Translate this page into:
Single-stage revision anterior cruciate ligament reconstruction for anatomic, massive dilated tunnels using “the sandwich technique”
*Corresponding author: Dhruv Paul, Department of Sports Medicine, Arthroscopy and Joint Reconstruction, Manipal Hospital, Bengaluru, Karnataka, India. dhrv.paul@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thonse C, Paul D, Shukla S, Shetty DK. Single-stage revision anterior cruciate ligament reconstruction for anatomic, massive dilated tunnels using “the sandwich technique.” J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_47_2024
Abstract
At present, revision anterior cruciate ligament reconstruction (ACL-R) with dilated tunnels is managed as a two-stage procedure which results in longer recovery and rehabilitation as well as late return to sports. In the present “sandwich” technique, management of revision ACL-R with dilated tunnels can be carried out as a single-stage procedure, which basically entails sandwiching the tibia end of bone patellar tendon bone graft in between the allograft and the tibial tunnel. The present case highlights the use of a novel technique coined as the “sandwich technique” for managing revision ACL-R in a 38-year-old male with dilated femoral and tibial tunnels which is usually managed through staged procedures. Single-stage “sandwich technique” is a viable option in managing revision anterior cruciate ligament scenarios with massive, dilated tunnels, thus decreasing the morbidity, mental agonies, and financial obligations associated with an additional procedure.
Keywords
Sandwich technique
Single-stage revision anterior cruciate ligament reconstruction
Dilated anterior cruciate ligament tunnels
Novel technique
Revision anterior cruciate ligament reconstruction
INTRODUCTION
Anterior cruciate ligament reconstruction (ACL-R) represents a cornerstone in the management of knee injuries, with the primary goal of restoring stability and function, and facilitating the return to pre-injury levels of activity. Despite advancements in surgical techniques and rehabilitation protocols, a subset of patients undergoing ACL-R experiences suboptimal outcomes, necessitating revision surgeries.
The ACL-R revision rate for adults is reported at 4.1% at 5 years in the Danish registry, while the United States and Norway community registries report 0.9–1.5% revision rates.[1,2]
The concept of ACL-R failure remains multifaceted and lacks a universally accepted definition. While some definitions prioritize objective measures such as increased anteroposterior laxity or positive pivot-shift tests, others adopt a broader perspective, considering factors such as pain, stiffness, and functional limitations. This variability underscores the complexity inherent in assessing ACL-R outcomes and identifying patients in need of revision surgery.[3]
Revision ACL-R poses unique challenges compared to primary reconstructions, requiring a comprehensive understanding of the underlying causes of failure and tailored surgical strategies. The success of revision ACL-R hinges on meticulous patient evaluation, precise surgical techniques, and optimized postoperative rehabilitation protocols.
Recent literature underscores the importance of adopting a staged approach to revision ACL-R, prioritizing graft selection, tunnel positioning, and fixation methods to optimize outcomes.[4]
In the present case scenario, the reason for revision ACL-R was graft laxity with a dilated tibial tunnel with secondary varus deformity. Single-stage revision ACL-R with bone grafting and high-tibial osteotomy were considered which avoid a second surgery which is usually the case in two-stage revisions. As a result, post-operative rehabilitation time is reduced which facilitates early return to sports.
PRESENTATION OF THE CASE
This is a case of a 38-year-old male with complaints of right knee instability with deformity. The patient provided a history of primary ACL-R done 10 years back, after which post-operative recovery was uneventful; however, he suffered a twisting injury while playing football 8 years back, following which he had complaints of knee instability and managed his situation with a hinged knee brace all these years long. The patient was unable to return to sports but was able to manage his daily activities with the brace.
On examination, the anterior drawer test, Lachman test, and pivot shift test, all showed grade 3 positivity [Video]. Magnetic resonance imaging scan of the right knee showed a tear of proximal attachment of the anterior cruciate ligament (ACL) graft with laxity of the remaining fibers [Figure 1].
Video:
Video:A quick capture of this unique case with pre-operative clinical findings , short intra-operative video and 3-month follow up clinical and CT scan captures.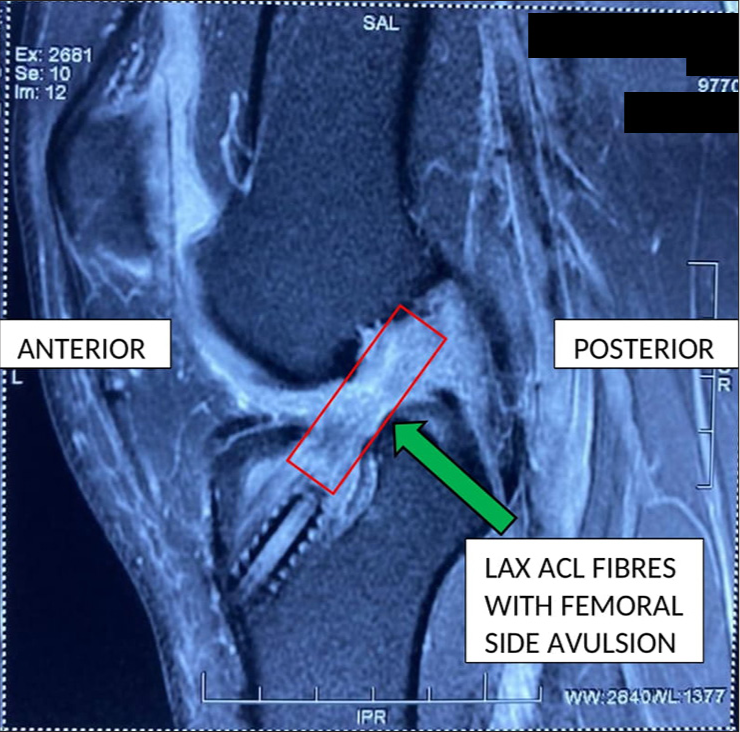
- Magnetic resonance imaging scan of the right knee showing tear of femoral attachment of anterior cruciate ligament graft with (green arrow) laxity of the remaining fibers.
Pre-operative assessment
Pre-operatively planning was executed based on computed tomography (CT) scan, standing scannogram, and single-leg lateral stance view.
Medial proximal tibial angle was 83.1°, lateral distal femoral angle was 86.1, and posterior slope angle was 10°.
Alpha angle calculated by Miniaci method was found to be 8.3° [Figure 2].
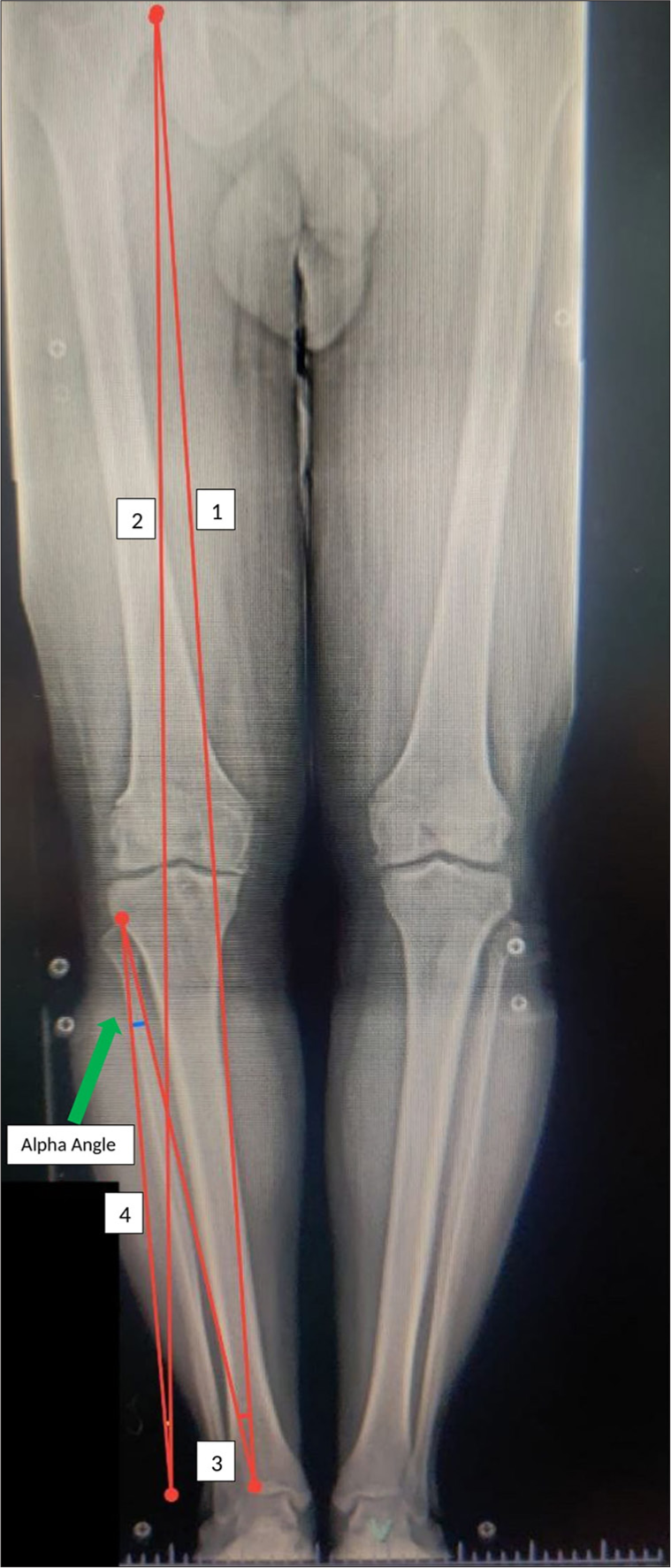
- A standing scanogram Line 1 representing pre-operative mechanical axis: Line 2: Planned weight-bearing line; Angle between lines 3 and 4 represents alpha angle calculated by Miniaci’s method – 8.3° as shown by green arrow.
On pre-operative CT scan, the femoral tunnel diameter was found to be 11.9 mm and the tibial tunnel diameter was 20.5 mm [Figures 3a and b, 4a and b].
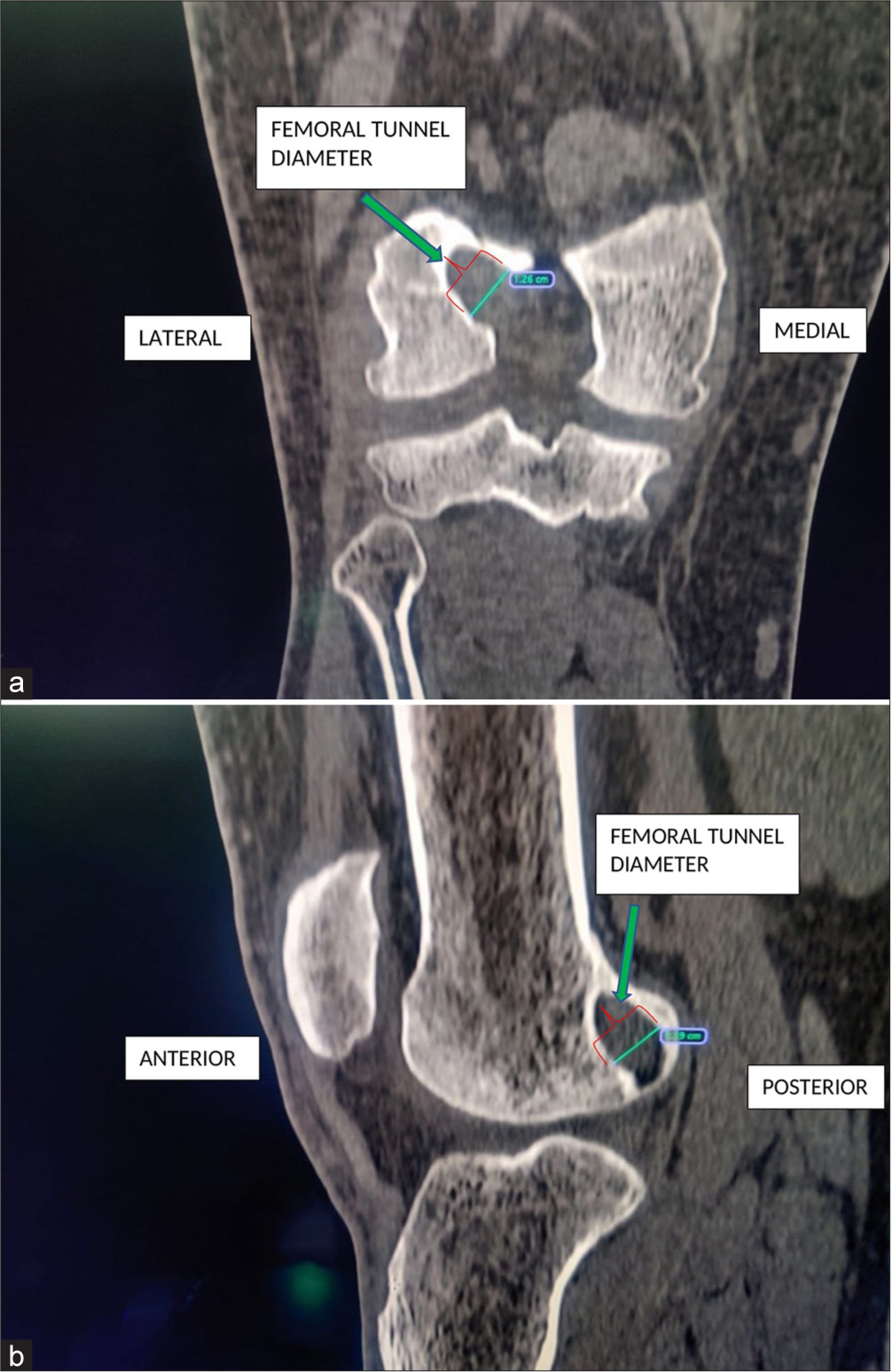
- (a) Pre-operative computed tomography scan coronal section showing femoral tunnel diameter (green arrow) of 12.6 mm, (b) Pre-operative computed tomography scan sagittal section showing femoral tunnel diameter (green arrow) of 11.9 mm.
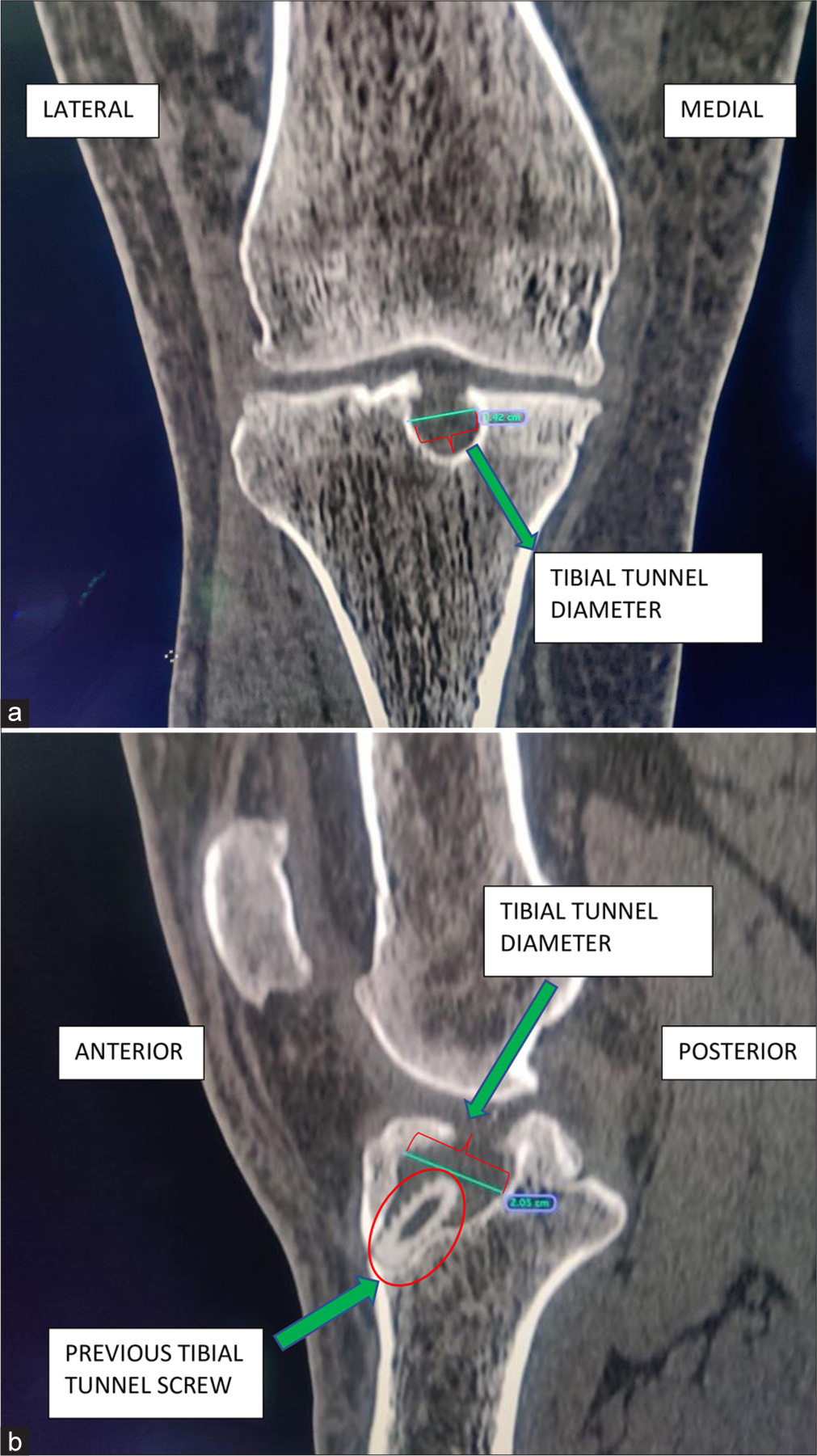
- (a) Pre-operative computed tomography scan coronal section showing tibial tunnel diameter (green arrow) of 14.2 mm. (b) Pre-operative computed tomography scan sagittal section showing tibial tunnel diameter (green arrow) of 20.5 mm.
Based on pre-operative assessment for single-stage revision, bone grafting and bone-patellar tendon-bone (BPTB) graft were planned with correction of varus with high-tibial osteotomy.
SURGICAL TECHNIQUE
The patient was in a supine position under spinal anesthesia with a tourniquet applied. Standard anteromedial and anterolateral portals were made, and a diagnostic arthroscopy was performed. The previous ACL graft was completely disrupted along with medial compartment grade 2 osteoarthritis [Video]. The old ACL graft remnant was cleared using a 4.5 mm shaver and radiofrequency ablator (RFA). Both femoral and tibial tunnels were cleared off [Video]. The dilated tibial tunnel was confirmed on diagnostic arthroscopy, and the initial plan of high-tibial osteotomy with single-stage ACL revision with the “Sandwich technique” was then executed.
Graft harvesting
Bone patellar tendon graft harvest was planned because hamstring tendon graft was harvested for the primary ACL-R. A midline incision of 5 cm was taken from the inferior pole of the patella to the superior aspect of the tibial tuberosity [Figure 4]. Dissection was made down to the level of paratenon. The paratenon was split and carefully reflected off the underlying tendon, thus allowing side-to-side repair. At the tibial tubercle, 30 mm was measured and marked with electrocautery for the bone plug. A saw blade was used to harvest the bone plug in the trapezoidal shape. The bone plug and tendon were lifted until the remaining attachment to the patella was left behind. The bone plug was marked at 20 mm and harvested using a bone saw. The middle third of the patellar tendon, width 10 mm and length 110 mm, including the patellar bone plug of 20 mm (10.5 mm width) and tibial tubercle bone plug of 30 mm (11 mm width), was procured with the help of a saw and 5 mm osteotome [Figure 5a]. As the tibial tunnel was dilated up to 20.5 mm, the bone graft was used to sandwich the tibial end of the graft for a press-fit fixation [Figure 5b].
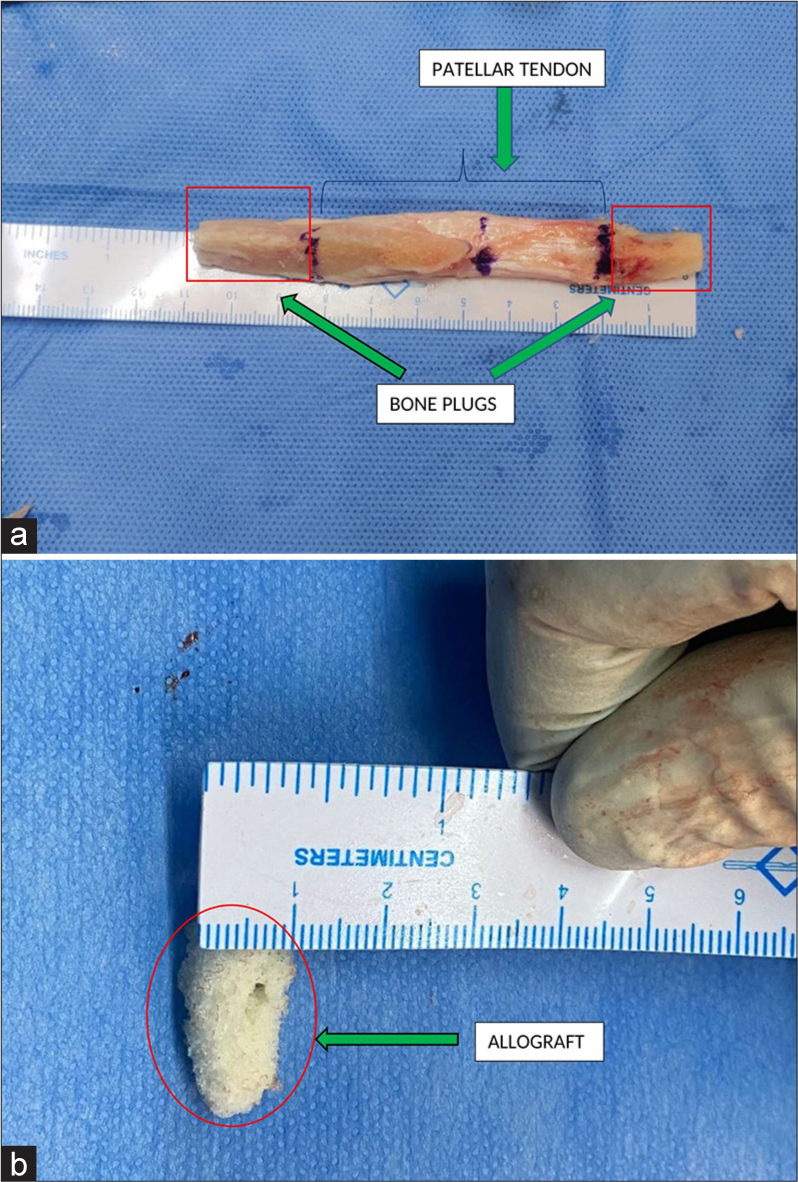
- (a) Showing the (green arrow) bone patellar tendon bone graft measuring 110 mm in length and width of 10 mm. (b) Showing the (green arrow) allograft used for the sandwich technique.
Graft preparation
Initial graft preparation was done by removing the fat pad attached to the graft with the help of scissors and bone nibbler. Bone plugs on either end were fashioned to 10.5 mm on the femoral end and 11 mm on the tibial aspect. Once the bone plug was structured to the appropriate shape, a 2 mm K-wire was used to create two holes through the bone plugs. Number 5 Ethibond was then passed through each of the drill holes [Figure 6a and 6b].
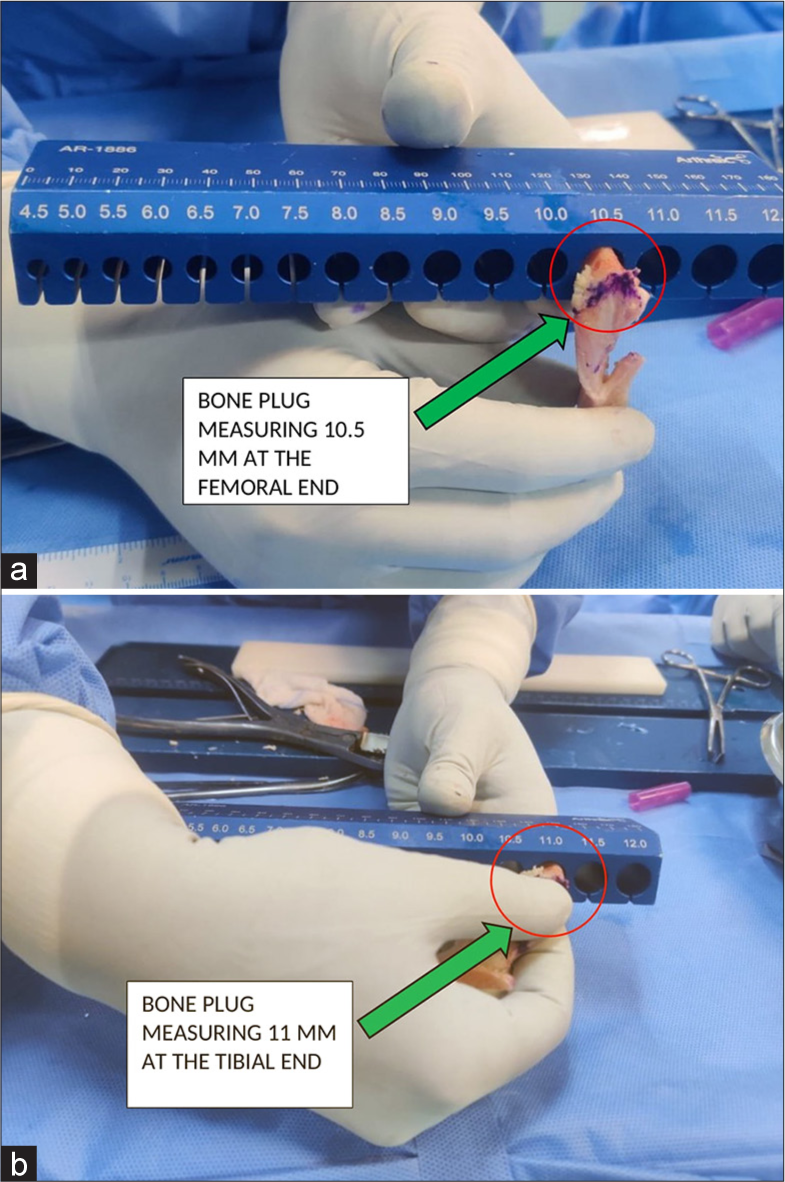
- (a) (green arrow) Bone patellar tendon bone graft measurement of femoral end – 10.5 mm. (b) (green arrow) Bone patellar tendon bone graft measurement of tibial end – 11 mm.
Tunnel preparation
Femoral tunnel
The previous femoral tunnel was identified and found to be in an optimal position, and a plan to ream a femoral tunnel through the inside-out technique was carried out. The knee was brought to a flexed position, and a beath pin was passed through the anteromedial portal into the previous femoral tunnel. The knee was then hyperflexed and the beath pin was advanced through the lateral femoral condyle. Sequential reaming was done with a 4.5 mm Endobutton reamer followed by 6 mm and 10 mm reamers. A femoral tunnel length of 40 mm was calculated, and a shuttle suture was passed with the help of a the beath pin.
Tibial tunnel
A previous tibial tunnel was identified. It was optimally placed. A guide pin was passed through the tunnel, and the accurate location was confirmed. The tibial tunnel was drilled to the appropriate size of the bone plug (11 mm) through an outside-in technique.
High-tibial osteotomy
Standard high-tibial medial opening wedge osteotomy was performed for varus correction of 8 mm to unload the medial compartment of the knee [Figure 7]. Intra-operatively, a 10 mm reamer was placed in the tibial tunnel to avoid screw placement through the tibial tunnel and osteotomy was fixed with a size 1 new clip plate [Figure 8a and b]. During the opening of the medial wedge osteotomy, there occurred a Type 3 Takeuchi lateral hinge fracture which was managed by a percutaneous 6.5 mm cannulated cancellous screw from lateral to medial direction [Figure 9].
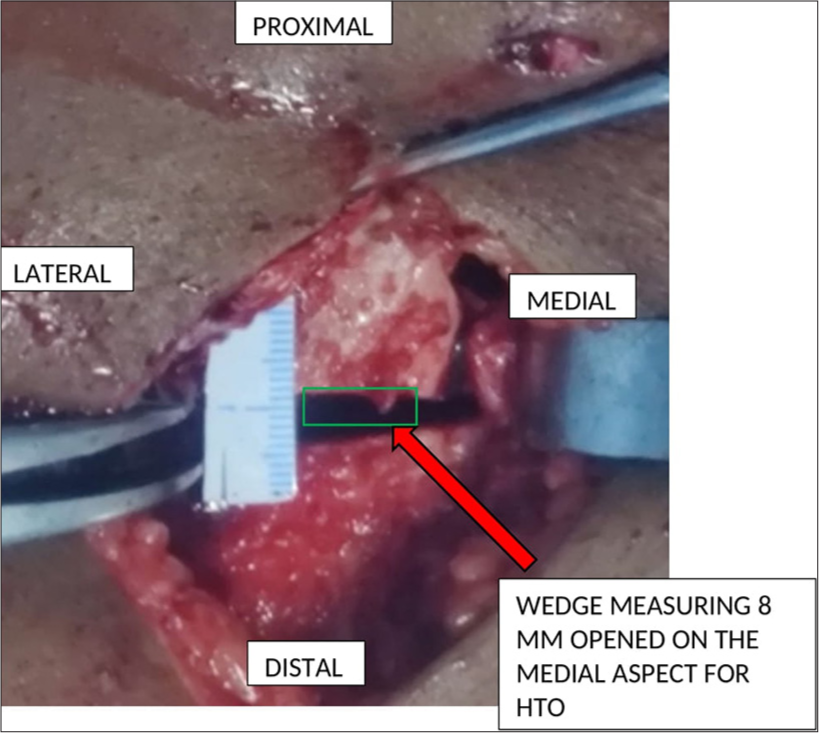
- Showing (red arrow) medial opening wedge osteotomy, correction done according to Miniaci’s method as calculated above.
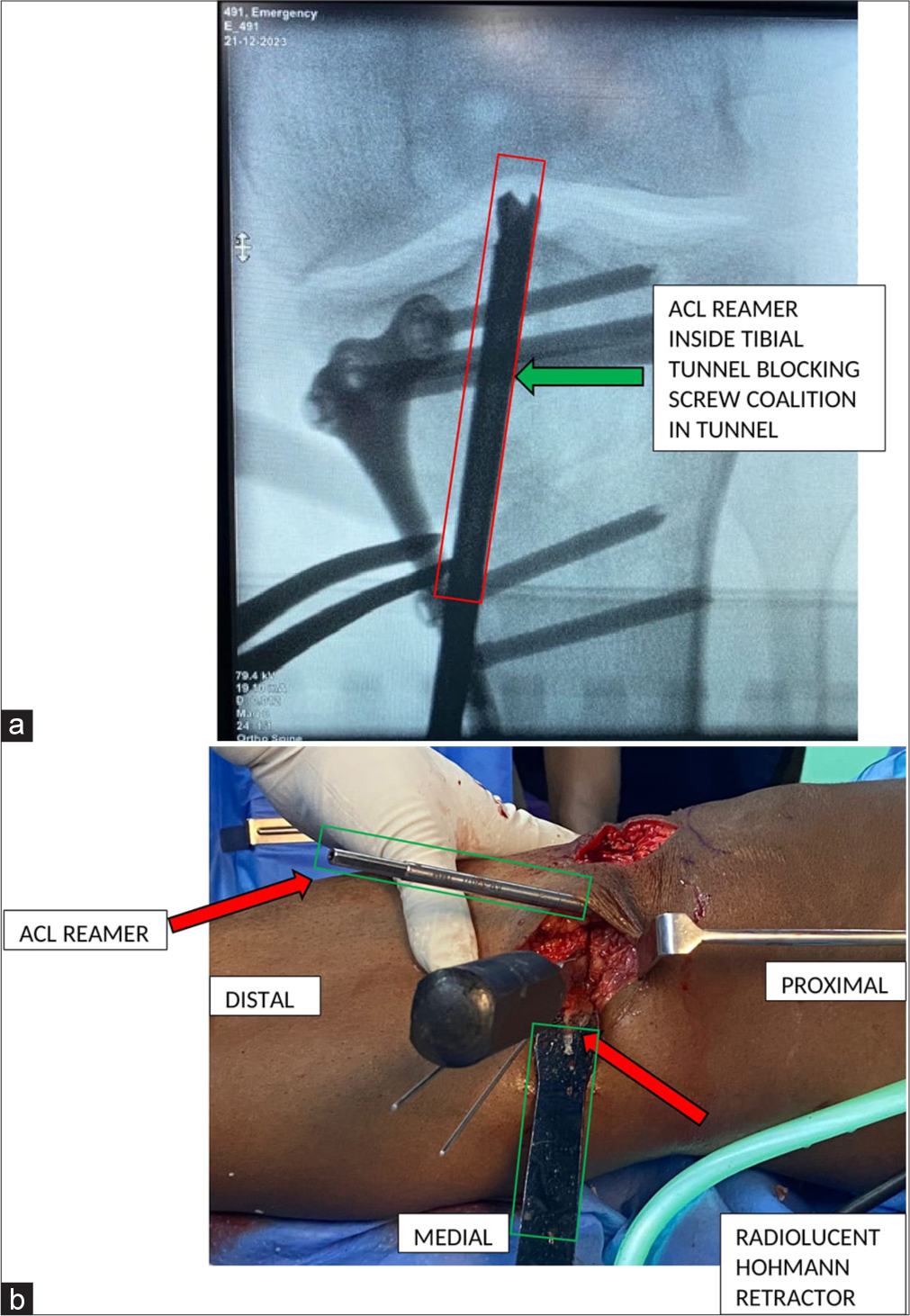
- (a) Showing an intra-operative C arm image demonstrating occlusion of tibial tunnel by placing a (green arrow) 8 mm drill in situ to avoid passage of screws into the tibial tunnel. (b) Showing an intra-operative end on image demonstrating occlusion of tibial tunnel by placing a (red arrow) 8 mm drill in situ to avoid passage of screws into the tibial tunnel.
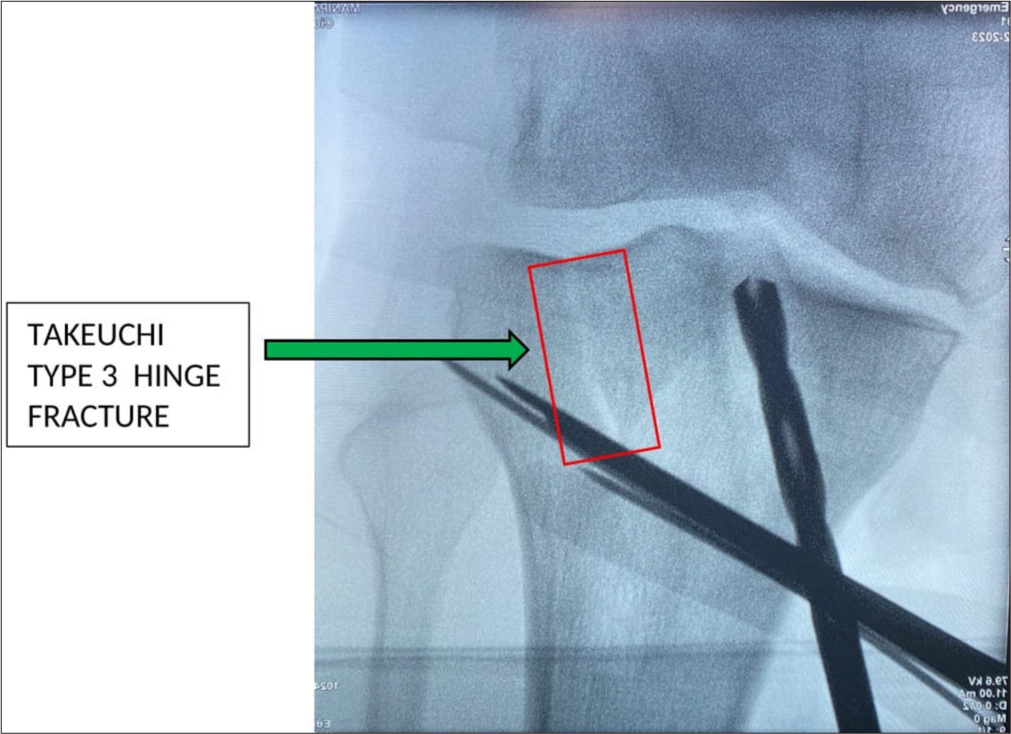
- Showing an intra-operative C arm image demonstrating a Type 3 Takeuchi lateral hinge fracture.
Graft passage
The loop end of the shuttle suture was then retrieved through the tibial tunnel with the help of a grasper. The suture from the tibial tubercle bone plug was passed through the tibial and femoral tunnels with the help of a shuttle suture. The cancellous portion of the graft was placed anteriorly in the femoral tunnel. Once the graft was in the appropriate position in the femoral tunnel, a nitinol wire was placed adjacent to the graft within the anterior aspect of the tunnel. A 7 × 20 bio composite screw was inserted under adequate tension to obtain femoral fixation of the graft. The loop ends of the tight rope (Arthrex) were tied over the lateral end of the femoral tunnel over a standard 14 mm size attachable button system (ABS) button (Arthex).
Sandwich technique
For tibial fixation, as the tunnel was dilated, an allograft was used alongside the BPTB graft (Sandwich technique) to obtain a secure fixation in the tibial tunnel. Using the above sandwich technique, we could obtain a press fit fixation of graft in the tibial tunnel and then a nitinol wire was passed through the tibial tunnel in the anterior aspect of the graft and secured with a screw of size 10 × 30 while the tension was maintained on either side of the graft [Figures 10 and 11]. A pictorial demonstration of the sandwich technique and the post-operative X-ray is shown [Figure 12a and b] [Video].
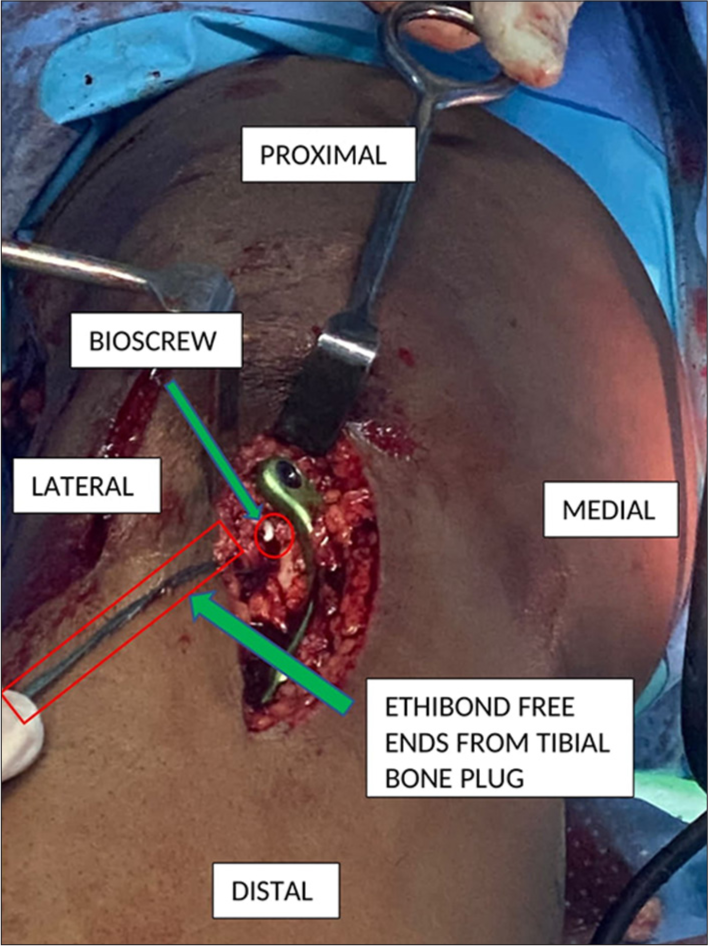
- The “Sandwich” technique where the tibial end of bone patellar tendon bone graft is getting sandwiched between the allograft on the one side and bioscrew on the other side.
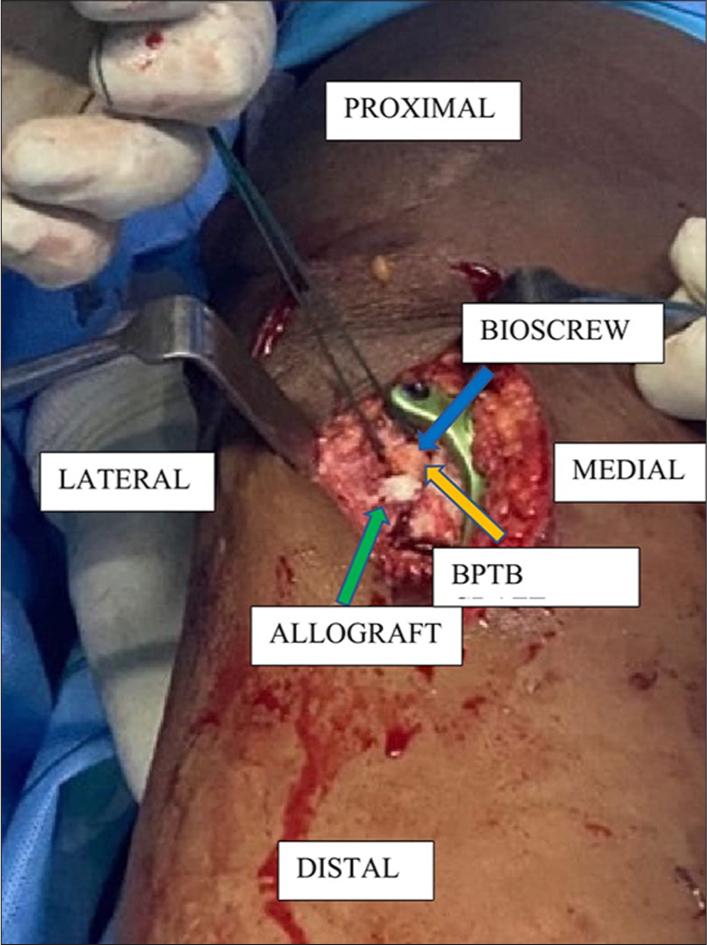
- Demonstration of sandwich technique in sagittal section where the tibial end of (orange arrow) bone patellar tendon bone (BPTB) graft is getting sandwiched between the (green arrow) allograft on the one side and (blue arrow) bioscrew on the other side.
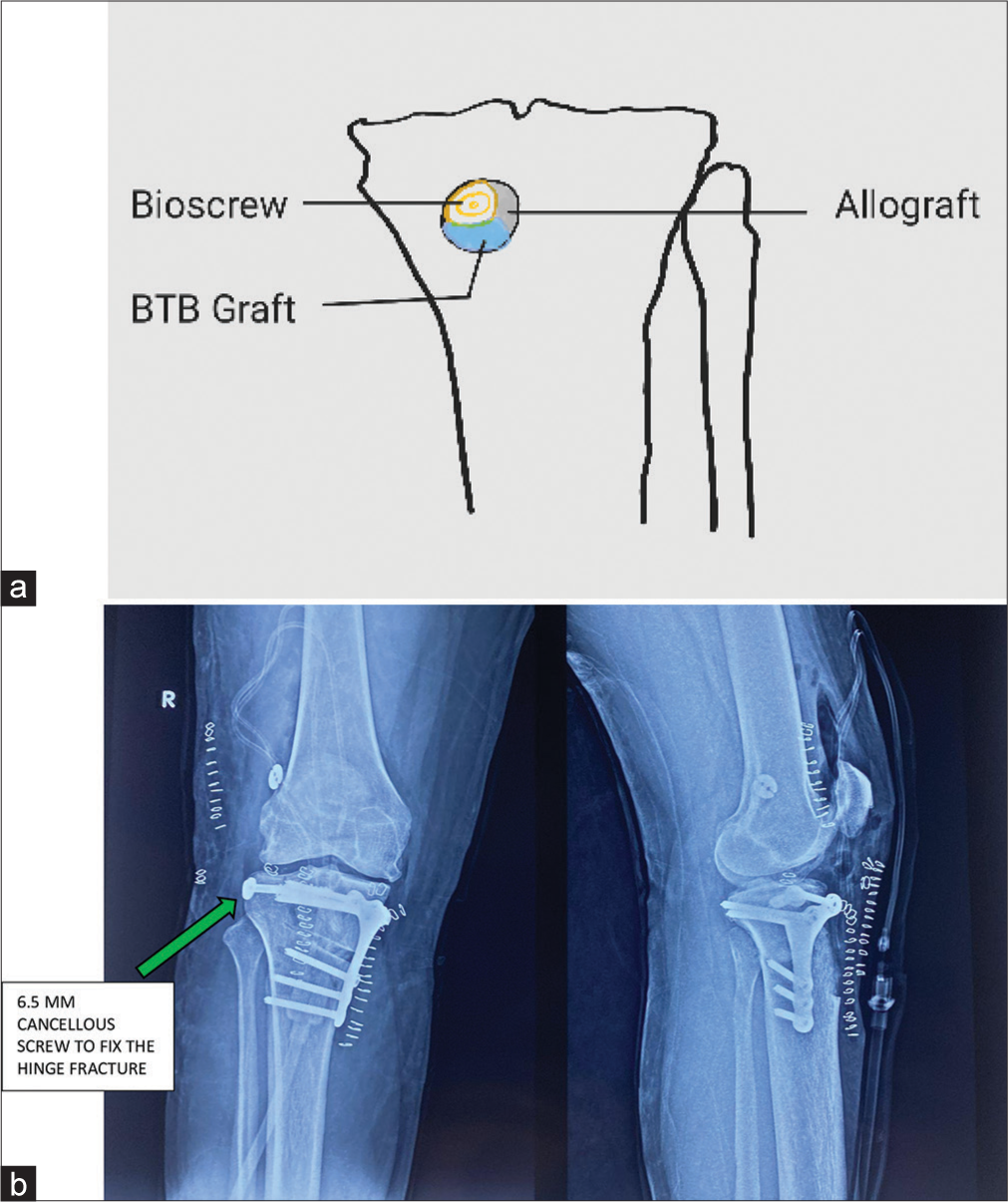
- (a) Pictorial demonstration of sandwich technique in coronal section. (b) Shows immediate post-operative X-ray showing medial wedge high-tibial osteotomy and (green arrow) lateral cancellous screw to fix the hinge fracture.
Follow-up
At a 3-month follow-up, the patient can bear full weight and walk, and has full range of motion with no extension deficit and excellent knee stability [Video]. Follow-up CT scan shows healing osteotomy site and hinge fracture [Video]. Standing scanogram shows neutral alignment with adequate varus correction [Figure 13].

- Standing scanogram at 3-month follow-up shows neutral alignment. Red line from the center of the femoral head to the mid-point of the ankle (mechanical axis) passes just lateral to the mid point of the knee as planned (pre-op varus corrected).
DISCUSSION
Revision ACL-R presents a multifaceted challenge for both knee surgeons and rehabilitation specialists. Achieving a favorable clinical outcome hinges on identifying and addressing all factors predisposing to graft failure, alongside the successful implementation of an anatomically correct and biologically integrated ACL graft. Technical obstacles include managing previous hardware, navigating limited graft options, correcting malpositioned tunnels, addressing tunnel expansion, and managing concurrent meniscal and ligamentous injuries and associated limb alignment issues.[4] The majority of revision ACL-Rs can often be completed in a single-stage procedure. An ideal scenario for this approach involves completely non-anatomic tunnels with minimal dilation. In situations where there are anatomically positioned but dilated tunnels, additional considerations come into play. Utilizing an outside-in drilling technique for the femur and altering the trajectory as needed can help achieve healthy bone within the tunnel walls while still maintaining the anatomical insertion site. In general, tunnel dilatation up to 14-16 mm can be managed effectively in a one-stage surgery, particularly when the tunnel locations are close to anatomical positions.[5,6]
In the present case, the tibial tunnel was anatomically positioned with a diameter of 20.5 mm, quite higher than the critical limit as proposed for a single-stage revision. Furthermore, in this case, there was a varus deformity in the knee of 8°, which was tackled with a medial opening wedge high-tibial osteotomy. Correction of varus deformity by high-tibial osteotomy was necessary to unload the medial compartment of the knee and to halt the progress of osteoarthritis in the medial compartment, which is usually the natural course in an ACL-deficient knee.
The concept of a sandwich technique, which involves bone grafting in the dilated tibial tunnel and sandwiching the BPTB graft between the allograft and the inner aspect of the tibial tunnel, is a novel technique which cuts down the need for a second surgery and a faster recovery and early return to sports which was a primary concern in two-stage revision.
Limitations of sandwich technique for revision ACL-R
Longer duration of surgery
Proper patient selection as the procedure can be done only for previously correctly placed dilated tunnels
When an additional procedure like the above high tibial osteotomy (HTO) was included and chances of iatrogenic fracture and improper placement of screw through the plate into the ACL tunnel
Short-term follow-up (3 months).
CONCLUSION
The current technique entails a simple and organized management technique to address each of the lacunae from the index surgery , thus, providing predictable outcomes. Managing and treating beyond the conventional remains the crux when handling such complicated revision scenarios.
Author contributions
CT and DP: Concepts, design, manuscript preparation, and manuscript editing and review; SS: Manuscript preparation, manuscript editing and review, and data analysis; DS: Manuscript preparation, manuscript editing and review, and statistical analysis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Revision ACL reconstruction: Principles and practice. Indian J Orthop. 2021;55:263-75.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and outcome after revision anterior cruciate ligament reconstruction: Results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40:1551-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction: Why do failures occur? Instr Course Lect. 1995;44:391-406.
- [Google Scholar]
- Revision anterior cruciate ligament reconstruction. Sports Health. 2014;6:504-18.
- [CrossRef] [PubMed] [Google Scholar]
- Technical considerations in revision anterior cruciate ligament (ACL) reconstruction for operative techniques in orthopaedics. Oper Tech Orthop. 2017;27:63-9.
- [CrossRef] [PubMed] [Google Scholar]
- Tunnel widening in revision anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2010;18:695-706.
- [CrossRef] [PubMed] [Google Scholar]







