Translate this page into:
Meniscal root tears: Solving the silent epidemic

*Corresponding author: Robert F. LaPrade, M.D., Ph.D., Complex Knee and Sports Medicine - Twin Cities Orthopedics, 4010 W 65th St, Edina, Minnesota 55423, United States of America. laprademdphd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: LaPrade RF, Floyd ER, Carlson GB, Moatshe G, Chahla J, Monson JK. Meniscal root tears: Solving the silent epidemic. J Arthrosc Surg Sports Med 2021;2(1):47-57.
Abstract
In this review article, the authors describe the most current knowledge surrounding meniscal root tears with a primary focus on diagnosis, management, and implications for the health of the knee joint. Historically overlooked or treated with meniscectomy, meniscal root tears are now known to disrupt the biomechanical role of the meniscus in the joint, leading to the rapid development of knee osteoarthritis. Tears of the medial and lateral posterior meniscal roots are associated with differing etiologies and sequelae, especially in regard to their action as secondary stabilizers of the knee, making root tears an important consideration in ligament reconstruction surgery. We will discuss diagnostic challenges and well-established hallmarks of meniscus tears on imaging, and will conclude by explaining the preferred method for surgical repair of the meniscal roots and appropriate rehabilitation.
Keywords
Meniscus
Meniscal root
Meniscal root repair
Meniscal root tear
Spontaneous osteonecrosis of the knee
INTRODUCTION
Understanding of the functional consequences of meniscal deficiency has evolved over the past several decades. While meniscectomy was once performed as a matter of course, the essential role of the meniscus in preserving the integrity of the knee joint is now clear. Meniscus repair is performed preferentially today, and recognition of the importance of meniscal root tears has been demonstrated by biomechanical and clinical outcome studies which will be discussed in this review. A meniscal root tear is defined as an avulsion of the attachment, or a complete radial tear within 1 cm of the anterior or posterior tibial attachments of the menisci.[1-3] Root tears cause the meniscus to extrude, increasing joint contact pressures and leading to the rapid development of joint space narrowing, subchondral insufficiency fractures (SIFK), and occasionally the hallmark findings of spontaneous osteonecrosis of the knee (SONK) on magnetic resonance imaging (MRI).[1]
Abundant evidence has emerged in recent years tying meniscal root tears to progression of osteoarthritis and demonstrating that non-operative treatment of meniscal root tears is ineffective.[4-9] In a cohort of 197 knees undergoing total knee arthroplasty (TKA), posterior medial meniscal root tears were observed in 78% of patients under 60 years of age undergoing TKA.[10] Chung et al. (2015) observed that at 5-year follow-ups, patients undergoing medial meniscus posterior root repairs had significantly better Lysholm and International Knee Documentation Committee (IKDC) scores, less radiographic evidence of osteoarthritis progression, including joint space narrowing and Kellgren-Lawrence (K-L) grading, and no conversion to arthroplasty compared to meniscectomy.[5] Similarly, Krych et al. (2017) found that unrepaired medial meniscal root tears failed in 87% of patients with a 31% conversion to TKA.[7]
In this review, we describe the incidence, pathology, and long-term consequences of meniscal root tears, as well as diagnostic modalities and the most current methods for repairing these often-neglected forms of meniscal injury.
MENISCAL ROOT TEARS: INCIDENCE AND ETIOLOGY
Tears of the meniscal root have been reported to comprise up to 10–21% of all meniscal tears, making up a significant proportion of all meniscus pathology.[1] It has been reported that, despite the contribution of these injuries to degenerative joint disease,[11,12] they often go undiagnosed at initial presentation.[4,13] Injuries tend to occur in deep squatting/ flexion. There is often a rotatory component, particularly in lateral posterior root tears, and a high proportion of meniscal root tears, particularly lateral root tears, have an associated anterior cruciate ligament (ACL) injury.[13]
Most medial sided lesions occur in the fourth or fifth decade of life, and until recent years many have been treated nonoperatively or with meniscectomy.[14,15] Posterior medial root tears have also been associated with patients who have higher K-L grades of osteoarthritis, varus or valgus deformity depending on the side of the tear.[16] Medial meniscal root tears are often, but not always, seen in older patients, females, and more obese individuals, and tend to be the result of age-related degenerative changes in the meniscus and lower-energy mechanisms.[6,17-19]
Characteristic differences have been observed between medial and lateral tears. Lateral meniscal root tears are more often seen in younger and male patients, with acute traumatic causes and multiple ligamentous injuries. Lateral root tears have also been reported to be 10.3 times more likely to occur concomitantly with ACL tears than medial root tears.[13] The presence of meniscal root tears has been reported concomitantly with 8–12% of ACL tears,[13,20] and 81% of lateral meniscal root tears have been reported to occur together with ACL injuries.[13]
THE MENISCUS: BIOMECHANICAL ROLE IN THE KNEE AND IMPORTANCE OF THE ROOT ATTACHMENTS
The menisci are fibrocartilaginous wedge-shaped structures that play many roles in the knee, including transmitting axial loads across the tibiofemoral articulation, increasing joint congruency, contact area and stability, decreasing contact pressures, and contributing to shock absorption, lubrication, and joint proprioception.[21-26] The essential function of the meniscus in dissipating forces across the joint is enabled by a longitudinal orientation of circumferential collagen fibers which convert compressive forces to circumferential hoop stresses.[21,22] The meniscal root attachments are vital to this role, anchoring the meniscus and preventing extrusion during joint loading.[27] It follows that detachment of the meniscus from one of its roots alters the normal kinematics of the knee, as has been demonstrated by biomechanical studies showing root tears to be equivalent to total meniscectomy.[4] Significant increases in tibiofemoral joint contact pressures have been described with root tears, along with decreased contact surface area.[4,9,25]
Allaire et al. reported that medial meniscal root tears are equivalent to subtotal medial meniscectomy, with increased contact pressures and decreased contact area.[4] Padalecki et al. showed that medial meniscus posterior root repair up to 9 mm from the root restores contact pressures back to normal.[25,28] Structural properties of the roots themselves have been reported to vary by location; the anterior meniscal roots have been measured to be stronger in terms of mean ultimate failure strengths, while the posterior lateral root is reported to be weakest, followed by the posterior medial root.[29-31]
Meniscal root tears must be repaired anatomically, or they will not function normally in the joint.[32] A 5 mm fixation distance from the anatomic site has been reported to make the difference between a functional repair and a nonfunctional, non-anatomic repair.[2] Studies have shown decreases in contact area of the tibiofemoral joint with non-anatomic repair, resulting in increased average contact pressures in knees with non-anatomic posterior medial meniscus root repairs.[2] By contrast, while non-anatomic posterior medial root repairs are functionally equivalent to a medial meniscectomy, anatomic root repairs have been shown to restore normal contact pressures and contact area for both the medial and lateral menisci.[2,25,28,33,34]
MENISCUS ROOT: ANATOMY
For most of the history of knee surgery, the meniscal root attachments were thought of qualitatively in reference to the cruciate ligament attachments. Now, cadaveric studies have demonstrated more precise anatomical relationships, along with the significance of accessory fiber structures which serve to strengthen their connections to the tibial plateau.[35] There are four meniscal roots which anchor the anterior horns of the medial and lateral meniscus (AHMM, AHLM) and the posterior horns (posterior horn of the medial meniscus [PHMM], and PHLM) [Figure 1]. Each of these attachments contains a central bundle of fibers and supplemental attaching fibers.
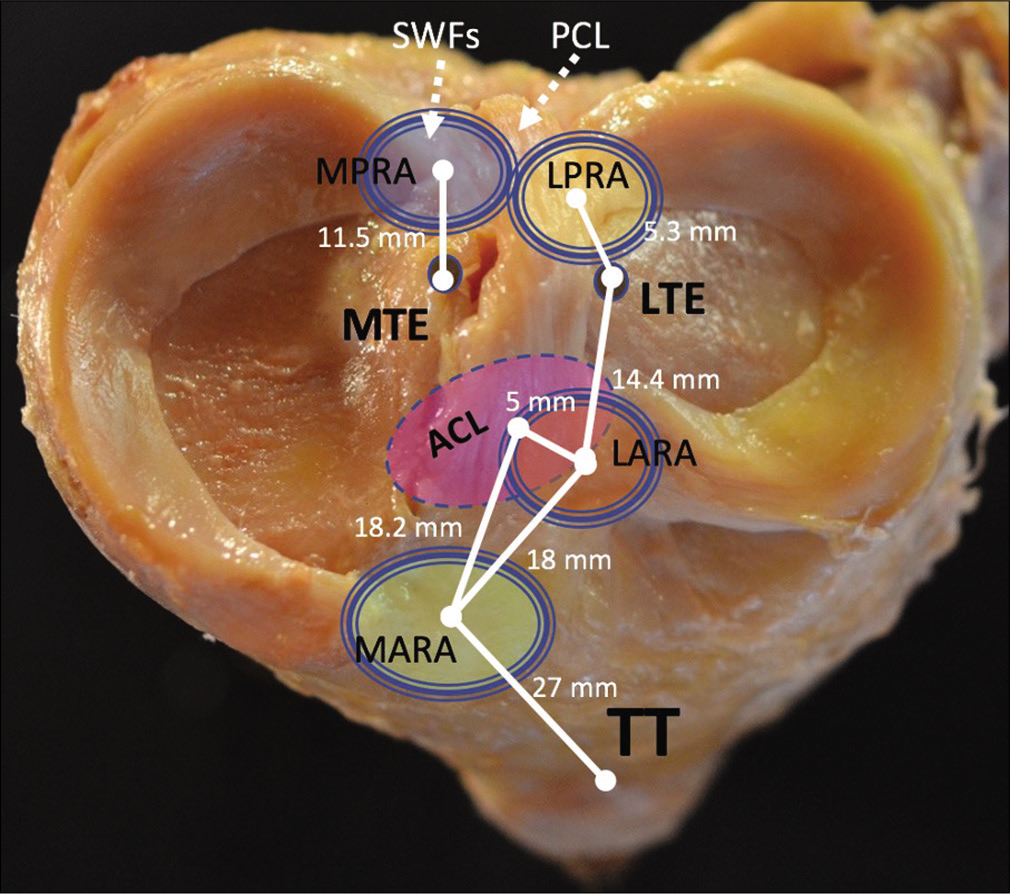
- Medial and lateral tibial plateau. Useful landmarks in relation to meniscal roots are shown. MPRA: Medial posterior root attachment, LPRA: Lateral posterior root attachment, LARA: Lateral anterior root attachment, MARA: Medial anterior root attachment, ACL: Anterior cruciate ligament, TT: Tibial tubercle, MTE: Medial tibial eminence, LTE: Lateral tibial eminence, SWFs: Shiny White fibers of the posterior medial meniscus root, PCL: Posterior cruciate ligament. The distances between meniscal root attachments and landmarks like the MTE, LTE have been established by cadaver studies and are important for anatomic meniscal root repair. Non-anatomic meniscal root repair is often equivalent to meniscectomy in terms of progression to osteoarthritis. Therefore, a precise knowledge of meniscal root anatomy is necessary to reduce the menisci to anatomic position. Sometimes, this requires an extensive release with arthroscopic biters or comparable tools if the menisci have scarred into an extruded position against the capsule. The SWFs and PCL are represented with dashed lines, indicating their attachments are actually inferior to the level of the tibial plateau.
Anterior medial meniscal root
This attachment lies 27.5 mm anterior to the apex of the medial tibial eminence (MTE). The anterior medial root inserts 18.2 mm anteromedial to the tibial ACL attachment, and 4 mm posterior to the anterior rim of the medial tibial plateau. The mean total area of the footprint is 110.4 mm2.[27] Additional supplemental fibers have been reported to be responsible for 43.9% of the native root area, and 28.4% of native root strength.[31] It is important to be aware of the anatomic position of the anterior medial meniscal root attachment because it may be weakened or disrupted during intramedullary tibial nailing, leading to residual pain in some patients.[36]
Anterior lateral meniscal root
The fibers of this attachment interdigitate with the ACL insertion on the tibia. The overlap constitutes 63.2% of the anterior lateral meniscus root attachment and 40.7% of the ACL tibial portion.[27] The fibers in the anterior lateral root are of uniform density (unlike the other roots which have central and supplemental portions). The size of the attachment is 140.7 mm2, and the fibers actually burrow beneath the ACL attachment. The center of the anterior lateral root is 5 mm anterolateral to the center of the ACL attachment, and 13.4 mm anterior to the nearest edge of the posterior lateral root attachment. Injury during anatomic ACL reconstruction may be unavoidable, but the significance of this injury is unclear.[9,31]
Posterior medial meniscal root
The posterior medial root is 11.5 mm posterior to the apex of the MTE and 3.5 mm lateral to the articular cartilage inflection point of the medial plateau, and 8.2 mm anteromedial to the nearest point of the tibial PCL footprint.[35] The medial posterior root has been reported to have a mean area of 30.4 mm2, and the Shiny White Fibers (SWFs), a fibrous expansion of the PHMM, are reported to account for an average of 38.8% of the native root attachment, and a significant (47.8%) proportion of native root strength against ultimate failure load. These SWFs are visible arthroscopically, and are an important landmark for posterior medial meniscus root repair and in PCL reconstruction.[37]
Posterior lateral meniscal root
The lateral posterior root is only 10.1 mm from the lateral anterior root (the medial anterior and posterior roots are much farther apart). The most significant surgical landmark for the posterior lateral meniscus root is its relationship to the LTE. The lateral posterior root is 5.3 mm posteromedial to the apex of the lateral tibial eminence (4.2 mm medial and 1.5 mm posterior), 4.3 mm medial from the lateral articular cartilage edge, and 12.7 mm anterior to the nearest point on the PCL footprint. It is also anterolateral to the medial meniscus posterior root attachment, in keeping with the more circular shape of the lateral meniscus.[35] The posterior lateral root also has supplemental medial fibers, which account for 30.7% of the native root attachment area (83.1 mm2) and 17.6% of the native root strength.[31]
The meniscofemoral ligaments (MFLs, of Wrisberg/ posterior, and Humphrey/anterior) additionally have been reported to stabilize lateral compartment pressures and preserve meniscal function to some degree in cases of an isolated posterior lateral meniscus root tear.[38] These attachments from the PHLM to the intercondylar notch appear to alleviate some of the increased mobility and extrusion seen with posterior medial meniscus root tears, or in posterior lateral root tears with concomitant MFL tears.[3]
MENISCAL ROOTS AND THE ACL
While the ACL is the primary stabilizer against anterior tibial translation (ATT), the lateral meniscal posterior root has been reported by biomechanical studies to serve as a secondary stabilizer of ATT during pivoting in an ACL deficient knee.[9,12] Lateral meniscus root tears have been reported in 12.4% of ACL tears and have been demonstrated to increase tension on the graft in ACL reconstructions.[39-43] A recent study of ACL primary and revision reconstructions analyzed healing rates of meniscal repairs when performed during the first part of two-stage ACL revision reconstructions with bone grafting. The authors found a high incidence of meniscal root tears in both primary (15.5%) and revision (26.2%) ACL cases. The incidence of lateral meniscus posterior root tears was 4 times higher than medial in both primary and revision subsets.[44] The authors also assessed the healing of meniscal tears when repaired during 2-stage ACL revision reconstruction, finding a healing rate of 82.3% for root tears repaired with a transtibial technique. These authors suggest not only that revision ACL cases may have a higher incidence of undiagnosed root tears but that root repair during 2-stage ACL reconstructions yields excellent results.[44]
Another factor known to be associated with poor ACL reconstruction outcomes is increased posterior tibial slope (PTS) of >12°.[42,45-47] Salmon has shown increased PTS to be the most significant factor in ACL reconstruction failure, and Bernhardson demonstrated a linear increase of force on the ACL graft with increasing degrees of PTS.[45,47] In a recent study, Samuelsen et al. explored the relationship between increased PTS, medial meniscal root tears, and ACL graft forces.[42] Their findings reinforced that (1) ACL graft forces are increased in the setting of posterior medial meniscal tears, (2) increased PTS linearly increased forces across the graft, and (3) meniscal root repair restored graft forces to normal when compared to the intact state, and, significantly, that posterior medial meniscal root tears served to potentiate the effects of increased PTS at 30° of flexion.
DIAGNOSIS: CHALLENGES AND HALLMARKS
Meniscal root tears can be difficult to spot on physical examination and imaging and have historically been underdiagnosed.[13] While lateral tears are often associated with trauma or sports, most patients with medial posterior root tears (70%) are not able to recall an inciting event, and only a minority (10–15%) recall any episodes of locking or buckling.[9,16,48,49] Patients may or may not have heard an associated “pop.” It may be difficult to elicit pain from subjects with passive range of motion; deep flexion, especially under load, as in squatting, may be helpful in identifying a posterior root tear in particular. McMurray’s test is sometimes used, though it has poor sensitivity. Some authors have described palpable medial meniscal extrusion with varus force in extension in those with posterior medial root tears.[50] Some combination of positive results from these physical examination maneuvers is present in 50–60% of meniscal root tears.[16] Because of the complementary biomechanical relationship of the lateral meniscus root and ACL, a 3+ Lachman and 3+ pivot shift test during physical examination should raise suspicion for a combined ACL and lateral meniscus posterior root tear.[2,9]
Magnetic resonance imaging (MRI) is the gold-standard for imaging to detect root tears, with a reported specificity of 73%, sensitivity of 77%, positive predictive value of 22%, and negative predictive value of 97%.[49] Several characteristic signs of root tears have been described for MRI, including increased fluid accumulation around the meniscal roots, >3 mm meniscal extrusion on a coronal image from the tibial articular edge, and the so-called “Ghost Sign,” consisting of the absence of an identifiable meniscus on sagittal MRI [Figure 2].[16] Radial tears adjacent to the meniscal root can be observed as linear areas of high signal intensity, perpendicular to the meniscus. Vertical linear defects at the meniscal root itself are referred to as “truncation signs.” These, along with the ghost sign, have all been reported to have a high reproducibility, sensitivity, and specificity in detection of medial meniscus posterior root tears.[8,9,51]
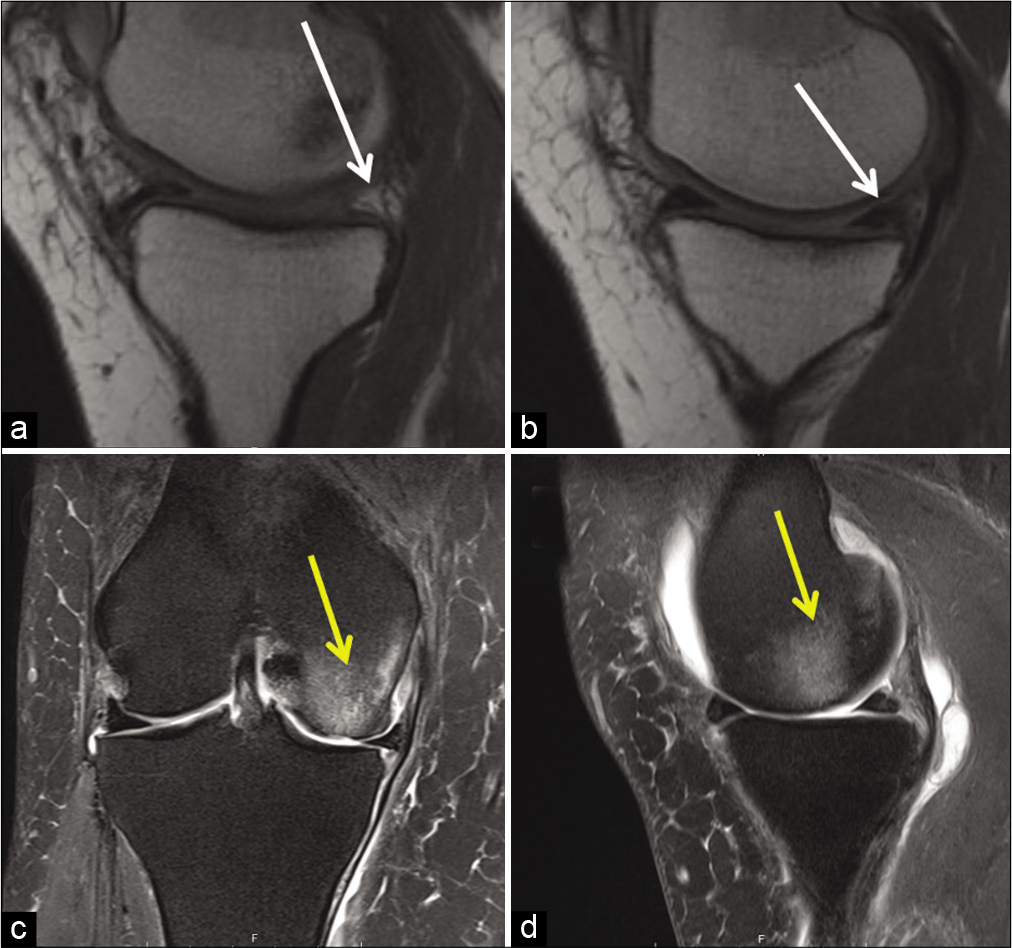
- Magnetic resonance imaging (MRI) is the gold standard for diagnosis of meniscal root tears. Two hallmark radiological signs of posterior root tears can be seen above. (a) Demonstrates a “Ghost Sign,” or lack of radiologic evidence of a meniscus posteriorly (white arrow), contrasted with (b), which shows a normal meniscus on sagittal MRI. (c) Shows a coronal and (d) a sagittal view of bone edema, correlated with a spontaneous osteonecrosis of the knee, or “SONK” lesion (yellow arrow). The term SONK is a misnomer, as the radiologic appearance is caused by edema and subchondral insufficiency fractures in knees with posterior root tears virtually 100% of the time.
A significant development in the identification of root tears on imaging is the growing consensus that SONK lesions seen on MRIs represent the effects of root tears. Historically believed to be idiopathic events, SONK lesions are related to subchondral insufficiency and bone edema that develop after root tears, though the exact pathogenesis remains controversial.[1,48,52-55] Some authors have suggested these bright, ill-defined lesions on MRI be referred to as “subchondral insufficiency fractures,” (SIFK) to better reflect their etiology.[1,52]
Arthroscopy allows for direct visualization of meniscal root tears, extrusion, and cartilage lesions. However, even diagnostic arthroscopy can miss meniscal root tears if the root attachments themselves are not tested with a probe, along with the stability of the meniscal body. Therefore, it is recommended to probe every meniscal root to ensure its firm attachment.
CLASSIFYING MENISCAL ROOT TEARS
Meniscal root lesions are divided into five types based on a system described by LaPrade et al. [Figure 3].[3] The most common is a Type 2 tear, consisting of a complete radial tear within 9 mm of the center of the meniscal root attachment. These are further divided into 2A (complete radial tears to <3 mm from the center of the meniscal root), 2B (3–6 mm from the root), and 2C (6–9 mm from the root). Anterior root injuries occur far less frequently (5/71 knees in LaPrade et al., 2014) and have been observed to be mostly Type 5 bony avulsion fractures of the anterior lateral meniscus root. Type 3 tears, involving a combined complete radial tear at the root and a bucket-handle tear, are quite difficult to repair and most often present acutely. Descriptions of the other types are given in [Figure 3]. This classification system is applied to medial and lateral posterior meniscal root tears.[3] A posterior root tear classification system for the lateral meniscus was additionally proposed by Forkel et al. to take into account the stabilizing effects of the meniscofemoral ligaments in the lateral compartment.[56]
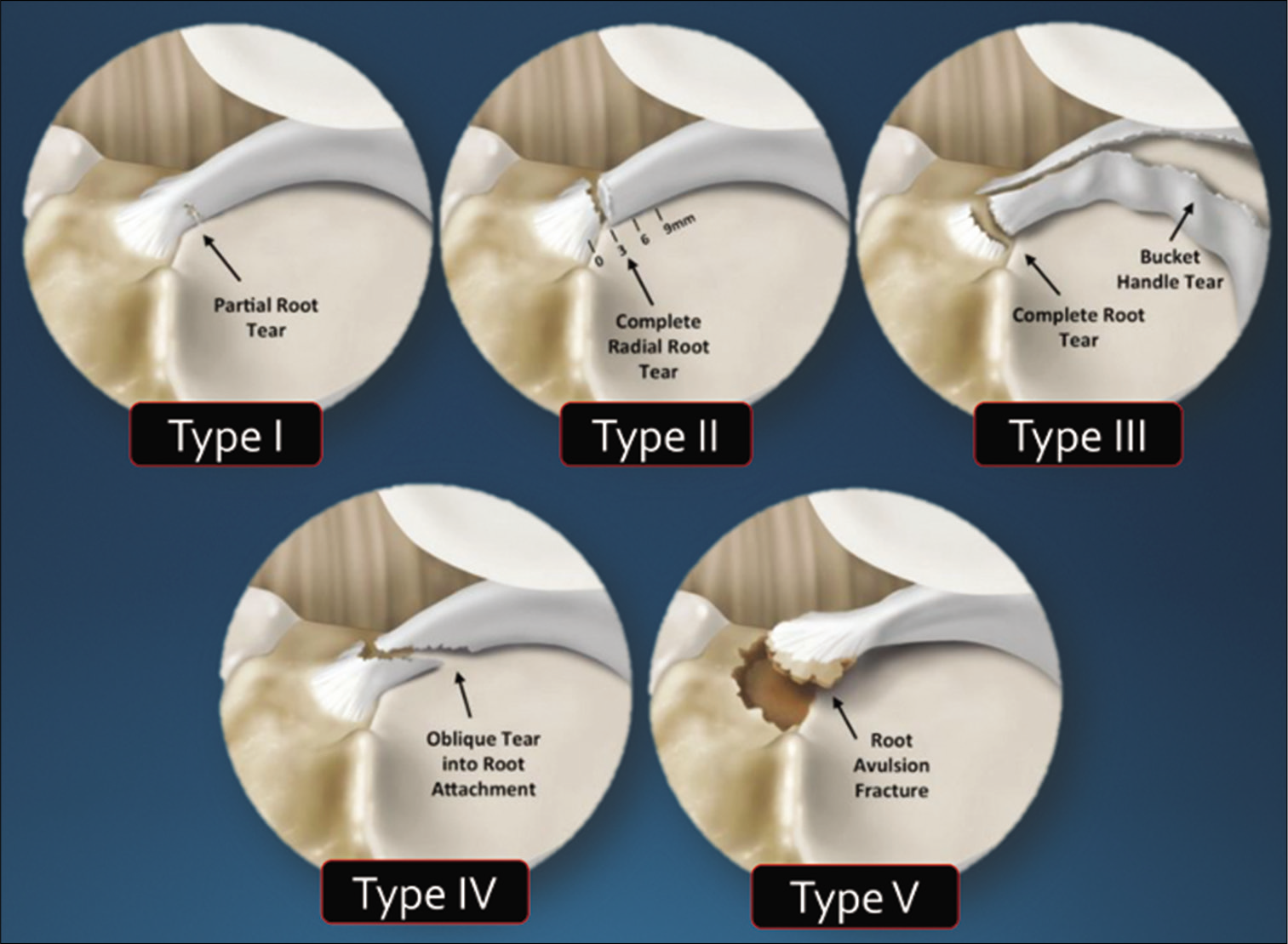
- Classification of meniscal root tears according to LaPrade (2014). Type 1 tears are partial, stable root tears. Type 2, the most common, is complete radial tears near the root attachment, subdivided into types A, B, and C, according to whether they are <3 mm, 3–6 mm, or 6–9 mm from the center of the attachment, respectively. Type 3 are “disaster tears,” involving a bucket-handle tear with a complete root detachment. Type 4 tears are oblique tears propagated into the root attachment, and Type 5 tears are bony avulsions, and may present chronically as meniscal ossicles.
MENISCAL ROOT REPAIR: TRANSTIBIAL TUNNEL PULLOUT TECHNIQUE = GOLD STANDARD
Non-operative treatment
Treatment of meniscal root tears is aimed at preventing development of osteoarthritis by restoring normal joint contact pressures and kinematics. Therefore, while saving the meniscus is desirable, in patients with severe cartilage degeneration (Outerbridge Grades III-IV), especially in the elderly, obese or patients who are poor surgical candidates, non-operative treatment may be reasonable. This typically consists of non-opioid analgesics, physical therapy, activity modification, and unloader bracing for symptomatic relief.[9] Exercise-based interventions with physical therapy, focused on quadriceps strength and overall fitness, have shown comparable outcomes to arthroscopic meniscectomy in older patients with degenerative meniscal tears;[57-59] however, such interventions have not been investigated in the context of meniscal root tears. Given the disruptive impact of a root tear on the overall function of the meniscus, more immediate surgical intervention is advocated with a comprehensive course of physical therapy following surgery to restore strength, function, and overall cardiovascular fitness.[7,60]
Meniscectomy
A recent study reported that for medial meniscus root tears, meniscus repair, meniscectomy, and non-operative treatment resulted in progression to osteoarthritis in 53.0%, 99.3%, and 95.1% of patients, respectively.[60] Meniscectomy led to arthritis more often than non-operative treatment, and from an economic perspective meniscal root repair has been shown to be a cost-saving intervention.[60] Other studies have additionally linked non-operative management or meniscectomy in the treatment of meniscal root tears to poor clinical outcomes and conversion to TKA.[5,7] Removal of the meniscus is now rarely indicated, except in advanced degenerative tears or those causing mechanical symptoms for the patient – though progression to osteoarthritis can be expected.[9]
Additional considerations: Varus alignment
Varus alignment may present a complicating factor in some patients. There is no clearly defined circumstance in which a patient should undergo concurrent proximal tibial osteotomy (PTO) and medial meniscal root repair. In the authors’ practice, if a patient presents with minimal or no radiographic signs of medial compartment arthritis, proceeding solely with root repair is felt to be adequate.
In general, for patients who may be over 55 years of age, performing a concurrent PTO increases the difficulty of the recovery process and increases the risk of lateral hinge fracture or delayed union. The authors have found that treating these patients with a medial unloader brace once they initiate weight bearing at 6 weeks after a root repair helps to unload the repair and leads to successful outcomes. The amount of arthritis of the affected compartment and the status of the ipsilateral compartment articular cartilage should be assessed and consideration may be given to an unloading osteotomy concurrent with the meniscal root repair.
Repair
While other techniques have been described in specific circumstances, such as use of suture anchors,[61,62] the gold-standard for root repair is a transtibial pullout technique [Figure 4].[63-66] This technique uses tibial tunnels which are used to re-anchor the meniscal root to the tibial plateau by passing sutures through the meniscal root and retrieving them through the tunnels. The preferred technique of the authors uses a curved curette to first debride the tibial attachment site to bleeding bone to facilitate healing. Trephination of the MCL with a spinal needle has been used by some authors to facilitate access to the back of the joint without damaging articular cartilage.[67]
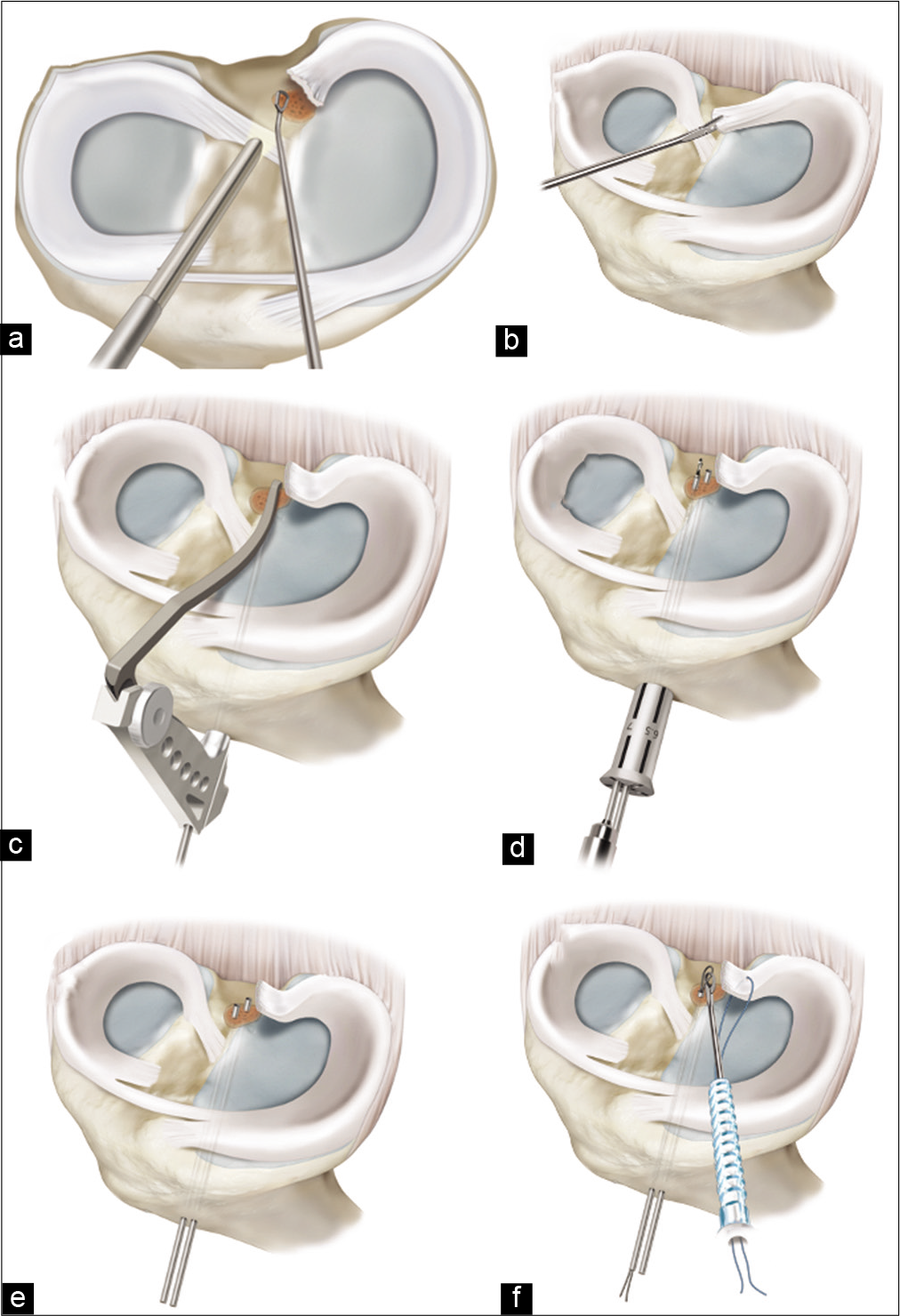
- Illustration of an anatomic two-tunnel transtibial medial meniscus posterior root repair. (a) The torn attachment site is prepared to a bleeding bone bed using a curved curette. (b) Sutures are placed through the detached root of the meniscus (c) a cannulated guide is used to drill two transtibial tunnels from just adjacent to the ipsilateral side of the tibial tubercle to the anatomic attachment site of the root on the tibial plateau. (d) An offset is used to drill the tibial tunnels 5 mm apart. (e) The cannulas are left in place in the tibial tunnels to facilitate (f) passage of two simple sutures using suture passers.
A 3-cm incision is then made adjacent to the tibial tubercle on the ipsilateral side to the meniscal tear. A cannulated aiming device and offset are used to drill two transtibial tunnels 5 mm apart, and then a tibial tunnel guide is used to ream the tunnels. The cannulas are left in place to facilitate suture passage. Anatomic positioning of the tunnels within the posterior root attachment site should be visualized arthroscopically. Two simple sutures are passed through the meniscal root, and shuttled down the more posterior or anterior tibial tunnel (one for each).[68] A cannula is often used to facilitate passage and avoid catching a soft tissue bridge. While different arrangements of mattress sutures or modified Mason-Allen arrangements have been proposed for anchoring the meniscal roots, two simple sutures are accepted as producing the least displacement and maintaining the highest stiffness in the repair construct.[69] The damaged root must be reduced to its anatomic attachment site; in the case of a chronic injury the meniscus may be scarred into an extruded position and a peripheral meniscocapsular release may be required for anatomic reduction.[2,68] Once reduction of the root is accomplished, the sutures through the tibial tunnel are tied over a button (or some kind of cortical fixation device) on the anterior tibia to avoid suture cut-in [Figure 5].[68]
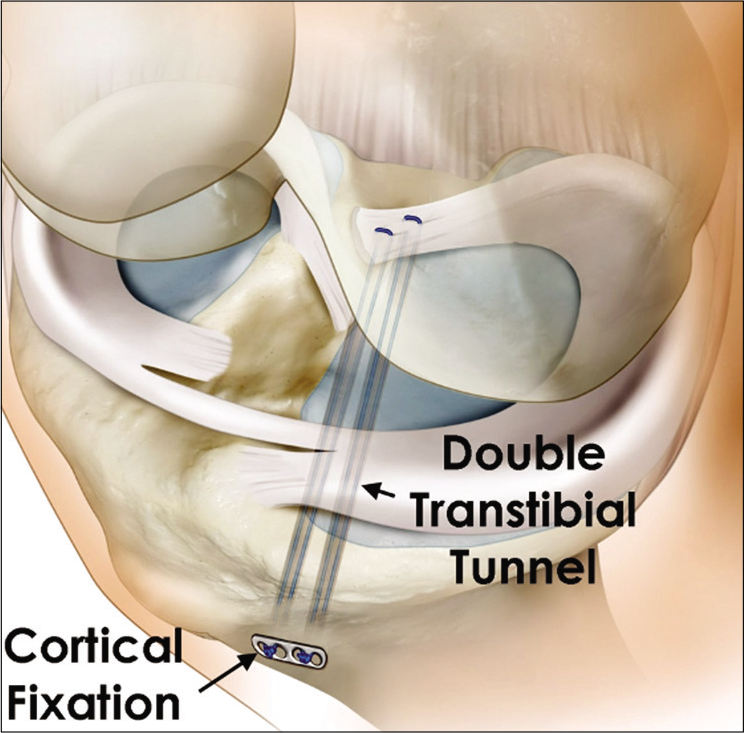
- Cortical fixation of transtibial meniscal root repair. After creating two transtibial tunnels, passing sutures through the detached root of the meniscus and down the tibial tunnels, the sutures are tensioned to reduce the root of the meniscus to anatomic position. Non-anatomic root repairs do not restore normal joint biomechanics, nor do they halt the progression of osteoarthritis. The sutures are then tied over the anterior tibial cortex using a button or cortical fixation device to prevent cut-in to the bone.
REHABILITATION
After surgical repair of a meniscal posterior root, the patient should remain non-weightbearing for a minimum of 6 weeks. During the first 2 weeks postoperatively, early joint range of motion is advocated for joint nutrition but is limited to 90 degrees of flexion, as progression into deeper flexion increases peak contact pressure and posterior extrusion forces at the posterior meniscal root.[70,71] Motion into knee flexion is performed passively for the first 6 weeks to avoid hamstring pulling forces, specifically through the semimembranosus attachment at the posterior knee joint capsule, adjacent to the posterior medial meniscus. At 6 weeks, if the patient is progressing well, they gradually progress toward full weightbearing over a 2–3 week period and may consider wearing an unloader brace to modulate medial compartment loading. Aggressive resisted hamstring curling into knee flexion and deeper squatting beyond 70 degrees of knee flexion should be avoided during the first 4 months postoperatively to avoid excessive tension and loading at the healing meniscus root repair.[72-74] Physical therapy should follow a stepwise progression, specifically addressing quadriceps muscle strength, general strengthening for all lower extremity muscle groups, joint proprioception and overall postural stability, and cardiovascular fitness with low impact activities.[75]
OUTCOMES OF MENISCAL ROOT REPAIR
This transtibial repair technique is reported to restore to normal contact mechanics in most cases.[25] LaPrade et al. reported on a cohort of 45 knees, with improvements in Lysholm, SF-12 PCS and SF-12 MCS, and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores after transtibial tunnel root repair, with no significant differences in functional outcome scores between patients <50 years of age and >50 years of age.[68] Lysholm scores increased by an average of 40 points in lateral meniscus posterior root repairs (35 pre-operative to 75 post-operative) and 30 points for medial meniscus posterior root repairs. WOMAC pain/disability scores decreased by 42 in the lateral group and 26 in the medial group after repair with the transtibial pull-out method. Patients at a mean age of 55 experienced an average 32 point improvement in Lysholm scores, while a comparative meniscectomy cohort had only a 12 point improvement postoperatively. Lee et al. reported on a cohort of 27 knees, using second-look arthroscopy to verify healing of meniscal root repairs. They found the mean Hospital for Special Surgery (HSS) score improved from 61.1 preoperatively to 93.8 at 2 years, and the mean Lysholm score improved from 57.0 preoperatively to 93.1 at 2 years postoperatively.[76] Another meta-analysis[77] and systematic review[6] reported similar improvements in functional and subjective scores after surgical repair of meniscus tears.
One lingering issue with meniscal root repair is the phenomenon of post-operative extrusion of the meniscus, which has been observed on MRI and of itself can lead to osteoarthritis.[78-81] A recent biomechanical study examined meniscal extrusion and the success of anatomic transtibial pullout suture techniques in restoring normal joint contact mechanics. The authors found that a central (peripheral) stabilization suture in an anatomic repair does not by itself significantly eliminate extrusion, but may be useful clinically in the long-term and for chronic tears.[79]
CONCLUSION
Meniscal root tears have been called a “silent epidemic.”[1] Much progress has been made since meniscectomy was the treatment of choice for meniscal tears. Meniscectomy, non-operative management, and non-anatomic repair are recognized to be ineffective at restoring the native kinematics of the joint, and fail to stop progression to osteoarthritis. Awareness of root tears and how to spot them has improved, but is far from perfect. The results of many years of research and the work of many authors argue unequivocally for repairing meniscal root tears when possible. Finding root tears can be difficult, even on MRI. Recognizing radiological signs closely correlated with root tears, such as the “ghost sign,” SONK lesions, and peripheral extrusion of the meniscus can help the practitioner spot these injuries, along with a thorough clinical exam and history.[76] Surgical repair has been described with excellent results using a transtibial tunnel pull-out technique, with anatomic reduction of the meniscus and fixation on the anterior tibia. Even with anatomic fixation, extrusion remains a problem and more work is needed to elucidate whether an additional stabilization suture is a practical solution to this issue in the long term. After surgery, patients must not neglect to follow an appropriate rehabilitation regimen.
And probe every root attachment!
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
Robert F. LaPrade MD, PhD: Consultant for Arthrex, Ossur, Smith and Nephew and Linvatec Royalties: Arthrex, Ossur and Smith and Nephew Research grants; Smith and Nephew and Ossur Editorial Boards: AOSSM, JEO and KSSTA Committees: AOSSM, AANA, ISAKOS Jorge Chahla MD, PhD: Consultant for Arthrex, Ossur, Smith and Nephew and CONMED Royalties: Elsevier Research grants; Arthrex,CONMED, Smith and Nephew and Ossur Editorial Boards: Arthroscopy and AJSM. Committees: AOSSM, AANA, ISAKOS, ESSKA.
References
- Meniscal root tears: A silent epidemic. Br J Sports Med. 2018;52:872-6.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43:912-20.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363-9.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a tear of the posterior root of the medial meniscus, Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922-31.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: A minimum 5-year follow-up. Arthroscopy. 2015;31:1941-50.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: A systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31:1808-16.
- [CrossRef] [PubMed] [Google Scholar]
- Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25:383-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23:152-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical evaluation of the root tear of the posterior horn of the medial meniscus in total knee arthroplasty for osteoarthritis. Knee Surg Relat Res. 2015;27:90-4.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:1439-43.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: A biomechanical study. Orthop J Sports Med. 2017;5:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior meniscus root tears: Associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23:3127-31.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical techniques and outcomes of repairing meniscal radial tears: A systematic review. Arthroscopy. 2016;32:1919-25.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal repair outcomes at greater than five years: A systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94:2222-7.
- [CrossRef] [PubMed] [Google Scholar]
- An evidence-based approach to the diagnosis and treatment of meniscal root tears. Minerva Ortop Traumatol. 2017;68:81-90.
- [Google Scholar]
- Medial versus lateral meniscus root tears: Is there a difference in injury presentation, treatment decisions, and surgical repair outcomes? Arthroscopy. 2020;36:1135-41.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40:1606-10.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of arthroscopic posterior medial meniscus root repair: Association with body mass index. J Am Acad Orthop Surg. 2019;27:104-11.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: A missed epidemic? How should they be treated? In: The Menisci. Berlin: Springer; 2017. p. :49-61.
- [CrossRef] [Google Scholar]
- Engineering the Knee Meniscus. United States: Morgan Claypool Publishers, Rice University; 2009.
- [CrossRef] [Google Scholar]
- Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92:1398-408.
- [CrossRef] [PubMed] [Google Scholar]
- A novel repair method for radial tears of the medial meniscus: Biomechanical comparison of transtibial 2-tunnel and double horizontal mattress suture techniques under cyclic loading. Am J Sports Med. 2016;44:639-45.
- [CrossRef] [PubMed] [Google Scholar]
- The basic science of human knee menisci: Structure, composition, and function. Sports Health. 2012;4:340-51.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42:699-707.
- [CrossRef] [PubMed] [Google Scholar]
- Proprioception following partial meniscectomy in stable knees. Knee Surg Sports Traumatol Arthrosc. 2011;19:207-13.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of the anterior root attachments of the medial and lateral menisci: A quantitative analysis. Am J Sports Med. 2014;42:2386-92.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical consequences of a tear of the posterior root of the medial meniscus, Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):257-70.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root suturing techniques: Implications for root fixation. Am J Sports Med. 2011;39:2141-6.
- [CrossRef] [PubMed] [Google Scholar]
- Geometry, time-dependent and failure properties of human meniscal attachments. J Biomech. 2010;43:463-8.
- [CrossRef] [PubMed] [Google Scholar]
- Structural properties of the meniscal roots. Am J Sports Med. 2014;42:1881-7.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: A biomechanical study. Arthroscopy. 2010;26:358-65.
- [CrossRef] [PubMed] [Google Scholar]
- Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471-9.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24:1469-77.
- [CrossRef] [PubMed] [Google Scholar]
- Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342-7.
- [CrossRef] [PubMed] [Google Scholar]
- Intramedullary tibial nailing reduces the attachment area and ultimate load of the anterior medial meniscal root: A potential explanation for anterior knee pain in female patients and smaller patients. Am J Sports Med. 2015;43:1670-5.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic double-bundle posterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e149-56.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: Efficacy of different repair techniques. Arthroscopy. 2014;30:833-40.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29:226-31.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591-7.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med. 2016;44:3126-31.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior medial meniscus root tears potentiate the effect of increased tibial slope on anterior cruciate ligament graft forces. Am J Sports Med. 2020;48:334-40.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral meniscal root tears associated with anterior cruciate ligament injury: Classification and management (SS-70) Arthroscopy. 2004;20:e32-3.
- [CrossRef] [Google Scholar]
- Incidence and healing rates of meniscal tears in patients undergoing repair during the first stage of 2-stage revision anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47:3389-95.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial slope and its effect on force in anterior cruciate ligament grafts: Anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med. 2019;47:296-302.
- [CrossRef] [Google Scholar]
- Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:1529-36.
- [CrossRef] [PubMed] [Google Scholar]
- 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: The catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46:531-43.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016-30.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus posterior root tear: A comprehensive review. Knee Surg Relat Res. 2014;26:125-34.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2011;19:2072-5.
- [CrossRef] [PubMed] [Google Scholar]
- Radial meniscal tears: Significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005;185:1429-34.
- [CrossRef] [PubMed] [Google Scholar]
- The role of meniscal tears in spontaneous osteonecrosis of the knee: A systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47:501-7.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of medial and lateral meniscus root tears. PLoS One. 2015;10:e0141021.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal root injury and spontaneous osteonecrosis of the knee: An observation. J Bone Joint Surg Br. 2009;91:190-5.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal extrusion and spontaneous osteonecrosis with root tear of medial meniscus: Comparison with horizontal tear. Arthroscopy. 2013;29:726-32.
- [CrossRef] [PubMed] [Google Scholar]
- Different patterns of lateral meniscus root tears in ACL injuries: Application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23:112-8.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors, diagnosis and non-surgical treatment for meniscal tears: Evidence and recommendations: A statement paper commissioned by the Danish society of sports physical therapy (DSSF) Br J Sports Med. 2018;52:557-65.
- [CrossRef] [PubMed] [Google Scholar]
- Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: Randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of exercise type and dose on pain and disability in knee osteoarthritis: A systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66:622-36.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: Clinical and economic effectiveness. Am J Sports Med. 2019;47:762-9.
- [CrossRef] [PubMed] [Google Scholar]
- Suture anchor repair for a medial meniscus posterior root tear combined with arthroscopic meniscal centralization and open wedge high tibial osteotomy. Arthrosc Tech. 2018;7:e755-61.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscal root repair using curved guide and soft suture anchor. Clin Orthop Surg. 2018;10:111-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006;22:795.e1-4.
- [CrossRef] [PubMed] [Google Scholar]
- A pull out suture for transection of the posterior horn of the medial meniscus: Using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15:1510-3.
- [CrossRef] [PubMed] [Google Scholar]
- A new surgical technique for arthroscopic repair of the meniscus root tear. Knee Surg Sports Traumatol Arthrosc. 2009;17:1433-6.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical evaluation of a transtibial pull-out meniscal root repair: Challenging the bungee effect. Am J Sports Med. 2014;42:2988-95.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous medial collateral ligament release in arthroscopic medial meniscectomy in tight knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:1540-5.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884-91.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical evaluation of different suture materials for arthroscopic transtibial pull-out repair of posterior meniscus root tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:132-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37:124-9.
- [CrossRef] [PubMed] [Google Scholar]
- Medial meniscus posterior root tear induces pathological posterior extrusion of the meniscus in the knee-flexed position: An open magnetic resonance imaging analysis. Orthop Traumatol Surg Res. 2018;104:485-9.
- [CrossRef] [PubMed] [Google Scholar]
- Rehabilitation following meniscal root repair: A clinical commentary. J Orthop Sports Phys Ther. 2016;46:104-13.
- [CrossRef] [PubMed] [Google Scholar]
- Measurement of meniscofemoral contact pressure after repair of bucket-handle tears with biodegradable implants. Arch Orthop Trauma Surg. 2005;125:254-60.
- [CrossRef] [PubMed] [Google Scholar]
- Internal pressure of human meniscal root attachments during loading. J Orthop Res. 2013;31:1507-13.
- [CrossRef] [PubMed] [Google Scholar]
- Knee pain and mobility impairments: Meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48:A1-50.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: Radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25:951-8.
- [CrossRef] [PubMed] [Google Scholar]
- A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24:1455-68.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556-63.
- [CrossRef] [PubMed] [Google Scholar]
- Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019;47:1591-600.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29:295-301.
- [CrossRef] [PubMed] [Google Scholar]
- Increased extrusion and ICRS grades at 2-year follow-up following transtibial medial meniscal root repair evaluated by MRI. Knee Surg Sports Traumatol Arthrosc. 2018;26:2826-34.
- [CrossRef] [PubMed] [Google Scholar]







