Translate this page into:
“Fish head” sign on magnetic resonance imaging in knee synovitis – An observational pilot study
*Corresponding author: Dr. Rajesh Botchu, Department of Musculoskeletal Radiology, Royal Orthopaedic Hospital, Birmingham, United Kingdom. drrajeshb@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saad A, Reddy Venati U, Ariyaratne S, Shah A, Bugata SK, Iyengar K, et al. “Fish head” sign on magnetic resonance imaging in knee synovitis – An observational pilot study. J Arthrosc Surg Sports Med. 2024;5:12-6. doi: 10.25259/JASSM_7_2024
Abstract
Objectives:
Synovitis, characterized by joint inflammation, has various causes, including inflammatory, infectious, degenerative, traumatic, hemorrhagic, and neoplastic origins. Early detection is essential, and magnetic resonance imaging (MRI) plays a vital role in identifying synovial diseases before they lead to irreversible joint damage. It provides characterization and non-invasive monitoring of synovial changes. This study introduces and describes the novel “fish head” sign, a unique identifier of early knee synovitis on MRI.
Materials and Methods:
We conducted a retrospective analysis of 50 MRI cases of patients with rheumatoid arthritis (RA)-related synovitis who were referred to our clinic due to knee pain. The primary aim was to uncover insights into the “fish head” sign, a unique imaging feature observed on sagittal views of the lateral meniscus using proton density (PD)-weighted fat-suppressed sequences.
Results:
Within our cohort of 50 patients, 20 displayed the fish head sign on MRI, whereas 30 did not exhibit this sign. 17/20 of these patients had mild synovitis, 1/20 patients had moderate synovitis, and 2/20 patients had severe synovitis. Fourteen patients with synovitis did not demonstrate the sign.
Conclusion:
Our study introduces the “fish head” sign observed in PD MRI images of early knee synovitis among patients with RA. This unique sign has the potential to serve as a diagnostic tool or adjunct for patients with synovitis of the knee, reducing the need for contrast-enhanced imaging. This discovery offers valuable insights into the field of synovitis assessment, imaging, and diagnosis.
Keywords
Synovitis
Fish head sign
Effusion
Meniscus
Rheumatoid arthritis
Radiography
Magnetic resonance imaging
INTRODUCTION
Synovitis is a condition characterized by the inflammation of the synovial membrane within joints.[1-4] The synovium is an intricate membrane enveloping diarthrodial joints, tendon sheaths, and intraarticular structures, such as the fibrous joint capsule, fat pads, and intraarticular ligaments, and plays a pivotal role in maintaining joint health.[5] It synthesizes crucial synovial fluid responsible for joint lubrication, chemical balance, and nourishment to chondrocytes, thereby ensuring the well-being of articular cartilage.[5] However, certain structures such as articular cartilage, menisci, labra, and the small bone bare areas remain exempt from its coverage.
The causes of synovitis encompass a diverse range of potential differential diagnoses, including inflammatory, infectious, degenerative, traumatic, hemorrhagic, and neoplastic etiologies.[2-4] Synovitis has been shown in various studies to lead to intraarticular structural damage, particularly affecting cartilage, as part of pathological processes involving the synovium, ultimately contributing to irreversible joint deterioration.[2,6]
Hence, early detection of the disease holds critical significance.[3,7] Imaging plays an important role in identifying synovial diseases before they progress to irreversible joint impairment.[1,8,9] Developing familiarity with distinct imaging findings associated with synovial disorders aids in accurate diagnosis and timely intervention.[8,9] While clinical assessment forms the foundation for diagnosis, incorporating advanced imaging modalities significantly enhances diagnostic accuracy and facilitates continuous monitoring of synovial diseases. Among various imaging tools, gadolinium-enhanced magnetic resonance imaging (MRI) has emerged as a valuable tool for evaluating and monitoring synovitis.[10] In addition, ultrasonography (US), radiography, and dual-energy computed tomography have proven to be useful.[11,12] This study introduces a novel sign referred to as the “fish head” sign, a unique identifier of synovitis presence in the knee on MRI. This distinctive sign, observed within knee synovitis cases, offers a fresh perspective to comprehend the intricacies of synovial pathology. Hence, this study aims to describe this sign, thereby contributing to the evolving understanding of synovitis.
MATERIALS AND METHODS
Purpose
The primary purpose of this investigation was to elucidate insights into a newly identified imaging feature termed the “fish head” sign. This distinctive sign was observed in sagittal views of the lateral meniscus using proton density-weighted fat-suppressed (PDFS) sequences. The evaluation of these MRI scans was carried out by our senior authors.
Study design
This retrospective cohort study was conducted following approval from the local hospital clinical audit and effectiveness committee. We retrospectively reviewed our radiology information system and picture archiving and communication system, analyzing 50 consecutive MRI cases of patients referred to our rheumatology clinic due to knee pain and a prior clinical diagnosis of rheumatoid arthritis (RA)-related synovitis. A combination of both MRI scans performed on several different scanners (both 1.5 and 3 Tesla field strengths) was used to maximize the number of patients in the cohort. Scans used were performed on either one of 3T GE MR750W, 1.5T GE 450W, 1.5T Siemens Aera, 3T Siemens Skyra, or 1.5T Siemens Symphony MRI scanners.
Exclusion criteria
Patients with a history of prior knee surgery, infection, meniscal pathology, or the presence of metallic implants were excluded from our study cohort.
Image analysis
All MRI images were reviewed by two fellowship-trained musculoskeletal radiologists with over 10 years of experience. Sagittal PDFS sequences were used as these are sensitive to fluid and synovitis and demonstrate the typical bow-tie appearance of the meniscus. Synovitis was graded as mild, moderate, and severe based on the number of sites within the knee involved, including medial and lateral parapatellar recess, suprapatellar, infrapatellar, intercondylar, and medial and lateral parameniscal regions. The lateral meniscus was assessed at the level of the proximal tibiofibular articulation. Alteration in the normal morphology was a positive “fish head” sign.
Description of the “fish head” sign on MRI
The “fish head” sign manifests as a noticeable alteration in the morphology of the anterior horn of the lateral meniscus, evident on sagittal PDFS images. This alteration is characterized by a reduction in vertical height, rounding of the superior and inferior surfaces of the anterior horn of the meniscus, as well as an anterior bowing of the anterior horn of the lateral meniscus, resembling that of a fish head. This contrasts with the classical triangular-shaped appearance of the anterior horn seen in normal cases. A visual representation of this unique sign is provided in [Figures 1 and 2].
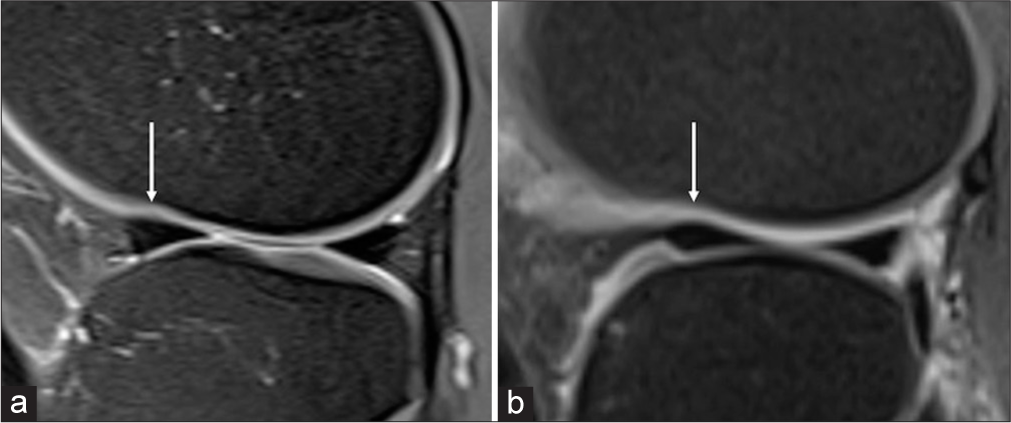
- Sagittal proton density-weighted fat-suppressed image of the knee showing (a) normal morphology of anterior (arrow) and posterior horns of lateral meniscus and (b) “fish head” sign of the anterior horn of lateral meniscus (arrow).
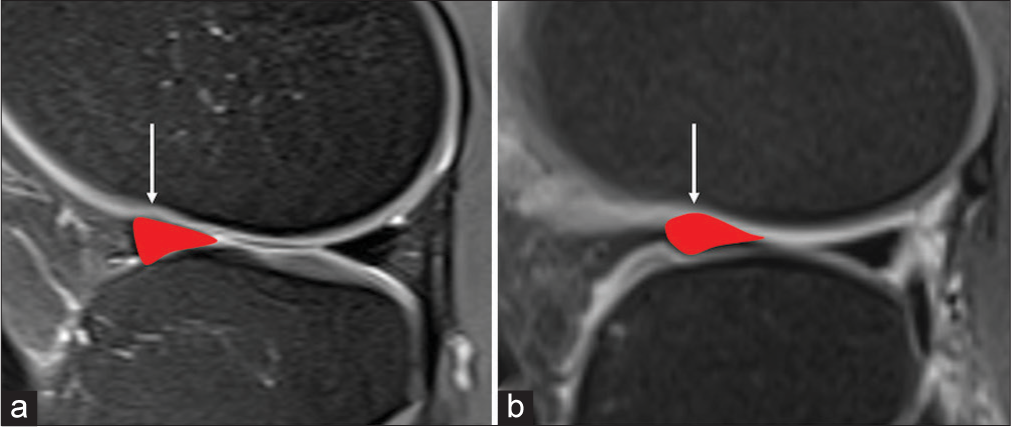
- Sagittal proton density-weighted fat-suppressed image of the knee highlighting (a) normal morphology of anterior (arrow) horn of lateral meniscus and (b) “fish head” sign of anterior horn of lateral meniscus with schematic overlay (arrow).
Statistical analysis
We employed simple descriptive statistics to analyze the data. Patient demographics, severity of synovitis based on MRI findings, and the presence of the “fish head” sign were documented. Data compilation was performed using Microsoft Excel.
RESULTS
Among the 50 patients comprising our cohort, a notable female predominance was observed, with a gender ratio of 2.6 females to 1 male (36 females and 14 males). The average age of our study population was 55.68 years, ranging from 17 to 83 years. Of the entire cohort of 50 patients, 20 individuals exhibited the “fish head” sign on MRI, whereas the remaining 30 patients did not manifest this sign.
Among the 20 patients with the fish head sign, 15 were female, and five were male patients. Furthermore, based on disease severity, 17 of these patients were identified as having mild synovitis, one patient exhibited moderate synovitis, and two patients had severe synovitis. Fourteen patients with synovitis did not demonstrate the sign. One possible explanation for this is that synovitis did not involve the anterior horn of the lateral meniscus.
There was no “fish head” sign in patients without synovitis. The fish head sign was seen in the anterior horn of the lateral meniscus only. Our study suggests that the presence of this sign is more likely to be observed in patients with mild synovitis. There was good agreement between the two readers.
DISCUSSION
Synovial inflammation has been implicated in contributing to knee joint dysfunction, pain, and disability in patients with osteoarthritis (OA) as well as inflammatory conditions, of which RA is most common.[1,2,6,8,13] The hallmark of RA is characterized by synovial proliferation, leading to joint effusion, where an accumulation of exudate results from heightened vascular permeability within the inflamed synovial tissue.[14,15] This sequence progresses to the development of synovial pannus, periarticular bone demineralization, cartilage degradation, and subchondral osseous erosions. Damage to other intra-articular structures, particularly cartilage, typically arises because of pathological processes originating in the synovium, ultimately leading to irreversible joint deterioration.[2,6] In the context of OA, synovitis may manifest early in the disease’s progression, with an excess of synovial fluid stemming from mechanical irritation due to degenerated cartilage and bone.[4] This triggers an amplified production of hyaluronic acid by intimal fibroblasts, further influenced by frictional forces inherent in OA.[5]
Regardless of the underlying cause, a wealth of evidence from the literature substantiates the persuasive notion that targeting synovial inflammation offers a rational pathway for therapeutic intervention to effectively manage symptoms, particularly in patients with inflammatory conditions such as RA.[15,16] Consequently, the significance of early diagnosis cannot be overstated, as it plays a pivotal role in ensuring that patients receive timely and appropriate management.
Patients with intraarticular joint synovitis often exhibit non-specific symptoms, mainly pain, arising from the synovitis itself or concurrent joint issues.[17,18] These symptoms require a comprehensive understanding of their underlying causes. Recent studies have illuminated the intricate connection between knee pain and specific joint synovitis, as observed through MRI, especially in OA and inflammatory joint conditions. These investigations reveal that changes in pain scores correspond well with effusion and synovitis fluctuations over time.[11,17-20] Moreover, they emphasize the independent link between effusion-synovitis and knee symptoms, highlighting its capacity to trigger symptoms apart from other structural issues. In RA-associated synovitis, clinical presentations vary. Patients may experience non-weight-bearing pain, night-time discomfort, and classic inflammation signs in the affected joint, often extending to other joints due to the disease’s systemic nature.[16] Thus, understanding its diverse clinical manifestations is essential for precise diagnosis and tailored treatments.
Various methods are employed to detect and characterize synovitis, including imaging techniques and histologic assessments, especially in early synovial disease stages, before joint damage becomes irreversible.[10-12,17,19] While plain radiography and US assist in diagnosis, MRI is the established standard for diagnosing and tracking synovial diseases.[10,17] This recognition is backed by initiatives such as Outcome Measures in Rheumatology and the European League Against Rheumatism, emphasizing standardized magnetic resonance assessment of synovial conditions.[21,22] MRI comprehensively assesses joint components, encompassing synovium, cartilage, bone marrow, and other structures. It non-invasively evaluates synovial volume and active inflammation, often through dynamic contrast-enhanced techniques highlighting heightened vascularity. Fat-saturated T2-weighted and post-contrast fat-saturated T1-weighted sequences provide insights into synovitis tenosynovitis and adjacent tissues. Moreover, post-contrast fat-suppressed T1-weighted sequences efficiently distinguish synovial proliferation from joint effusion.[23]
Gadolinium-enhanced MRI has emerged as a valuable diagnostic tool for identifying synovial disorders, concurrently detecting bone marrow edema and erosions.[10] Furthermore, the use of dynamic MRI plays a pivotal role in highlighting active disease, effectively presenting a synovial enhancement pattern.[11] However, in situations where contrast-enhanced MRI accessibility is limited, recent evidence suggests assessing synovitis alongside effusion. This poses a challenge to radiologists in distinguishing inflamed synovium from the joint fluid within the synovial cavity, as both exhibit equivalent high signal intensities.[24] Alternatively, Hoffa’s synovitis offers an indirect avenue for assessment, characterized by hyperintense signal changes within Hoffa’s fat pad on non-contrast fat-suppressed proton density (PD) or T2-weighted fast spin echo sequences. It is important to note that signal changes within Hoffa’s fat pad are not exclusive to synovitis; they may also encompass edema, cysts, or Hoffa’s ganglion.[25]
In the present study, we introduce a novel and previously unreported imaging sign, termed the “fish head” sign, observed on sagittal PDFS MRI images during the early stages of synovitis in the knee among patients with RA. We hypothesize that in early synovitis, there is a thickening of the synovium, which causes a mass effect, particularly on the anterior horn of the lateral meniscus, resulting in the “fish head” sign. This was not noted in the posterior horn of the lateral meniscus or medial meniscus, and this could be due to the relatively greater space around these structures. This distinctive sign has the potential to serve as an adjunct diagnostic marker for early synovitis.
We anticipate that this unique imaging feature holds promise for future applications, aiding in the prompt diagnosis and effective management of patients presenting with knee synovitis. By enhancing diagnostic accuracy and offering a practical solution, the fish head sign may contribute significantly to improving patient outcomes and advancing the understanding of synovitis-related pathologies.
Limitations
The sample size was relatively small, which may introduce potential limitations in terms of statistical power and the generalizability of our results. While the findings are significant within the context of our study population, further investigation involving larger cohorts would be valuable to validate the robustness and applicability of the “fish head” sign in a broader context. The specificity and sensitivity of this sign need to be confirmed in large cohort and multi-institutional studies.
In addition, our study exclusively focused on patients presenting with synovitis in the context of RA. As a result, caution must be exercised when attempting to extrapolate these findings to cases of synovitis arising from other conditions or etiologies. The heterogeneity of synovitis across various disease states could influence the manifestation and significance of the “fish head” sign, warranting future investigations that encompass a wider spectrum of synovitis-related pathologies.
Finally, it is important to consider the impact of our institution’s imaging protocols on the results. Since we exclusively utilized PD and PDFS MRI sequences and did not employ contrast-enhanced imaging, there may be nuances that the imaging modality might not fully capture. While the “fish head” sign emerged as a promising marker without the need for contrast enhancement, it is plausible that further nuances could be revealed with the use of different imaging techniques. Therefore, the scope of the “fish head” sign’s applicability should be considered within the context of the imaging methodologies employed in this study. We also utilized scans performed on a range of different MRI scanners and included studies from both 1.5 and 3T scanners to maximize the cohort numbers, which may also have potentially impacted the outcomes.
CONCLUSION
Our study describes the novel “fish head” sign seen on sagittal PDFS MRI images of early knee synovitis among RA patients. This sign could serve as a standalone diagnostic tool or adjunct for synovitis cases without the need for contrast-enhanced imaging. The sign presents a promising avenue for early diagnosis and effective management of knee synovitis in RA. Further research is needed to validate its broader applicability and potential impact on patient care. This new imaging feature could contribute to improved outcomes and a deeper understanding of synovitis-related conditions.
Key points
A fish head sign can be seen in patients with early synovitis
It has the potential to be a diagnostic tool or adjunct for diagnosing synovitis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Synovitis in knee osteoarthritis: A precursor of disease? Ann Rheum Dis. 2016;75:390-5.
- [CrossRef] [PubMed] [Google Scholar]
- Synovitis-an inflammation of joints destroying the bone. Swiss Med Wkly. 2012;142:w13692.
- [CrossRef] [PubMed] [Google Scholar]
- The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat Rev Rheumatol. 2010;6:625-35.
- [CrossRef] [PubMed] [Google Scholar]
- The role of synovitis in osteoarthritis pathogenesis. Bone. 2012;51:249-57.
- [CrossRef] [PubMed] [Google Scholar]
- Hyaluronan and synovial joint: Function, distribution and healing. Interdiscip Toxicol. 2013;6:111-25.
- [CrossRef] [PubMed] [Google Scholar]
- Monoarticular synovitis of knee: Dealing with the dilemma. SICOT J. 2020;6:48.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of knee synovitis using non-contrast-enhanced qDESS compared with contrast-enhanced MRI. Arthritis Res Ther. 2021;23:55.
- [CrossRef] [PubMed] [Google Scholar]
- Synovitis: A potential predictive factor of structural progression of medial tibiofemoral knee osteoarthritis-results of a 1 year longitudinal arthroscopic study in 422 patients. Osteoarthritis Cartilage. 2005;13:361-7.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of synovitis in osteoarthritis: Current status and outlook. Semin Arthritis Rheum. 2011;41:116-30.
- [CrossRef] [PubMed] [Google Scholar]
- Gadolinium-free assessment of synovitis using diffusion tensor imaging. NMR Biomed. 2022;35:e4614.
- [CrossRef] [PubMed] [Google Scholar]
- Basic radiological assessment of synovial diseases: A pictorial essay. Eur J Rheumatol. 2017;4:166-74.
- [CrossRef] [PubMed] [Google Scholar]
- Lead synovitis: The important role of radiology on diagnosis and follow-up: Case report. Radiol Case Rep. 2022;17:3539-44.
- [CrossRef] [PubMed] [Google Scholar]
- The association between meniscal damage of the posterior horns and localized posterior synovitis detected on T1-weighted contrast-enhanced MRI-The MOST study. Semin Arthritis Rheum. 2013;42:573-81.
- [CrossRef] [PubMed] [Google Scholar]
- Angiogenesis in rheumatoid arthritis. Arthritis Res. 2002;4(Suppl 3):S81.
- [CrossRef] [PubMed] [Google Scholar]
- Grading of chronic synovitis-a histopathological grading system for molecular and diagnostic pathology. Pathol Res Pract. 2002;198:317-25.
- [CrossRef] [PubMed] [Google Scholar]
- Rheumatoid arthritis: Pathological mechanisms and modern pharmacologic therapies. Bone Res. 2018;6:15.
- [CrossRef] [PubMed] [Google Scholar]
- Relation of synovitis to knee pain using contrast-enhanced MRIs. Ann Rheum Dis. 2010;69:1779-83.
- [CrossRef] [PubMed] [Google Scholar]
- Association of joint Inflammation with pain sensitization in knee osteoarthritis: The Multicenter Osteoarthritis Study. Arthritis Rheumatol. 2016;68:654-61.
- [CrossRef] [PubMed] [Google Scholar]
- Synovitis in knee osteoarthritis assessed by contrast-enhanced Magnetic Resonance Imaging (MRI) is associated with radiographic tibiofemoral osteoarthritis and MRI-detected widespread cartilage damage: The MOST Study. J Rheumatol. 2014;41:501-8.
- [CrossRef] [PubMed] [Google Scholar]
- Synovitis in osteoarthritis: Current understanding with therapeutic implications. Arthritis Res Ther. 2017;19:18.
- [CrossRef] [PubMed] [Google Scholar]
- The development of the EULAR-OMERACT rheumatoid arthritis MRI reference image atlas. Ann Rheum Dis. 2005;64(suppl_1):i8-10.
- [CrossRef] [PubMed] [Google Scholar]
- The OMERACT MRI in Arthritis Working Group-update on status and future research priorities. J Rheumatol. 2015;42:2470-2.
- [CrossRef] [PubMed] [Google Scholar]
- MRI of synovitis and joint fluid. J Magn Reson Imaging. 2019;49:1512-27.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic and interventional radiology fundamentals of synovial pathology. Acta Biomed. 2020;91:107-15.
- [Google Scholar]
- Superolateral Hoffa's fat pad edema: Association with patellofemoral maltracking and impingement. Am J Roentgenol. 2010;195:1367-73.
- [CrossRef] [PubMed] [Google Scholar]







