Translate this page into:
Is anterior and posterior ankle impingement under-diagnosed? A review

-
Received: ,
Accepted: ,
How to cite this article: Khurana A, Singh I, Singh MS. Is anterior and posterior ankle impingement under-diagnosed? A review. J Arthrosc Surg Sports Med 2021;2(1):58-65.
Abstract
The impingement of the ankle is diagnosed based on history, clinical signs, physical examination, and conventional radiographic observations and is often a diagnosis of exclusion. Normal X-rays may display spurs, but are mainly useful in the evaluation of other osseous and articular diseases, which may masquerade impingement symptoms. Orthopedic literature seems to embrace the idea that magnetic resonance imaging (MRI) plays a significant role in pre-operative imaging of impingement lesions and MRI is a highly useful method for evaluating acute and chronic foot and ankle disorders. Arthroscopy of the ankle is an important minimally invasive procedure for the treatment of this disease. The majority of patients who have refractory symptoms are treated for ankle impingement using debridement through arthroscopy or an open procedure. According to recent reports, arthroscopic patients for osseous impingement had done better than soft-tissue impingement arthroscopic patients. Ankle arthroscopy has outstanding functional outcomes with few complications and reproducible results. Diagnosis and treatment should be initiated immediately in sportsmen so that the competing athlete can return to sport in an expedient way. The surgeon’s increased suspicion of this disorder is necessary to avoid substantial loss of time and early management. This review highlights the author’s arthroscopic method of impingement resection and discusses the latest available literature on etiopathogenesis, diagnosis, and management of both anterior and posterior ankle impingement. A greater understanding of this disorder can assist the clinician in the early diagnosis and intervention of impingement in sportsmen and dancers. Early diagnosis and intervention are the foundation for successful return to the profession and daily activities.
Keywords
Ankle impingement
Ankle arthroscopy
Posterior ankle impingement syndrome
Footballer’s ankle
Ankle pain
ANTERIOR ANKLE IMPINGEMENT
Introduction
Anterior ankle impingement has been variously described as “athlete’s” ankle and “footballers” ankle in early descriptions before investigation into the etiopathogenesis of the condition and the terminology has since been replaced with anterior ankle impingement syndrome.[1] Restricted ankle dorsiflexion with ankle pain has been the hallmark of this condition and causes of the condition include not just bony but also soft tissues impingement.
Posterior ankle impingement syndrome (PAIS) is a clinical disorder characterized by pain in posterior ankle on performing activities involving forced plantar flexion.[2] PAIS is also referred to as “Os trigonum syndrome” and “posterior tibiotalar compression syndrome.”[3] The condition does not only necessarily arise from bone but also arises from soft-tissue component also. It arises from compression of soft tissues between posterior process of calcaneus and posterior tibia on plantar flexion of ankle which includes the posterior talofibular, intermalleolar, tibiofibular ligaments, and the posterior capsule. Unlike anterior ankle impingement that is common in sportsmen, posterior impingement is commonly seen in dancers.[4] The specific dance position associated with posterior impingement is sustained and frequent high degree plantar flexion (en point or demi-pointe).[5] Other professions involving regular use of such ankle movements include footballers, gymnasts, cricketers, horizontal jumpers, and they commonly experience features of PAIS.[6-8]
Non-operative treatment has been suggested as the initial management for this condition which includes rest, bracing, and physical therapy. In most cases, this is not successful and surgical intervention is warranted.[9-11] Classically, open ankle arthrotomy has been used but has been associated with various complications including excessive scarring, delayed wound healing, and iatrogenic damage to tendons and cutaneous nerves.[12,13] Over time arthroscopic debridement has taken over traditional open approaches with equivalent to better outcomes and lower complication rate.[9,10,14]
The purpose of this study was to appraise the available literature and describe current knowledge regarding ankle impingement, describe the author’s technique for surgical management of various impingement syndromes and simultaneously provide an evidence based review of various treatment options available for managing this under diagnosed and ignored entity.
Etiopathogenesis
Ankle impingement can either be bony or soft-tissue impingement. In addition, impingement can be either anteromedial or anterolateral. Classically, anteromedial impingement is described in sportsmen.[15] It was earlier thought that forceful plantar flexion in athletes to be the most important etiological factor leading to anterior capsular traction and later capsular hypertrophy.[1,9] This was deemed implausible as the capsule is attached more proximal to origin of spurs.[16] This lead to more a recent and plausible explanations including recurrent microtrauma leading to bony impingement of talar neck to distal tibia.[17,18] Moreover, chronic ankle instability is associated with osteophyte formation in medial ankle compartment which originates at the non-weight bearing cartilage rim which occurs most in supination trauma.[19-21]
Anterolateral impingements are mostly post-traumatic. The etiology for anterolateral impingement is more diverse and has been thought to be a result of chronic ankle instability, recurrent micro-trauma, traction, and a myriad of other mechanical factors.[18] Soft-tissue impingement occurs due to hypertrophy of synovium, capsule, and adjoining capsular ligaments which are believed to get entrapped, torn, and inflamed in the lateral gutter of ankle joint. This occurs due to incomplete healing leading to persistent inflammation with subsequent scarring and synovitis.[22] Another explanation for anterolateral impingement is reactive synovitis in the lateral gutter following intra-articular hematoma.[23]
Clinical features
Patients are typically young athletes with persistent ankle swelling, pain, and limited ankle dorsiflexion who often have a preceding history of recurrent ankle sprains.[12,24] The pain is classically exaggerated with kicking, stair climbing, and running. Hyperdorsiflexion causes pain with a false negative test has been frequently reported making it a non-specific finding. Establishing a diagnosis is, thus, dependent a combination of clinical and radiological findings. Location of anteromedial (medial to tibialis anterior tendon) and anterolateral tenderness differentiates the two impingement types clinically.[12] Common differential diagnosis include stress fractures (Tibiotalar), osteochondral lesions (OCD), loose bodies, ankle arthritis, and painful instability. Pain in OCD is deeper and not movement specific unlike impingement pain which is often localized to a superficial plane.
Investigations
Baseline investigations needed in patient suspected of having impingement symptoms is a weight bearing anteroposterior (AP) and lateral X-ray of the ankle that shows findings when there is obvious bone impingement, osteophytes, and reduction in tibiotalar joint space if present.[25] An oblique AMI X-ray has also been described where the beam is tilted in a 45° craniocaudal direction and the leg is rotated 30° in external rotation with foot plantar-flexed. This view has been reported to detect osteophytes in cases with anteromedial impingement when the same cannot be picked up by lateral X-rays.[26]
Magnetic resonance imaging (MRI) shows thickened synovium, anterolateral gutter scarring, and soft-tissue impingement. It is also important to cover differential diagnosis with inversion ankle injuries which include stress fractures (Tibiotalar), OCD, loose bodies, ankle arthritis, and painful instability. Axial T1-weighted images are useful to detect anterolateral gutter scarring while a coronal images can identify injury to anterior band of deltoid ligament which is apparent as thickening and edematous. Variable sensitivities and specificities are described in literature but the authors of present review believe MRI to be the most efficient investigation in cases of suspected anterior ankle impingement [Figure 1].[27-29]

- (a) Lateral ankle radiograph with associated osteophytes from the anterior tibial plafond (solid arrow) and anterior talar neck (outlined arrow), (b and c) axial and sagittal magnetic resonance imaging cuts showing anterior impingement lesion, and (d) arthroscopic view of anterior impingement lesion before debridement (outlined arrow).
CT scan has been described but it does not add much to existing diagnostic modalities. It, however, helps in clear delineation of bony pathologies such as osteophytes, ossicles, and loose bodies.[30] Ultrasound has been investigated by McCarthy et al. and has a high correlation to operative findings to detect soft-tissue hypertrophy and impingement.[31] Pre-operative planning using all feasible investigation should be carried out to distinguish between soft-tissue and bony impingement.
Setup for ankle arthroscopy
Ankle arthroscopy for impingement is carried out under spinal or general anesthesia with the patient placed supine on the operating table. The authors prefer foot at the edge of bed without use of traction for ankle arthroscopy for impingement lesion [Figure 2]. A pouch placed at the edge of the table helps catch the fluid overflow and gravity flow saline is used conventionally. The surgeon stands at the end of the bed looking toward the head with the screen in the line of vision. The authors prefer to use a 4 mm shaver and 4 mm arthroscope which is adequate for most procedures. Some surgeons use smaller arthroscopes which is more of personal preference and as per ones comfort. A long curved and thin (4 mm) beveled osteotome is used which is longer with a broad handle. The osteotome has angled tip which helps get out bone from different positions around the ankle which the authors feel is quite a useful device. A 4 mm round or oval burr which is occasionally used along with occasional use of an arthrowand for soft-tissue debridement.

- (a-c) Arthroscopy portals for anterior ankle arthroscopy used in managing anterior ankle impingement.
Procedure
The anteromedial and anterolateral portals allow for proper visualization during anterior ankle arthroscopy. The first portal is the anteromedial portal which is entered first. One can inject saline depending on one’e comfort which helps in locating the anterolateral portal. The arthroscope is inserted in the medial portal that helps visualize the lateral side well and helps visualize neuro-vascular structures before making the lateral portal. Additional use of the posterolateral portal has been described by some authors.[14] As determined by thorough pre-operative evaluation of radiology, first soft-tissue impingement is removed, followed by removal of bony impingement The gutters are cleared and the osteophytes are shaved with use of osteotome. After major bone is removed, the edges are shaved off with use of a burr. The anteromedial tibia, talus, and medial malleolus are cleared in cases with anteromedial impingement. Similar clearance is carried out anterolaterally. Arthrofibrosis is cleared using a arthrowand as this tissue is fairly strong and its rather hard to remove using a shaver. Occasionally, an 11 number blade can be used to break it up taking care not to damage the articular surface.
Post-operative protocol
Weight bearing is avoided for a couple of days following the procedure with use of crutches to ambulate. Weight bearing is gradually begun with gait training started at 2 weeks and full weight bearing resumed at 4 weeks. Closed lunge maneuvers are avoided for the initial 4 weeks as this is expected to cause inflammation along anterior part of ankle and can promote fibrosis. Open chain exercises, calf relaxation, massage, and range of motion (ROM) exercises are promoted for next 6–8 weeks.
Post-operative failure/complications
Poorly done arthroscopy seldom works and a major cause for second opinions are insufficient clearance and this is along the medial gutter. The surgeon must look along the antermedial gutter when looking at the anterior ankle. Another major cause is post-operative arthrofibrosis and this is commonly due to aggressive physiotherapy, early return to sport or rarely genetic predisposition to arthrofibrosis.
Another reason why arthroscopy does not work is a different diagnosis which includes arthritis, osteochondral defect, ongoing missed instability, and rarely navicular osteophyte or low grade stress fracture of the navicular. This re-emphasizes the need for a proper and detailed pre-operative workup. Recurrent arthrofibrosis can be managed by systemic use of steroids, nonsteroidal anti-inflammatory drugs, gentle mobilization, and steroid injection into the joint that may have to be repeated at 4–6 weeks. Other complications such as complex regional pain syndrome and superficial peroneal nerve neuropraxia have been reported.[22] Complication rate is rather low and has been reported to be under 5%.[32]
Operative outcomes
The results and reported surgical outcomes of arthroscopic resection of anterolateral impingement are good to excellent over mid to long term.[33-38] There is, however, paucity of data for anteromedial impingement resection.[22] van Dijk et al. have compared results of anteromedial to anterolateral impingement resection and have found superior outcomes with anteromedial impingement lesions following surgery.[39]
POSTERIOR ANKLE IMPINGEMENT
Etiopathogenesis
As with anterior impingement syndromes, posterior impingement can be both soft tissue and bony. Major cause of impingement posteriorly is bony and arises due to two very related pathologies which are the “Os trigonum” and stieda process.[40] A secondary ossification center forms at the posterolateral aspect of talus and usually fuses with the posterior talus in adolescence, if this fusion creates a large posterolateral talar process, it is called the stieda process.[41] However, if the same fails to fuse, an os trigonum is formed, which articulates with the talus through a synchondrosis (7–14% cases).[42] The specific dance position associated with posterior impingement is sustained and frequent high degree plantar flexion (en point or demi-pointe). Repetitive plantarflexion trauma is postulated to prevent proper closure of os trigonum ossification center.[43]
Clinical features
Symptomatology consists of posterior ankle pain exacerbated by plantar flexion or dorsiflexion which involves compression and distraction of the injured tissues. Pain is localized on the back of the ankle to anterior to Achilles. There is associated tenosynovitis of the flexor hallucis longus (FHL) tendon.[44]
Patients describe pain and tenderness on the posterolateral aspect of the ankle on active plantar-flexion. Pain is exacerbated with axial loading as well as with great toe dorsiflexion as FHL pushes against the ossicles over its groove along the talus.
Investigations
Conventional radiography including weight bearing AP and lateral views of the ankle is carried out. The lateral view is more helpful in confirming presence of stieda process/os trigonum. This also tells about the size of the pathological lesion. Lateral radiograph in 25° of external rotation gives more detailed information about the size. This is because axis of the talus is not 90°. Size may be under-estimated in neutral rotation. Additional X-ray views are carried out in ankle plantar-flexion.[40]
MRI helps confirm diagnosis and excludes any other pathology in posterior ankle like a cyst or a low lying FHL muscle belly. T2-weighted image shows bone edema, synchondrosis, and soft-tissue signal changes [Figure 3].[43,45]
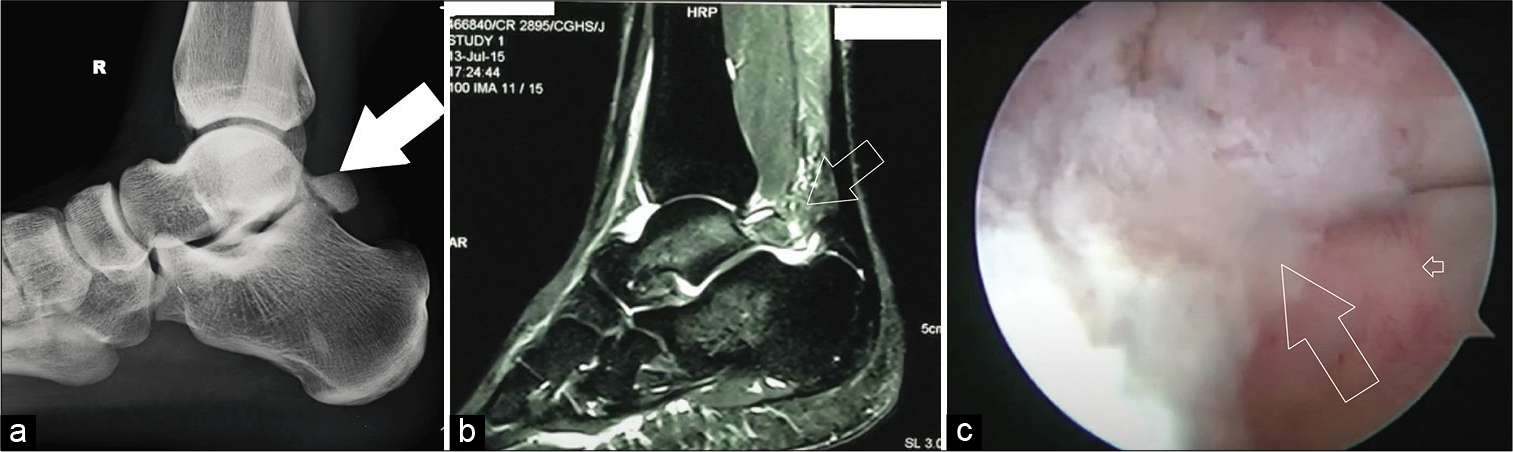
- (a) Lateral ankle radiograph with associated osteophytes from the posterior tibial plafond (solid arrow), (b) Sagittal magnetic resonance imaging showing posterior impingement lesion (outlined arrow), and (c) arthroscopic view of posterior impingement lesion before debridement (outlined arrow).
Treatment options start with physical therapy, activity modification, and ultrasound-guided injections.[46] Athletes looking for fast solutions is candidates for early arthroscopic resection of soft tissue and joint washout. Good symptomatic and functional results have been shown in resistant cases with arthroscopic debridement.[47]
Arthroscopic setup for posterior ankle arthroscopy
The authors of the present study opt for the endoscopic excision of the os trigonum because of reported advantages of minimal scar and good soft-tissue healing, ability to assess, and address any associated intra-articular pathology and the advantage of early return to sports.[48] In prone position under general anesthesia with tourniquet control, surface marking demarcating the Achilles tendon, both malleoli, and the desired portal sites is done [Figure 4].

- Setup for posterior ankle arthroscopy used in managing posterior ankle impingement.
A horizontal line is made from lateral to medial across the Achilles Tendon, starting at the tip of lateral malleolus. Standard poster medial and poster lateral portals were made 5 mm anterior to tendon-Achilles just above the horizontal line. A 4 mm arthroscope and normal saline through a pressure pump set at 40 mmHg pressure are used as the irrigating fluid. Diagnostic endoscopy is first performed.
Surgical technique
The portals are made lateral and medial to the Achilles Tendon. Once the lateral portal is made, nick and spread technique is used. Posteromedial portal is made rather carefully to avoid neurovascular structures.
Arthroscopy photo
A rent has to made in the crural fascia. The crural fascia is removed using a shaver till the subtalar joint space is visualized. The rent in the fascia is slowly enlarged to get the full view of the os trigonum and then of the medially lying tendon of FHL. The tendon acts as an anatomical landmark and use of shaver or burr medial to it carries a high risk of neurovascular injury to the adjacent posterior tibial neurovascular bundle. The soft-tissue around the os trigonum is gradually cleared to obtain a full view of the bony lesion. In the process ligament attachments, namely, talar attachment of posterior talofibular ligament and posterior intermalleolar ligament are released from the bony lesion. Then, with the use of a shaver the os trigonum is gently removed till endoscopy and fluoroscopy confirmed a smooth bony contour on the posterior aspect with no impingement on extreme plantar flexion.
The os trigonum bone is soft and can be easily excised piecemeal with use of a shaver and punch forceps. Another option for debridement is to use a 5 mm osteotome to break the piece en mass or use of a burr may help with removal of the os trigonum. The tendon of FHL is visualized by pulling it in the endoscopic field of vision with the arthroscopic probe. The tendon is examined for changes of tear, split tendon, low lying anomalous muscle belly, or constricting fibrous bands around it which could be the causes of recurrent tendinitis along with the impinging os trigonum. The pulley around the tendon is also released to allow smooth gliding of the tendon. In the process of removal of the os trigonum, the posterior ankle and subtalar joint capsules are also excised which aids in the intra-articular examination of these joints to identify any coexisting pathologies such as OCD and bony osteophytes which can be dealt with at the same time. FHL is an important landmark and it is important to keep lateral to it. Passive movement of great toe confirms FHL identification. Neurovascular structures lie in the fatty tissue medial to FHL.
Post-operative protocol
Initial post-operative management is same as anterior ankle arthroscopy with icing and compression. Gait training with crutches, gentle ROM and core exercises are begun in the first 2 weeks. Patients remain non-weight bearing for the first 2 days with gradual return to full weight bearing by 4 weeks. Once swelling subsides by the 3rd week joint mobilization, gait reeducation and compression manual therapy is initiated. Patients reach full strength by 6–8 weeks; however, return to full training and sports specific drill should begin by 12–14 weeks.[48]
Complications
Complication rates range from 2.3% to 8.5% which include sural nerve injury, injury to medial neurovascular structures, and difficult identification and impalement of FHL.[32,49]
ANKLE IMPINGEMENT AN UNDER-DIAGNOSED ENTITY
Kushare et al. suggest that an average delay of more than 1½ years from the time of the complaint, when patients are diagnosed, indicates that ankle impingement is typically missing from the radar of ankle pain physicians.[50] This is especially true of young patients with PAIS, where the condition is often misdiagnosed. Diagnosis of ankle impingement primarily requires a detailed history and accurate clinical examination complemented by imaging methods. Lack of awareness not only among primary care physicians but also among sports physicians and general orthopedic surgeons, contributes to the delay in presentation to the specialist foot and ankle surgeon. This review highlights the need for improved understanding and clinical diagnosis of this disease by pediatric orthopedic surgeons, pediatricians, primary care athletic doctors, and other doctors interested in the treatment of young athletes to prevent delay in treatment.
CONCLUSION
Ankle impingement is a diagnosis of exclusion based on history, clinical signs, physical assessment, and conventional radiographic findings. Standard ankle radiographs may show “impingement spurs,” but are primarily useful in the assessment of other osseous and articular pathologies that may mimic impingement symptoms. Although lesions associated with soft-tissue impingement can only be detected by cross-sectional imaging, orthopedic literature appears to embrace the notion that MRI plays little role in the pre-operative impingement of the ankle. Sensitivity, specificity, and accuracy of MRI for the diagnosis of soft-tissue impingement are significantly improved by the presence of native joint fluid. Since ankle MRI is not routinely used specifically for the assessment of ankle impingement, ankle arthrography is rarely performed. The same applies to computed tomography arthrography, which is effective in assessing soft-tissue impingement and associated OCD. As a result, soft-tissue impingement is likely to be under-recognized and under-reported in standard imaging practice. Liu et al. argued that although MRI has been established as a very beneficial tool in the assessment of certain acute and chronic foot and ankle disorders, the results of his study show that the physical examination of the patient is very reliable in determining the diagnosis of anterolateral ankle impingement.[29] Ankle arthroscopy provides an effective, minimally invasive method for managing this condition with good to excellent results at a low complication rate. In most cases, ankle impingement is treated with conservative measures, with arthroscopic surgical debridement, or with an open procedure reserved for patients with refractory symptoms.
Chronic anteromedial and posterior ankle pain are a recurrently over-looked entity that often leads to delayed diagnosis and therefore a significant amount of time lost to athletes. The arthroscopic impingement resection delivers excellent functional results, with few complications and reproducible results. Diagnosis and treatment should begin in a timely manner, enabling a competitive athlete to return to sport in a timely manner. Increased suspicion on the part of the surgeon to recognize this condition is essential in preventing a significant loss of time to play without a definitive diagnosis. This review sets out the author’s method of arthroscopic impingement lesion resection and reviews the latest available literature on etiopathogenesis, diagnosis, and management of the condition.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Posterior ankle impingement syndrome. J Am Acad Orthop Surg. 2005;13:365-71.
- [CrossRef] [Google Scholar]
- Management of posterior impingement in the ankle in athletes and dancers. Foot Ankle Int. 2015;36:988-94.
- [CrossRef] [Google Scholar]
- Characteristics and prevalence of musculoskeletal injury in professional and non-professional ballet dancers. Braz J Phys Ther. 2016;20:166-75.
- [CrossRef] [Google Scholar]
- Posterior endoscopic excision of Os trigonum in professional national ballet dancers. J Foot Ankle Surg. 2016;55:927-30.
- [CrossRef] [Google Scholar]
- Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology. 2000;215:497-503.
- [CrossRef] [Google Scholar]
- Soft-tissue and osseous impingement syndromes of the ankle: Role of imaging in diagnosis and management. Radiographics. 2002;22:1457-69.
- [CrossRef] [Google Scholar]
- The management of posterior ankle impingement syndrome in sport: A review. Foot Ankle Surg. 2015;21:1-10.
- [CrossRef] [Google Scholar]
- Anterior ankle pain in sports medicine: Aetiology and indications for arthroscopy. Arch Orthop Trauma Surg. 1991;110:293-7.
- [CrossRef] [Google Scholar]
- Arthroscopy of the ankle and foot. J Bone Joint Surg Am. 1993;75:1233-42.
- [CrossRef] [Google Scholar]
- Os trigonum excision in dancers via an open posteromedial approach. Foot Ankle Int. 2017;38:27-35.
- [CrossRef] [Google Scholar]
- Anterior and posterior ankle impingement. Foot Ankle Clin. 2006;11:663-83.
- [CrossRef] [Google Scholar]
- Excision of os trigonum in dancers via an open posteromedial approach. JBJS Essent Surg Tech. 2018;8:e31.
- [CrossRef] [Google Scholar]
- Advancements in ankle arthroscopy. J Am Acad Orthop Surg. 2008;16:635-46.
- [CrossRef] [Google Scholar]
- Etiology of the anterior ankle impingement syndrome: A descriptive anatomical study. Foot Ankle Int. 2004;25:382-6.
- [CrossRef] [Google Scholar]
- Impingement exostoses of the talus and tibia. J Bone Joint Surg Am. 1957;39:835-920.
- [CrossRef] [Google Scholar]
- The relationship of the kicking action in soccer and anterior ankle impingement syndrome. A biomechanical analysis. Am J Sports Med. 2002;30:45-50.
- [CrossRef] [Google Scholar]
- Anatomical reconstruction and Evans tenodesis of the lateral ligaments of the ankle, Clinical and radiological findings after follow-up for 15 to 30 years. J Bone Joint Surg Br. 2002;84:232-6.
- [CrossRef] [Google Scholar]
- Anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: A 2-to 10-year follow-up, multicenter study. Knee Surg Sports Traumatol Arthrosc. 2000;8:173-9.
- [CrossRef] [Google Scholar]
- Medial ankle pain after lateral ligament rupture. J Bone Joint Surg Br. 1996;78:562-7.
- [CrossRef] [Google Scholar]
- Anteromedial impingement in the ankle joint: Outcomes following arthroscopy. Am J Sports Med. 2010;38:2017-24.
- [CrossRef] [Google Scholar]
- Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med. 1991;19:440-6.
- [CrossRef] [Google Scholar]
- Impingement exostoses of the talus and fibula secondary to an inversion sprain. A case report. Foot Ankle. 1983;3:282-5.
- [CrossRef] [Google Scholar]
- MRI of ankle and lateral hindfoot impingement syndromes. AJR Am J Roentgenol. 2010;195:595-604.
- [CrossRef] [Google Scholar]
- Oblique radiograph for the detection of bone spurs in anterior ankle impingement. Skeletal Radiol. 2002;31:214-21.
- [CrossRef] [Google Scholar]
- Anterolateral impingement of the ankle: Effectiveness of MR imaging. Radiology. 1998;207:357-60.
- [CrossRef] [Google Scholar]
- MRI evaluation of anterolateral soft tissue impingement of the ankle. Foot Ankle Int. 2010;31:655-61.
- [CrossRef] [Google Scholar]
- Diagnosis of anterolateral ankle impingement: Comparison between magnetic resonance imaging and clinical examination. Am J Sports Med. 1997;25:389-93.
- [CrossRef] [Google Scholar]
- Anterolateral ankle impingement: Diagnostic performance of MDCT arthrography and sonography. AJR Am J Roentgenol. 2010;194:1575-80.
- [CrossRef] [Google Scholar]
- Anterolateral ankle impingement: Findings and diagnostic accuracy with ultrasound imaging. Skeletal Radiol. 2008;37:209-16.
- [CrossRef] [Google Scholar]
- Complications in ankle arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2012;20:1420-31.
- [CrossRef] [Google Scholar]
- Arthroscopic treatment of ankle anterior bony impingement: The long-term clinical outcome. Foot Ankle Int. 2014;35:148-55.
- [CrossRef] [Google Scholar]
- Arthroscopic treatment of impingement of the ankle reduces pain and enhances function. Scand J Med Sci Sports. 2002;12:69-72.
- [CrossRef] [Google Scholar]
- Arthroscopic treatment of anterolateral soft tissue impingement of the ankle: Evaluation of factors affecting outcome. Arthroscopy. 2005;21:317-22.
- [CrossRef] [Google Scholar]
- Anterior tibiotalar spurs: A comparison of open versus arthroscopic debridement. Foot Ankle. 1992;13:125-9.
- [CrossRef] [Google Scholar]
- Arthroscopic treatment of anterior ankle impingement. Foot Ankle Int. 1997;18:418-23.
- [CrossRef] [Google Scholar]
- Arthroscopic treatment of soft-tissue impingement of the ankle in athletes. Arthroscopy. 1997;13:492-8.
- [CrossRef] [Google Scholar]
- A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25:737-45.
- [CrossRef] [Google Scholar]
- Surgical outcomes of os Trigonum syndrome in dancers: A case series. Orthop J Sports Med. 2020;8:2325967120938767.
- [CrossRef] [Google Scholar]
- Radiological study of the accessory skeletal elements in the foot and ankle (author's transl) Nihon Seikeigeka Gakkai Zasshi. 1981;55:357-70.
- [Google Scholar]
- MRI features of posterior ankle impingement syndrome in ballet dancers: A review of 25 cases. Clin Radiol. 2004;59:1025-33.
- [CrossRef] [Google Scholar]
- Stenosing tenosynovitis of the flexor hallucis longus tendon and posterior impingement upon the Os trigonum in ballet dancers. Foot Ankle. 1982;3:74-80.
- [CrossRef] [Google Scholar]
- Posterior ankle impingement in the dancer. Curr Sports Med Rep. 2011;10:371-7.
- [CrossRef] [Google Scholar]
- Conservative management of posterior ankle impingement: A case report. J Can Chiropr Assoc. 2016;60:164-74.
- [Google Scholar]
- Treatment of hindfoot and ankle pathologies with posterior arthroscopic techniques. EFORT Open Rev. 2017;2:230-40.
- [CrossRef] [Google Scholar]
- Endoscopic management of posterior ankle impingement syndrome-a case report. J Clin Orthop Trauma. 2017;8:S21-5.
- [CrossRef] [Google Scholar]
- Posterior ankle and hindfoot arthroscopy. JBJS Essent Surg Tech. 2012;2:e15.
- [CrossRef] [Google Scholar]
- Posterior ankle impingement-an underdiagnosed cause of ankle pain in pediatric patients. World J Orthop. 2019;10:364-70.
- [CrossRef] [Google Scholar]






