, and eccentric muscle strength,[14] may occur in the context of hip arthroplasty, and precipitate tendinopathy or partial tears. Finally, given the close proximity of the RF to the acetabular cup, repetitive friction or prosthetic loosening, similar to that seen in iliopsoas tendinosis/bursitis, may be contributory.[15,16] Further prospective and retrospective studies are required to better understand the underlying pathophysiology. Given that RF tendinopathy is less common when compared to other hip pathologies, the differential diagnosis of pain postoperatively include septic/aseptic loosening, post-operative pseudotumor and iliopsoas bursitis/impingement which may all present with groin pain and can be exacerbated by hip flexion, greater trochanteric pain syndrome should also be considered but presents with pain over the greater trochanter.
Current treatment for RF tendinopathy includes a combination non-invasive and minimally invasive options. Symptoms may initially be managed conservatively with oral NSAID medications, physiotherapy, and US-guided steroid injection.[17] In cases with tendon calcification, surgical excision,[18] extracorporeal shock wave therapy,[19] or percutaneous irrigation of tendon calcification[20] are reported with generally positive outcomes. For patients in which conservative measures do not resolve symptoms, the next step for treatment will be guided by local institutional experience and preference.
CONCLUSION
US provides a comprehensive means of assessing patients with chronic pain following hip arthroplasty. It may accurately identify abnormalities of the straight head of the RF which is an underreported cause of chronic pain and should be included in routine US protocols.
Ethical approval
The Institutional Review Board approval is not required since it was a retrospective study.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The role of ultrasound in the assessment of post-operative complications following hip arthroplasty. Skeletal Radiol. 2012;41:1035-46.
- [CrossRef] [PubMed] [Google Scholar]
- Hip arthroplasty. Part 2: Normal and abnormal radiographic findings. Clin Radiol. 2009;64:961-71.
- [CrossRef] [PubMed] [Google Scholar]
- Current literature and imaging techniques of aseptic lymphocyte-dominated vasculitis-associated lesions (ALVAL) Clin Radiol. 2013;68:1089-96.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br. 2009;91:1566-74.
- [CrossRef] [PubMed] [Google Scholar]
- An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23:493-9.
- [CrossRef] [PubMed] [Google Scholar]
- Musculoskeletal ultrasound: Technical guidelines. Insights Imaging. 2010;1:99-141.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment on patient outcomes of primary hip replacement: An interrupted time series analysis from 'The National Joint Registry of England and Wales' BMJ Open. 2019;9:e031599.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of the proximal rectus femoris musculotendinous unit. Magn Reson Imaging Clin N Am. 2005;13:717-25.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated, full-thickness proximal rectus femoris injury in competitive athletes: A systematic review of injury characteristics and return to play. Orthop J Sports Med. 2023;11:23259671221144984. Doi: 10.1177/23259671221144984
- [CrossRef] [PubMed] [Google Scholar]
- Management of proximal rectus femoris injuries-do we know what we're doing?: A systematic review. Biol Sport. 2023;40:497-512.
- [CrossRef] [PubMed] [Google Scholar]
- Management of acute calcific tendinitis around the hip joint. Am J Sports Med. 2014;42:2659-65.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of rectus femoris proximal tendinopathies. Skeletal Radiol. 2016;45:889-97.
- [CrossRef] [PubMed] [Google Scholar]
- Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453:293-8.
- [CrossRef] [PubMed] [Google Scholar]
- Rectus femoris muscle injuries in football: A clinically relevant review of mechanisms of injury, risk factors and preventive strategies. Br J Sports Med. 2013;47:359-66.
- [CrossRef] [PubMed] [Google Scholar]
- Iliopsoas bursitis following total hip replacement. Arch Orthop Trauma Surg. 2004;124:720-3.
- [CrossRef] [PubMed] [Google Scholar]
- Results after arthroscopic treatment of iliopsoas impingement after total hip arthroplasty. Arch Orthop Trauma Surg. 2022;142:189-95.
- [CrossRef] [Google Scholar]
- Acute calcific tendinitis of the rectus femoris. J Bone Joint Surg Br. 1996;78:814-6.
- [CrossRef] [PubMed] [Google Scholar]
- Calcific tendinitis of the rectus femoris. Orthopedics. 2009;32:490.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal shock wave therapy for calcific tendinitis at unusual sites around the hip. Orthopedics. 2010;33:769.
- [CrossRef] [PubMed] [Google Scholar]
- Calcific tendinopathy of the direct head of rectus femoris: A rare cause of groin pain treated with ultrasound guided percutaneous irrigation. J Ultrasound. 2020;23:425-30.
- [CrossRef] [PubMed] [Google Scholar]







