Translate this page into:
Clinical outcomes of primary anterior cruciate ligament reconstruction using six-strand hamstring autograft
*Corresponding author: Hardik Dodiya, Department of Pharmacology, Lallubhai Motilal College of Pharmacy, Ahmedabad, Gujarat, India. hardikdodiya15@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shah N, Dodiya H, Damor R, Pachore J. Clinical outcomes of primary anterior cruciate ligament reconstruction using six-strand hamstring autograft. J Arthrosc Surg Sports Med. 2024;5:24-31. doi: 10.25259/JASSM_1_2024
Abstract
Objectives:
Quadrupled and five-strand hamstring tendon (HT) autografts are commonly used in anterior cruciate ligament reconstruction (ACLR), but there is significant variability in graft diameter. The six-strand HT autograft has been introduced to increase graft diameter in patients with undersized HT grafts and may achieve better clinical outcomes. None of the studies has reported clinical outcomes following this technique in Indian patients. We investigated clinical outcomes in patients who underwent primary ACLR using a six-strand HT autograft technique with a minimum six-month follow-up.
Materials and Methods:
Fifty-five patients who underwent primary ACLR using six-strand HT autografts with interference screw fixation were included in the study. These patients were followed up at three and six months for the evaluation of clinical outcomes. Subjective evaluations included the TegnerLysholm score, anterior cruciate ligament-quality-of-life (ACL-QOL) score, and International Knee Documentation Committee (IKDC) subjective score. Laxity assessments of the knees were performed using the Lachman test and the pivot-shift test. Functional evaluation of the patients was performed with an overall IKDC objective score.
Results:
The mean IKDC subjective score was significantly improved at three-month (63.42 ± 5.38) and six-month (82.82 ± 7.49) follow-up after surgery (P < 0.05) when compared with pre-operative scores (50.55 ± 1.84). A similar finding was also noted with the Tegner-Lysholm score and ACL-QOL score in our study. All patients have achieved normal to near-normal functional outcomes at six months in our study without any major complications. The most commonly found complication was paresthesia (21.80%) in the present study.
Conclusion:
In the primary ACLR, six-strand hamstring autograft achieves similar clinical outcomes and complications as reported with four-strand or five-strand HT autografts. However, the percentages of patients who achieved normal to near-normal outcomes were higher in the present study (100%) as compared to earlier reported data using four-strand or five-strand HT autografts (~85%). The six-strand graft technique is a useful means of increasing graft diameter when faced with an undersized hamstring graft.
Keywords
Anterior cruciate ligament reconstruction
Six-strand hamstring autograft
International knee documentation committee score
Clinical outcomes
INTRODUCTION
One of the most common knee ailments is anterior cruciate ligament (ACL) damage, which was reported 86.5% of the knee injuries in India.[1] The common and frequent cause of ACL tears is an injury sustained during sports.[2] Over 2 million ACL injuries occur around the world every year and are also found more prevalent in young female athletes.[3,4] ACL reconstruction (ACLR) has been recognized as the standard surgical procedure to achieve good clinical outcomes.[5] ACLR also produces an early return to sports activity. Surgical techniques have improved over the years to achieve better clinical outcomes in ACL injury patients.[6] Numerous variables, such as graft category, graft fixation techniques, tunnel parameters, graft diameter, and rehabilitation protocol, influence the clinical outcomes following ACLR.[7]
There are various graft options that exist for ACLR, such as bone-patellar tendon-bone (BPTB) autograft, hamstring tendon (HT) autograft, quadriceps tendon autograft, and allograft tissue.[8] Previously, BPTB was the most commonly used graft for ACLR but was also associated with loss of extensor mechanism, patellar fracture, anterior knee pain, and patella infera which forced the orthopedician to do the surgery using HT autograft which tended to evolve toward greater residual laxity.[9] Some of the most often used graft materials are semitendinosus and gracilis, which have good clinical results following ACLR.[10-12] However, ACLRs with smaller diameter HT grafts are also associated with an enhanced probability of re-surgery or worse clinical outcomes. There are two methods to enlarge the size of the autograft: (a) allograft augmentation or (b) multiple folds of the graft to produce a five or six-strand graft. Research has demonstrated that allograft augmentation for hamstring ACLR has higher re-rupture rates than autograft alone, which has led to a greater focus on five and six-strand HT autograft methods. In the five and six-strand hamstring autograft techniques, the semitendinosus and/or gracilis tendons are tripled over to produce the extra strand(s). It has been observed that this method increases the graft diameter by more than 1 mm.[1]
There are no studies that have assessed the clinical results of six-strand HT autograft in Indian patients who underwent ACLR. We hypothesized that our patients who underwent ACLR using six-strand HT autograft would demonstrate excellent knee outcome scores and have better stability.
MATERIALS AND METHODS
Study center
This study was conducted at a multispecialty hospital. Study documents, including study protocol, have been approved by the Institutional Ethics Committee (IEC). Good Clinical Practice (GCP) guidelines, the Declaration of Helsinki and its later revisions, and other relevant local regulatory guidelines were followed during the study’s execution.[13-15]
The participants were allowed to withdraw from the study at any time voluntarily.
Study patients
We have conducted a single-center, assessor-blind, and prospective clinical study at a multispecialty hospital. In this study, we have included participants older than 18 years who underwent ACLR using a six-strand hamstring (semitendinosus and gracilis) autologous graft. The patients who met exclusion criteria were not randomized in the study such as ACLR using other than six-strand hamstring (semitendinosus and gracilis) autologous graft, multiligamentous injury, previous ACLR repair, revision of ACLR, injury to posterolateral corner, and contralateral ACL injury/reconstruction. Sixty-eight patients were screened for participation in the study. After a thorough evaluation of patients, 55 patients met the eligibility criteria in the present study. Before beginning any study-related activities or procedures, an informed consent form was signed by each patient and their duly authorized representatives. Patients’ information was collected, including contact information, demographic information, the amount of time that had passed between the injury and surgery, the diameter of the graft, the cause of the ACL tear, the status of any related meniscal and collateral ligament injuries, and information about the surgical procedures and complications. Study participants were followed up at three months and six months.
Pre-operative evaluation
All the patients underwent routine pre-operative blood investigations, routine urine analysis, radiographic investigations, electrocardiogram, and 2D echocardiography.
Surgical procedure
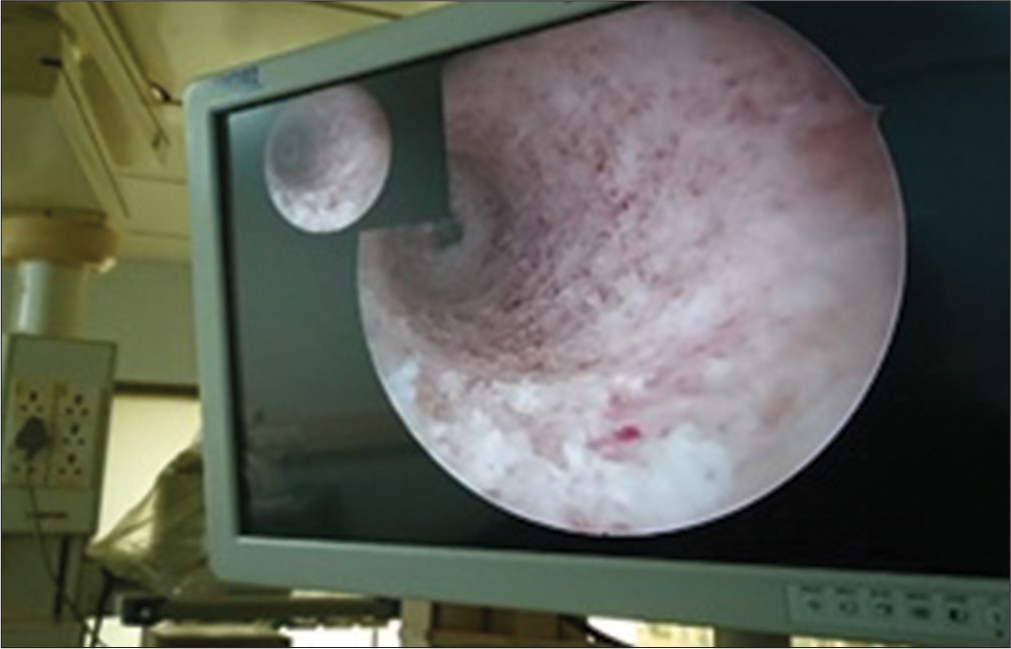
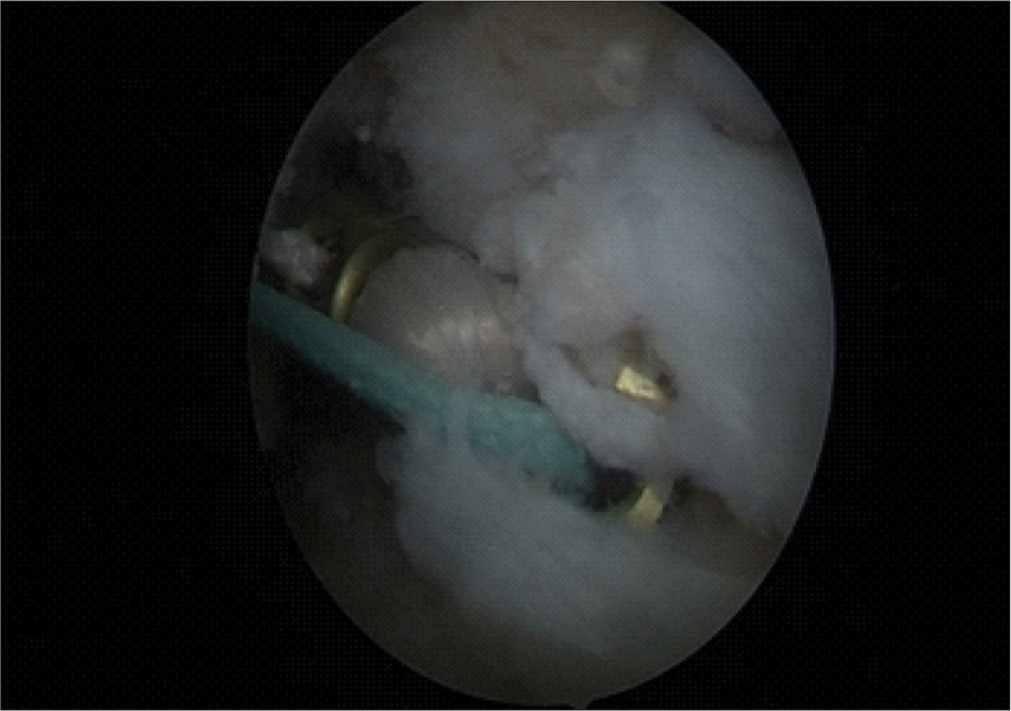
Surgery was performed under spinal anesthesia in a supine position. Standard anteromedial and anterolateral portals were taken, and the intraarticular collection was evacuated. The diagnostic knee arthroscopy was performed without a tourniquet to confirm magnetic resonance imaging report findings and clinical diagnosis [Figure 1]. All grafts were obtained by a single orthopedic surgeon who was an expert in HT graft harvesting. A 3-centimeter oblique incision was made centered over the pes anserine tendon insertion to harvest the HTs in a conventional manner. After separating the distal ends of the gracilis and semitendinosus tendons, the closed tendon stripping tool was used to harvest them. Each tendon of gracilis and semitendinosus was sutured independently. Then, semitendinosus was cut to size as per gracilis length. Then, both grafts were triplicated together [Figure 2]. All measurements were taken following the blunt removal of the fat and muscle that was attached. However, this procedure was finished before any additional post-harvest modifications or graft trimming. Krackow whip stitches were used to loop both tendons to make a six-stranded graft [Figure 3]. Femoral and tibial tunnels were selected to make press fit graft thickness [Figure 4]. Using the inside-out technique, the knee was high flexed, and with a femoral aimer, the femoral tunnel was drilled sequentially using first the guide pin, then the EndoButton drill, and finally the flower tip drill to the predetermined length. The femoral tunnel was made at the 10 o’clock to 11 o’clock position on the right side and 2 o’clock to 1 o’clock position on the left side, just anterior to the posterior condylar ridge. The average length of the femoral tunnel was 35-40 mm [Figure 5]. The tibial tunnel was drilled using a jig with a pre-determined angle of 55°. The point of insertion was negotiated at the intersection of the anterior tibial spine and the anterior root of the lateral meniscus intersection. Subsequently, the graft was passed and secured at the femoral end by confirmed average 20 mm EndoButton positioning [Figures 6 and 7]. While maintaining the graft tension, the knee was cycled several times to avoid any kinks. The tibial end of the graft was seated and secured with a 1 mm oversized polyetheretherketone interference screw with maintaining the knee in posterior 30° flexion and applying posterior drawer force. Afterward, the knee was fully extended and observed for notching. If notches were noted, notchplasty was performed. Afterward, the knee was taken through a full range of motion (ROM). The harvest site was closed in layers followed by the closure of portals. Sterile dressing was performed, and the leg was braced in a long-extension knee brace. All patients were treated with an antibiotic (intravenously, cefazolin injection 2 g, 1 h before surgery and 1 g 8 hourly for 48 h post-surgery). After 48-h post-surgery, patients were prescribed oral antibiotics and analgesics for five days. On the 14th post-operative day, the sutures were taken out.
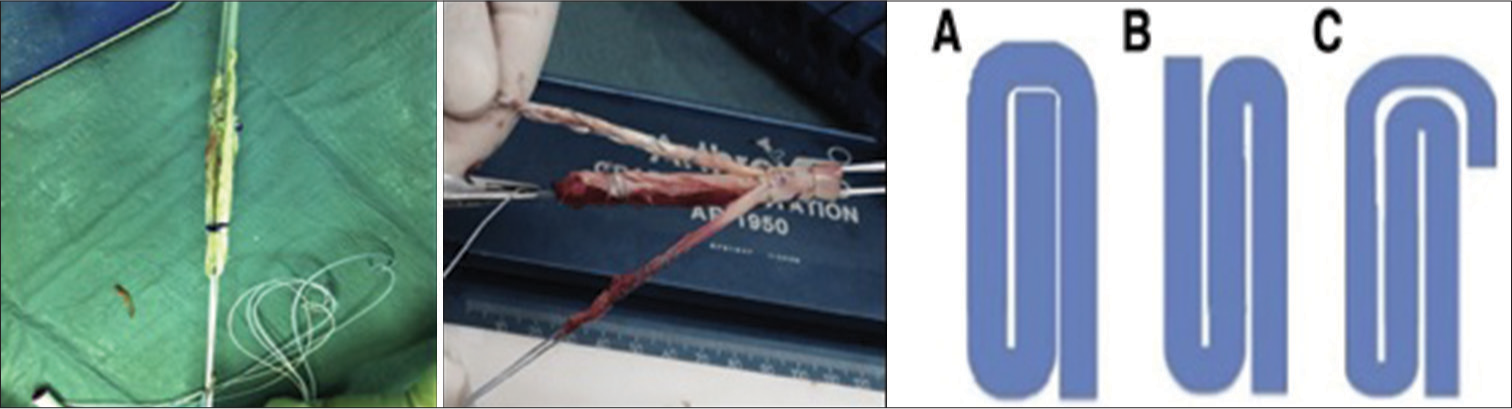
- Six-strand autograft and different configurations for tripling (Option A or Option B or Option C).
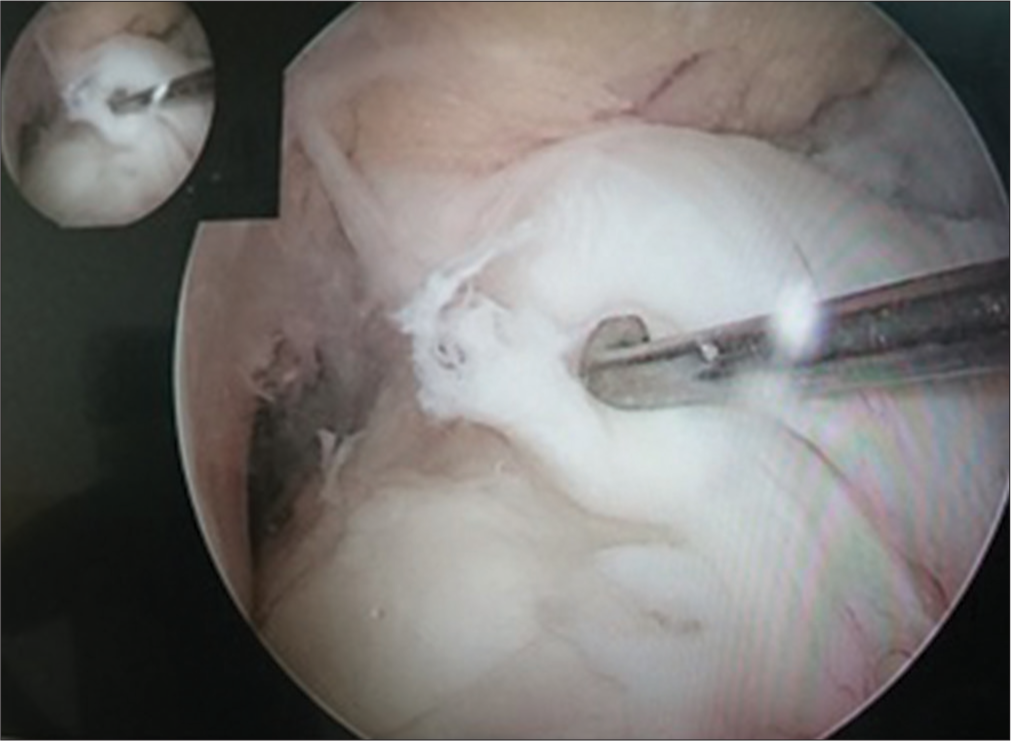
- Anterior cruciate ligament knee laxity assessments.
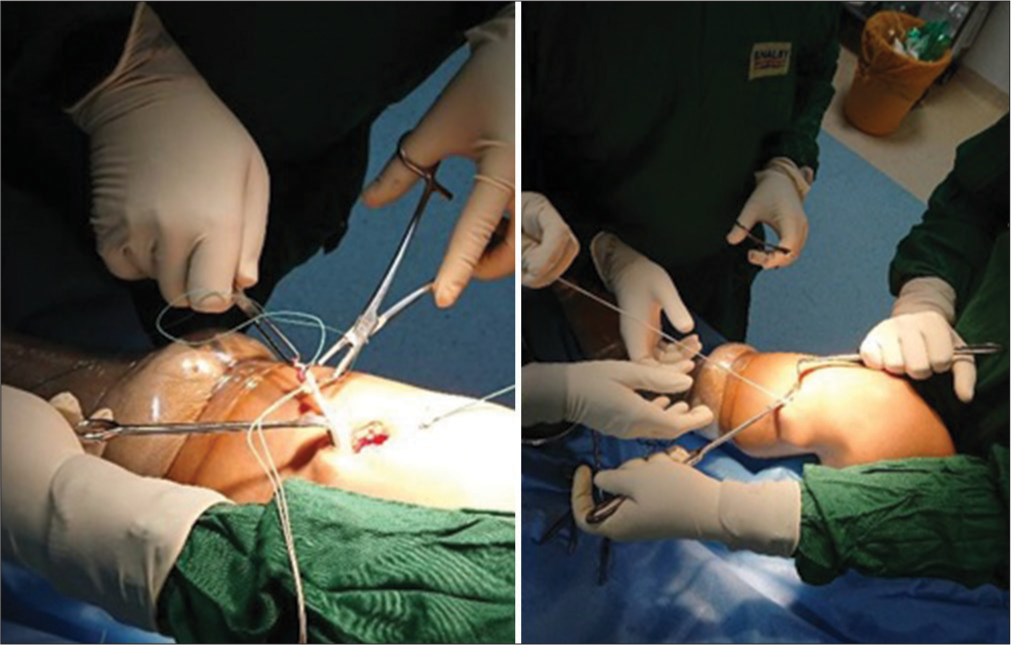
- Graft harvesting.
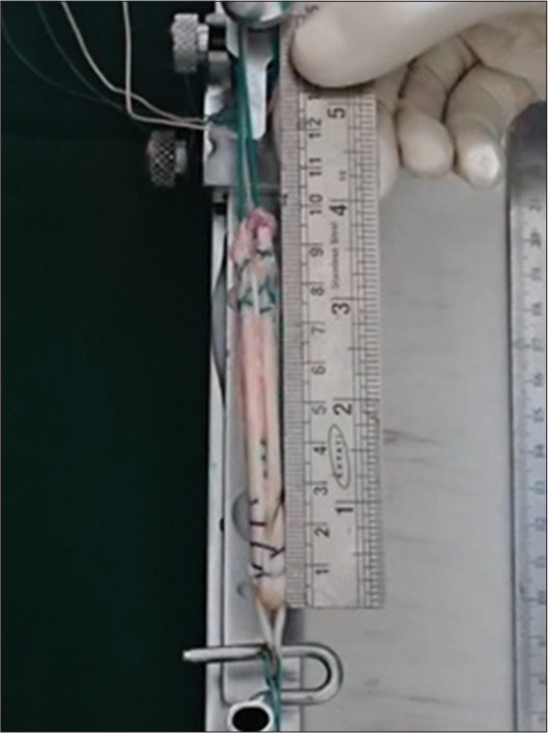
- Graft pretension and final length.
- Anteromedial portal view of femoral tunnel.

- Femoral tunnel length.
- Scope view of endobutton passage.
Post-operative rehabilitation protocol
Beginning on the 1st day following surgery, post-operative rehabilitation was planned based on the outcome of the meniscal procedure. The patient was instructed to perform hamstring stretches, ankle pumps, and quadriceps strengthening exercises on the 1st post-operative day. The patient was instructed to perform a progressive ROM with the goal of reaching 120° in six weeks if meniscus repair was not necessary. In addition, weight-bearing (as tolerated) was suggested. On the other hand, if the patient had meniscal repair, knee ROM and weight-bearing were prohibited for six weeks. It has been suggested that patients can use crutches or canes to walk. Such assistive devices continued until the gait became normal. Education on balance and proprioception began as soon as the gait stabilized. Patients were instructed to resume running, jogging, and household chores after three months and then resume farming, agriculture, other jobs, and sports after 12 months.
Clinical evaluation
Pre-operative and post-operative clinical evaluations were conducted at three-month and six-month intervals. A blinded orthopedic surgeon conducted all of the clinical evaluations to reduce the possibility of bias. Both subjective and objective evaluations were part of the clinical evaluation. For both the subjective and objective evaluations, the International Knee Documentation Committee (IKDC) form was utilized.[16] Further, subjective evaluation was also performed using the Tegner-Lysholm score (excellent [>90], good [84–90], fair [65–83], and poor [<65]).[17] The Lachman and pivot-shift tests were used to measure the laxity of the knees.[18] The objective evaluation was performed using an overall IKDC score. Patients were also evaluated using ACL-quality-of-life (ACL-QOL) questionnaires.[19] The ACL-QOL has been translated from English into Hindi and Gujarati language by native translators fluent in Hindi and Gujarati, respectively. The translations have been performed by an authorized translation agency. These documents were back-translated into English by an authorized translation agency. The original and translated documents were reviewed and approved by the IEC. The 31 questions in the ACL-QQL are broken down into five domains: Physical complaints and symptoms, work-related issues, leisure activities and competitive sports, lifestyle, and social and emotional aspects. Every question has a score between 0 and 100. A higher score denotes a higher standard of living.[19] According to IKDC recommendations, follow-up visits were made to operated knees to evaluate osteoarthritic changes in weight-bearing AP, lateral, and skyline views. The results were rated as normal (≥90 score), near-normal (80–89 score), abnormal (70–79 score), and severely abnormal (<70 score).
Sample size determination
In the previous studies, the reported mean IKDC subjective score was 81.8 at a six-month follow-up period.[20] In the present study, assuming a mean IKDC score of 88 at a six-month follow-up period, a standard deviation (SD) of 10.6 (as per reported earlier data), a two-sided significance level of 5%, a power of 80%, and a drop-out rate of 10%, a total sample size of 55 was estimated.
Statistical analysis
Categorical variables had been mentioned as number (percentage), and continuous variables had been mentioned as mean (±SD). Categorical variables were analyzed using the Chi-square test and Fischer’s exact test, whereas continuous variables were analyzed using an independent t-test (two-tailed). A one-way analysis of variance was used to compare IKDC subjective scores, Tegner-Lysholm score, ACL-QOL scores, and overall IKDC objective score from baseline (before surgery) to each follow-up after surgery. P < 0.05 was considered statistically significant. The Statistical Package for the Social Sciences (SPSS) Statistic Version 19.0 (IBM Co.) was used to perform statistical analysis.
RESULTS
Baseline characteristics
A total of 55 participants were enrolled to participate in the study. Forty-five participants were male, and ten patients were female, with a mean age of 31 years. The average body mass index of study participants was 27.5 kg/m2. Twenty-nine patients had right ACL tear, whereas 26 patients had left ACL tear. The major cause of ACL tear was road traffic accidents (63.60%) in our study. In the present study, associated meniscal injuries were lateral (38.20%) and medial (25.35%), whereas 10.90% of patients had both (lateral and medial) meniscal injuries. The majority of the study participants underwent partial meniscectomy (67.27%) for the meniscal injury. The details of patient characteristics are described in Table 1.
| Parameters | Value |
|---|---|
| Age, year, mean±SD (range) | 31.1±10.2 |
| Body mass index, kg/m2, mean±SD | 27.50±4.39 |
| Mean time to surgery after injury, months, mean (range) | 5.30 (1–24) |
| Graft diameter, mm, mean±SD | 8.27±0.53 |
| Graft length, cm, mean±SD | 8.12±0.59 |
| Gender, n(%) | |
| Male | 45 (82.00) |
| Female | 10 (18.00) |
| Side of injury, n(%) | |
| Right | 29 (52.80) |
| Left | 26 (47.20) |
| Etiology, n(%) | |
| Sports injury | 5 (9.10) |
| Road traffic accident | 35 (63.60) |
| Work (household/farm) | 15 (27.30) |
| Associated meniscal injury, n(%) | |
| Both menisci | 6 (10.90) |
| Medial meniscus | 14 (25.45) |
| Lateral meniscus | 21 (38.20) |
| None | 14 (25.45) |
| Meniscal procedure, n(%) | |
| None | 16 (29.10) |
| Meniscal repair | 2 (3.63) |
| Partial meniscectomy | 37 (67.27) |
SD: Standard deviation
Clinical outcomes
Knee laxity assessment by Lachman test and pivot-shift test revealed grade 2 ACL tear (58.20% and 63.60%) before surgery. In our study, pre-operative IKDC, Tegner-Lysholm, and ACL-QOL mean scores were 50.55, 57.84, and 463.82, respectively. These scores were statistically increased at three months (63.42, 67.50, and 1731.64) and six months (82.82, 86.26, and 2755.64) follow-up periods, respectively (P < 0.05). Overall, the IKDC score was also statistically improved at six months follow-up in our study participants (P < 0.001). Forty-five patients had near-normal IKDC scores, whereas 10 patients had normal IKDC scores after six months of the surgery. The details of laxity assessment [Table 2], subjective scores [Table 3], and overall IKDC score [Table 4] were summarized in tabular format.
| Parameters | Grade | n(%) |
|---|---|---|
| Lachman test | 0 | 0 (0) |
| 1 | 10 (18.20) | |
| 2 | 32 (58.20) | |
| 3 | 13 (23.60) | |
| Pivot-shift test | 0 | 0 (0) |
| 1 | 9 (16.40) | |
| 2 | 35 (63.60) | |
| 3 | 11 (20.00) |
| Parameters | Before surgery | Follow-up period | P-value | |
|---|---|---|---|---|
| 3-month | 6-month | |||
| IKDC score | 50.55±1.84 | 63.42±5.38 | 82.82±7.49 | <0.001* |
| Tegner-Lysholm score | 57.84±2.09 | 67.50±6.38 | 86.26±7.12 | <0.001* |
| ACL-QOL score | 463.82±153.82 | 1731.64±176.98 | 2755.64±223.68 | 0.020* |
IKDC: International knee documentation committee, ACL-QOL: Anterior cruciate ligament-quality of life *Statistically significant difference exists between pre-operative scores and post-operative scores
| Parameters | Grade | Before surgery n(%) | Follow-up period | P-value | |
|---|---|---|---|---|---|
| 3-month n(%) | 6-month n (%) | ||||
| Overall IKDC score | Normal (A) | 0 (0) | 0 (0) | 10 (18.20) | <0.001* |
| Near-normal (B) | 0 (0) | 20 (36.40) | 45 (81.80) | ||
| Abnormal (C) | 0 (0) | 35 (63.60) | 0 (0) | ||
| Severely abnormal (D) | 55 (100) | 0 (0) | 0 (0) |
IKDC: International knee documentation committee. *Statistically significant difference exists between pre-operative scores and post-operative scores
Complications
Table 5 summarizes the complications that occurred at the six-month follow-up in the study. There were 12 cases of paresthesia (21.80%), six cases of hardware prominence (10.90%), four cases of superficial infection (7.27%), three cases of hemarthrosis (5.45%), and two cases of knee effusion (3.63%).
| Complications | n (%) |
|---|---|
| Superficial infection | 4 (7.27) |
| Knee effusion | 2 (3.63) |
| Hemarthrosis | 3 (5.45) |
| Hardware prominence | 6 (10.90) |
| Paresthesia | 12 (21.80) |
DISCUSSION
In the present study, we evaluated clinical outcomes in patients who underwent ACLR using a six-strand HT autograft. There are several factors that affect the clinical outcome following ACLR. However, surgical techniques such as graft material and graft configuration, and rehabilitation protocol are important factors for obtaining better clinical outcomes following ACLR.[7] As per recent literature, none of the single surgical methods have been accepted as superior when compared with other surgical options.[21] ACLR using hamstring autograft has been used in clinical practice for many years.[22] To the best of our knowledge, no research has yet examined the clinical and functional results in Indian patients undergoing ACLR surgery utilizing the six-stranded semitendinosus (ST) and gracilis (G) autologous graft technique.
In our study, IKDC subjective score was significantly improved at three months (63.42 ± 5.38) and six months (82.82 ± 7.49) follow-up when compared with pre-operative scores (50.55 ± 1.84). In a previous study of ACLR using fourfold hamstring autograft, the mean IKDC subjective score after a six-month follow-up was 82.16.[23] Further, Singh and Singh also reported IKDC subjective score of 79.02 ± 1.30 at six months follow-up after performing ACLR using a four-stranded hamstring graft.[24] Abdul et al. reported IKDC subjective score at 12 months was 76.3 ± 20.1 after ACLR using the TransLateral.[25] Calvo et al. also reported a mean post-operative IKDC subjective score of 96.8 (range 82–100) after at least a two-year follow-up in participants operated on for ACLR utilizing a five-strand hamstring autograft.[26] Our study also showed greater improvement in Tegner-Lysholm score at three-month (67.50 ± 6.38) and six-month (86.26 ± 7.12) follow-up as compared to pre-operative score (57.84 ± 2.09). Sherchan et al. also reported a Tegner-Lysholm score of 88.26 ± 8.53 (urban patients) and 84.82 ± 8.53 (rural patients) after 24 months of doing primary ACLR using the HT.[27] In another study utilizing HT graft, the reported average Tegner-Lysholm score was 88.37 at the six-month follow-up.[23] Moreover, the reported mean Tegner-Lysholm score was 97.1 (80–100) after a minimum of two years of follow-up in patients who underwent ACLR using the five-strand hamstring autograft technique.[26] Therefore, our study findings of the IKDC subjective score and Tegner-Lysholm score were in line with the previously reported data of the IKDC subjective score and Tegner-Lysholm score in participants who underwent ACLR using either four-strand hamstring autograft technique or five-strand hamstring autograft technique. No significant difference was reported with respect to the IKDC subjective score and Tegner-Lysholm score using the six-strand HT autologous graft technique for ACLR surgery.
The ACL-QOL score is one of those final results that have previously been shown to be valid, responsive, and reliable in adult populations. It remains the only (PROM) patient-reported outcome measure for quality of life in ACL deficient patients and ACLR patients.[28] In the present study, ACL-QOL score was statistically increased (P = 0.020) at three-month (1731.64 ± 176.98) and six-month (2755.64 ± 223.68) follow-up when compared with pre-operative scores (463.82 ± 153.82). Heard et al. reported that mean post-operative ACL-QOL scores were 515 at six months (n = 446), 673 at 12 months (n = 280), and 815 at 24 months (n = 100).[19] Similarly, Abdul et al. also reported statistically significant improvement in knee injury and osteoarthritis outcome score (KOOS)-QoL (Knee Injury and Osteoarthritis Outcome Score-Quality of Life) score after surgery (average score difference; 39.20 ± 25.60) using the TransLateral (single tendon autograft) technique at minimum one year follow-up period.[25] Further, Singh and Singh also showed significant improvement in post-operative KOOS score (83.22 ± 2.26) when compared with pre-operative score (38.58 ± 1.65) in patients who underwent ACLR using hamstring graft and structural rehabilitation.[24] Our results showed abnormal overall IKDC scores in 63.60% of patients at three months, and none of the patients had abnormal overall IKDC scores at six months. At six months, 81.80% of patients had near-normal overall IKDC scores, and 18.20% of patients had a normal IKDC score. In the previous studies, the reported normal to near-normal IKDC overall score was 85.5%, 79.6%, and 85%, respectively.[23,29-31] In contrast to published results, our study showed a 100% normal to near-normal IKDC overall score at a six-month follow-up period. In the present study, we observed 12 cases of paresthesia (21.80%), six cases of hardware prominence (10.90%), four cases of superficial infection (7.27%), three cases of hemarthrosis (5.45%), and two cases of knee effusion (3.63%). The reported complications were also in line with the reported complications in the previous studies.[24,25,27] The present study did not report any new complications.
Limitations
We have calculated the sample size considering a power of 80% in the present study. However, considering 90% power with a larger sample size can be useful to achieve better clinical outcomes using a six-strand HT autograft as compared to a four-strand or five-strand HT autograft. The present study has no surgical comparator arm. Hence, we cannot perform a head-to-head comparison of clinical outcomes after the respective surgical procedures in our study. Moreover, we can also add more subjective parameters and objective parameters (such as KT1000 or KT2000) to evaluate clinical outcomes after ACLR using the six-strand HT autograft. In addition, the follow-up period was restricted to six months and can be extended to two years in future studies.
CONCLUSION
The six-strand hamstring autograft achieves comparable clinical outcomes and complications as reported with four-strand or five-strand hamstring autograft in primary ACLR patients. However, the percentages of patients who achieved normal to near-normal outcomes were higher in the present study (100%) as compared to earlier reported data (~85%), indicating the validity of our assumed hypothesis. In the event that the hamstring graft is undersized, the six-strand HT graft technique is another helpful method for boosting graft diameter. Increased graft diameter may improve subjective outcomes and reduce revision rates. However, large-scale studies are advised to confirm the routine use of a six-strand hamstring autograft to achieve excellent clinical and functional outcomes after primary ACLR when compared with conventional four-strand or five-strand hamstring autograft.
Ethical approval
This research/study was approved by the Institutional Ethics Committee of Shalby Hospital (Reference number: ECR/711/INST/GJ/2015 dated 07 May 2018).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Epidemiological profile of sports-related knee injuries in northern India: An observational study at a tertiary care centre. J Clin Orthop Trauma. 2016;7:207-11.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament knee injuries In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022.
- [Google Scholar]
- Functional outcomes of anterior cruciate ligament reconstruction with tibialis anterior allograft. Bull Hosp Jt Dis. 2013;71:138-43.
- [Google Scholar]
- The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med. 2000;28:98-102.
- [CrossRef] [PubMed] [Google Scholar]
- Does anterior cruciate ligament reconstruction prevent or initiate knee osteoarthritis?-A critical review. J Arthrosc Jt Surg. 2019;6:133-6.
- [CrossRef] [Google Scholar]
- Large-diameter anterior cruciate ligament reconstruction technique with 8-strand semitendinosus and gracilis graft. Arthrosc Tech. 2021;10:e981-6.
- [CrossRef] [PubMed] [Google Scholar]
- Initial graft tension and the effect on postoperative patient functional outcomes in anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:934-41.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament graft choices. Sports Health. 2012;4:63-8.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcome after arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft-A prospective analysis. J Dent Med Sci. 2021;20:27-39.
- [Google Scholar]
- Patellar tendon versus 4-strand semitendinosus and gracilis autografts for anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials with mid-to long-term follow-up. Arthroscopy. 2020;36:2279-291.e8.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: An 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39:2161-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction with 4-strand hamstring tendon construct may be biomechanically superior to 5-strand hamstring tendon construct when using femoral suspensory fixation. Arthrosc Sports Med Rehabil. 2022;4:e1097-102.
- [CrossRef] [PubMed] [Google Scholar]
- World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191-4.
- [CrossRef] [PubMed] [Google Scholar]
- Integrated addendum to ICH E6 (R1): Guideline for good clinical practice E6 (R2), Vol. 2. Current Step 4 Version 2015:1-60.
- [Google Scholar]
- National ethical guidelines for biomedical and health research involving human participants New Delhi: Indian Council of Medical Research; 2017. p. :1-170.
- [Google Scholar]
- The international knee documentation committee subjective knee evaluation form: Normative data. Am J Sports Med. 2006;34:128-35.
- [CrossRef] [PubMed] [Google Scholar]
- Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-49.
- [CrossRef] [Google Scholar]
- The Lachman test is the most sensitive and the pivot shift the most specific test for the diagnosis of ACL rupture. Aust J Physiother. 2006;52:66.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament quality of life (ACL-QOL) questionnaire: Responsiveness to change up to 2-years post ACL reconstruction. Arthroscopy. 2015;31:e5-6.
- [CrossRef] [Google Scholar]
- Effect of high-grade pre-operative knee laxity on outcomes of anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:3077-82.
- [CrossRef] [PubMed] [Google Scholar]
- Controversies in ACL revision surgery: Italian expert group consensus and state of the art. J Orthop Traumatol. 2022;23:32.
- [CrossRef] [PubMed] [Google Scholar]
- Five-strand hamstring autograft in primary anterior cruciate ligament reconstruction. J Knee Surg. 2019;32:366-71.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the results of arthroscopic anterior cruciate ligament reconstruction using hamstring tendon graft. Int. J Sci. Res. 2017;6:55-7.
- [Google Scholar]
- Outcome assessment after anterior cruciate ligament reconstruction among non-athletes. Int J Contemp Med Res. 2020;7:J1-5.
- [Google Scholar]
- Clinical outcomes of primary anatomic all-inside anterior cruciate ligament reconstruction using the TransLateral technique: A minimum one-year follow-up study. Knee. 2020;27:1753-63.
- [CrossRef] [PubMed] [Google Scholar]
- Five-strand hamstring autograft versus quadruple hamstring autograft with graft diameters 8.0 millimeters or more in anterior cruciate ligament reconstruction: clinical outcomes with a minimum 2-year follow-up. Arthroscopy. 2017;33:1007-13.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of single bundle arthroscopic anterior cruciate ligament reconstruction in a limited resource setting. J ISAKOS. 2021;6:187-92.
- [CrossRef] [PubMed] [Google Scholar]
- Validity, reliability, and responsiveness of the anterior cruciate ligament quality of life measure: A continuation of its overall validation. Clin J Sport Med. 2017;27:57-63.
- [CrossRef] [PubMed] [Google Scholar]
- Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. Arthroscopy. 2001;17:795-800.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:137-45.
- [CrossRef] [PubMed] [Google Scholar]
- SCIENTIFIC PAPER Short-term Results for Anterior Cruciate Ligament Reconstruction Using Autologous Hamstring Graft with the Cross-pin Femoral Fixation Technique. Hong Kong Journal of Orthopaedic Surgery. 2003;7:33-42.
- [Google Scholar]






