Translate this page into:
Recent advances and future trends in patellofemoral instability

*Corresponding author: Bobby Singh Anand, Department of Orthopaedics, South West London Elective Orthopaedic Centre, Surrey, United Kingdom. bobbyanand@me.com
-
Received: ,
Accepted: ,
How to cite this article: Anand BS, Ho S, Kambhampati S. Recent advances and future trends in patellofemoral instability. J Arthrosc Surg Sport Med 2020;1(1):110-7.
Abstract
Patellofemoral joint instability (PFJI) is a challenging condition affecting primarily young patients. It can be both physically and mentally disabling. There are numerous factors which contribute to stability of the patellofemoral joint and thorough clinical assessment and appropriate radiological investigations are essential in determining which risk factors need to be corrected to prevent further episodes of dislocation. One of the key operations utilized in the management of PFJI is medial patellofemoral ligament (MPFL) reconstruction, to restore the patellar restraint against lateral translation. The complications that can result from MPFL reconstruction can be largely divided into complications resulting from technical error or selection of operation for a patient’s specific risk factors. Some risk factors of PFJI can precipitate the need for additional operations being performed alongside MPFL reconstruction, including trochleoplasty, lateral retinacular lengthening, and tibial tuberosity osteotomy. Failure to identify the need for concurrent operations will result in persistent PFJI. This update article will outline the approach to assess a patient presenting with PFJI and the risk factors which should be identified and corrected. It will also cover the various management options with respect to these factors, with some important considerations for each.
Keywords
Patella instability
Medial patellofemoral ligament
Trochleoplasty
Patella
Osteotomy
INTRODUCTION
Patellofemoral joint instability (PFJI) is a broad term that describes a range of conditions, from mild patella maltracking to chronic recurrent patella dislocations. Acute patella dislocation makes up 2–3% of all acute knee injuries.[1] The risk of a redislocation following a 1st time dislocation ranges from 17 to 71%.[2,3] There is growing interest in risk stratification for this condition and a number of assessments have been proposed to try to quantify and understand the risk of a redislocation in a particular individual.[4]
The clinical consequences from patella dislocations are well described and include osteochondral lesions of either the patella or lateral femoral condyle,[5] disruption of the medial patellofemoral ligament (MPFL),[6] or progression to osteoarthritis in chronic disease or recurrent dislocations.[7] The psychological impact on patients from this condition has been observed by surgeons, but health-related quality of life measures for the patellar instability population are limited. This is particularly so for the young adolescent population.[8]
Considering the young demographics of these injuries, determining the most effective management for these patients is essential to both return them to previous levels of physical activity, managing their mental state and preventing further episodes of instability. Management of PFJI has significantly evolved over the past 10 years. Improved understanding of the biomechanics, anatomy, and clinical data has helped develop a more structured management approach for this challenging condition. This article aims to examine the recent advances that have been made into assessing and managing PFJI as well as the future trends that can be considering when approaching PFJI patients.
STABILITY
The stability of the patellofemoral joint is determined by numerous factors. These can be divided into either local static or dynamic factors and distant static or dynamic factors. These elements have been extensively described in the literature.[9-11] Table 1 summarizes the key contributors to PFJI.
| Soft tissue factors | Bony factors |
|---|---|
| MPFL injury | Trochlear dysplasia |
| VMO atrophy/weakness | Patella alta |
| Tight lateral structures | Rotational abnormalities of lower limb: Femoral version, external tibial torsion |
| Medial retinaculum laxity | Axial malalignment of lower limb |
| General ligament laxity | Patellar hypoplasia |
| ITB complex | |
| Abductors and external rotators of the hip | |
| Rotation/hyperpronation of the foot | |
Independently, the major factors that guide decision-making are trochlear dysplasia, patellar tilt of 20° or more, excessive tibial tuberosity-trochlea groove (TT:TG) displacement of 20 mm or greater, and the presence of patella alta.[10,12]
Apart from MPFL and medial quadriceps tendon femoral ligament (MQTFL), other ligaments have been identified around the PFJ, but their role in the stability of the patellofemoral joint has not been established. These include medial patellotibial ligament (MPTL), medial patellomeniscal ligament (MPML), and medial patellofemoral complex. These have been classified as a proximal group (MQTFL and MPFL) and a distal group (MPTL and MPML) of ligaments.[13] The distal group is believed to provide stability of PFJ at 90° of flexion.
ASSESSMENT
Clinical and radiological assessment of the patient is paramount to plan correctly before considering surgical intervention. This has been well described[9,14] and is summarized in Table 2.
| Key aspects of history | Clinical assessment | Imaging |
|---|---|---|
| Age at first dislocation Family history History of trauma Position of limb involved during dislocation Frequency of dislocation Disability and expectations Direction of instability Previous surgery Impact on life/sport Pain issues |
Limb alignment Medial retinacular laxity Lateral structure tightness Parapatellar tenderness – Bassett’s sign Patellar height and position (squinting patellae, grasshopper sign) Patellar tracking – J sign/reverse J sign Patellar translation (>2 quadrants) Apprehension test (Fairbank test) Q angle Lower limb rotational assessment Laxity assessment (Beighton score) Core strength Rule out other knee trauma |
Plain radiogra MRI CT with rotationaprofile assessme |
Radiological assessment forms an important part of clinical decision-making. Plain radiographs are useful. The true lateral view is used to assess patella alta and dysplasia. Our preferred method is to use the Caton-Deschamps index for patella height. Trochlear dysplasia can be classified with the lateral view using Dejour classification [Table 3]. Axial views are used to assess patellar tilt, depth sulcus angle, congruence angle subluxation, and trochlear dysplasia.
| Dejour classification | |
|---|---|
| Type A | Crossover sign, fairly shallow trochlea (sulcus angle >140°) |
| Type B | Crossover sign, flat trochlea and supratrochlear spur |
| Type C | Crossover sign with double contour, medial hypoplasia |
| Type D | Type C features + vertical link between facets (“cliff pattern”) |
MRI is important as it helps to detect associated chondral, osteochondral, and MPFL injuries. It is recommended for the 1st time dislocations to rule out injuries potentially needing surgery. There is also growing understanding of newer measurements that can be made on cross-sectional imaging.
The use of sagittal trochlea length seems to be growing in importance and studies are starting to show that such measures correlate with clinical outcomes.[14]
Rotational profile CTs by the method of Dejour et al.[12] allow for the assessment of a number of different anatomical factors which can contribute to PFJI. This includes an assessment of rotational profile including femoral anteversion and tibial torsion, patellar and trochlear tilt and depth,[12] and TT:TG distance can be made. Where the trochlea is severely dysplastic and cannot be used for reliably measuring TT:TG, TT to posterior cruciate ligament (PCL) origin may be used.[15] CT is also very useful when planning trochleoplasty surgery. A normal TT:TG distance is 2–9 mm. A TT:TG distance greater than 20 mm is pathological but is typically seen in combination with trochlea dysplasia. This patient group is far more prone to PFJI.
The patellar instability score is a useful tool as it uses key parameters to guide surgical intervention. The factors measured are age, positive anamnesis of contralateral patella dislocation, patella tilt (less than or more than 20°), patella alta, TT:TG distance, and trochlear dysplasia. Patients with a score of more than 4 are recommended surgery due to higher risk of redislocation.[16]
CONSERVATIVE MANAGEMENT OPTIONS
Non-operative management through functional rehabilitation can be considered in patients with acute 1st time patellar dislocations without loose bodies or osteochondral fractures. Conservative treatment of acute dislocations is a brief period of immobilization followed by early mobilization. POP cast application and extended immobilization up to 6 weeks lead to stiffness of the knee. Physiotherapy plays a significant role in focusing on gait, core stability, and strengthening of the quadriceps to try to conservatively correct some of the anatomical factors contributing to PFJI.[17]
Multiple randomized control trials have looked at outcomes of non-operative versus operative management, with the key finding that rates of redislocation following operative intervention were significantly lower than conservative management, with two-thirds of conservatively managed patients continuing to have instability symptoms, anterior knee pain, and, in turn, worse satisfaction.[18]
MPFL
The MPFL together with the superficial medial collateral ligament forms one of the layers of the medial retinaculum of the knee, along with the investing layer, and the deep medial collateral ligament and joint capsule. It acts as the primary passive stabilizer of the patella in flexion of 20–30° and helps track the patella into the trochlear groove. It also acts to provide between 50 and 80% of stability in resisting lateral displacement of the patella.
The MPFL has attachments to both the distal femur and the patella. The MPFL inserts into the upper two-thirds of the patella after conjoining with the deep portion of the VMO, the femoral attachment has been attributed to a number of different sites through cadaveric studies.
These include a radiographical point 1 mm anterior to the posterior cortex extension line, 2.5 mm distal to the posterior origin of the medial femoral condyle (Schottle’s point), a confluence point posterior to the posterior cortex extension line but anterior to the confluence of the posterior femoral cortex and Blumensaat’s line on a true lateral radiographic view of the knee,[18] and the origin of the medial femoral epicondyle.[19]
Surgical management of PFJI is evolving. In the absence of good quality studies to aid in the decision making for the treatment of PFJI, an international consensus statement adds some value to guide decision making in PFJI.[20]
Given the importance of the MPFL in the stability of the patellofemoral joint and its disruption in 90–100% of lateral patellar dislocations, the MPFL reconstruction has become the primary operation performed in PFJI patients. The techniques used to perform an MPFL reconstruction can vary significantly.[21]
MPFL RECONSTRUCTIONS, FAILURE, AND COMPLICATIONS
MPFL reconstructions have been shown to achieve satisfactory clinical outcomes through reducing patella dislocation events, improving function, and returning to pre-injury levels of activity.[22-24] However, complications from surgery can be high. Systematic reviews have reported complication rates up to 26.1%.[25-27] Recurrent patella instability is reported to occur in 13.8% of patients post-MPFL reconstruction.[27] Other complications include loss of range of movement, patellar fractures, and patellofemoral joint arthrosis.
These complications can be largely split into two groups; complications resulting from not tailoring the operation to the patient’s individual risk factors and complications resulting from technical error.
Patient-specific surgery in PFJI is an important area with growing evidence. Studies have highlighted that failures of MPFL reconstruction can be high in the presence of significant trochlear dysplasia and high TT:TG distances. Failure to address these bony factors can lead to poor outcomes and complications.[28,29] It is, therefore, crucial to address significant bony abnormalities. In our practice (Anand), 18% of PFJ stabilization procedures involve a bony procedure, usually a trochleoplasty. The key bony factors to consider are lower limb alignment (increased valgus), patella alta, trochlear dysplasia, or rotational problems.[18]
An isolated MPFL reconstruction is appropriate for patients who report recurrent patellar dislocations as well as having excessive lateral patellar translation on examination, with normal or low-grade/type A Dejour trochlear dysplasia, minimal patella alta (Caton-Deschamps index <1.4), and the absence of a J sign. They should also have no lateral patellofemoral load seen on imaging and a tuberosity sulcus angle between 0 and 5° of valgus.
TECHNICAL COMPLICATIONS OF MPFL RECONSTRUCTIONS
There are three main technical complications that can arise from MPFL reconstruction surgery. These are improper femoral tunnel placement, overtensioning of the graft, and patellar fractures.
The correct placement of the femoral tunnel continues to lack a firm consensus, particularly given there have been different sites for the MPFLs femoral insertion identified as noted above, and changes in this attachment can significantly increase medial contact pressures as well as medial patellar tilt, given that it is responsible for length change and tension of the graft during flexion and extension of the knee.[9]
Intraoperatively, this femoral attachment point for the MPFL should be identified on a true lateral view using fluoroscopy. This helps to prevent the graft being fixed either too proximal and anterior or too distal and posterior. Both can result in recurrent PFJI. The former can also cause increased tightness in flexion, leading to medial patellofemoral articular overload, causing pain and loss of flexion. Conversely, the latter can cause tightness in extension, extensor lag, and pain on knee extension.[30,31]
Another consideration when fixing the MPFL graft is the tension it is placed under in both flexion and extension. It should be noted that the MPFL should be acting to prevent lateral patellar translation rather than pulling the patella into the trochlea groove. As such, the aim should not be to “tension” the graft. Placing the graft under excess tension in flexion can cause pain and loss of flexion, while excess tension in extension can cause pain and extensor lag. The former can also cause increased forces through the medial patellar facet.
Fixing the graft with the knee flexed at 40–60° at the furthest point between attachment sites can reduce the risk of it being overtensioned, with intraoperative assessment for two to three patellar quadrants with a hard stop. Comparing the tension to the contralateral MPFL also helps guide the tension, the graft should be fixed at.[9,25,32]
In cases where an MPFL reconstruction graft has been overtensioned, complex pain problems can be created as the medial patella facet is overloaded. Usually, a release of the MPFL ligament can be performed arthroscopically to reverse this problem. Thaunat and Erasmus described two case reports where overtensioning, one in flexion and the other in extension, was identified and corrected by sequential partial tenotomies, with regular comparison to the contralateral patella, relieving symptoms of pain, and reduced range of movement.[33]
The third main technical-related complication of MPFL reconstruction is fractures through the patella which can lead to failure. Three main fracture types have been classified: The Type I transverse fractures through the patellar tunnel or drill hole, Type II superior pole, or sleeve avulsion fractures associated with excessive superior patellar dissection, proximal realignment or lateral release, and last, Type III medial rim avulsion fractures through patellar drill holes, associated with persisting PFJI post-stabilization procedures.
Techniques and principles have been described to reduce fracture risk. This includes avoiding transverse tunnels through the whole patella and reducing diameter of tunnels, ensuring an adequate bone bridge, and minimizing devascularization of the patellar superior pole during dissection. If using a gracilis tendon autograft, suturing to soft tissue without a bone tunnel can reduce fracture risk, as can securing grafts by suture anchors rather than an endobutton or screw.[34]
MPFL GRAFT CHOICE
Most published data on MPFL reconstruction outcomes are based on the use of autografts. There is growing interest in the use of alternate grafts to reduce donor site morbidity. The use of allografts for MPFL reconstruction is well established and no significant difference in redislocation rates has been found between autograft (5.7%) and allograft (6.7%). In the same systematic review, autograft reconstructions were, however, associated with greater post-operative improvements in Kujala scores when compared to allograft (32.2 vs. 22.5, P < 0.001).[35]
Synthetic grafts also seem to perform equally well, but this should be interpreted with caution as numbers are low. Patients treated with adductor tendon autograft seem to have high redislocation failure rates ranging from 5.6% to 8.3%.[35,36]
LATERAL RELEASES/LATERAL RETINACULAR LENGTHENING
Although previously isolated lateral releases have been a popular operation for patellofemoral pain, excessive lateral pressure syndrome, and PFJI around the 1970–1980s, this is now no longer recommended for PFJI. The International Patellofemoral Study Group performed a survey in 2004, which found that isolated lateral releases are now rarely performed.[36]
This relates to inconsistent outcomes postoperatively, with unsatisfactory improvements in pain, worsening instability, and complications including potentially disabling iatrogenic medial patellar instability (IMPI).[36-38] Lateral retinacular lengthening has no established role in native patella instability but is being used for IMPI. Sanchis-Alfonso et al. assessed outcomes of patients who had been experiencing disabling IMPI following lateral retinacular reconstruction using a central strip of iliotibial band, demonstrating significant improvement in Lysholm knee scores and VAS scores, as well as resolution of pre-operative anxiety and kinesiophobia.[38]
TROCHLEOPLASTY
Reshaping the trochlea groove is an attractive but technically challenging option for correcting the major bony problem in patella instability. The indications for trochleoplasty surgery include advanced Dejour C/D dysplasia with positive J sign [Figure 1].
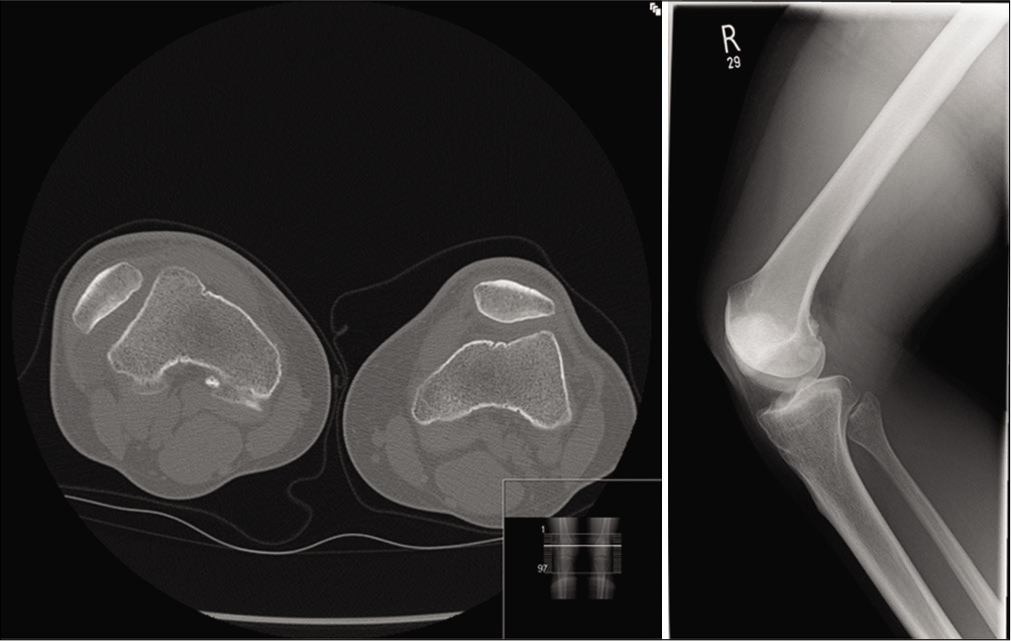
- Case of advanced Dejour D dysplasia and chronically dislocated patella. The patient had a thin flap trochleoplasty and medial patellofemoral ligament reconstruction performed.
Trochleoplasty can be performed as a stand-alone procedure or as a combined operation. In general, the consensus is toward a combined procedure approach. In a recent systematic review, Ren et al. showed improved functional outcome scores and a lower return to theater for combined MPFL and trochleoplasty v isolated trochleoplasty.[39]
Trochleoplasty can be performed utilizing a thin flap (Bereiter type) or thick flap (Dejour) techniques [Figure 2]. Both techniques have been shown to have good outcomes.[40-42] Trochleoplasty can be used for both primary operative management of PFJI and also for revision surgery in failed previous PFJI surgery.[43]

- A lateral parapatellar approach with thin flap elevation in advanced trochlea dysplasia and creation of groove with taping technique to hold osteotomy.
A systematic review in 2017 by Longo et al. reported the thin flap Bereiter trochleoplasty seems to be the most efficient procedure in terms of post-operative patella redislocation, post-operative osteoarthritis, and ROM, but the highest mean post-operative Kujala score was seen in the patients who had a thick flap by Dejour procedure. No clear surgical superiority was found between the two techniques. Interestingly, a relatively low rate of osteoarthritis and pain was found with both techniques.[44] Randomized clinical trials are needed to compare these techniques, but this is challenging due to the low number of cases.
Arthroscopic trochleoplasty surgery has been promoted as an elegant solution. The evidence base around this remains limited, but some promising early data have been published.[45,46] Arthroscopic trochleoplasty may potentially offer a solution to the challenge of knee stiffness that is sometimes found after open trochleoplasty surgery.[47,48]
When assessing PFJI patients with marked trochlear dysplasia, a tibial tuberosity-PCL (TT:PCL) distance can be more useful instead of a TT:TG distance in determining the location of the tibial tuberosity independent of the trochlear shape, given that high TT:TG could result from either tibial tuberosity lateralization or trochlear groove medialization without discrimination.[49]
TIBIAL TUBERCLE OSTEOTOMY (TTO)
Different procedures for transfer of the tibial tubercle have been described in the literature ranging from anteriorization (Maquet technique), medialization (Elmslie-Trillat), distalization, and anteromedialization (AMZ).[50] Of these techniques, AMZ has given consistent results in the presence of patellar instability overtime. The primary indications for AMZ include a TT:TG distance >20 mm, an increased TT:PCL distance, and patella alta with a Caton-Deschamps index >1.2. The aim of a TTO should be to aim to restore a post-operative distance of 10–15 mm, though with care to avoid overmedialization.[9] If TT-TG distance is <15 mm, MPFL reconstruction can restore normal patellofemoral kinematics and contact mechanics.[18] An important prerequisite for the procedure is intact proximal patellar articular surface. It is not recommended if the proximal patella is degenerative.[51] An excessive TT-TG distance influences the valgus alignment of the extensor mechanism directly and so acts as a valgus displacing force on the patella. This can cause an excessively lateralized position, potentially stretching the MPFL and worsening risk of recurrent PFJI.[52]
The success rates for the AMZ have been reported to range from 86 to 97%, but the indications for surgery are not isolated to PFJI.[53-57] TTO is often used only for distalization of the patella (X53) to address instability without altering TT:TG. It is also important to note that trochleoplasty can also allow for proximal realignment and correct for 10 mm of distalization and 4 mm of medialization[9] so offers a more anatomical approach to correcting such abnormalities.
The overall risk of a major complication is reported to be in the region of 3%. Such complications include non-union, stress fractures, vascular injury, and compartment syndrome. Furthermore, removal of metal work is an issue and has been reported to be needed in 49% of AMZ cases.[58]
OUTCOMES AND CONCLUSION
PFJI is a challenging condition that can have a significant physical and mental impact on a young population. To determine the correct management for these patients, detailed assessment with attention to detail is vital. Key aspects of the history, examination, and figure findings form the basis of care. We recommend the algorithm proposed in Table 4 as a simplified approach to a complex problem. The value of the true lateral views of the knee on plain radiographs should not be underestimated. The key factors that contribute to patella instability are trochlear dysplasia, patella height, patellar tilt of 20° or more, and excessive TT:TG displacement. Other factors should be considered as understanding and treatment options evolve.
| Patella instability problem | Surgical option |
|---|---|
| No major bone issues (mild dysplasia, mild/moderate alta) | Isolated MPFL |
| Significant dysplasia (B-D) | Trochleoplasty + MPFL |
| Significant patella alta | TTO – distalization only +/-MPFL |
| Increased valgus (trauma/iatrogenic) | Distal femur osteotomy |
| Isolated increased TT:TG | TTO medialization/AMZ |
| Rotational deformity | Derotational osteotomy proximal femur |
MPFL reconstruction plays a key role in many PFJI patients in restoring stability, with multiple randomized control trials showing good outcomes, and as such is one of the most common procedures for PFJI. However, it is not the solution for all patients. Complications can be high both due to patient selection and technical errors. Correct tunnel placement and avoiding graft overtensioning are important.
It is equally important that significant bony anatomical abnormalities should be corrected with surgery in combination with reconstruction of the MPFL. Isolated MPFL reconstructions play a role in patients who have normal or low-grade/Type A Dejour trochlear dysplasia and no excessive patella alta. In the presence of high-grade trochlear dysplasia, a trochleoplasty procedure should be considered. Either a thin flap or thick flap technique is acceptable and this should be combined with an MPFL reconstruction. In the presence of gross patella alta, a tibial tuberosity osteotomy should be considered. More complex anatomical abnormalities are rare but often require additional osteotomies.
Future developments will focus on understanding longer term outcomes and refining trochleoplasty surgery, most likely with the use of robotics. The use of synthetic or biologically engineered grafts offers the potential to reduce morbidity and complications for MPFL surgery. Randomized prospective studies are limited and these will guide further improvements to care.
Declaration of patient consent
Patients consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Srinivas Kambhampati is on the Editorial Board of the Journal.
References
- Acute patellar dislocations: A natural history. Am J Sports Med. 1986;14:117-20.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28:472-9.
- [CrossRef] [PubMed] [Google Scholar]
- An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc Rev. 2007;15:78-81.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting risk of recurrent patellar dislocation. Curr Rev Musculoskelet Med. 2018;11:212-60.
- [CrossRef] [PubMed] [Google Scholar]
- Acute dislocation of the patella. Am J Sports Med. 1996;24:52-60.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: A systematic review. Am J Sports Med. 2010;38:181-8.
- [CrossRef] [PubMed] [Google Scholar]
- Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res. 1997;339:115-62.
- [CrossRef] [PubMed] [Google Scholar]
- Validity, reliability, and responsiveness of the Banff patellar instability instrument (BPII) in a adolescent population. J Pediatr Orthop. 2018;38:e629-33.
- [CrossRef] [PubMed] [Google Scholar]
- Patellofemoral joint instability: Where are we in 2018? In: ESSKA Instructional Course Lecture Book. Berlin, Germany: Springer; 2018. p. :112-70.
- [CrossRef] [Google Scholar]
- Generalized joint laxity and contralateral patellar hypermobility in unilateral recurrent patellar dislocators. Arthroscopy. 2006;22:861-5.
- [CrossRef] [PubMed] [Google Scholar]
- First-time patellofemoral dislocation: Risk factors for recurrent instability. J Knee Surg. 2015;28:303-9.
- [CrossRef] [PubMed] [Google Scholar]
- Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26.
- [CrossRef] [PubMed] [Google Scholar]
- Concepts of the distal medial patellar restraints: Medial patellotibial ligament and medial patellomeniscal ligament. Sports Med Arthrosc Rev. 2019;27:143-9.
- [CrossRef] [PubMed] [Google Scholar]
- Patellofemoral instability. In: Petrera M, Dwyer T, Gobbi A, eds. The Patello Femoral Joint: State of the Art in Evaluation and Management. Berlin, Germany: Springer; 2014.
- [CrossRef] [Google Scholar]
- Variation in tibial tuberosity-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med. 2013;42:389-93.
- [CrossRef] [PubMed] [Google Scholar]
- Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc. 2014;22:2308-14.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database of Syst Rev. 2015;2:CD008106.
- [CrossRef] [Google Scholar]
- Patellofemoral joint instability: A review of current concepts. J Orth Trauma. 2016;6:1-8.
- [CrossRef] [Google Scholar]
- Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215-20.
- [CrossRef] [Google Scholar]
- Patellar instability management: A survey of the international patellofemoral study group. Am J Sports Med. 2017;46:3299-306.
- [CrossRef] [PubMed] [Google Scholar]
- Medial patellofemoral ligament reconstruction: Fixation technique biomechanics. J Knee Surg. 2015;29:303-9.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations. Am J Sports Med. 2016;44:2993-3005.
- [CrossRef] [PubMed] [Google Scholar]
- Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014;30:1018-25.
- [CrossRef] [PubMed] [Google Scholar]
- Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: A systematic review. Arthroscopy. 2015;31:1372-80.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916-23.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41:1030-8.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent patellofemoral instability rates after MPFL reconstruction techniques are in the range of instability rates after other soft tissue realignment techniques. Knee Surg Sports Traumatol Arthrosc. 2020;28:1919-31.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of risk factors on clinical outcomes following anatomical medial patella femoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2013;21:318-24.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral tunnel enlargement after medial patellofemoral ligament reconstruction: Prevalence, risk factors, and clinical effect. Am J Sports Med. 2014;42:297-301.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of error in the identification of anatomical landmarks on the accuracy of Q angle values. Clin Biomech. 2001;16:710-3.
- [CrossRef] [Google Scholar]
- Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage. Am J Sports Med. 2006;34:1478-85.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med. 2000;28:345-9.
- [CrossRef] [PubMed] [Google Scholar]
- Management of overtight medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:480-3.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar fracture after medial patellofemoral ligament surgery. J Bone Joint Surg Am. 2011;93:e971-8.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of graft source and configuration on revision rate and patient-reported outcomes after MPFL reconstruction: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25:2511-9.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral retinacular release: A survey of the international patellofemoral study group. Arthroscopy. 2004;20:463-8.
- [CrossRef] [PubMed] [Google Scholar]
- Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16:383-8.
- [CrossRef] [PubMed] [Google Scholar]
- Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy. 2015;31:422-7.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated trochleoplasty for recurrent patellar dislocation has lower outcome and higher residual instability compared with combined MPFL and trochleoplasty: A systematic review. Arch Orthop Trauma Surg. 2019;139:1617-24.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of trochlear dysplasia as predictor of clinical outcome after trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1615-61.
- [CrossRef] [PubMed] [Google Scholar]
- Trochleoplasty with a flexible osteochondral flap. Bone Joint J. 2017;99:344-50.
- [CrossRef] [PubMed] [Google Scholar]
- Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41:998-1004.
- [CrossRef] [PubMed] [Google Scholar]
- The Lyon's sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. Int Orthop. 2012;37:433-9.
- [CrossRef] [PubMed] [Google Scholar]
- Trochleoplasty techniques provide good clinical results in patients with trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2018;26:2640-58.
- [CrossRef] [PubMed] [Google Scholar]
- Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2014;22:2484-90.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic deepening trochleoplasty for chronic anterior knee pain after previous failed conservative and arthroscopic treatment. Report of two cases. Int J Surg Case Rep. 2017;40:63-8.
- [CrossRef] [PubMed] [Google Scholar]
- The role of trochleoplasty in patellofemoral instability. Sports Med Arthrosc Rev. 2012;20:171-80.
- [CrossRef] [PubMed] [Google Scholar]
- Modified Dejour trochleoplasty for severe dysplasia: Operative technique and early clinical results. Knee. 2006;13:266-73.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial tuberosity-posterior cruciate ligament distance. Am J Sports Med. 2012;40:1119-25.
- [CrossRef] [PubMed] [Google Scholar]
- Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;177:176-81.
- [CrossRef] [Google Scholar]
- Anteromedial tibial tubercle transfer. The Patello Femoral Joint: State of the Art in Evaluation and Management 2014
- [CrossRef] [Google Scholar]
- Tibial tuberosity osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34:305-9.
- [CrossRef] [PubMed] [Google Scholar]
- Patellofemoral instability in athletes. Am J Sports Med. 2010;38:992-9.
- [CrossRef] [PubMed] [Google Scholar]
- The outcomes of modified fulkerson osteotomy procedure to treat habitual patellar dislocation associated with high-grade trochlear dysplasia. Arthroscopy. 2017;33:e74.
- [CrossRef] [Google Scholar]
- Anteromedialization of the tibial tubercle: A 4-to 12-year follow-up. Oper Tech Sports Med. 2000;8:131-7.
- [CrossRef] [Google Scholar]
- Anteromedial tibial tubercle transfer without bone-graft. Am J Sport Med. 1990;18:490-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anteromedial tibial tubercle transfer in patients with chronic anterior knee pain and a subluxation-type patellar malalignment. Am J Sport Med. 1997;25:375-81.
- [CrossRef] [PubMed] [Google Scholar]
- The incidence of complications of tibial tubercle osteotomy: A systematic review. Arthroscopy. 2015;31:1819-25.
- [CrossRef] [PubMed] [Google Scholar]






