Translate this page into:
Evaluation of associated meniscal and chondral injuries in patients undergoing arthroscopic anterior cruciate ligament reconstruction

*Corresponding author: Dr. Shakti Swaroop, Department of Orthopaedics, Institute of Medical Sciences and Sum hospital, Bhubaneswar, Orissa. drshaktiswaroop@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta P, Swaroop S, Arya R. Evaluation of associated meniscal and chondral injuries in patients undergoing arthroscopic anterior cruciate ligament reconstruction. settings. J Arthrosc Surg Sports Med 2021;2(1):34-40.
Abstract
Objectives:
Anterior cruciate ligament (ACL) injury of the knee is commonly associated with meniscal and chondral lesions. This study was performed to assess the relative risk factors as well as the extent of the meniscal and chondral pathology at the time of arthroscopic ACL reconstruction.
Materials and Methods:
In this prospective study, patients undergoing ACL reconstruction were enrolled. Association of meniscal and chondral lesions was analyzed with age, sex, body mass index (BMI), mechanism of injury (sports-related or not), time gap between injury and surgery (<3 month and >3 months), and instability episodes. Logistic regression and Pearson Chi-square test were applied for evaluating the association.
Results:
A total of 55 patients (mean age 30 years [19–50 years]; 45 male:10 female) underwent arthroscopic ACL reconstruction, out of which 20 (36.3%) had isolated lateral meniscus tear, 14 (25.4%) had isolated medial meniscus tear, and 3 (5.4%) had both lateral and medial meniscus tear. BMI (P = 0.031) and instability episodes (P = 0.033) were predictor for meniscal lesions. Male sex was associated with significantly higher medial (P = 0.049) and lateral meniscal (P = 0.008) lesions. The older age group (>30 years) was associated with medial meniscus lesions (P = 0.047), while the younger age group (<30 years) had significantly higher lateral meniscal lesions (P = 0.008). Chronic ACL injuries (>3 months) had a significantly higher risk of medial meniscus lesions (P = 0.006). Age (>30 years) (P = 0.002) and obesity (BMI >30 kg/m2) (P = 0.043) were predictors of chondral lesions.
Conclusion:
Significant association is observed between age (>30 years), male gender, obesity, and chronicity with medial meniscal injuries in patients with an ACL injury, while younger patients (<30 years) and patient operated within 3 months had a higher incidence of lateral meniscus lesions. Age and BMI (>30 kg/m2) were predictors of chondral lesions in ACL injury.
Keywords
Anterior cruciate ligament reconstruction
Incidence of meniscal lesions
Incidence of chondral lesions
Predictor of meniscal lesions
Predictor of chondral lesions
INTRODUCTION
Anterior cruciate ligament (ACL) injuries have become one of the most common intra-articular injuries of the knee seen in orthopedic clinics. ACL injury can be caused due to contact or non-contact traumatic condition. However, non-contact conditions are more prevalent.[1] Most of the patients with ACL injury are found to have associated injury to other intra-articular structures such as meniscus, ligaments, and cartilage. These associated injuries can occur at the time of index trauma or secondary to internal derangement caused over time in an ACL deficient knee.
Meniscal injuries are commonly seen in association with ACL injury. The incidence, pattern, and location of meniscal injury are dependent on several factors. It has been noted that lateral meniscal lesions are quite common in acute ACL injuries. In the older ACL injuries, however, medial meniscus tears are more common. Furthermore, pattern and distribution of meniscal tear also differ based on the side involved (i.e., medial versus lateral).[2] There is a high prevalence of chondral lesions associated with ACL injury which may be attributed to the complex interaction of knee kinematics, patient activity level, and biological mediators.
Our objective was to identify the predictors of chondral and meniscal lesions in patients undergoing ACL reconstruction and also documents the type and incidence of meniscal and chondral injuries.
MATERIALS AND METHODS
A prospective clinical study of evaluation of meniscal and chondral lesions in patients undergoing arthroscopic ACL reconstruction started after approval from the Institutional Review Board done at tertiary care center over a time period of 18 months. Fifty-five patients with complete ACL tear were included in the study. Patients with the previous surgery on the affected knee or Grades 2 and 3, MCL, LCL or PCL injury, fractures, and osteoarthritis were excluded from the study. All patients were subjected to thorough clinical, functional, and radiological examination, both pre- and post-surgically according to routine protocol. The presence and characteristics of meniscal tears and chondral lesions observed during arthroscopic ACL reconstruction were documented immediately after surgery. The meniscal lesions were classified according to O’Conners classification,[3] and chondral injuries were classified according to the Modified Outerbridge classification system.[4] Relationship of meniscal and chondral lesions with age, sex, body mass index (BMI), mechanism of injury, time to surgery, and instability episode was done by logistic regression, and their association was also examined by Pearson’s Chi-square test after cross-tabulation. For this purpose, age was divided in two groups based on age (<30 years and >30 years), BMI (<24.99 kg/m2, 25–29.99 kg/m2 and >30 kg/m2), and time to surgery (<3 months and >3 months). The level of significance was 5% for all statistical analyses. Statistical analysis was performed using Statistical Package for the Social Science system version SPSS 20.0.
RESULTS
In our study of 55 patients, the age of the patients ranged from 18 to 50 years with a mean age of 30 years (SD 8.36). Forty five (81.8%) were male patients with 28 (50.9%) patients with BMI <24.99 kg/m2, 23 (41.8%) patients with BMI between 25 and 29.99 kg/m2, and 4 (7.3%) patients with BMI >30 kg/m2. About 35 (63.6%) patients had non-sports related injury. Thirty (54.5%) patients were operated within 3 months of injury and 25 (45.5%) patients were operated after 3 months of injury. The mean duration of time to surgery was 7.65 months (SD 10). Forty-three (78.2%) patients had a history of frequent instability episodes [Table 1].
| Age (years) | |
|---|---|
| <30 | 31 |
| >30 | 24 |
| Sex | |
| Male | 45 |
| Female | 10 |
| BMI (kg/m2) | |
| <24.99 | 28 |
| 25–29.99 | 23 |
| >30 | 4 |
| Mechanism of injury | |
| Sports related | 20 |
| Non-sports related injury | 35 |
| Time to surgery (months) | |
| <3 | 30 |
| >3 | 25 |
| Instability episodes | |
| Yes | 43 |
| No | 12 |
Arthroscopic findings [Table 2 and Figure 1] – in our study group, we found that 37 (67.3%) patients had meniscal tears associated with ACL injury. Of which 20 (36.3%) cases had isolated lateral meniscus tear, 14 (25.4%) cases had isolated medial meniscus tear, and 3 (5.4%) cases had both lateral and medial meniscus tear. The pattern of meniscal lesions is described in [Table 3 and Figure 2]. Chondral lesions were seen in 17 (30.9%) cases only and most of the lesions were seen involving the medial femoral condyle (MFC) [Figure 3].
| Overall meniscal tear | |
|---|---|
| Yes | 37 |
| No | 18 |
| Isolated lateral meniscus tear | 20 |
| Isolated medial meniscus tear | 14 |
| Both meniscus tear | 3 |
| Chondral lesion | |
| Yes | 17 |
| No | 38 |
| Pattern | Medial meniscus | Lateral meniscus |
|---|---|---|
| Radial | 2 | 3 |
| Horizontal | 0 | 8 |
| Complex | 9 | 12 |
| Longitudinal | 0 | 1 |
| Bucket handle | 9 | 2 |

- Arthroscopic findings (a) horizontal tear lateral meniscus, (b) bucket handle tear lateral meniscus, (c) complex tear posterior horn medial meniscus, (d) posterior horn tear lateral meniscus, (e) radial tear lateral meniscus, (f) Grade 1 chondral lesion on the medial femoral condyle, and (g) Grade 3 chondral defect.
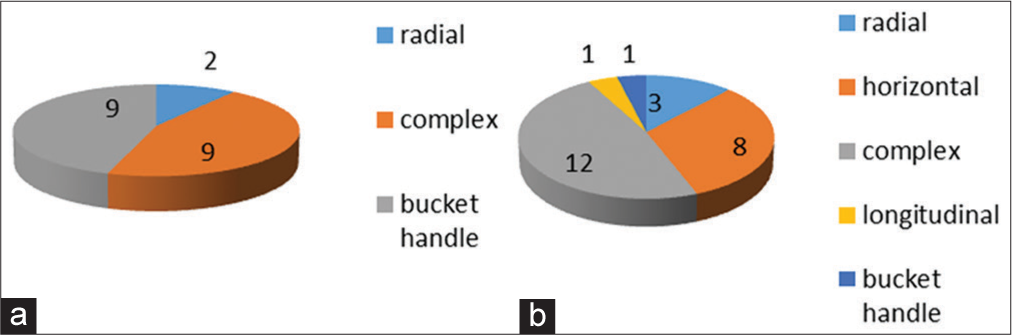
- Pattern of meniscal injuries (a) pattern of medial meniscus tear (b) pattern of lateral meniscus tear.
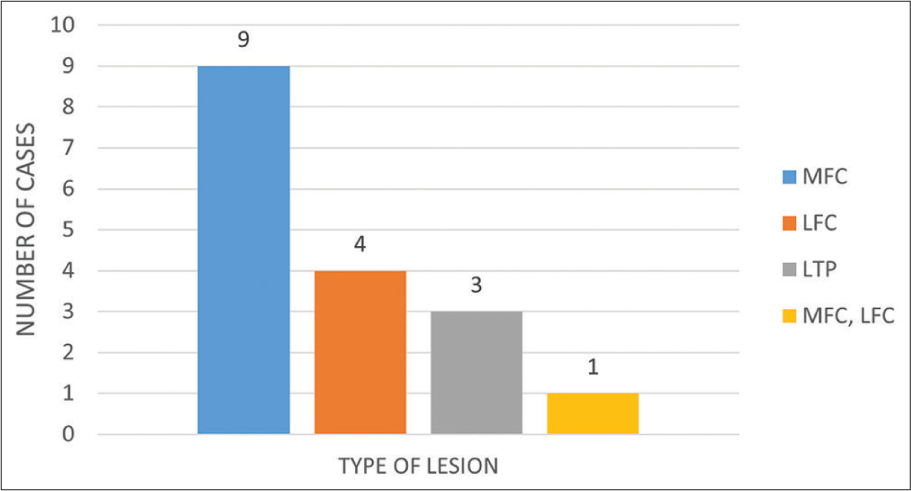
- Distribution of site of chondral lesion.
Predictor of intra-articular injuries
The complete data of correlation of meniscal and chondral lesions is shown in [Table 4a and 4b and Figure 4]. Age is a significant predictor of meniscal injuries. About 37% patients who were >30 years had a significantly higher incidence of medial meniscal lesions (P = 0.047) as compared to younger age group. About 51.6% of patients of younger population (<30 years) had lateral meniscal lesions. Chondral injuries were found more frequently (58.3%) in >30 years age group (P = 0.002)
| Meniscal lesions | P-value | Medial meniscal lesions | P-value | Lateral meniscal lesions | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (%) | No (%) | Yes | No | Yes (%) | No (%) | ||||
| Age (years) | |||||||||
| <30 | 23 (74.2) | 8 (25.8) | 0.214 | 16.1 | 83.9 | 16 (51.6) | 15 (48.4) | 0.008 | |
| >30 | 14 (58.3) | 10 (41.7) | 37.5 | 62.5 | 0.047 | 4 (16.7) | 20 (83.3) | ||
| Sex | |||||||||
| Male | 32 (71.1) | 13 (28.9) | 0.198 | 20 | 80 | 20 (44.4) | 25 (55.6) | 0.008 | |
| Female | 5 (50) | 5 (50) | 50 | 50 | 0.049 | 0 (0) | 10 (100) | ||
| BMI (kg/m2) | |||||||||
| <24.99 | 15 (53.6) | 13 (46.4) | 0.031 | 17.9 | 82.1 | 8 (28.6) | 20 (71.4) | 0.459 | |
| 25–29.99 | 20 (87) | 3 (13) | 39.1 | 60.9 | 0.106 | 10 (43.5) | 13 (56.5) | ||
| >30 | 2 (50) | 2 (50) | 0 | 100 | 2 (50) | 2 (50) | |||
| MOI | |||||||||
| Sports related | 16 (80) | 4 (20) | 0.128 | 30 | 70 | 9 (45) | 11 (55) | 0.314 | |
| Non sports related | 21 (60) | 14 (40) | 22.9 | 77.1 | 0.559 | 11 (31.4) | 24 (68.6) | ||
| TTS (months) | |||||||||
| <3 | 19 (63.3) | 11 (36.7) | 0.495 | 20 | 80 | 11 (36.7) | 19 (63.3) | 0.959 | |
| 0.309 | 9 (36) | 16 (64) | |||||||
| >3 | 18 (72) | 7 (28) | 32 | 68 | -0.006 | ||||
| Instability episode | |||||||||
| Present | 32 (74.4) | 11 (25.6) | 0.033 | 27.9 | 72.1 | 17 (39.5) | 26 (60.5) | 0.355 | |
| Absent | 5 (41.7) | 7 (58.3) | 16.7 | 83.3 | 0.429 | 3 (25) | 9 (75) | ||
| Chondral lesions | P-value | ||
|---|---|---|---|
| Yes (%) | No (%) | ||
| Age (years) | |||
| <30 | 3 (9.7) | 28(90.3) | 0.002 |
| >30 | 14 (58.3) | 10(41.7) | |
| Sex | |||
| Male | 12(26.7) | 33(73.3) | 0.149 |
| Female | 5 (50) | 5 (50) | |
| BMI | |||
| <24.99 | 9 (32.1) | 19 (67.9) | 0.043 |
| 25–29.99 | 5 (21.7) | 18 (78.3) | |
| >30 | 3 (75) | 1 (25) | |
| MOI | |||
| Sports related | 2 (10) | 18 (90) | 0.01 |
| Non-sports related | 15 (42.9) | 20 (57.1) | |
| TTS (months) | |||
| <3 | 10 (33.3) | 20 (66.7) | 0.67 |
| >3 | 7 (28) | 18 (72) | |
| IE | |||
| Present | 13 (30) | 30 (69.8) | 0.83 |
| Absent | 4 (33.3) | 8 (66.7) |

- Correlation of predictors with the intra- articular injuries (a) Predictors correlated with meniscal lesions (b) predictors correlated with medial meniscus lesions (c) Predictors correlated with lateral meniscus lesions (d) Predictors correlated with chondral lesions.
Gender
Females had a higher incidence of medial meniscus tears (50%) as compared to males (20%) (P = 0.049). However, lateral meniscus tears were more common in males (44.4%). In our study, no lateral meniscus tear was observed in females (P = 0.008).
BMI
The percentage of chondral lesions was 32.1% in cases with BMI <24.99 kg/m2, 21.7% in cases with BMI between 25 and 29.99 kg/m2, and 75% in cases with BMI >30 kg/m2. The association of chondral lesions with obesity was significant (P = 0.043). With increasing BMI, there is an increase in the incidence of meniscal tears (P = 0.031).
Mechanism of injury
About 42.9% of patients with non-sports related injuries had chondral lesions (P = 0.01), while there was no significant association of mechanism of injury with meniscal tears.
Interval from injury to surgery
Patients who were operated within 3 months had medial meniscus tears in only 20%, while 32% of patients who were operated after 3 months had medial meniscus tears. The relationship of medial meniscal lesion with chronicity of lesion was found to be statistically significant (P = 0.006).
Instability episodes predicted a significant increase in overall meniscal tear (P = 0.033).
DISCUSSION
Our primary hypothesis was to find the association of predictors of meniscal and chondral injuries. Males and younger age group (<30 years) predicted higher occurrence lateral meniscus tear. Females, age (>30 years) and chronicity of injury (>3 months), predicted a higher incidence of a medial meniscus tear. Age (>30 years), obesity (BMI >30 kg/m2), and non-sports related injuries predicted chondral injuries. The knowledge of the various predictors which lead to associated intra-articular injuries in ACL deficient knee helps the surgeon to plan the management which should be tailor made for each patient.
Many authors have investigated the association between these predictors and intra-articular lesions at the time of ACL reconstruction. Tandogan et al.[5] noticed that older patients exhibit more medial meniscal tear than the younger population. Similarly, increasing age is also a significant predictor of chondral lesions.[6-9]
In our study, MFC was the most commonly involved site for chondral lesions in both the age groups. The incidence of involvement of MFC in the older age group was much higher (29.2%) and severe in grade (Grade 1 – 25%, Grade 2 – 29%, and Grade 3 – 4.2%) as demonstrated by Tandogan et al.[5] and Kluczynski et al.[7] It has been seen that the cartilage lesions were most commonly found on MFC as the medial compartment is the major weight-bearing portion and also possibly due to the concomitant meniscal lesion. Moreover, during flexion knee pivots on MFC and rolls over it instead of a simple hinge-like movement. This complex motion may attribute to the injury in this area.[10]
Kluczynski et al. found that males predicted more lateral as well as medial meniscal tears compared to females.[7] A similar conclusion was also drawn by Brambilla et al.[8] and Piasecki et al.[8] Complex tear was the most common pattern of meniscal tear in both males (31.1%) and females (40%). The most common site of meniscal lesion was the posterior horn (males – 35.6% and females – 40%). However, when considering the body of meniscus, 33.3% of male subjects recorded lesions as against only 10% of female subjects had lesions. A higher percentage of meniscal lesions in males can be due to greater varus alignment and higher generation of force.[11]
Increasing BMI is associated with increasing chondral lesions which are similar to result found by other authors also.[7,8] There is an increase in the incidence of chondral lesions on MFC with an increase in obesity. However, this association was not statistically significant. Increased BMI was also associated with more lateral meniscus injuries and lesser medial meniscus injuries. This was similar to the study by Melissa et al. who observed, obesity predicted more chondral injuries and fewer medial meniscal tears compared to patients with normal BMI.[7] The association between BMI and the prevalence of the meniscal and chondral lesions suggests that mechanical load on the knee joint of overweight individuals is quite high, as suggested by a higher incidence of arthrosis. Therefore, early ACL reconstruction is advisable in this subgroup of patients.
In our study, chondral lesions were associated with non-sports related injuries and were statistically significant (P = 0.01). Røtterud et al. found that the sport/activity factor was a significant predictor for articular cartilage lesions.[12] This contradictory finding in our study could be due to selection bias, as most of our patients had non-sports related injuries. Furthermore, the presence of these lesions in non-sports related injuries indicates that the lesions could have been present earlier and were diagnosed incidentally on arthroscopy.
Patients who underwent arthroscopy after 3 months of injury had an overall higher incidence of meniscal lesions. This observation was in agreement with most of the articles in the literature.[5,8,13-15] We observed a relationship between time to surgery and the type of meniscal tear. The incidence of complex tear roses from 26.7% (in <3 months group) to 40% (in >3 months group). This correlation was not statistically significant, possibly due to the limited sample size.
August Fok et al. found that patients who underwent ACL reconstruction after 12 months delay had a significantly higher incidence of medial meniscus tear compared to the subgroup which underwent early ACL reconstruction.
However, there was no increase in the incidence of lateral meniscus tear associated with delayed ACL reconstruction. They also found that patients with longer surgical delay had a higher incidence of cartilage damage.[15] Tandogan et al. observed an increasing trend of medial meniscus lesion with a delay in surgery.
Patients with instability episodes had a higher incidence of overall meniscal lesions (74.4%) compared to the group with no history of instability episode (41.7%). This association was found to be statistically significant (P = 0.033). Furthermore, patients with a history of instability episodes had a higher percentage of lateral meniscus lesions (39.5%) as compared to patients with no instability episodes (25%). Palmer[16] proposed that, due to the different mobility of the 2 menisci, there is a difference in the incidence of meniscal tears associated with ACL injury. As the lateral meniscus is more mobile, it becomes more susceptible to “a combination of unusual compression and shear force during an (acute) twisting injury to the knee.” On the other hand, medial meniscus is much less mobile and tightly attached to the tibia compared to the lateral side.
Levy et al.[17] suggested that during movement of the knee, there is an increase in translation of the tibia anteriorly which causes the wedging of the posterior horn of the medial meniscus between the femur and tibia, acting as a mechanical block. Hughston[18] proposed a similar mechanism explaining the cause of medial meniscal tears in an ACL-deficient knee. As the function of ACL is lost due to injury, there is an increased translation of tibia anteriorly. This leads to wedging of medial meniscus between the femur and tibia. Simultaneously, the contraction of the semimembranosus muscle along the posterior capsule creates a large amount of stress at the periphery of meniscus. As the force of contraction become strong enough, there will be tearing of the medial meniscus either at the periphery or at the meniscocapsular junction.
There are few limitations to our study. First, the sample size of our data was quite limited because of which few predictors became significant factors. The second limitation is that though we know the type of activity performed at the time of injury, we are not aware of the accurate physical activity patient performs before the injury and also during the interval between the injury and surgery as these can influence the incidence of secondary injury.
CONCLUSION
The pathogenesis of meniscal and chondral lesion associated with ACL injury is multifactorial and complex. ACL injury is commonly associated with such lesions and should be managed promptly during ACL reconstruction. Our understanding of these predictors helps us to identify these lesions at an early stage and prevent long-standing comorbidity of the knee. A significant association is observed between age (>30 years), male gender, obesity, and chronicity with medial meniscal injuries in patients with ACL injury, while younger patients (<30 years) and patient operated within 3 months had a higher incidence of lateral meniscus lesions. Age and BMI (>30 kg/m2) were predictors of chondral lesions in ACL injury.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Prateek Gupta is on the Editorial Board of the Journal.
References
- Osteoarthritis in the anterior cruciate ligament-deficient knee-epidemiology, biomechanics, and effects on the meniscus and articular cartilage. US Musculoskelet Rev. 2010;5:65-9.
- [Google Scholar]
- Traumatic chondral lesions of the knee diagnosis and treatment. In: Modern Arthroscopy. London: Intech Open; 2011. p. :179-96.
- [CrossRef] [Google Scholar]
- Arthroscopy of lower extremity In: Campbell's Operative Orthopaedics (12th ed). Amsterdam: Elsevier; 2013. p. :2397-400.
- [Google Scholar]
- The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43B:752-7.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: Relationship with age, time from injury and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12:262-70.
- [CrossRef] [PubMed] [Google Scholar]
- Articular and meniscal pathology associated with primary anterior cruciate ligament reconstruction. J Knee Surg. 2013;26:185-93.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: A prospective study. Am J Sports Med. 2013;41:2759-65.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of associated lesions in anterior cruciate ligament reconstruction: Correlation with surgical timing and with patient age, sex and body mass index. Am J Sports Med. 2015;43:2966-73.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of meniscal lesions accompanying anterior cruciate ligament tears: A retrospective analysis of 156 patients. Rev Chir Orthop Reparatrice Appar Mot. 2006;92:448-54.
- [CrossRef] [Google Scholar]
- Interactions between severity and location of chondral lesions and meniscal tears found at arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2011;19:1699-703.
- [CrossRef] [PubMed] [Google Scholar]
- Intraarticular injuries associated with anterior cruciate ligament tear: Findings at ligament reconstruction in high school and recreational athletes. An analysis of sex-based differences. Am J Sports Med. 2003;31:601-5.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of gender and sports on the risk of full-thickness articular cartilage lesions in anterior cruciate ligament-injured knees: A nationwide cohort study from Sweden and Norway of 15 783 patients. Am J Sports Med. 2011;39:1387-94.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of timing of ACL reconstruction in surgery and development of meniscal and chondral lesions. Phys Sportsmed. 2012;40:36-40.
- [CrossRef] [PubMed] [Google Scholar]
- Timing of anterior cruciate ligament reconstruction and incidence of meniscal and chondral injury within the knee. Int J Prev Med. 2013;4(Suppl 1):S98-103.
- [Google Scholar]
- Delay in ACL reconstruction is associated with more severe and painful meniscal and chondral injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21:928-33.
- [CrossRef] [PubMed] [Google Scholar]
- On the injuries to the ligaments of the knee joint: A clinical study. Acta Chir Scand. 1938;81(Suppl 53):1-282.
- [Google Scholar]
- The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64:883-8.
- [CrossRef] [PubMed] [Google Scholar]






