Translate this page into:
A novel surgical technique for arthroscopic fixation of lateral end clavicle fracture using FiberWire and FiberTape

*Corresponding author: Ketansinh Pramodsinh Solanki, Department of Orthopaedics, Soundarapandian Bone and Joint Hospital, Chennai, Tamil Nadu, India. ketansinhs24@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Solanki KP, Soundarapandian RS, Manoharan S. A novel surgical technique for arthroscopic fixation of lateral end clavicle fracture using FiberWire and FiberTape. J Arthrosc Surg Sports Med 2020;1(2):199-206.
Abstract
Objectives:
Lateral end of clavicle fractures is associated with coracoclavicular ligament disruption and, hence, poses a surgical challenge for the management. Surgical techniques already described have high failure rates and hardware-related complications. The objective of the study is to assess the clinical and radiological outcome of the novel surgical technique of arthroscopic coracoclavicular stabilization and indirect anatomical reduction of the lateral end of clavicle fracture using FiberWire and FiberTape.
Materials and Methods:
We conducted a retrospective review of 15 consecutive patients with displaced, unstable Neer Type II and V distal clavicle fractures who underwent this surgical technique from 2016 to 2020. Primary outcome variables were radiographic union, patient satisfaction, and post-operative shoulder function. Pre-operative and post-operative University of California, Los Angeles (UCLA), and American Shoulder and Elbow Surgeons (ASES) scores were compared. Secondary outcome variables included intraoperative complications, post-operative complications, and time to radiographic union.
Results:
In our study, 12 were male patients and three female patients, with a mean age of 43 years. The mean post-operative follow-up period was 23 months. Results were satisfactory in all 15 cases, all 15 were had excellent as per UCLA and ASES score. All fractures healed within a mean period of 6 weeks. Only one patient had developed malunion due to over-tightening of FiberWire, although his functional outcome was not compromised with this.
Conclusion:
We present a novel surgical technique for fixing displaced distal lateral clavicle with arthroscopic coracoclavicular stabilization with FiberWire and FiberTape that resulted in a 100% union rate and excellent clinical outcomes with minimal complications.
Keywords
Lateral end of clavicle fracture
FiberWire
FiberTape
Shoulder arthroscopy
Coracoclavicular stabilization
INTRODUCTION
Clavicle fractures are the most common injuries involving upper limb trauma in clinical practice, and lateral end of the clavicle fracture usually accounts for 10–28% of all the cases.[1,2] The lateral end of the clavicle fracture is defined as a fracture of the clavicle lateral to the attachment of the coracoclavicular ligament.[3] Hence, these fractures are invariably associated with coracoclavicular ligament injury-causing disruption of the suspensory mechanism of the acromioclavicular joint.
The lateral end of clavicle fractures is difficult to manage due to the very small fragment size of lateral end of the clavicle and concurrent ligament disruption causing fracture instability. Regionally in the clavicle, the distal end of the clavicle has presented with the highest rate of non-union.[4] Valuable knowledge regarding the anatomy of the acromioclavicular joint has been helpful in exploring various treatment strategies. The acromioclavicular ligament and capsule play a major role in the horizontal stability of the acromioclavicular joint. The vertical stability of the acromioclavicular ligament joint is mainly maintained by coracoclavicular (CC) ligaments (trapezoid and conoid ligaments). The trapezoid ligament is located 2–3 cm medial to the AC joint, and the conoid ligament is located 4–4.5 cm medial to the AC joint.[5]
Neer has given a classification of the distal end of clavicle fractures in three types based on the integrity of coracoclavicular ligaments and the degree of involvement of acromioclavicular joint.[6] Later, Craig added two additional subtypes to the original classification.[7] Road traffic accidents and sports injury have been the most common mode of injury in young individuals, while in elderly patients, low energy fall accounts for the lateral end clavicle fractures.
The deforming forces of this fracture are the muscle forces pulling the medial fragment superiorly and posteriorly and the weight of the arm on the shoulder girdle pulling the lateral fragment inferiorly and anteriorly.[8] Thus, the principle for the management of such fractures is to counter the deforming forces and bony apposition of the fractured fragment, which can be achieved directly by fixation of the bone fragments, but the lateral fragment is often too small to get hold with any implant.[8,9] Indirectly, (1) acromion can be fixed along the fracture, but the normal rotational movement of AC joint during abduction and flexion would be hampered requiring implant removal and also chances of secondary osteoarthritis of AC joint prevails and (2) fixing the proximal fragment of the clavicle with coracoid and achieving coracoclavicular stabilization. There are several open as well as arthroscopic techniques for fixation. Open techniques include conventional locking plates, intramedullary fixations with knowles pin /AO screw, hook plate, distal radius plate, and coracoclavicular buttons (can be used arthroscopically also). Oh et al.,[10] in a meta-analysis of 425 cases (60 treated conservatively and 365 surgically), concluded that open techniques of fixation despite having excellent healing rate have higher complication rates (22.2 %), while arthroscopic techniques include tight rope device with double button, single Endobutton devices, tunnels in the clavicle, use of allografts like Dacron ligament, FiberTape, and FiberWire sutures. Arthroscopic techniques have shown excellent results. However, they are also associated with few complications and have special indications and not indicated in comminuted and Type V Neer lateral end fractures. However, there is no consensus regarding the optimal strategy for the management of these fractures.
Based on these principles and arthroscopic anatomy of the coracoid process, in this study, we present a novel technique for fixation of unstable and comminuted lateral end of the clavicle fracture Type II and Type V by arthroscopic coracoclavicular stabilization with FiberWire No #2 and FiberTape. It has advantages of being minimally invasive, no need for any metal implant, cost-effective, minimum complication rate, and easier learning curve than available arthroscopic techniques for such fractures.
MATERIALS AND METHODS
We retrospectively recruited 15 consecutive patients who underwent arthroscopic FiberWire fixation for the displaced lateral end of clavicle fracture meeting the inclusion criteria after approval from the Institutional Ethical Committee.
Inclusion criteria
We included that the patients (1) age more than 18 years and (2) NEER II and V lateral end clavicle fracture were included in the study.
Exclusion criteria
(1) Fracture more than 4 weeks old, (2) undisplaced fracture of lateral end of clavicle, and (3) patients having floating shoulder injury were excluded from the study.
Final follow-up results were evaluated in May 2020 using University of California Los Angeles shoulder score (the University of California and Los Angeles [UCLA] score), American Shoulder and Elbow Surgeons score (ASES score), ROM assessment, and post-operative radiographs. Postoperative radiographs were obtained on day 1 after surgery, at the end of 1 month, at the end of 2 months, and at 3 months follow-up.
Surgical technique
Anesthesia: General anesthesia
Position: Lateral decubitus position with operative arm traction of 3–5 kg
The surface anatomic landmarks (acromioclavicular joint, coracoid process, and the site of the fracture) are identified before commencing the procedure after sterile paint and drape
Conventional glenohumeral joint arthroscopy through a posterior portal is first carried out; diagnostic arthroscopic examination of the glenohumeral joint is performed to look for any concomitant glenohumeral injuries, followed by the placement of an anterior-superior portal
Subacromial bursa debridement is performed through the anterolateral portal to view the coracoacromial (CA) ligament. This structure is then followed. The rotator interval and subscapular bursa are cleared using both a shaver and RF and the base of the coracoid process is exposed
At this point, arthroscopy is kept on hold and a 1.5 cm skin incision is made at the anterior-superior aspect of the medial fragment of the clavicle, approximately 1.5 cm from the fracture site after confirming under fluoroscopy
Resuming the arthroscopy, two 16 gauze spinal needles are then placed: One from the anterior aspect of the clavicle to reach the medial part of the coracoid under arthroscopic guidance. The second needle is placed from the posterior aspect of the clavicle to the lateral part of the coracoid [Figure 1]
Prolene suture is then passed through the spinal needles and retrieved through the anterior portal. A FiberWire No #2 and a FiberTape are shuttled under arthroscopic visualization. Now, the sutures are placed under the coracoid and around the clavicle about 1.5 cm from the fracture site over medial fragment [Figure 2]
The site on the clavicle where the sutures are to be knotted is roughened with a rasp to avoid sliding of the sutures on tightening
Again arthroscopy is kept on hold and the reduction of the fracture is carried out, where the surgeon exerts an upward force lifting the arm, while the assistant pulls down the medial fracture fragment by direct pressure without opening the fracture site
After verifying the reduction of fracture fragments by fluoroscopy, the FiberWire is first tied down. It is made sure that there is no over reduction at this point. The FiberTape is next tied over the clavicle [Figure 3].
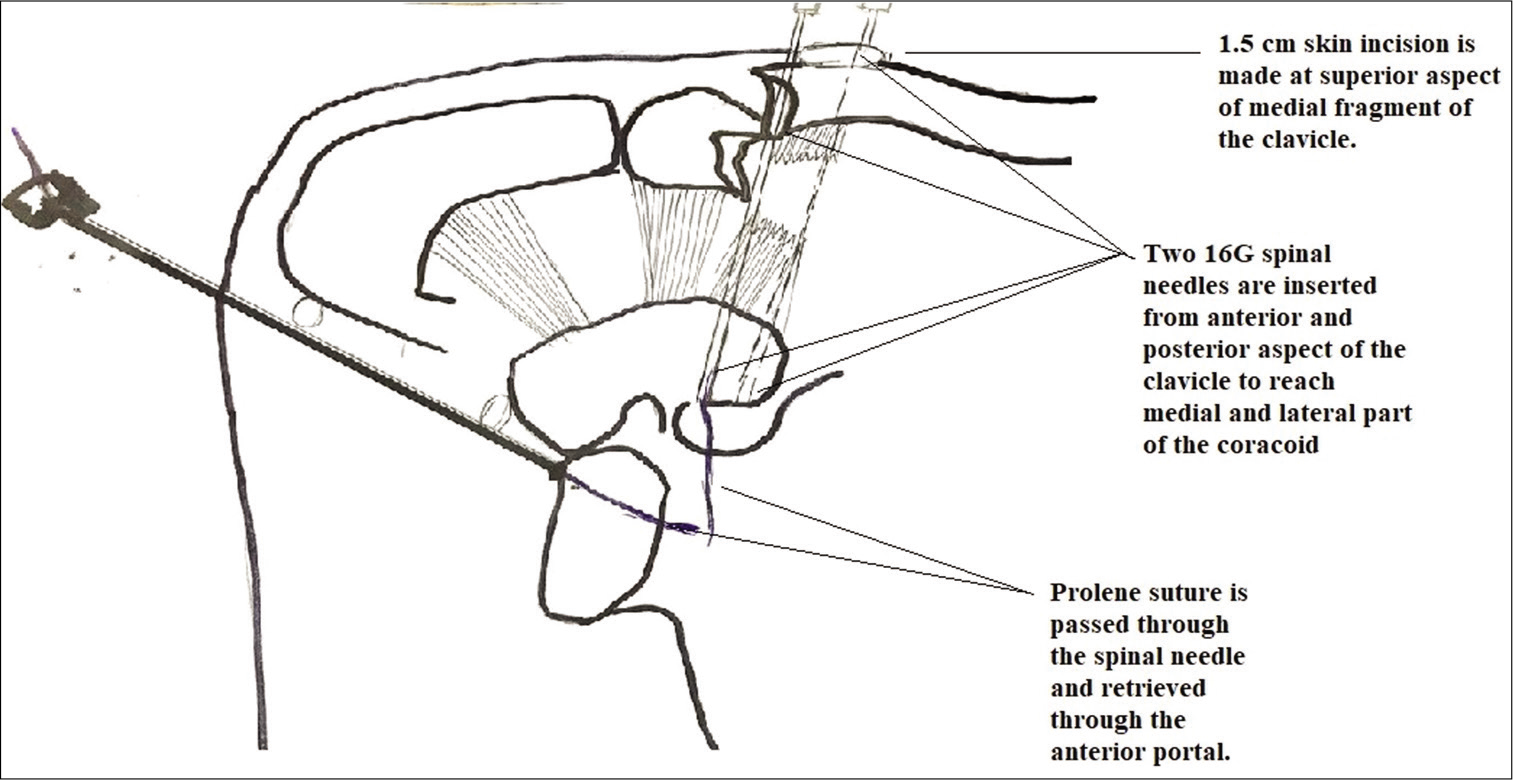
- Schematic diagram showing the steps of technique for retrieval of Prolene suture from anterior portal.
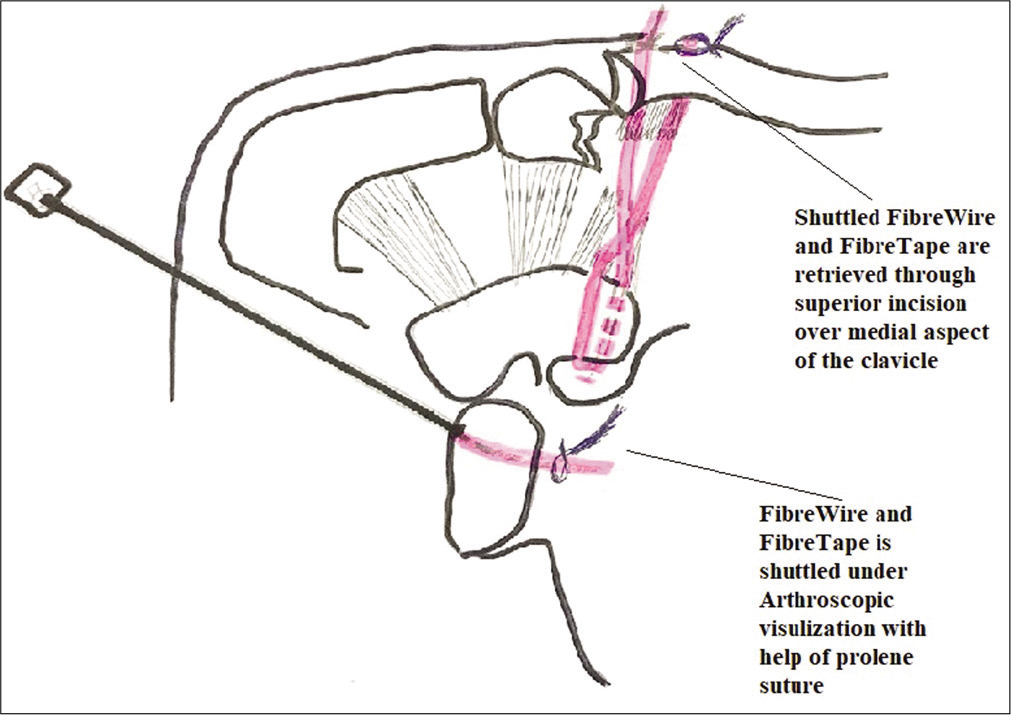
- Schematic diagram showing shuttling of FiberWire and FiberTape to clavicle medial fracture fragment under arthroscopic visualization.
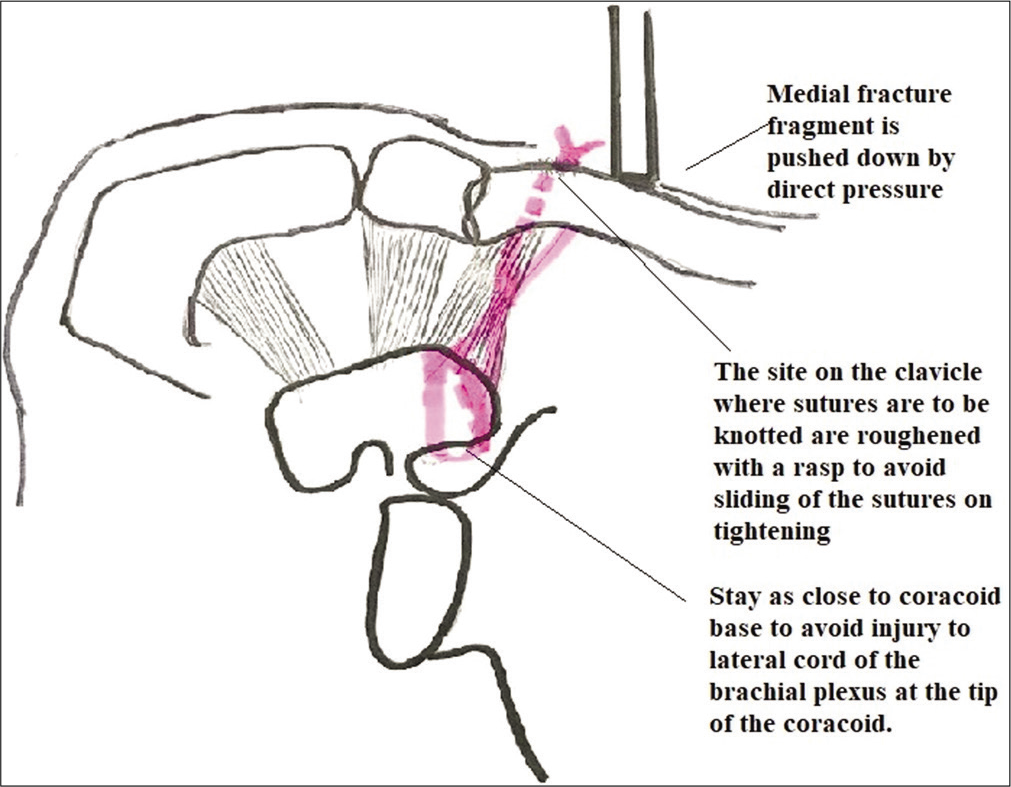
- Schematic diagram showing final knotting of the FiberWire and tape over medial fracture fragment of clavicle.
Post-operative rehabilitation protocol
Patients were given a shoulder arm immobilizer for 4 weeks, followed by gradual mobilization with passive and gravity assisted pendulum exercises. As patients became, more comfortable, active shoulder mobilization exercises are initiated. The patient returned back to their routine activity in 2 months after radiographs showed good healing.
RESULTS
Our study group had 12 male patients and three female patients, with a mean age of 43 years (youngest 27 years and oldest 70 years). The mean duration of the stay in the hospital was of 2 days (ranging from 1 to 4 days). Only one patient was left hand dominant, and rest all were right hand dominant. About 46.66% of patients had sustained an injury on the dominant arm. About 86.66% of the patient had a mode of injury of fall from the 2 wheeler. One patient also had ipsilateral tibia shaft fracture. No other patient had polytrauma. Preoperatively, none of the patient had any history of the previous shoulder problems or surgery of the shoulder joint. Out of 15 patients, 12 patients had Type II Neer fracture and rest three had Type V Neer fracture, and there was no loss of follow-up at the final follow-up. Thus, final outcomes were determined for all the 15 patients. Demographics and outcomes of our study are depicted in [Table 1].
| Patient number | Age | Gender | Side | Mode of injury | Neer classification | Follow-up (months) | Dominant hand | Complications | Post op rom | Restriction of rom compared to opposite shoulder | ASES score | UCLA score | Radiologicaunion on follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 27 | Male | Left | 2 Wheeler slip | 5 | 48 | Right | 150 | No | 94 | 35 | Present | |
| 2 | 56 | Female | Right | 2 Wheeler slip | 2B | 48 | Right | 150 | No | 88 | 35 | Present | |
| 3 | 32 | Female | Right | 2 Wheeler slip | 2B | 40 | Right | 150 | No | 92 | 35 | Present | |
| 4 | 52 | Male | Right | Slip and fall | 5 | 31 | Right | 150 | No | 90 | 35 | Present | |
| 5 | 62 | Female | Left | 2 Wheeler slip | 2B | 29 | Right | 150 | No | 86 | 31 | Present | |
| 6 | 27 | Male | Left | 2 Wheeler slip | 5 | 24 | Right | 150 | No | 96 | 35 | Present | |
| 7 | 37 | Male | Right | 2 Wheeler slip | 2A | 24 | Right | Over-tightening of FiberWire | 150 | No | 93 | 35 | Present |
| 8 | 67 | Male | Right | 2 Wheeler slip | 2A | 22 | Right | 140 | No | 87 | 31 | Present | |
| 9 | 35 | Male | Left | 2 Wheeler slip | 2B | 17 | Right | 160 | No | 91 | 35 | Present | |
| 10 | 26 | Male | Left | 2 Wheeler slip | 2B | 10 | Right | 160 | No | 94 | 35 | Present | |
| 11 | 70 | Male | Right | 2 Wheeler slip | 2B | 9 | Right | 140 | No | 70 | 31 | Present | |
| 12 | 55 | Male | Left | Direct hit in car | 2B | 8 | Left | 140 | No | 86 | 35 | Present | |
| 13 | 31 | Male | Left | 2 Wheeler slip | 2B | 8 | Right | 150 | No | 92 | 35 | Present | |
| 14 | 43 | Male | Left | 2 Wheeler slip | 2A | 5 | Right | 150 | No | 95 | 35 | Present | |
| 15 | 30 | Male | Left | 2 Wheeler slip | 2A | 6 | Right | 160 | No | 94 | 35 | Present |
The mean post-operative follow-up period was 23 months (range, 6–48 months). Results were satisfactory in all 15 cases with complete functional recovery of all the patients. Mean VAS (visual analog score) of all the patient was 1. The mean score for the University of California Los Angeles shoulder score (UCLA score) was 34 (maximum score 35), and the ASES score was 89 (maximum score 100). Both the scores are considered excellent. All the patients had achieved a full functional range of motion at shoulder joint comparable to the opposite shoulder. No patient had to undergo re-surgery.
On a plain radiograph, all the fractures healed within a mean period of 8 weeks (ranging from 6 to 12 weeks) and there was no non-union or delayed union. All the patients were able to resume their work with a mean period of 10 weeks.
Postoperatively, no patient had any immediate or delayed wound complication. Only one patient had developed malunion due to intraoperative over-tightening of FiberWire and FiberTape on serial X-rays. However, the patient remains asymptomatic and functional outcome was not compromised on 2 years follow-up. Serial radiographs showing follow-up all the type of fractures in Figure 4a–c.
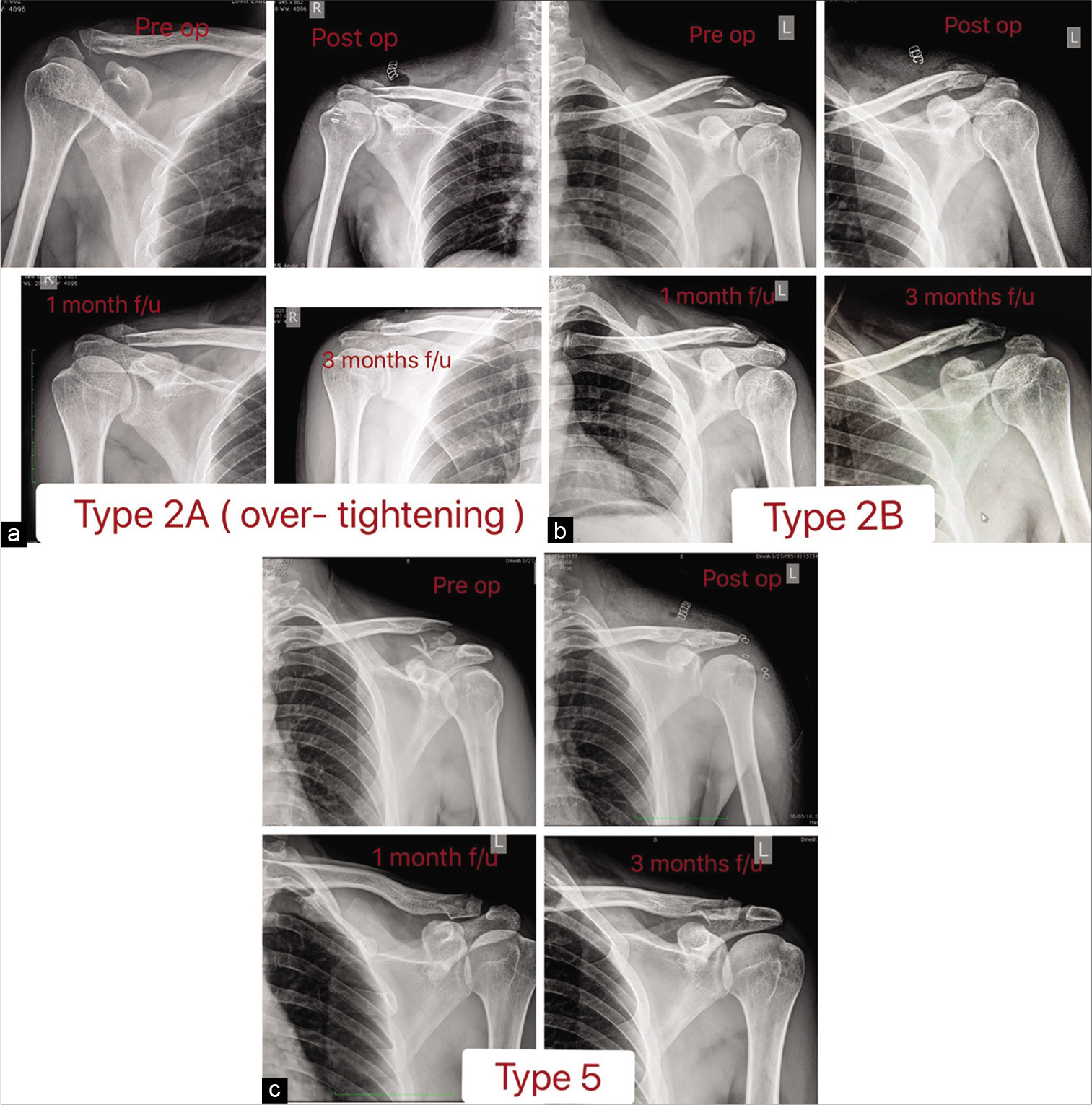
- (a) Follow-up of Neer type 2A (displaced fracture with intact conoid and trapezoid ligament). showing mal reduction due to over-tightening. (b) Follow-up of Neer type 2B (displaced fracture with torn conoid ligament). (c) Follow-up of Neer type 5 (comminuted fracture pattern).
DISCUSSION
The important finding of this study was that arthroscopic coracoclavicular stabilization of comminuted and displaced Neer Type II and V fractures achieves satisfactory outcomes at a mean follow-up of 2 years (ranging from 6 months to 4 years). The patient satisfaction and functional recovery were high. The complication rate was very low with no delayed union or non-union. The result of our study was superior to conventional open techniques such as hook plate, locking plates, coracoclavicular screw fixation, and intramedullary fixation. Our results were comparable with other arthroscopic surgical techniques of coracoclavicular stabilization with lesser complication rates and cost effective with unchallenging learning curve for arthroscopy surgeons.
We had encountered a complication of malreduction, leading to malunion. The reason for it was due to over-tightening of the FiberWire. To overcome this situation, the FiberWire is tightened first and reduction is checked with fluoroscopy, if there is any over-tightening, it is corrected by loosening the same. It is pointed out that if the FiberTape is tightened first then it is not possible to loosen this knot if it is over-tightened, so it is knotted after fiber wire. As we use FiberTape, the chances of erosion of the clavicle are minimized and no erosions were seen in any of the patients compared to any of the previous studies.
We came across two similar studies in the literature, where arthroscopic FiberWire and/or FiberTape fixation for distal end of clavicle fractures was done. Checchia et al.,[11] in 2008, proposed a surgical technique for coracoclavicular cerclage with two FiberWire #5. They designed two special instruments named coracoid hook with flat 90 degree and helical 110-degree curves at the tip for the transport of the FiberWires around the coracoid and to be tied over the medial fragment. They reported satisfactory results with a 15-month follow-up. Nevertheless, the patients had complications: One frozen shoulder and one infection. Our technique superior because we do not require any additional instruments other than routine arthroscopic instruments. Transport of wire is done first with Prolene suture through 16G spinal needle and later shuttled with FiberWire. Using only FiberWire may cause slippage of FiberWires, leading to loss of reduction.
Nourissat et al.[12] presented a technique of arthroscopic stabilization for Neer Type 2 fractures with FiberTape. In this technique, two FiberTape is tied down at the fracture site , hence opening the fracture site. The FiberTape is passed around the clavicle and over the knee of the coracoid anterior to attachment of trapezoid ligament. In our technique, there is no opening of the fracture site. Thus, there is no disturbance to the fracture hematoma and can also be used in comminuted Type V Neer fracture. Tying the suture near the tip of the coracoid increases the chances of injury to the lateral cord of the brachial plexus. Hence, in our technique, while during arthroscopy, we stay as close to the coracoid base to avoid injury to lateral cord of brachial plexus at the tip of the coracoid.[13]
The incidence of complications after procedures including coracoclavicular fixation has been reported to be 4.8%.[10] Xiong et al.[14] did a comparison for three different methods of internal fixation for distal end of clavicle fracture, and they concluded that coracoclavicular stabilization with either using single or double Endobutton technique is associated with some complications, such as suture failure and microgenesis of the coracoid process. Rose et al.[15] and colleagues presented arthroscopy-assisted treatment of displaced distal clavicle fractures utilizing curved buttons and suture tape with a single coracoclavicular tunnel and they had identified that one problem with coracoclavicular fixation techniques is iatrogenic fracture of the clavicle and coracoid associated with large diameter bone tunnels used to secure the implants. Takase et al[16] reported good functional results and bony union achievement in a series of seven patients treated with an artificial ligament and an end button with a mean follow-up of 2 years and 5 months. No complications occurred. Similarly, Loriaut et al[17] presented to report a technique with double button device for 21 patients, and they experienced single implant failure.
There are various open techniques for internal fixation of these fractures. However, due to the high complication rate, they are not preferred mode of treatment. The complication rate was significantly higher when using the hook plate (40.7 %).[10] Hook plate has a risk of damaging acromioclavicular ligaments, fracture of the acromion, rotator cuff tear, and dislocation of hook plate before healing and subacromial impingement.[18] With the locking plate, it is very difficult to hold the very small lateral fragment, fracture at the medial end of the plate, risk of infections, and also re-surgery to remove that the implant is mandatory in majority of the cases of plating.[19] Internal fixation with distal radius locking plate is that it has limited indications in patients with non-comminuted and with large distal fracture fragment.[20] In other modalities like coracoclavicular screws, intramedullary fixation with knowles pin/AO screws and tension band wiring risk of implant migration (9.3%) and acromioclavicular arthritis with hardware related complications prevails.[21]
There are several techniques combining the internal fixation techniques such as K wires and distal radius plating with Endobutton use for coracoclavicular stabilization.[19,22] However, they cannot be used in small size and communition of the distal fragment.
Our technique is a minimally invasive technique with minimum damage to soft-tissue structures and without opening of the fracture site reducing the risk of infection. This technique does not require the use of hardware, thus providing the additional advantage of avoiding re-operations for removal of hardware. However, our study group is small, has not been blinded, or compared with any other control group. Hence, further studies are necessary.
CONCLUSION
This is a novel minimally invasive surgical technique that preserves acromioclavicular joint anatomy and without damaging adjacent soft-tissue structures. Our technique resulted in 100% union rate with excellent functional and radiological outcomes with minimal complication rate. We have improvised on already existing arthroscopic techniques to overcome the intraoperative difficulties and make it easier for beginners and cost effective.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49:774-83.
- [CrossRef] [Google Scholar]
- Arthroscopic resection of the distal clavicle with a superior approach. J Shoulder Elbow Surg. 1995;4:41-50.
- [CrossRef] [Google Scholar]
- Biomechanical study of the ligamentous system of the Acromioclavicular joint. J Bone Joint Surg Am. 1986;68:434-40.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of clavicle fractures: Current concepts review. J Shoulder Elbow Surg. 2012;21:42-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ligamentous anatomy of the distal clavicle. J Shoulder Elbow Surg. 2003;12:355-9.
- [CrossRef] [Google Scholar]
- Fractures of the distal third of the clavicle. Clin Orthop. 1968;58:43-50.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures of the clavicle In: Rockwood CA, Matsen FA, eds. The Shoulder. Philadelphia, PA: W. B. Saunders; 1990. p. :367-412.
- [Google Scholar]
- Injuries to the clavicle and Acromioclavicular joints. Orthop Clin North Am. 1987;18:433-8.
- [Google Scholar]
- The mechanism of clavicular fractures. A clinical and biomechanical analysis. J Bone Joint Surg Br. 1988;70:431-64.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of distal clavicle fracture: A systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131:525-33.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of distal clavicle fractures using an arthroscopic technique. J Shoulder Elbow Surg. 2008;17:395-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic stabilization of Neer Type 2 fracture of the distal part of the clavicle. Arthroscopy. 2007;23:674.e1-6744.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship of the lateral cord of the brachial plexus to the coracoid process during arthroscopic coracoid surgery: A dynamic cadaveric study. Am J Sports Med. 2008;36:1998-2001.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of unstable distal clavicle fractures (Neer Type II): A comparison of three internal fixation methods. J Int Med Res. 2018;46:4678-83.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopy-assisted treatment of displaced distal clavicle fractures utilizing curved buttons and suture tape with a single coracoclavicular tunnel. Tech Hand Up Extrem Surg. 2018;22:94-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic stabilization for Neer Type 2 fracture of the distal clavicle fracture. Arch Orthop Trauma Surg. 2012;132:399-403.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of arthroscopic treatment for displaced lateral clavicle fractures using a double button device. Knee Surg Sports Traumatol Arthrosc. 2015;23:1429-33.
- [CrossRef] [PubMed] [Google Scholar]
- The clavicle hook plate for Neer Type II lateral clavicle fractures. J Orthop Trauma. 2009;23:570-4.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of vertically unstable lateral clavicle fractures (Neer 2b) with locked plate fixation and coracoclavicular ligament reconstruction. Arch Orthop Trauma Surg. 2013;133:935-9.
- [CrossRef] [PubMed] [Google Scholar]
- Noncomminuted lateral end clavicle fractures associated with coracoclavicular ligament disruption: Technical considerations for optimal anatomic fixation and stability. Int J Shoulder Surg. 2014;8:86-9.
- [CrossRef] [PubMed] [Google Scholar]
- Temporary coracoclavicular screw fixation for displaced distal clavicle fractures. J Orthop Surg (Hong Kong). 2007;15:9-11.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of arthroscopy-assisted treatment for distal clavicle fractures. Arch Orthop Trauma Surg. 2019;139:1393-8.
- [CrossRef] [PubMed] [Google Scholar]






