Translate this page into:
A minimally invasive revolution: The future of arthroscopy and sports medicine
-
Received: ,
Accepted: ,
How to cite this article: Vaishya R. A minimally invasive revolution: The future of arthroscopy and sports medicine. J Arthrosc Surg Sports Med. 2023;4:27-9. doi: 10.25259/JASSM_5_2024
CHANGING LANDSCAPE OF ARTHROSCOPY
The landscape of sports medicine is undergoing a fascinating transformation driven by advancements in arthroscopy.[1] This minimally invasive surgical technique, once a novelty, is now at the forefront of treating joint injuries and promoting faster recoveries for athletes and active individuals alike. One of the most significant trends is the shift toward tissue and joint preservation. Arthroscopic procedures are no longer solely focused on removal; instead, surgeons are prioritizing the repair and reconstruction of ligaments, menisci, and other vital structures, which not only improves long-term joint health but also enables a quicker return to activity. Technology is playing a crucial role in this evolution. High-definition cameras and advanced instrumentation offer unparalleled visualization and precision during surgery. The rise of robotic-assisted arthroscopy is another exciting development. Robots provide enhanced stability and control, potentially leading to even less invasive procedures and faster healing times. Furthermore, the field is embracing regenerative medicine. Techniques utilizing stem cells and other biological materials are being explored to promote healing and potentially even regenerate damaged cartilage. It holds immense promise for athletes with chronic injuries and could revolutionize post-surgical rehabilitation.
Looking ahead, the focus will likely be on personalization. By factoring in a patient’s age, activity level, and individual biology, surgeons can tailor procedures and rehabilitation plans to optimize outcomes. In addition, the use of biomarkers to identify and diagnose injuries earlier is another promising avenue for the future. However, challenges remain. The high cost of advanced technology and the need for robust evidence-based practices to support the use of regenerative therapies are considerations that need to be addressed.
This editorial will briefly discuss the recent advances and future directions in the field of arthroscopy and sports medicine.
RECENT ADVANCES
The world of arthroscopy and sports medicine is constantly evolving, with several recent exciting advancements, to mention a few examples:
Anterior cruciate ligament (ACL) surgery
Conventionally, ACL tears were treated with reconstruction. Now, advancements allow for repair in some cases, potentially leading to faster healing and better long-term outcomes.[2] Anatomic ACL reconstruction is preferred as it restores the function of the native ACL. The concept of individualized ACL reconstruction has been propagated recently, which tailors the procedure based on factors such as patient anatomy and injury severity.[3] Remnant-sparing techniques in ACL reconstruction may improve joint proprioception and potentially lead to quicker recovery and improved joint stability.[4] Recognizing the role of bone shape in ACL injuries, some corrective measures are being incorporated during ACL reconstruction to address underlying predispositions.[5]
Meniscal tear treatment
There is an increased awareness and focus on meniscal tear repair over removal, whenever possible, as the presence of meniscus is now well-recognized and crucial for long-term knee health. In addition, there have been substantial improvements in the surgical techniques of meniscal repair. The use of stem cells and other biological therapies, such as platelet-rich plasma (PRP) are also being used to promote healing in tears.[6]
Rotator cuff tears treatment
Arthroscopic surgery for rotator cuff repair remains the gold standard, but techniques continue to evolve. “No sling” or early mobilization protocols after surgery are showing promising results for faster recovery of movement without compromising healing rates.[7] Materials such as acellular dermal matrix scaffolds and PRP are used to augment the repair process to improve healing and tendon quality.[8] For larger or irreparable tears, new approaches such as superior capsular reconstruction or tendon transfers are offering improved function and pain relief.[9]
Articular cartilage repair
Stem cells and other biological materials are being explored to enhance healing and potentially regenerate damaged cartilage.[10] It is a promising field of regenerative medicine, especially for chronic injuries, and the research in this field is increasing globally.[11]
Advanced implants and instrumentation
Improved operating tools and implants allow for more precise and minimally invasive procedures, leading to faster recovery times.[12]
FUTURE DIRECTIONS
The future of arthroscopy and sports medicine promises even greater precision, personalization, and potentially preventative measures, as depicted in Figure 1 and described ahead.
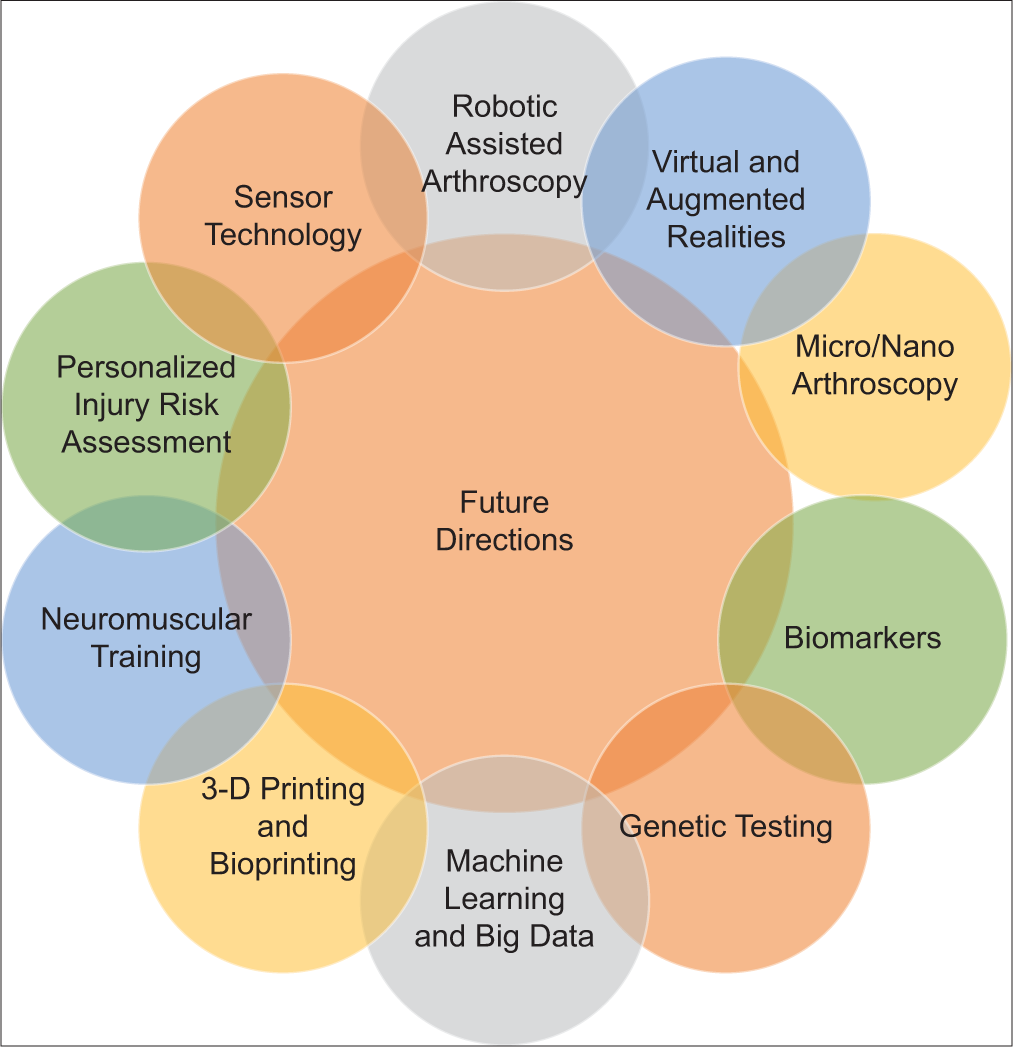
- Future directions in arthroscopy and sports medicine.
Enhanced minimally invasive techniques
Robotic-assisted surgery
Robotic surgery is slowly penetrating the area of arthroscopic surgery after gaining popularity in arthroplasty. It is expected to provide greater control and precision during surgery, which could lead to smaller incisions, faster healing times, and reduced surgical complications.[13]
Virtual reality (VR) and augmented reality (AR)
VR could be used for surgical planning and training, while AR could provide surgeons with real-time information during procedures, improving decision-making.[14]
Micro or nano-arthroscopy
This emerging technique utilizes even smaller instruments and cameras, potentially allowing for even less invasive joint procedures on an outpatient basis.[15]
Precision medicine and personalized care
Biomarkers
Several biomarkers are being used to assess different aspects of health, sports performance, and recovery in sports persons. Identifying specific biomarkers in blood or other samples could allow for earlier and more accurate diagnosis of injuries.[16]
Genetic testing
Understanding an individual’s genetic predisposition to certain injuries could lead to preventative strategies and personalized rehabilitation programs. The genetic information may also be useful to understand and make improvements in specific athletic performance, where their genetic predisposition may be less favorable.[17]
Machine learning and big data
Analyzing vast datasets of patient information could help predict injury risk and personalize treatment plans for optimal outcomes.[18]
Advanced repair and regeneration
Biologic therapies
Continued research on stem cells, growth factors, and other biological materials holds promise for promoting healing, potentially even regenerating damaged tissues.[19]
3D printing and bioprinting
Creating custom implants or scaffolds using 3D printing technologies could aid in tissue repair and regeneration efforts. 3D bioprinting controls the distribution of cells and biological materials to reconstruct human tissues, such as cartilage and tendons. Emerging strategies such as hybrid bioprinting, and 3D printing technology have shown possibilities of wide application.[20]
Preventative strategies
Neuromuscular training
Several preventive strategies have been developed for sport-related injuries. Programs that improve neuromuscular control and proprioception could help prevent injuries before they occur.[21] Wearable sensors help monitor joint health and movement patterns, potentially identifying issues early and preventing injuries.[22] In addition, by analyzing an individual’s biomechanics, movement patterns, and other factors, one could create personalized risk assessments and implement preventative strategies.
CONCLUSION
The field of arthroscopy and sports medicine is on a dynamic trajectory. By embracing minimally invasive techniques, tissue preservation, and cutting-edge technologies, this field is poised to significantly improve the lives of athletes and active individuals, allowing them to return to activities faster and stronger than ever before.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The evolving trends in arthroscopy and sports medicine. J Clin Orthop Trauma. 2022;31:101915.
- [CrossRef] [PubMed] [Google Scholar]
- Bridge enhanced ACL repair vs. ACL reconstruction for ACL tears: A systematic review and meta-analysis of comparative studies. SICOT J. 2023;9:8.
- [CrossRef] [PubMed] [Google Scholar]
- Remnant preservation may improve proprioception after anterior cruciate ligament reconstruction. J Orthop Traumatol. 2022;23:22.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in knee shape between ACL injured and non-injured: A matched case-control study of 168 patients. J Clin Med. 2021;10:968.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal tears: Current understanding, diagnosis, and management. Cureus. 2020;12:e8590.
- [CrossRef] [Google Scholar]
- To sling or not to sling the shoulder after rotator cuff repair: Which side are you on? Ann Transl Med. 2020;8:972.
- [CrossRef] [PubMed] [Google Scholar]
- Biologics to improve healing in large and massive rotator cuff tears: A critical review. Orthop Res Rev. 2020;12:151-60.
- [CrossRef] [PubMed] [Google Scholar]
- Superior capsular reconstruction versus latissimus dorsi tendon transfer for irreparable rotator cuff tears: Minimum 5-year outcomes. Orthop J Sports Med. 2023;11:23259671231166703.
- [CrossRef] [PubMed] [Google Scholar]
- Current therapeutic strategies for stem cell-based cartilage regeneration. Stem Cells Int. 2018;2018:8490489.
- [CrossRef] [PubMed] [Google Scholar]
- The upsurge in research and publication on articular cartilage repair in the last 10 years. Indian J Orthop. 2019;53:586-94.
- [CrossRef] [PubMed] [Google Scholar]
- Current advancements in therapeutic approaches in orthopedic surgery: A review of recent trends. Front Bioeng Biotechnol. 2024;12:1328997.
- [CrossRef] [PubMed] [Google Scholar]
- Robot-assisted orthopedic surgeries around shoulder joint: Where we are? Biomed Eng Lett. 2023;13:553-9.
- [CrossRef] [PubMed] [Google Scholar]
- Application progress of artificial intelligence and augmented reality in orthopaedic arthroscopy surgery. J Orthop Surg Res. 2023;18:775.
- [CrossRef] [PubMed] [Google Scholar]
- In-office nano-arthroscopy of the shoulder with acromioplasty. Arthrosc Tech. 2023;12:e1423-8.
- [CrossRef] [PubMed] [Google Scholar]
- Biomarkers in sports and exercise: Tracking health, performance, and recovery in athletes. J Strength Cond Res. 2017;31:2920-37.
- [CrossRef] [PubMed] [Google Scholar]
- Machine learning methods in sport injury prediction and prevention: A systematic review. J Exp Orthop. 2021;8:27.
- [CrossRef] [PubMed] [Google Scholar]
- Application of stem cells in regeneration medicine. MedComm 2020. 2023;4:e291.
- [CrossRef] [PubMed] [Google Scholar]
- 3D bioprinted scaffolds for tissue repair and regeneration. Front Mater. 2022;9:925321.
- [CrossRef] [Google Scholar]
- Effect of integrative neuromuscular training for injury prevention and sports performance of female badminton players. Biomed Res Int. 2021;2021:5555853.
- [CrossRef] [PubMed] [Google Scholar]
- The use of wearable sensors for preventing, assessing, and informing recovery from sport-related musculoskeletal injuries: A systematic scoping review. Sensors (Basel). 2022;22:3225.
- [CrossRef] [PubMed] [Google Scholar]





