Translate this page into:
Cross-sectional area correlation of anterior tibial tendon and extensor hallucis longus tendon: A diagnostic approach for anterior tibial tendon dysfunction
*Corresponding author: Rajesh Botchu, Department of Musculoskeletal Radiology, Royal Orthopedic Hospital, Birmingham, United Kingdom drrajeshb@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mettu S, Shirodkar K, Ariyaratne S, Nischal N, Iyengar KP, Beale D, et al. Cross-sectional area correlation of anterior tibial tendon and extensor hallucis longus tendon: A diagnostic approach for anterior tibial tendon dysfunction. J Arthrosc Surg Sports Med. 2024;5:81-3. doi: 10.25259/JASSM_10_2024
Abstract
Objectives:
Anterior tibial tendon (ATT) pathologies, though infrequent, can significantly impact patient morbidity. This study aims to describe the cross-sectional area (CSA) of ATT on magnetic resonance imaging (MRI).
Materials and Methods:
A retrospective study was done on 50 consecutive patients with normal ATT who underwent ankle MRI. The CSA measurements of the ATT with the extensor hallucis longus tendon (EHLT) were measured by one consultant radiologist and one radiology fellow with one repeating measurement after a period of two weeks.
Results:
Patients were categorized into four age groups: <20, 20-40, 40-60, and >60 years. The average CSA ratio between ATT and EHLT was found to be 1.64, 1.63, 1.64, and 1.67, respectively, for each age group.
Conclusion:
These findings provide quantitative insights into the correlation between ATT and EHLT CSAs across different age brackets in normal population. These can aid in the diagnosis of pathologies of ATT, such as tendinopathy and tear.
Keywords
Anterior tibial tendon
Tendinopathy
Magnetic resonance imaging
Cross-sectional area
Correlation
INTRODUCTION
Anterior tibial tendon (ATT) pathologies are not uncommon and can cause anterior ankle pain. ATT usually sustains minor stress due to its relatively straight course compared to the posterior tibial tendon. While abnormalities are less common, degenerative tendinosis can occur, leading to partial or complete ATT tears, often spontaneous and unrelated to trauma.[1] Symptoms of tendinosis manifest as intermittent dull pain over the front of the ankle, worsening with activity, particularly uphill walking or running. Weakness during foot elevation may also be present.[2] Tendons are exposed to considerable tensile loading during the force-transmitting mechanism and, therefore, are vulnerable to developing load-induced injury.[3] The tendon thickens in response to frequent tensile overload or sudden stress. This increase in tendon thickness can occur due to temporary swelling and edema or long-lasting disorganized repair.[4] Thickening of ATT due to stress response is apparent on imaging. Despite extensive research on the cross-sectional area (CSA) correlation between tibialis posterior and flexor hallucis longus tendons, the relationship between ATT and adjacent extensor hallucis longus tendon (EHLT) remains unexplored.[5,6] This study aims to investigate the CSA correlation between the normal ATT and EHLT.
MATERIALS AND METHODS
Study design and population
This retrospective study evaluated 50 consecutive patients who underwent ankle magnetic resonance imaging (MRI). Exclusion criteria comprised patients with ankle MRI scans related to trauma, infection, and neoplasm. Patient demographics, including age and sex, were recorded.
Imaging parameters
Ankle MRI was performed on 3T MRI, Ingenia Elition; Philips Healthcare, Best, the Netherlands. The study utilized axial and sagittal proton density (PD) with a repetition time of 2499 ms, echo time of 30 ms, a slice thickness of 3 mm, and field of view of 160 mm.
Image analysis
A fellowship-trained musculoskeletal radiology consultant with over 10-year experience and a fellow assessed the images. Analysis was done on axial sections taken 2 cm cranial to the ankle joint. Tendons were manually traced along the perimeter contours on 2D axial images. Peritendinous sheath was not included while tracing the tendon contour. CSA of ATT and EHLT was calculated [Figure 1]. The ratio of CSAs between the ATT and EHLT was then computed.
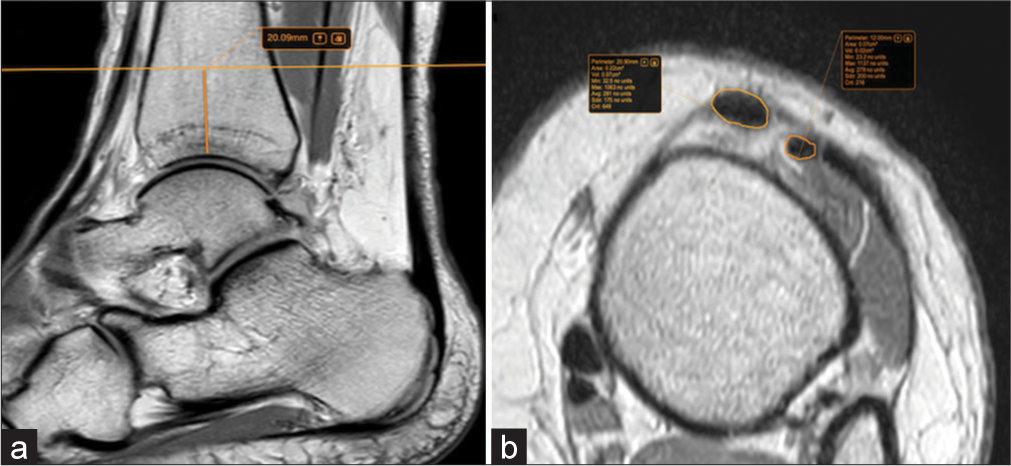
- (a) Proton-density (PD) sagittal image shows the reference point for measurements, 2 cm cranial to the ankle joint. (b) Cross-sectional area measurements, taken by manual tracing technique on PD axial age.
Statistical analysis
The statistical analysis of the study involved descriptive statistics and inferential analyses. Descriptive statistics included grouping continuous variables, such as age, and summarizing categorical variables, such as sex. For the inferential analysis, a paired t-test was conducted to assess the significance of the differences in CSA ratios between ATT and EHLT within each age group. In addition, an analysis of variance was employed to evaluate whether there were statistically significant differences in the mean CSA ratios among the different age groups. P < 0.05 was considered to be statistically significant. Intra-class coefficient was calculated to evaluate for intra- and inter-observer reliability.
RESULTS
The study included 50 patients ranging from 9 to 86 years, with an average age of 39.06 years, of which 26 were male. Patients with tumors, tears, and tendinopathy and those with a history of surgery were excluded from the study. The cohort, stratified by age (under 20, 20-40, 41-60, and above 60), exhibited age-specific CSA ratios of ATT to EHLT. Notably, the under-20 group displayed a mean CSA ratio of 1.64 (range: 1.15-2). In the 20-40 age range, the mean CSA ratio was 1.63 (range: 1.15-2.25). The 41-60 age group demonstrated a mean CSA ratio of 1.64 (range: 1.38-1.92), while those above 60 exhibited a mean CSA ratio of 1.67 (range: 1.27-2.09) [Table 1]. Despite variations, no statistically significant differences emerged between age groups. The overall cohort’s mean CSA ratio of ATT to EHLT was 1.65. There was good intra- and interobserver reliability with a kappa of 0.8.
| Cohort (Age in years) | <20 | 20–40 | 40–60 | >60 |
|---|---|---|---|---|
| Average ratio (ATT/EHLT) | 1.70 | 1.65 | 1.64 | 1.67 |
| Maximum ratio | 2.25 | 1.92 | 1.92 | 2.09 |
| Minimum ratio | 1.15 | 1.38 | 1.38 | 1.27 |
| Average age (years) | 15.5 | 28.2 | 50.3 | 67.5 |
| Maximum age (years) | 20 | 40 | 60 | 86 |
| Minimum age (years) | 9 | 20 | 40 | 60 |
ATT: Anterior tibial tendon, EHLT: Extensor hallucis longus tendon
DISCUSSION
ATT pathologies can cause anterior ankle pain. The ATT, exposed to tensile loading during force transmission, is prone to load-induced injuries. While complete tears are easily identifiable, clinical diagnosis of tendinosis or partial tears presents challenges.[7] MRI emerges as a valuable noninvasive tool, providing delineation of the ATT with uniform low-signal intensity on T1-weighted images and PD images. These offer excellent detailed anatomical insight at the tendon injury site. A previous study encompassing 28 patients with suspected ATT dysfunction identified a tendon thickness of ≥5 mm as a pathological characteristic.[8] Notably, this study did not consider age-related thickness variations. In our study, a size comparison with the adjacent EHLT revealed a consistent ratio across different age groups. This has important consequences for image interpretation as normal ratios are thus applicable to all patients irrespective of their age. Furthermore, considering the fact that established tendon area ratios at other sites, notably tibialis posterior and flexor hallucis longus serves as useful imaging marker of pathologies, the concept may also be explored in other tendons. This can add to diagnostic confidence in equivocal cases.
Previous researchers have found that tendon thickness is correlated with inflammation of a tendon.[9] However, partial damage and asymmetrical inflammatory thickening can occur rather than overall involvement giving rise to measurement bias.[10] Contrary to tendon thickness, CSA measurement served as a better diagnostic parameter, avoiding potential measurement biases. This approach allows for a more nuanced analysis of tendon dysfunction. A potential pitfall in employing CSA ratio for tendon dysfunction diagnosis is the presence of fibrosing tenosynovitis. In this condition, the dark adherent synovium may create an illusion of tendon hypertrophy on MRI.[6] Instances displaying normal tendon size yet presenting heightened signal intensity on T1, T2, or PD images warrant cautious diagnosis of a clinically relevant ATT lesion. This caution arises from the acknowledgment that signal intensity changes in the ATT substance can occur due to the magic angle artifact, even in the absence of actual tendon dysfunction.[11] This was proven in preceding investigations, where approximately 11% of asymptomatic individuals manifested signal abnormalities attributable to the magic angle artifact.[8] Notably, our current study deliberately omitted the consideration of signal intensity abnormalities. Consequently, the evaluation of abnormal tendon size through CSA measurements may sometimes serve as the sole indicator for assessing tendon dysfunction.
Limitations
This study has a few limitations. First, the small cohort size underscores the need for larger-scale studies to firmly establish the CSA correlation between the ATT and EHLT. In addition, the use of routine ankle axial imaging, rather than oblique axial imaging perpendicular to the long axis of the ATT, may introduce inaccuracies. While the latter is more precise, its uncommon usage in daily practice, attributed to time constraints and interpretational challenges for other structures, limits its feasibility.
CONCLUSION
This study suggests that the CSA of the ATT is approximately 1.6 times that of the extensor hallucis longus tendon. Noteworthy, deviations from this size correlation may imply an underlying pathology of the ATT.
Ethical approval
This was a retrospective study using anonymized data; hence, ethical approval not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Achilles tendon injuries. Curr Rev Musculoskelet Med. 2017;10:72-80.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy, bony pelvis and lower limb: Tibialis anterior muscles In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513304 [Last accessed on 2023 Aug 28]
- [Google Scholar]
- Tendon biomechanics and mechanobiology--a minireview of basic concepts and recent advancements. J Hand Ther. 2012;25:133-40. quiz 141
- [CrossRef] [PubMed] [Google Scholar]
- Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43:409-16.
- [CrossRef] [PubMed] [Google Scholar]
- Foot fellows review: Tibialis posterior: A review of anatomy and biomechanics in relation to support of the medial longitudinal arch. Foot Ankle. 1991;11:244-7.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of disorders of the posterior tibialis tendon. AJR Am J Roentgenol. 2000;175:627-35.
- [CrossRef] [PubMed] [Google Scholar]
- 3-Tendons and muscles, musculoskeletal MRI (3rd ed). Netherlands: Elsevier; 2020. p. :53-84.
- [CrossRef] [Google Scholar]
- Anterior tibial tendon abnormalities: MR imaging findings. Radiology. 2005;235:977-84.
- [CrossRef] [PubMed] [Google Scholar]
- The correlations between dimensions of the normal tendon and tendinopathy changed Achilles tendon in routine magnetic resonance imaging. Sci Rep. 2021;11:6131.
- [CrossRef] [PubMed] [Google Scholar]
- The value of the peroneus brevis tendon cross-sectional area in early diagnosing of peroneus brevis tendinitis: The peroneus brevis tendon cross-sectional area. Medicine (Baltimore). 2022;101:e31276.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-and inter-rater reliability for the measurement of the cross-sectional area of ankle tendons assessed by magnetic resonance imaging. Acta Radiol. 2022;63:481-8.
- [CrossRef] [PubMed] [Google Scholar]






