Translate this page into:
Functional outcome of hamstring versus peroneus longus tendon graft in arthroscopic anterior cruciate ligament reconstruction –A prospective comparative study
*Corresponding author: Sushant Thakur, Department of Orthopaedics, Armed Forces Medical College, Pune, India. sushantthakur1992@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vijay VK, Deepak DK, Pande H, Thakur S, Anand R. Functional outcome of hamstring versus peroneus longus tendon graft in arthroscopic anterior cruciate ligament reconstruction – A comparative study. J Arthrosc Surg Sports Med. 2024;5:32-7. doi: 10.25259/JASSM_22_2023
Abstract
Objectives:
The objective of this study was to determine whether there is any significant difference between the functional outcome of the knee using a hamstring (HS) graft and peroneus longus (PL) tendon graft after arthroscopic anterior cruciate ligament (ACL) reconstruction.
Materials and Methods:
A study was done on 140 patients from January 2021 to January 2022 as per inclusion criteria. All patients underwent arthroscopic ACL reconstruction using PL tendon and HS tendon grafts. Patients were followed up with the International Knee Documentation Committee (IKDC) and Modified Cincinnati Score (MCS) for a period of 12 months. Average time of surgery and complications if any were noted.
Results:
At one year follow-up, the IKDC score was 91.98 ± 3.92 and 91.74 ± 6.93, respectively, for PL and HS groups with P = 0.803. Similarly, the MCS had P = 0.161 and mean values for PL and HS groups being 92.86 ± 3.88 and 91.80 ± 4.67, respectively.
Conclusion:
The present study shows that the PL tendon autograft has slightly better outcomes on knee functional scores (IKDC and MCSs) to that derived from HS graft in arthroscopic reconstruction of ACL tear over one year of follow-up. PL can be considered as an alternative graft option, but further studies are needed in other sex and age groups and using different functional knee scores to establish the superiority of PL graft over HS graft.
Keywords
Anterior cruciate ligament
Peroneus longus
Hamstring
Modified Cincinnati score
INTRODUCTION
Knee stability is mainly provided by ligaments and involves the cruciate ligaments. The anterior cruciate ligament (ACL) and posterior cruciate ligament are the most important ones.[1] ACL plays an important role in stabilizing knee joints against translational and rotational forces. ACL tear may lead to knee instability, meniscus tear, and subsequent osteoarthritis.[2]
ACL reconstruction is a common procedure in orthopedics surgery.[3,4] ACL reconstruction can be performed using a variety of different surgical techniques as well as different graft materials.[5] Nowadays, bone-patellar tendon-bone (BPTB) and four-strand hamstring (HS) autografts are the two most common autografts used for ACL reconstruction and each has its advantages and disadvantages.[5-7] Although the BPTB autograft has been a gold standard, 40-60% of patients who have undergone ACL reconstruction using patellar tendon autograft have an anterior knee problem that can jeopardize the activity for the patients, who spend a lot of time on their knee for culture and job.[7,8] Quadrupled HS has become an increasingly popular alternative autograft and recent reports indicate less donor morbidity; however, the HS harvest medially can damage the saphenous nerve and could potentially lead to instability of the medial knee joint if ACL rupture accompanied by medial collateral ligament injury.[8,9] An ideal autograft should have an acceptable amount of strength, and size and be easily and safely harvested.[8] Surgical site infection may occur in patients with skin and soft-tissue injury in the area of pes anserine insertion from where the medial HS graft is harvested. In addition, another feasible autograft would be useful in revision situations or as a supplement to other autograft choices.[8] The peroneus longus (PL) tendon may be a potential autograft, as it is superficial in the lateral aspect of the distal leg and can be easily harvested. Important functions of PL include plantar flexion of the ankle, eversion of the sole, maintenance of the transverse arch, and steadying of the leg on the foot.[10-14] Previously, PL was used as a source of autologous tendon graft, but studies about its side effects are insufficient.[15-19] Studies have shown that the PL that had been taken did not have any effect on walking and did not interfere with ankle stability.[20] Biomechanical evaluations of the properties of complete PL grafts have been done recently and revealed that both the strength and stiffness of complete PL grafts are suitable for knee ACL reconstruction.[21,22]
Thus, the purpose of this study is to compare the impact of HS graft and PL graft on the knee using knee functional scores. This study was undertaken at a tertiary care teaching center in Western India in patients with ACL injury of the knee diagnosed clinically and by magnetic resonance imaging (MRI) (if indicated), who underwent ACL reconstruction using HS graft and PL graft, by assessing clinical outcomes in the knee using International Knee Documentation Committee (IKDC) Score and Modified Cincinnati score (MCS).
MATERIALS AND METHODS
We did a prospective comparative study from January 2021 to January 2022 at our institution. A total of 130 patients were enrolled, who underwent arthroscopic ACL reconstruction. One group of 65 patients underwent ACL reconstruction using HS tendon graft, while in another group of 65 patients, PL tendon graft was used and they were followed up for 12 months. Ethical approval was taken from the Institutional Ethical Committee.
Study population
The patients were enrolled from the outpatient department, who were diagnosed with ACL injury of the knee and underwent reconstructive surgery using PL tendon or HS autografts at this center from January 2021 to January 2022. They were recruited in the study after written informed consent. Patients in the age group between 20 and 45 years and having isolated ACL injuries were included in this study. Patients having other associated ligament injuries, chondral damage, meniscal injuries, fractures around the knee, osteoarthritis, presence of pathological conditions in lower extremities, or an abnormal contralateral knee joint were not included in this study. Patients were subjected to a detailed pre-operative clinical and radiological examination (radiographs and MRI) to establish the diagnosis and formulate the plan of treatment. They underwent diagnostic arthroscopy and a definitive procedure under the effect of spinal anesthesia.
Surgical technique
The patients were positioned and a tourniquet was applied over the thigh. Standard anterolateral and anteromedial portals were made. Diagnostic arthroscopy was done, followed by graft harvestation – either the ipsilateral PL or the HS tendon. Semitendinosus and gracilis tendons were harvested by standard procedure. For the peroneus tendon, a skin incision was made, 2–3 cm above and 1 cm behind the lateral malleolus. The PL and peroneus brevis tendons were identified. The location of the tendon division was marked, 2-3 cm above the level of the lateral malleolus [Figure 1]. The distal end of the PL tendon was sutured to the peroneus brevis tendon. The average size of the graft was 7-8 cm. The PL tendon was stripped with a tendon stripper [Figure 2]. Fibrous tissue was cleared off from the intercondylar notch for easy visualization. The femoral tunnel and the tibial tunnel were then prepared. After drilling the tunnels, implantation of the tendon with graft fixation on the femoral side with an Endobutton and graft fixation on the tibial side with a bioabsorbable screw was done.
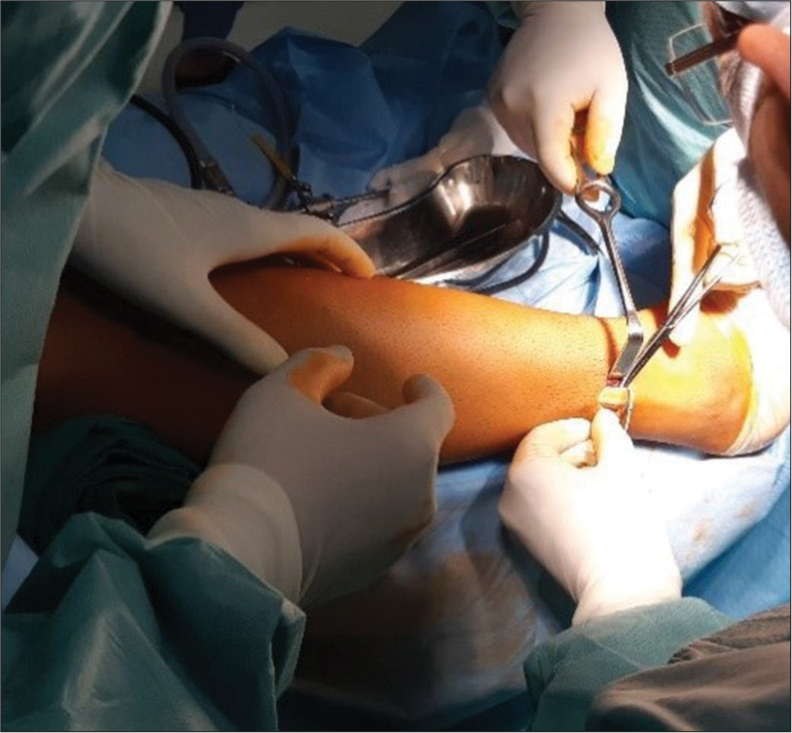
- Peroneus longus tendon graft harvestation technique.

- Peroneus longus tendon graft preparation.
Post-operative protocol
All patients were subjected to the same standard rehabilitation protocol irrespective of the type of tendon graft used. Wound examination was done on the 4th post-operative day followed by suture removal on the 14th post-operative day as per the hospital protocol. Regular documentation of the results for IKDC and MCS was done at postoperatively 6-week, 6-month, and 12-month intervals.
RESULTS
Out of a total of 141 patients evaluated, 130 patients were enrolled for the study, randomized to the HS and PL group of 65 patients each. Eleven patients were removed as they either satisfied the exclusion criteria, refused informed consent, or could not complete all the follow-ups [Figure 3]. The mean age of the participants was 31.7 ± 6.60 years and 30.38 ± 6.66 years in PT and HS groups, respectively, with a comparable distribution among both genders (P = 0.257). The maximum representation was in the age group of 31-40 years in both groups. The minimum representation was from the age of more than 40 years with only seven patients. The injury was more commonly found in the left ACL with a total of 73 patients in both groups. The mechanism of injury in participating patients was comparable with P = 0.482. The most common cause of injury was of contact sports with 45 patients in the PL group and 51 patients in the HS group. The mean values of the IKDC score at 6 weeks for the PL and HSs group were 75.86 ± 4.96 and 76.46 ± 7.64, respectively, with a comparable P = 0.596. Similar to the IKDC score, the MCS was comparable with P = 0.132 and mean values for PL and HS groups being 77.38 ± 5.03 and 79.09 ± 7.57, respectively. At 6-month follow-up, the IKDC scores were comparable with P = 0.544 and mean values for PL and HS groups being 83.25 ± 4.91 and 82.55 ± 7.75, respectively. Similarly, MCS at 6 months was 84.52 ± 4.93 and 83.65 ± 7.80, respectively, for the PL and HS group with a comparable P = 0.445. At one year follow-up, the IKDC score was 91.98 ± 3.92 and 91.74 ± 6.93, respectively, for PL and HS groups with P = 0.803. Similarly, the MCS had P = 0.161 and mean values for PL and HS groups being 92.86 ± 3.88 and 91.80 ± 4.67, respectively [Tables 1 and 2].
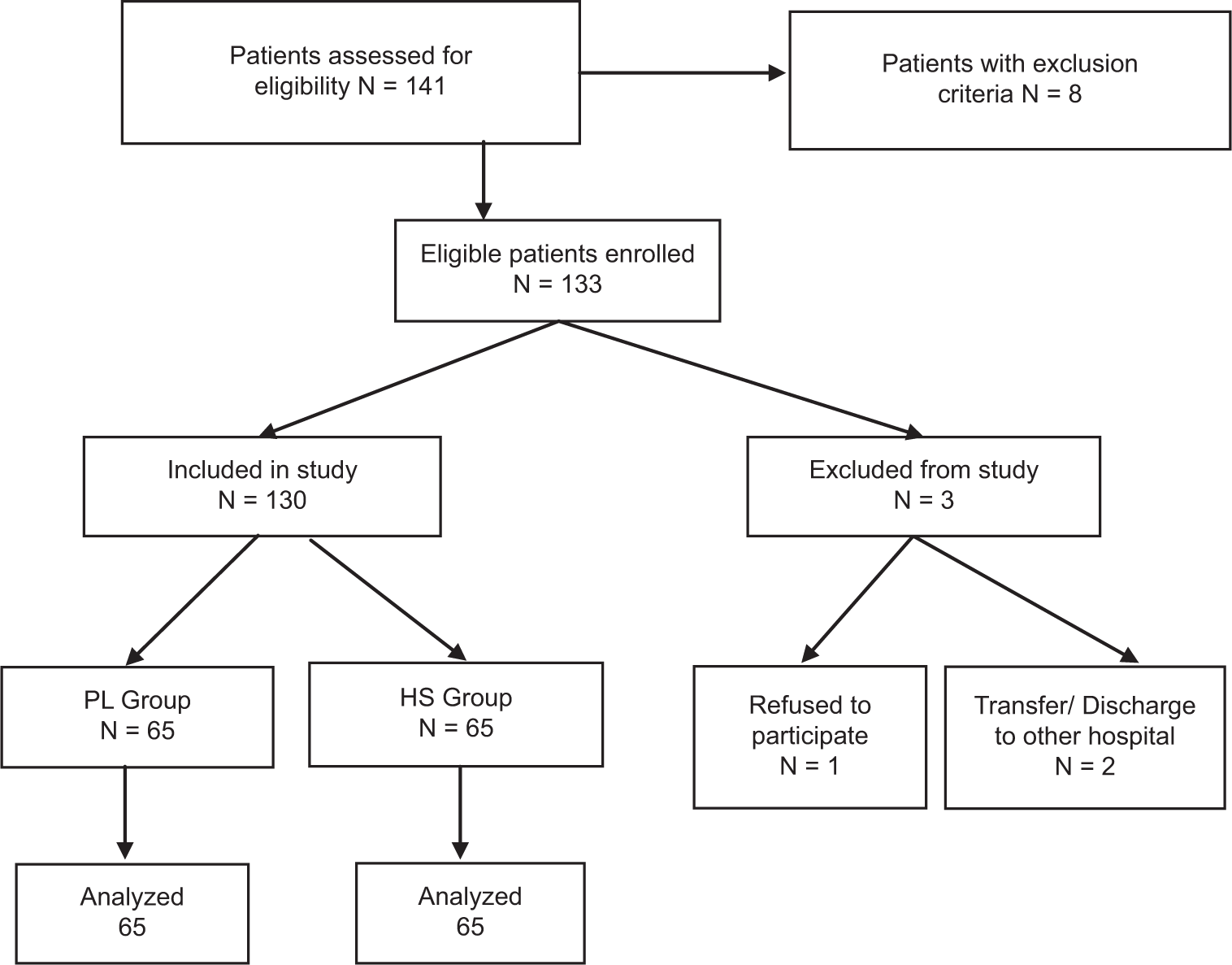
- Flow of participants in this study, hamstring (HS) tendon, and peroneus longus (PL) tendon.
| Group PL | Group HS | t | P-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| (a) | ||||||
| IKDC Pre-operative | 46.29 | 5.06 | 47.20 | 7.72 | −0.793 | 0.429 |
| IKDC 6 week | 75.86 | 4.96 | 76.46 | 7.64 | −0.531 | 0.596 |
| IKDC 6 month | 83.25 | 4.91 | 82.55 | 7.75 | 0.608 | 0.544 |
| IKDC 1 year | 91.98 | 3.92 | 91.74 | 6.93 | 0.249 | 0.803 |
| (b) | ||||||
| DIFF IKDC 6 week | 29.57 | 0.50 | 29.26 | 0.44 | 3.718 | 0.001 |
| DIFF IKDC 6 month | 36.95 | 0.91 | 35.35 | 1.24 | 8.378 | 0.001 |
| DIFF IKDC 1 year | 45.69 | 2.41 | 44.54 | 2.39 | 2.743 | 0.007 |
HS: Hamstring, PL: Peroneus longus, IKDC: International Knee Documentation Committee, SD: Standard deviation, P value: Probability value, t: t score, DIFF: Difference in scores at respective interval
| Group PL | Group HS | t | P-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| (a) | ||||||
| MCS- Pre-operative | 47.82 | 5.14 | 49.83 | 7.64 | −1.765 | 0.080 |
| MCS-6 week | 77.38 | 5.03 | 79.09 | 7.57 | −1.515 | 0.132 |
| MCS-6 month | 84.52 | 4.93 | 83.65 | 7.80 | 0.766 | 0.445 |
| MCS-1 year | 92.86 | 3.88 | 91.80 | 4.67 | 1.409 | 0.161 |
| (b) | ||||||
| DIFF MCS-6 week | 29.57 | 0.50 | 29.26 | 0.44 | 3.718 | 0.001 |
| DIFF MCS-6 month | 36.71 | 1.30 | 33.82 | 1.46 | 11.961 | 0.001 |
| DIFF MCS-1 year | 45.05 | 2.44 | 41.97 | 5.79 | 3.950 | 0.001 |
HS: Hamstring, PL: Peroneus longus, IKDC: International Knee Documentation Committee, SD: Standard deviation, MCS: Modified Cincinnati score, Pvalue: probability value, t: t score, DIFF: difference in scores at respective interval
DISCUSSION
Knee injuries leading to ACL tears are commonly seen in contact sports and sometimes in road traffic accidents or domestic injuries. ACL tear leads to knee instability, degeneration of the knee joint, and other complications. Hence, the reconstruction of ACL is of utmost significance in preventing these secondary complications. Its reconstruction has been tried with various methods including autografts, xenografts, and composite materials. The autografts are usually done by harvesting from different tendons such as the HS tendon, patellar tendons, and of late with PL tendon. Recent studies evaluating the usefulness of the PL tendon for ACL repair have found it to be promising and useful. The present study was done to add to the scientific evidence toward comparing the repair of ACL by HS or semitendinosus tendon and repair with peroneus longus tendon by comparing two known and validated knee scores. In our study, a total of 141 patients were evaluated and finally, 130 patients were enrolled for the study, randomized to HS and PL groups of 65 patients each. Eleven patients were removed as they either satisfied the exclusion criteria, refused informed consent, or could not complete all follow-ups.
Similar studies were performed without contradictory results which did not lead to satisfactory conclusions in the past. Multiple studies such as Feller et al.[23] and Keays et al.[19] have extensively studied the comparison between HS and patellar tendon grafts with most studies concluding no significant difference between the groups on IKDC and MCS scores.
Rudy and Phatama[20] compared the biomechanical properties of the cadaveric HS and PL tendons and reported that the HS has a lower average tensile strength value compared to the PL graft without significant difference (P > 0.05). Pearsall et al.[21] evaluated the biomechanical properties of the PL tendon along with two more autografts for its suitability for ligament reconstruction.
Following the cadaveric studies, several authors published their findings comparing the HS tendon with the PL tendon. Rhatomy et al.[6] compared the clinical outcome and donor site morbidity of ACL reconstruction with HS tendon autografts versus PL tendon autografts in patients with an isolated ACL injury. Fifty-two patients were studied. The authors concluded that ACL ligament reconstruction with PL autografts produces a functional score (IKDC, modified Cincinnati, Lysholm) comparable to that of HS autografts at a 1-year follow-up, with the advantages of larger graft diameter, less thigh hypotrophy, and excellent ankle function based on American Orthopedic Foot and Ankle Scale (AOFAS) and Foot and Ankle Disability Index (FADI) scores.
A total of 65 patients were included in the study, respectively, in PT and HS groups. Our study had many more patients than other studies comparing ACL reconstruction with either PL or HS tendons such as those by Rhatomy et al.[6] with 52 patients, Angthong et al.[7] with 24 patients, and Bi et al.[24] with 62 patients. The mean age of the participants was 31.7 + 6.60 years and 30.38 + 6.66 years in PT and HS groups, respectively, with a comparable distribution among both genders (P = 0.257). The maximum representation was in the age group of 31–40 years in both groups. The minimum representation is from the age of more than 40 years with only seven patients. The age of the patients was comparable to Rhatomy et al.,[6] Kerimoglu et al.,[15] Bi et al.,[24] and Khajotia et al.[25]
The injury was more commonly found in the left ACL with a total of 73 patients in both groups. The mechanism of injury in participating patients was comparable with P = 0.482. The most common cause of injury was contact sports with 45 patients in the PT group and 51 patients in the HS group. The mechanism of injuries was also found to be comparable to the study by Rhatomy et al.[6] which listed 69% of their patients having sports injuries in a cohort of 75 patients. However, another study by Rhatomy et al.[6] found sports injuries to be much more common than road traffic accidents on motorcycles or those due to domestic injuries.
The mean values of IKDC score at 6 weeks for PL and HS groups were 76.86 ± 4.96 and 76.46 ± 4.64, respectively, with a comparable P = 0.596. Similar to the IKDC score, the MCS was comparable with P = 0.132 and mean values for PL and HS groups being 77.38 ± 5.73 and 79.09 ± 7.57, respectively. At 6-month follow-up, the IKDC scores were comparable with P = 0.544 and mean values for PL and HS groups being 83.25 ± 4.91 and 82.55 ± 7.75, respectively. Similarly, MCS at 6 months was 84.52 ± 4.93 and 83.65 ± 7.80, respectively, for PL and HS groups with a comparable P = 0.445. Khajotia et al.[25] evaluating a cohort of 25 patients in India reported lower IKDC scores of 83.53 during the evaluation period of 6 months.
At one year follow-up, the IKDC score was 91.98 ± 3.92 and 91.74 ± 6.93, respectively, for PL and HS groups with P = 0.803. Similarly, the MCS had = 0.161 and mean values for PL and HS groups being 92.86 ± 3.88 and 91.80 ± 4.67, respectively. Lower IKDC scores of 89.3 ± 8.4 were reported by Bi et al.[24] in a cohort of 62 patients followed over 2.5 years by the authors. Similar IKDC scores were reported by Rhatomy et al.,[6] who reported IKDC scores of 92.5 ± 6.2 in a cohort of 52 patients. Similarly, Kerimoglu et al.[15] reported an IKDC score of 90 in their cohort of 27 patients undergoing single-bundle ACL repair. The authors noted this higher score at the end of 5 years, which was a much higher duration of evaluation as compared to our study. Similar to the previous study, Shi et al.[8] reported higher IKDC scores after 2 years of evaluation in 18 patients with ACL tears. In contrast to these studies, Angthong et al.[7] reported much lower IKDC scores of 58.6 ± 20.8 in their patient cohort comprising 24 Thai patients.
Limitations
Our study had some limitations as well. Follow-up data were calculated by the authors mentioned above, and none was blinded to the study. We did not take into consideration patient satisfaction with the level of functional outcome achieved which might differ from patient to patient and give different results in the long run and influence the study outcome. Other sex and age groups were and also other knee functional scores were not considered.
CONCLUSION
The present study shows that the PL tendon autograft has slightly better outcomes on knee functional scores (IKDC and MCSs) than the HS graft in arthroscopic reconstruction of ACL over one year of follow-up. PL can be considered as an alternative graft option, but further studies are needed in other sex and age groups and using different functional knee scores to establish the superiority of PL graft over HS graft.
Ethical approval
The research/study was approved by the Institutional Review Board at Armed Forces Medical College, Pune, number 56/2021, dated December 11, 20.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
The implants used were purchased as a part of the Government of India Procurement Policy for Defence.
References
- Anterior cruciate ligament reconstruction using the medial third of the patellar tendon. J Orthop Surg (Hong Kong). 2011;19:221-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective comparison of auto and allograft hamstring tendon constructs for ACL reconstruction. Clin Orthop Relat Res. 2008;466:2238-46.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction best practice: A review of graft choice. World J Orthop. 2014;5:23-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bone tunnel enlargement after ACL reconstruction using autologous hamstring tendons: A CT study. Int Orthop. 2007;31:49-55.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament double-bundle reconstruction with hamstring tendon autografts. Arthroscopy. 2007;23:109.e1-4.
- [CrossRef] [PubMed] [Google Scholar]
- Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sport Traumatol Arthrosc. 2019;27:3552-9.
- [CrossRef] [PubMed] [Google Scholar]
- The anterior cruciate ligament reconstruction with the peroneus longus tendon: A biomechanical and clinical evaluation of the Donor Ankle morbidity. J Med Assoc Thai. 2015;98:555-60.
- [Google Scholar]
- Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J Knee Surg. 2019;32:804-11.
- [CrossRef] [PubMed] [Google Scholar]
- Bone-patellar tendon-bone versus soft-tissue allograft for anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2016;32:394-402.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of extrinsic plantar flexors on forefoot loading during heel rise. Foot Ankle Int. 1995;16:464-73.
- [CrossRef] [PubMed] [Google Scholar]
- Foot movement and tendon excursion: An in vitro study. Foot Ankle Int. 1994;15:386-95.
- [CrossRef] [PubMed] [Google Scholar]
- Forces acting in the forefoot during normal gait-An estimate. Clin Biomech (Bristol, Avon). 2001;16:783-92.
- [CrossRef] [Google Scholar]
- The role of selected extrinsic foot muscles during running. Clin Biomech (Bristol, Avon). 2004;19:71-7.
- [CrossRef] [PubMed] [Google Scholar]
- The myth of muscle balance. A study of relative strengths and excursions of normal muscles about the foot and ankle. J Bone Joint Surg Br. 1985;67:432-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction with the peroneous longus tendon. Acta Orthop Traumatol Turc. 2008;42:38-43.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med. 2012;40:662-71.
- [CrossRef] [PubMed] [Google Scholar]
- Muscle strength evaluations after ACL reconstruction. Int J Sports Med. 2007;28:868-72.
- [CrossRef] [PubMed] [Google Scholar]
- The long-term contribution of muscle activation and muscle size to quadriceps weakness following total knee arthroplasty. J Geriatr Phys Ther. 2009;32:79-82.
- [CrossRef] [PubMed] [Google Scholar]
- A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: Patellar tendon versus semitendinosus and gracilis tendon graft. Am J Sports Med. 2007;35:729-39.
- [CrossRef] [PubMed] [Google Scholar]
- Tensile strength comparison between peroneus longus and hamstring tendons: A biomechanical study. Int J Surg Open. 2017;9:41-4.
- [CrossRef] [Google Scholar]
- A biomechanical comparison of three lower extremity tendons for ligamentous reconstruction about the knee. Arthroscopy. 2003;19:1091-6.
- [CrossRef] [PubMed] [Google Scholar]
- A biomechanical comparison of fan-folded, single-looped fascia lata with other graft tissues as a suitable substitute for anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:1641-7.
- [CrossRef] [PubMed] [Google Scholar]
- Early post-operative morbidity following anterior cruciate ligament reconstruction: Patellar tendon versus hamstring graft. Knee Surg Sports Traumatol Arthrosc. 2001;9:260-6.
- [CrossRef] [PubMed] [Google Scholar]
- All-inside single-bundle reconstruction of the anterior cruciate ligament with the anterior half of the peroneus longus tendon compared to the semitendinosus tendon: A two year follow up study. J Knee Surg. 2018;31(10):1022-30.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcome of arthroscopic reconstruction of anterior cruciate ligament tear using peroneus longus tendon autograft. Int J Res Orthop. 2018;4:898.
- [CrossRef] [Google Scholar]







