Translate this page into:
Anatomical and cost-effective technique of fixation of osteochondral defect of femur with absorbable sutures
*Corresponding author: Vikram Arun Mhaskar, Department of Orthopedics, Sitaram Bhartia Institute of Science and Research, New Delhi, India. drvikrammhaskar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mhaskar VA, Patel H. Anatomical and cost-effective technique of fixation of osteochondral defect of femur with absorbable sutures. J Arthrosc Surg Sports Med. 2025;6:32-6. doi: 10.25259/JASSM_28_2024
Abstract
Objectives:
Osteochondral defect in the femur commonly occurs as a focal defect. This can lead to locking and progressive degeneration. Treatment should involve fixing the fragment back wherever possible. Fixation can be done arthroscopically or by open surgery, with distinct advantages of the former. Techniques of fixation vary with biopins, screws, or anchors. Compression of the fragment to the freshened base is critical for union, and we describe a unique economical and biological technique that produces good compression and results at medium-term follow-up.
Method:
We describe a unique technique of using multiple crisscross absorbable No. 1 Vicryl sutures using the suture bridge technique to fix osteochondral fractures of the femur.
Results:
We had seven cases with no failures at a mean of 74 weeks follow-up. In all cases, radiological union was seen on computed tomography, magnetic resonance imaging, and X-rays. The mean knee injury and osteoarthritis outcome score for pain, activities of daily living, symptoms, sports, and recreational activity were calculated with statistically significant improvement in all parameters.
Conclusion:
This technique has not been described in the literature and combines the benefit of being biological with no permanent residual implant, cost-effective, and minimal implants that do not violate the fragment.
Keywords
Osteochondral defect
Anatomical fixation
Biopins
Crisscross suture technique
Cost-effective osteochondral fixation
INTRODUCTION
Osteochondral defects of the patella and femur are common in young active patients. They can occur due to trauma, repetitive impact, or due to unknown vascular insults. Patients with osteochondral defects present with symptoms of pain, instability, locking, and swelling.[1]
Osteochondral defects significantly hamper joint biomechanics and can eventually lead to joint degeneration. If this is managed conservatively by immobilization and physiotherapy, the outcomes are poor.[2]
Therefore, surgical management is preferred in young patients to preserve normal anatomy and relieve symptoms. Conventional techniques for the treatment of these defects can be classified into anatomical and non-anatomical. Non-anatomical techniques are chondroplasty, autologous or allograft transplantation, and microfracture.[3-6] Anatomical techniques are fixation using anchors, biopins, screws, etc. Fixation of the fragments can be done arthroscopically or through open surgery, with the former being more technically demanding.
Fixation is the most anatomical and biological way to fix the defects that occur due to mechanical causes such as trauma or overuse, as it reconstitutes the native morphology best. The advantage of using crisscross suture fixation and Bio-pins is that they are absorbable, give good compression, and do not require removal.[7] Outcomes with both implants are comparable. In fixation, the revision rates are higher if fixation is not done adequately and anatomically.
In all previous techniques of refixation, implants are passed through the fragment to stabilize and fix it, which runs the risk of breaking the fragment and is hard to use in smaller fragments. In this technique, the fragment is not violated with tunnels made adjacent to the fragment and sutures passed through them. The suture material used is No. 1 Vicryl, which gets completely absorbed in 56–70 days, which is sufficient time for the lesion to heal.
In literature, they suggest that surgeons with specific training do these procedures in that technique keeping in mind the patient’s age, requirements, and disability. We describe a technique that does not require any special instrumentation or implants in isolation and is cost-effective with good results. It can be supplemented with biopins to strengthen the construct wherever required.
MATERIALS AND METHODS
All cases with osteochondral lesions of the femoral condyle that were fixed primarily by arthroscopic suture bridge technique between January 2021 and July 2023 were followed up. Pre-operative X-rays and magnetic resonance imaging (MRI) [Figure 1] were done, and post-operative X-rays were done immediately post-surgery and at 6 weeks post-surgery. Computed tomography (CT) scan and MRI were done at 3 months post-surgery. The knee injury and osteoarthritis outcome score (KOOS) score was done preoperatively and at one year post-surgery. The inclusion and exclusion criteria were as per Box.

- (a-c) Preoperative magnetic resonance images of a representative case with the red arrows indicating the osteochondral lesion.
| Inclusion criteria |
|
| Exclusion criteria |
|
Arthroscopic femur osteochondral fracture fixation
First, diagnostic arthroscopy is performed with anteromedial and anterolateral portals [Video]. The osteochondral lesion is identified, and its fragment is identified [Figure 2a]. The base of the lesion is gently curetted to remove the fibrous tissue [Figure 2b]. Multiple microfractures are done in the bed with a bone awl to release fibroblasts [Figure 2c]. The fragment is manipulated to its bed using a probe so that it sits anatomically [Figure 3a]. A ‘K’-wire is then introduced through the anteromedial portal and using the sharp tip, the fragment is further made to sit anatomically when convinced the wire is drilled through the fragment to stabilize it temporarily [Figure 3b]. A Beath pin is then drilled through the medial femoral condyle at 3 o’ clock to the fragment and not violating it [Figure 3c]. This is loaded with one end of a No. 1 Vicryl that is delivered on the medial aspect of the femur outside the skin. Another Beath pin carrying the other end of the No. 1 Vicryl is drilled at 9 o’clock to the fragment and not violating it and the end is delivered on the medial aspect of the femur outside the skin [Figures 3d and e]. Multiple (at least 4) No. 1 Vicryl are passed similarly to surround the fragment all around [Figure 3f]. The ends of the sutures are delivered through the skin over the medial aspect of the thigh [Figure 4a]. Knicks are made on the skin connecting the two ends of each No. 1 Vicryl and the wound is dissected to the bone using artery forceps [Figure 4b]. The two ends of the sutures are delivered through the incision [Figure 4c]. The sutures are tied with multiple half hitches (at least three) to compress the fragment to its footprint [Figure 4d]. The fixed fragment is then viewed arthroscopically [Figure 4e].
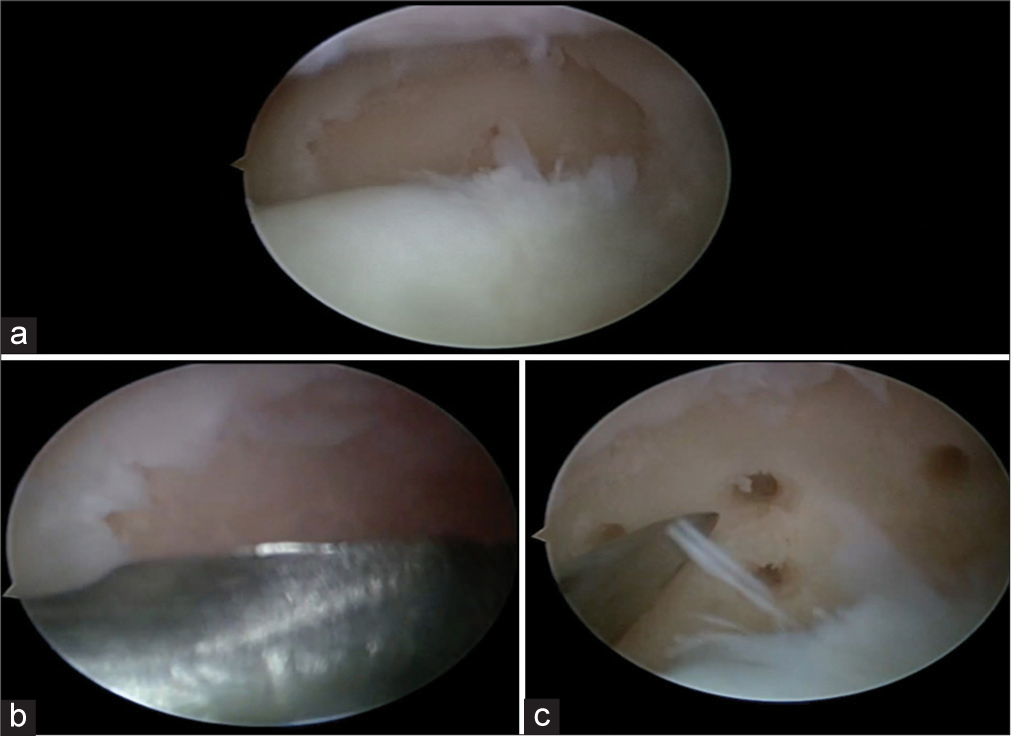
- (a) Arthroscopic image of an osteochondral fragment of the medial femoral condyle seen separated from its bed, (b) arthroscopic image showing the bed of the fragment being curetted, and (c) arthroscopic image showing microfractures being done in the bed of the fragment on the medial femoral condyle.
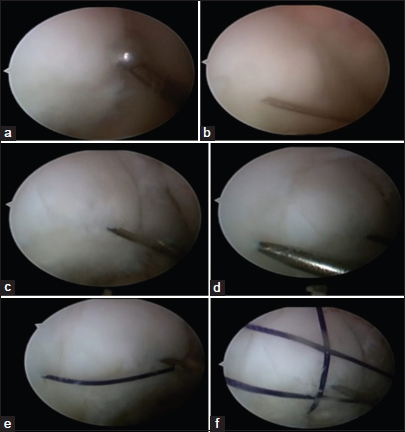
- (a) Arthroscopic image showing the fragment reduced to its anatomical location with a probe, (b) arthroscopic image showing the osteochondral fragment temporarily fixed to its bed with a ‘K’ wire, (c) arthroscopic image showing a beath pin carrying one end of a No. 1 Vicryl drilled through the medial femoral condyle at 3 o’ clock position to the fragment, (d) arthroscopic image showing a beath pin carrying the other end of a No. 1 Vicryl drilled through the medial femoral condyle at 9 o’; clock position to the fragment, (e) arthroscopic image showing a No. 1 Vicryl encircling the osteochondral fragment and compressing it to its bed, and (f) arthroscopic image showing multiple No. 1 Vicryl sutures stabilizing the fragment.
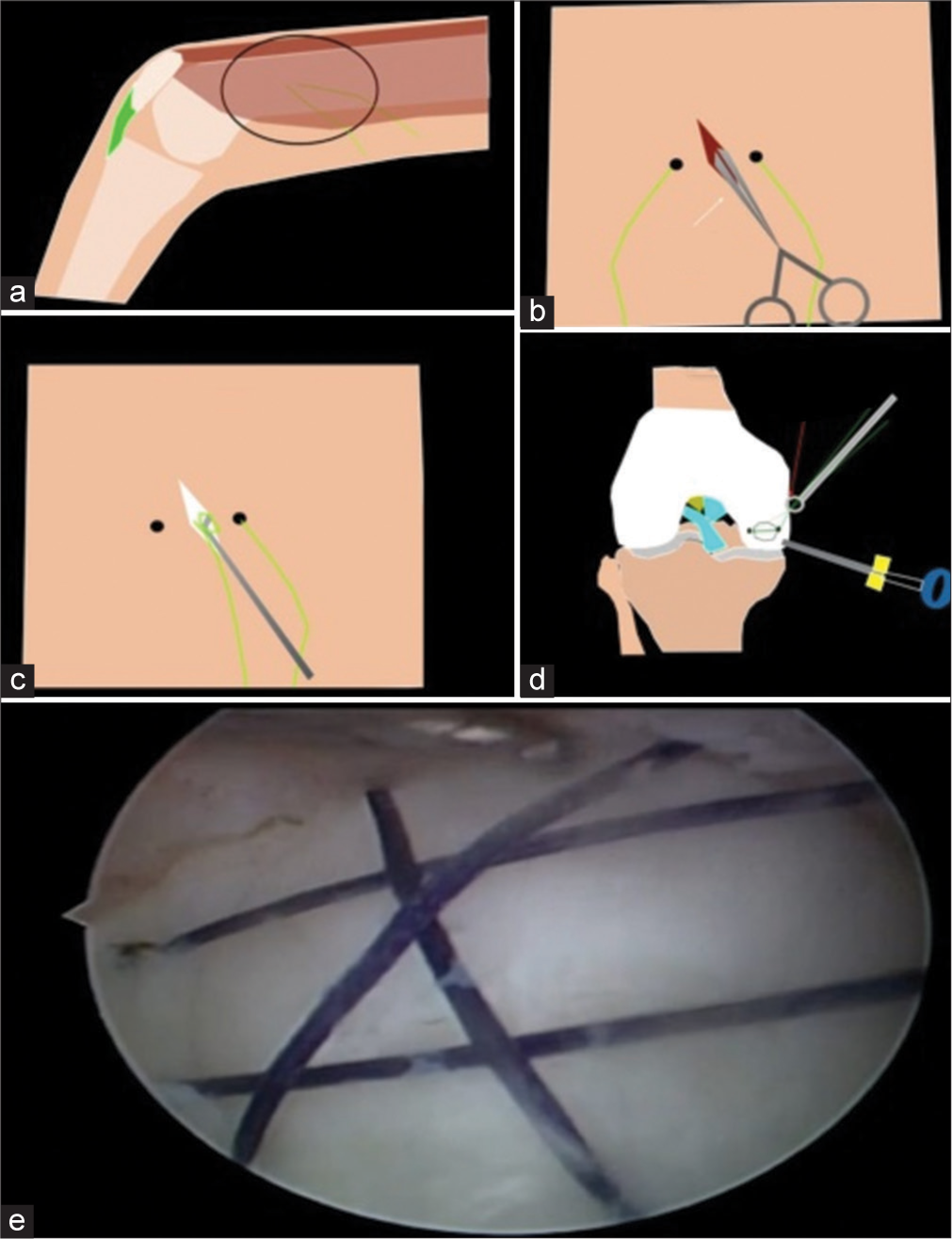
- (a) Illustration of No. 1 Vicryl sutures exiting through the medial aspect of the thigh (black circle), (b) illustration showing a linear incision made between the two ends of the same suture, (c) illustration showing a probe delivering the two ends of the suture through the wound, (d) illustration showing a knot pusher tying two ends of the suture on the medial femoral cortex to stabilize the fragment, and (e) arthroscopic image showing the stabilized fragment with multiple No. 1 Vicryl sutures.
Video:
Video:Technique of fixation of an osteochondral fragment fixation of the femoral condyle arthroscopically.Post-operative rehabilitation
The patient is kept non-weight bearing for six weeks on a long knee brace.
Range of motion (ROM) 0–30° for 2 weeks, 0–60° for 4 weeks and 0–90° for six weeks.
After six weeks the patient is allowed to weight bear as tolerated.
Sports are allowed after three months. X-rays were done at one month postoperatively, MRI scan [Figure 5a] and CT [Figure 5b] at three months post-surgery.
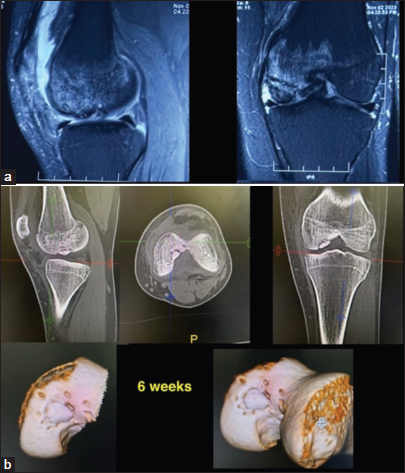
- (a) Magnetic resonance images after 3 months showing the fragment has healed and (b) computed tomographic scan images after 3 months showing the fragment has healed.
RESULTS
A total of seven male patients, who all had osteochondral defects were followed up for a mean 74 weeks post-surgery. All seven had traumatic episodes preceding the symptoms (four patients had two-wheeler road traffic accidents, one patient had a sports injury while playing football, and two slipped and fell from stairs). All seven cases had locking and pain as their symptoms. The mean age was 21 years and they were operated at a mean 31 days after injury.
The radiological union was found in 100% of our patients on X-rays, CT, and MRI. The mean KOOS score for pain preoperatively was 11.85%, and postoperatively, it was 87.85%. The mean KOOS for activities of daily living preoperatively was 15.57% and postoperatively was 87.57%, the mean KOOS for sports and recreational activities pre-operative was 4.85% and post-operative was 87.85%, the mean KOOS for symptoms preoperatively was 6.7% and postoperative was 88% at 12 months follow-up. No complications were observed during the period of study. Full ROM was achieved in all patients [Figures 6a and b].
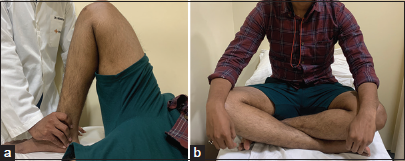
- (a) Full range of motion at 6 months postoperatively in a sample patient and (b) same patient sitting cross-legged at 6 months post-surgery.
DISCUSSION
Osteochondral lesions can happen due to injury or vascular insults like osteochondritis dissecans. Pain and mechanical symptoms like locking are the predominant symptoms. The femoral condyles and the patella are potential areas from where these fragments can separate. The fragment may partially separate from its bed or completely separate and form a loose body. Fragments coming from the patella when due to trauma can be associated with patellar subluxations and dislocations. Osteochondral lesions of the femoral condyle, especially the weight-bearing portion if not addressed can lead to degeneration of that compartment. Fixation of the fragment should be attempted wherever possible to reconstitute the anatomy of the area. Preparing the bed of the fragment is critical using a curette so that the fragment heals onto a raw and viable surface. This is especially important in cases of osteochondritis dissecans where the bed may be non-negotiable. In traumatic cases, bed preparation is essential as fibrous tissue may form over it when the fragment is separated for long. Removing this tissue exposes a viable and bleeding surface for proper healing. Fixation techniques can be open or arthroscopic with arthroscopic techniques being more technically demanding. Fixation has been shown to have good results and leads to the union of the fragment in the majority of cases reported in the literature.
Fixation devices range from suture anchors, screws, biopins, and absorbable and non-absorbable sutures. Metallic screws provide good compression but are permanent implants that remain in the knee. If left a little proud, they can destroy the tibial cartilage and lead to degeneration of the joint. There is an added problem of violating the fragment and causing potential comminution of the fragment. Biopins have the advantage of being absorbable and providing compression, being smooth they potentially cause less comminution. It is technically demanding to apply them arthroscopically as they are applied through cannulas through a small drill hole and getting the direction of tapping the pins can be difficult. Suture anchor fixation is also effective; however, it requires drilling through the bed of the fragment and uses absorbable and non-absorbable sutures. Although effective from a union point of view – nonabsorbable sutures remain and can abrade the cartilage.
No. 1 Vicryl (polyglactin 910) retains 65% of its strength at 14 days, undergoes minimal absorption for 40 days, and completely absorbs in 56–70 days which was used in this set of patients. We intended to use all absorbable sutures and pins only as anything non-absorbable on a joint surface can potentially cause continuous abrasion of the cartilage. Furthermore, the fixation device is useful only till the fragment unites and it can potentially have future hardware-related complications.
The technique also did not violate the fragment and indirectly compressed the fragment retaining the original anatomy. Multiple such sutures in different directions around the fragment give compression in different planes. The sutures subside into the cartilage when tied on the opposite cortex and potentially do not abrade against the tibial surface. We also used bio pins in two cases to supplement the all-suture fixation.
Potential advantages of the technique are that it provides good compression, is easily available, does not violate the fragment, and is bioabsorbable. Disadvantages are that it is technically demanding, the strength of the sutures is potentially less than non-absorbable ones and if the fragment does not unite, there is no mechanical stability provided by the sutures.
CONCLUSION
We present a novel technique of fixation of osteochondral defect of the femur with crisscross absorbable sutures. This technique has not been described before. It combines the benefit of being biological with no permanent residual implant, cost-effective, and minimal implants that do not violate the fragment.
Author contributions
VAM: Conceptualization, writing, and statistical analysis; HP: Assisted in drafting the manuscript, data collection, and statistics.
Ethical approval
The research/study complied with the Helsinki Declaration of 1975, as revised in 2008 (5).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Osteochondritis dissecans of the knee: Pathoanatomy, epidemiology, and diagnosis. Clin Sports Med. 2014;33:181-8.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondritis dissecans of the knee-conservative treatment strategies: A systematic review. Cartilage. 2019;10:267-77.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of existing cartilage repair technology. Sports Med Arthrosc Rev. 2008;16:196-201.
- [CrossRef] [PubMed] [Google Scholar]
- Fresh osteochondral allograft transplantation for the knee: Current concepts. J Am Acad Orthop Surg. 2014;22:121-33.
- [CrossRef] [PubMed] [Google Scholar]
- The history of radiofrequency energy and Coblation in arthroscopy: A current concepts review of its application in chondroplasty of the knee. J Exp Orthop. 2019;6:1.
- [CrossRef] [PubMed] [Google Scholar]
- Implantless fixation of a large osteocartilaginous fracture of the lateral femoral condyle in a child. Knee Surg Relat Res. 2017;29:72-5.
- [CrossRef] [PubMed] [Google Scholar]
- Bioabsorbable fixation of unstable osteochondritis dissecans lesions. Am J Sports Med. 2010;38:2065-70.
- [CrossRef] [PubMed] [Google Scholar]






