Translate this page into:
Modified technique for medial patellofemoral ligament reconstruction – Its outcome with 2-year follow-up

*Corresponding author: Vatsal Khetan, Department of Sports Medicine, Sportsmed, Mumbai - 400 025, Maharashtra, India. drvatsalortho2015@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khetan V, Sabnis B, Usman S, Joshi A. Modified technique for medial patellofemoral ligament reconstruction – Its outcome with 2-year follow-up. J Arthorsc Surg Sport Med 2021;2(1):26-33.
Abstract
Objectives:
The purpose of this study was to present our modified technique for MPFL reconstruction. We also present its functional outcome, complications, and patients’ satisfaction from the procedure.
Materials and Method:
This study is a retrospective analysis of prospectively collected data during the period of July 2015 and March 2019. Forty cases in patients with recurrent symptomatic patellar instability without a patellar fracture and who underwent isolated MPFL reconstruction were included in the study. Kujala scoring was done to assess the functional outcome at follow-up. Post-operative dislocation and apprehension were recorded in each case along with any complication. Patients were asked to complete a subjective questionnaire postoperatively during follow-up, to assess their satisfaction with the surgical procedure.
Results:
Pre-operative Kujala score was 45.85 which improved to 92.72 postoperatively at the time follow-up. The improvement in Kujala score was found to be highly significant (P < 0.01). Subjective assessment of the procedure: 72.5% of the patients had an excellent outcome. About 15% of the patients had a good outcome whereas 10% had a fair outcome. Only one patient had a poor outcome.
Conclusion:
In properly selected patients with recurrent patellar instability, isolated MPFL reconstruction appears to be a safe and efficient surgical procedure for the stabilization of patella, with a low failure rate. Consistent good results with early rehabilitation can be obtained using suture anchors to fix the implant on patella and using the described technique.
Keywords
Medial patellofemoral ligament technique
Suture anchors
Gracilis
INTRODUCTION
The medial patellofemoral ligament (MPFL) is a vital structure in the knee joint that provides stability to patella during movement of the knee. It acts as a check rein ligament which prevents patellar dislocation during early flexion of the knee before the patella engages in the trochlea.[1]
In addition, being a passive stabilizer, MPFL plays a role in patellar stabilization irrespective of any structural malalignment. Patellofemoral dislocations are commonly seen with a sudden quadriceps contraction in a valgus knee, when the knee is flexed over an externally rotated tibia.[2]
Recurrent patellar dislocation is a multifactorial phenomenon. Factors that contribute to it include patellar and femoral morphology and lower limb alignment in three planes.[3] MPFL reconstruction is the procedure of choice if the patient experiences patellofemoral dislocation despite adequate, non-surgical rehabilitation following a primary patellofemoral dislocation.
Usually, patients are advised to strengthen the knee joint, especially the vastus medialis, to regain knee joint stability. However, if they experience patellofemoral dislocation despite this, they are advised to undergo MPFL reconstruction.[4,5]
While there are various techniques for reconstruction that use different grafts and fixation methods,[6] most of them involve the use of procedures involving the bone, such as trochleoplasty, medialization, or anteromedialization of the tibial tuberosity. In this study, we have included patients who have undergone an isolated MPFL reconstruction. We have chosen patients with recurrent and habitual patellofemoral dislocations and performed MPFL reconstruction using gracilis autograft.
The purpose of this study was to present our modified technique for MPFL reconstruction. We also present its functional outcome, complications, and patients’ satisfaction from the procedure.
MATERIALS AND METHODS
Study design
This study is a retrospective analysis of prospectively collected data of consecutive 58 patients who underwent MPFL reconstruction during the period between July 2015 and March 2019. The surgeries were performed by a single surgeon (BS), following the same technique.
Level of evidence-4
Informed consent was taken from all the patients.
Patients with recurrent symptomatic patellar instability without a patellar fracture who underwent isolated MPFL reconstruction were included in the study. This left us with 40 knees, after we excluded patients who underwent any concurrent distal or proximal realignment procedure distal femoral osteotomy (DFO) or tibial tubercle transfer due to other structural abnormality [Figure 1].
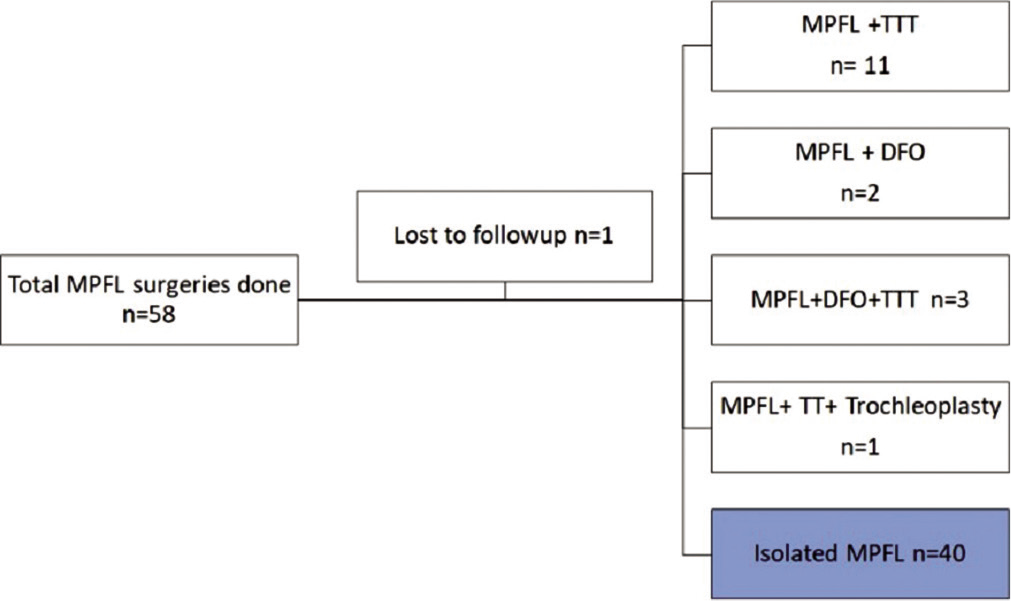
- Flowchart showing patient selection.
Clinically, patellar instability was assessed and confirmed based on the history of the patient and physical examination of the knee. Apprehension test, patellar tilt and patellar tracking were examined in every case. The Staheli rotation profile[7] was assessed in each patient. Radiologically, patellar height, trochlear dysplasia, patellar tilt, Q-angle, and tibial tubercle-trochlear groove (TT-TG) distance were measured to decide the surgical procedure. A scanogram was done to see the alignment. A specific algorithm was followed in managing recurrent patellar dislocations.
Pre- and post-operative Kujala scoring was calculated in each case.
In patients that had the Mikulicz point > 65% of the scale (valgus alignment), a medial closing wedge DFO was done to correct the alignment. If the TT-TG distance was more than 2 cm, a TT transfer to medialize the TT was done. In patients who had a Dejour trochlea Type 3 or 4, we performed a trochleoplasty.
Caton-Deschamps index was measured and if it was found to be > 1.2, a distalization ± medialization of the TT was performed. If the patient had a femoral internal rotation (> 20°), we performed a distal femoral derotation osteotomy. All of these procedures were combined with MPFL reconstruction using the same surgical technique as described. If, however, all the other parameters were within acceptable limits, isolated MPFL reconstruction was performed. Only patients who underwent isolated MPFL reconstruction were included in the study.
Postoperatively, patients were followed up at 6 weeks, 3, 6, and 12 months, and then annually. Clinical evaluation at follow-up was done by patellar tracking and apprehension test.
Kujala scoring was done to assess the functional outcome at follow-up. Post-operative dislocation and apprehension were recorded in each case along with any complication. Patients were asked to complete a subjective questionnaire postoperatively[8] during follow-up, to assess their satisfaction with the surgical procedure.
Recurrence of patellar dislocation after surgery was considered as a failure.
One patient was lost to follow up. She was from another country and was not reachable despite our best efforts to contact her through telephone, email, and letter.
Surgical technique
All surgeries were performed by a single surgeon (Author-2) using the same technique.
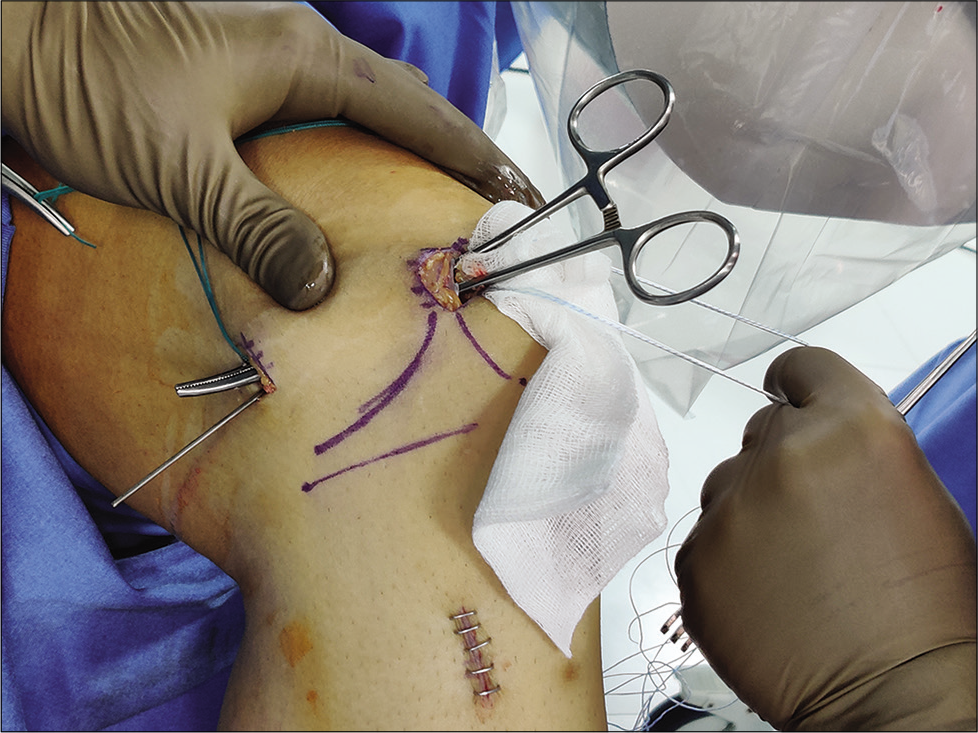
The patient was placed in a supine position and after adequate anesthesia (spinal or general, as per case), a tourniquet was applied around the thigh. Diagnostic arthroscopy was performed to remove any loose osteochondral body from patella or the lateral femoral condyle. Other intra-articular pathologies were addressed, and patellar tracking was assessed [Figure 2].
A gracilis graft was harvested through a 3 cm medial longitudinal incision over the pes anserinus. The graft was whipstitched with number 2 FiberWire (Arthrex Inc., USA).
A 2 cm longitudinal incision was made along the medial border of patella over the anatomical insertion of MPFL. After the skin and subcutaneous tissue, layer 1 (crural fascia), layer 2 (superficial MCL [patellar retinacular layer]), and layer 3 (joint capsule) were dissected to expose the patellar medial border. Extra-articular dissection was done. The superomedial border of the patella was freshened with a Rongeur – creating a longitudinal bony trough at the insertion site of MPFL.
2 × 5 mm double-loaded anchors (Stryker) were placed in the superomedial quadrant of patella to the north of the equator, aiming inferolaterally. Both the anchors were inserted in a parallel fashion. Care was taken not to violate the patellar articular cartilage [Figure 3].
The prepared graft was placed in the trough on the medial border and was tied down using one set of sutures from the anchor. The second set of sutures was used to transfix the graft to the patellar periosteum for extra strength [Figure 4].
The adductor tubercle (AT) and medial epicondyle (MEC) were palpated and a second 2 cm longitudinal incision was put between the two.
Dissection was then performed under the vastus medialis oblique (VMO) till the MEC for graft passage between the second (retinacular layer II) and the third (capsular) layer [Figure 5].
A 7 mm bony tunnel was then created over a guidewire at a point anterior to the midpoint between AT and MEC, at the isometric point, using Schöttle technique under fluoroscopy [Figure 6].The isometric point was identified in a dead lateral plane, proximal to the level of the posterior point of the Blumensaat line, 1 mm anterior to the posterior cortex extension line and 2.5 mm distal to the posterior origin of the medial femoral condyle.[9]
The graft was then passed under the VMO and pulled through the prepared tunnel into the femur.
The patella was held at the lateral border of trochlea and under adequate tension, the graft was fixed with a 7 mm × 25 mm RCI interference metal screw, with femur in 15° flexion, with the foot in neutral rotation.
Implant positions were confirmed through fluoroscopy [Figure 7].
The graft was visualized by arthroscopy – the extra-synovial position and satisfactory stable patellar tracking were confirmed [Figure 8].
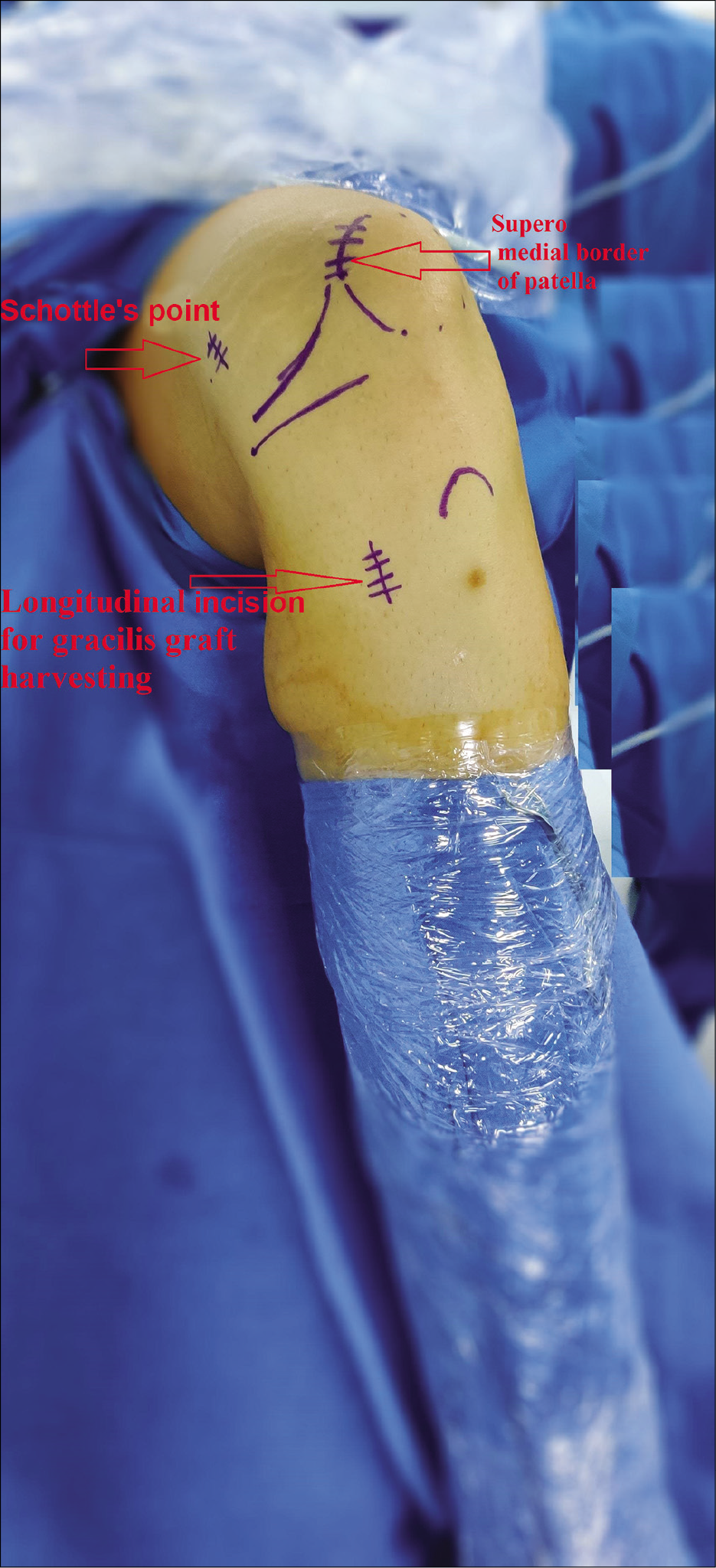
- A 27-year-old man who presented with recurrent patellar dislocation in his left knee. He was planned for medial patellofemoral ligament reconstruction. Landmarks were drawn after painting and draping. Schottels point, Superomedial border of patella and Longitudinal incision for gracilis graft harvesting are shown by arrows.
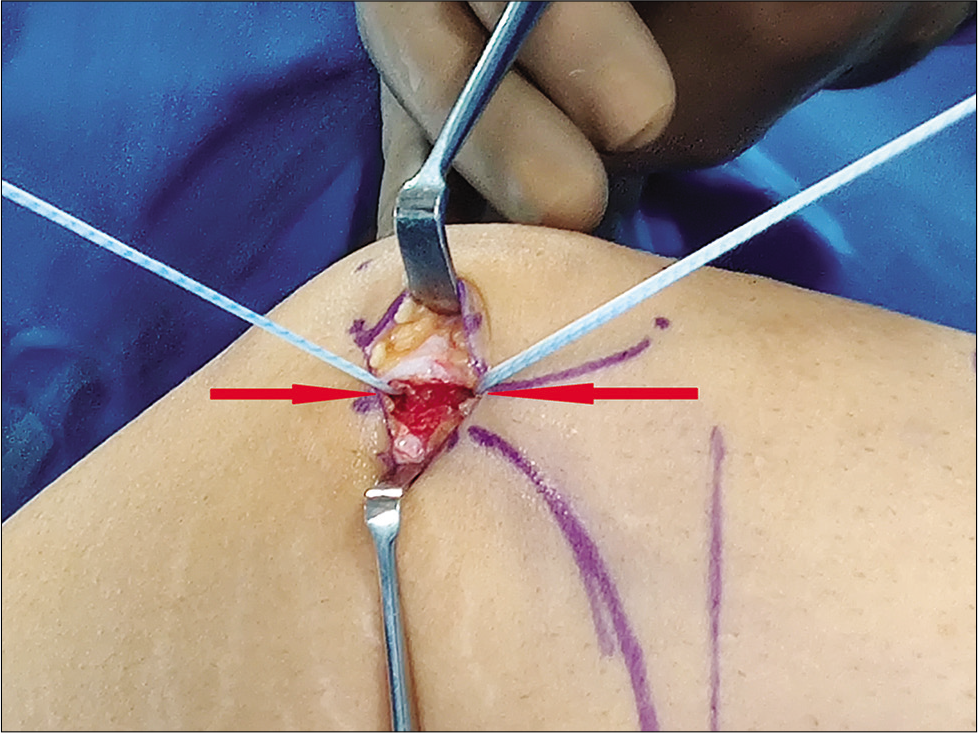
- Two suture anchors inserted parallelly, aiming inferolaterally in the superomedial compartment are shown with the arrow.
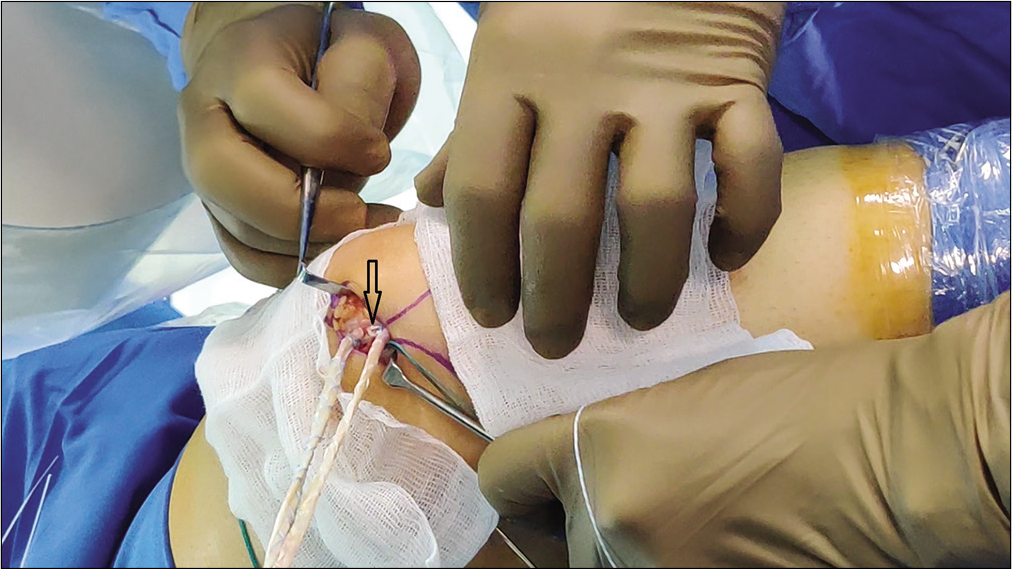
- Prepared graft was transfixed in the trough on the medial border of patella which is shown with the arrow.
- Graft passage preparation by dissecting under the vastus medialis oblique till the medial epicondyle. Artery forceps seen here are passed between the superficial medial collateral ligament and capsular layer.
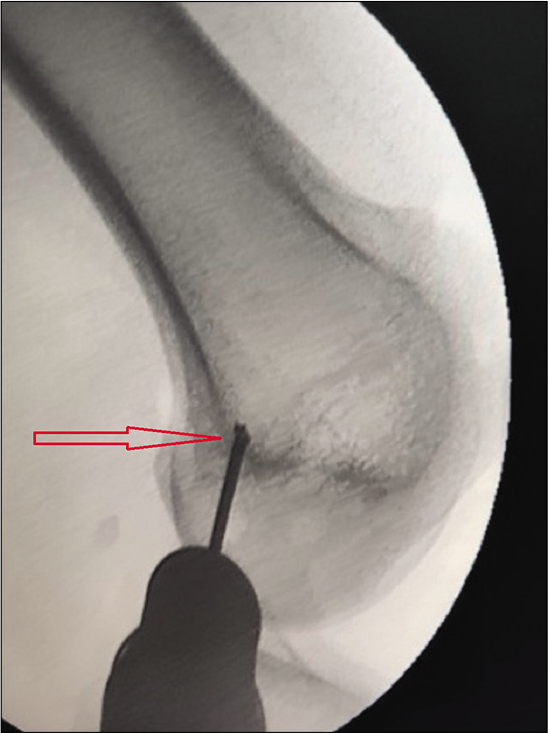
- The view of image intensifier showing the isometric point (marked by the arrow) between adductor tubercle and medial epicondyle at which the guide wire is drilled for creating the bony tunnel for passing the graft, using Schöttle technique.
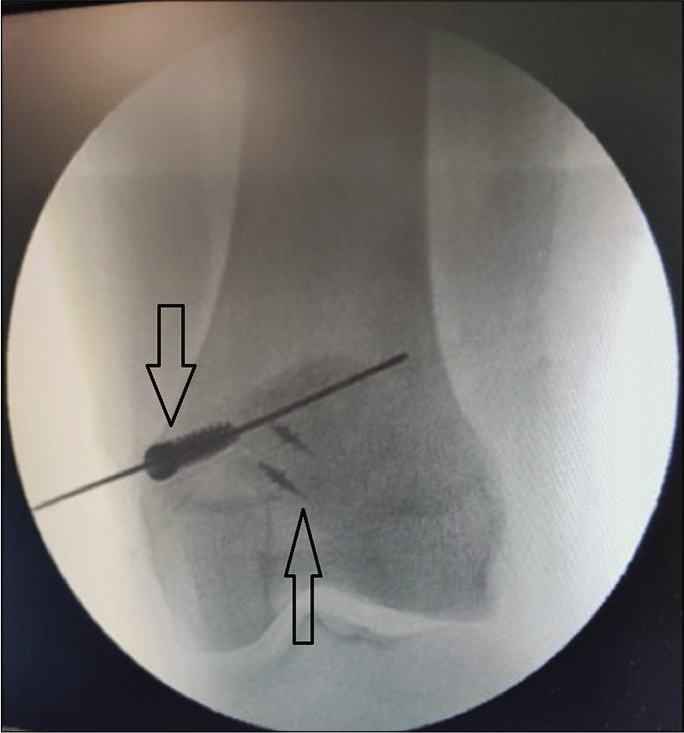
- Implant position confirmation image through fluoroscopy. Arrows mark the RCI interference screw in femur and the suture anchors in superomedial quadrant of patella.
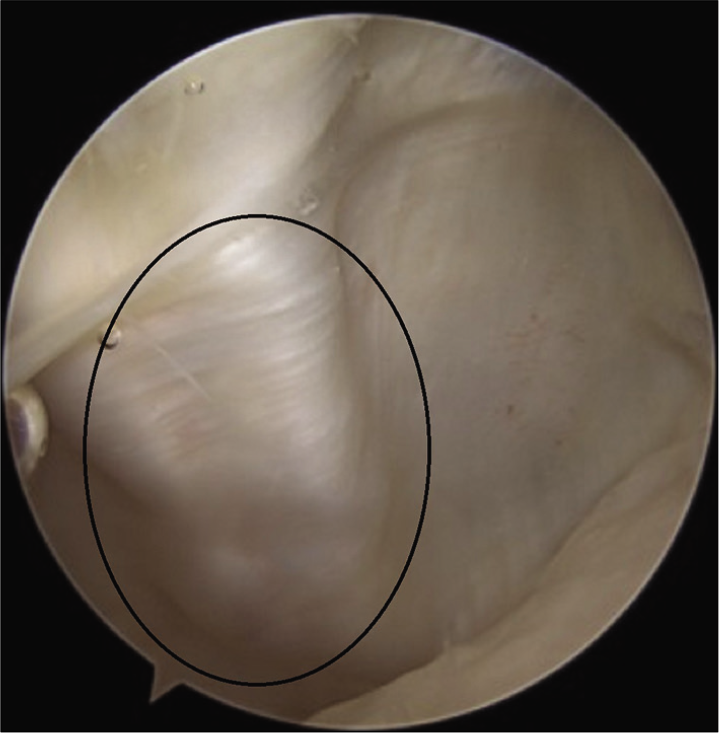
- Graft visualization by arthroscopy – the extra-synovial position as shown in circle.
Rehabilitation protocol
Postoperatively, the patient was allowed to mobilize with partial weight-bearing in the first 2 weeks with an extension knee splint.
After 2 weeks, full weight-bearing without the knee splint was allowed, depending on the quadriceps strength of the patient.
Range of movement exercises
0°–60° range was allowed in the first 2 weeks and was progressively increased as tolerated by the patient.
More than three-quarters of the patients were able to achieve a full range of motion by the end of 4 weeks.
All activities of daily living were allowed after 6 weeks.
Any kind of high impact activity was allowed after 3 months.
Competitive sports activities were allowed after 6 months.
Statistical analysis
Due to the non-normal distribution of the collected data, a non-parametric test was utilized to assess the statistical significance of our study.
Statistical calculations were performed using the IBM SPSS statistics software v. 26 for Windows. The statistical significance was set at P < 0.05, with a confidence interval of 95%.
Depending on the nature of the criteria (quantitative, such as observed values, mean, and standard deviation; qualitative, such as number and percentages of patients per class), a descriptive data analysis was carried out. Pre- and post-surgery Kujala scores were compared using the Wilcoxon sign test.
RESULTS
Our study had a total of 40 cases in 39 patients (one patient operated for bilateral knee). Twenty were female and 19 were male patients. The average age was 25 years (range 14–46 years). The mean follow-up period was 27.1 months (range 12–56 months) [Table 1].
| Parameter | Variable n (%) | Variable n (%) |
|---|---|---|
| Gender | Male – 19 (47.5) | Female – 21 (52.5) |
| Side | Right – 13 (32.5) | Left – 27 (67.5) |
| Age at surgery | Mean±SD | 24.7±7.9 |
| Minimum – 14 | Maximum – 46 |
Mean pre-operative Kujala score was 45.85 which improved to 92.72 postoperatively at the time follow-up.The above Box and Whisker graph shows the improvement in the Kujala score. It also shows the distribution of the score in the sample [Figure 9].
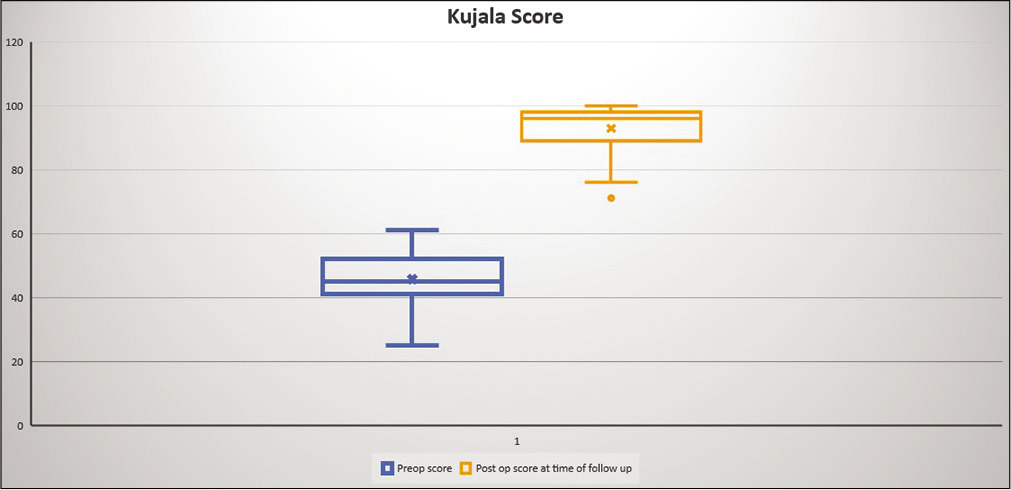
- Box and Whisker graph showing the improvement in the Kujala score.
The improvement in Kujala score was found to be highly significant (P < 0.01).
Subjective assessment of the procedure: 72.5% of the patients had an excellent outcome. About 15% of the patients had a good outcome whereas 10% had a fair outcome. Only one patient had a poor outcome.
Complications
The most common complication recorded was an occasional residual pain in the knee in 25% of the patients. Seven patients reported to have pain at the site of the femoral tunnel.
Patellar apprehension was recorded in seven patients. Two patients had patellar apprehension in performing sports activities, while five patients had apprehension in activities of daily living.
None of the cases had any post-operative stiffness, hematoma, or sepsis.
There was no failure (recurrent dislocation) seen.
DISCUSSION
The MPFL is the largest part of the medial ligamentous complex which, along with the lateral ligamentous complex, provides stability to the knee joint during its entire range of motion, and prevents patellofemoral dislocation.[10] The MPFL is a part of the medial patellar retinaculum and is found as a band of tissue that is seated in the layers between the deep fascia investing the sartorius muscle and the capsule of the knee joint. The ligament is formed by anterior and posterior fibers, superficially. The anterior fibers are a continuation of the vastus medialis while the posterior fibers anchor the patella to the MEC at the isometric point. The deep fibers of the ligament are vertically aligned and attach it to the midportion of the medial meniscus and the tibia.[10,11]
The MPFL is approximately 5–12 mm wide[12,13] and changes in length by only 1.1 mm during knee flexion from 0° to 90°.[14] It was found that the MPFL contributes up to 53% in the prevention of patellofemoral dislocations[15] and up to 60% with the knee in 20° flexion.[16] It has a mean tensile strength of 208 N.[17]
Nomura classified MPFL injuries on the basis of their location, duration of injury, and type of injury. Acute cases were divided into avulsion tear-type and substantial tear-type injuries, while chronic cases were divided in three groups – those with absent/discontinuous fibers, those with scar tissue, and those with loose femoral attachment.[18]
Recurrent patellofemoral dislocations are caused due to various reasons – abnormal patellar and/ or femoral morphology and altered lower limb rotational or valgus/varus alignment.[3] MPFL injuries that do not heal also contribute to recurrent dislocations. The rate of recurrent dislocations is as high as 63% after initial patellar dislocation.[19]
MPFL reconstruction becomes vital in managing a knee with recurrent patellar dislocations if the patient keeps dislocating their patella despite adequate conservative management.[4,5]
Sappey-Marinier et al. conducted a study in 2019[20] that evaluated 211 cases of isolated MPFL reconstruction. They had a minimum follow-up period of 3 years and were able to show an improvement in Kujala scores postoperatively (56.1 pre-operative to 88.8 post-operative).[20]
In 2004, Schöttle et al. assessed both the clinical and radiological outcomes of linear MPFL reconstruction in 12 patients (15 knees) using semitendinosus graft after a follow-up of 4 years.[21] Out of 15 knees (12 patients), 8 needed medialization of the tibial tuberosity. They also found their patients to have improved Kujala scores (53.3 points pre-operative to 85.7 post-operative).
In our study, we included 40 knees and followed them for a mean period of 27.1 months. Our Kujala scores improved from 45.85 (mean, pre-operative) to 92.72 (mean, postoperative), which is higher than the improvement shown in both the studies mentioned.
While we did not encounter any case with a recurrence of patellofemoral dislocation, 1 patient in the study by Schöttle et al. and 10 patients from the study by Sappey-Marinier et al. were classified as failures, that is, these patients reported recurrent patellar instability even after the surgery.
Sappey-Marinier et al. went on to identify the possible risk factors for failure, but in our case series, isolated MPFL reconstruction was only performed if the other structural parameters contributing to patellar instability were within normal limits. This can be a reason for the lack of any failures in our series.
Our subjective satisfaction assessment shows that 96% of our patients were satisfied with the surgery. One of the patients who did not have the desired result was found to have quadriceps weakening even after extensive physiotherapy, on regular follow-ups. This may have been the cause of her problems.
We modified the surgical steps used commonly for MPFL reconstruction. Although the anatomical fixation points, graft harvesting, and graft passage were similar to previously described standard techniques,[22,23] graft preparation and its fixation over the patella have been modified.
Various techniques for fixation of graft to patella have been described. Transverse or V-shaped transosseous tunnels through the patella for the passage of the graft have been shown to increase the risk of intraoperative or post-operative patellar fracture.[24] Even for the suture anchors, drilling transverse tunnels or converging tunnels may increase the risk of patellar fracture, as shown in various case reports.[25,26]
We recommend drilling two oblique parallel tunnels from the superomedial cortex toward the inferolateral direction in the midsubstance of the patella. Our technique has the following advantages. We reinforced the graft with non-absorbable, high tensile suture material (FiberWire – Arthrex Inc., USA). It forms a scaffolding around the graft which, in turn, protects the graft from any laceration-type injury by the anchor sutures and the titanium screw on the femoral side.
We used metal anchors which increases the pull out strength of the graft and offers a good purchase in the bone. Their biomechanical performance has been shown by Saper et al.[27] Third, the graft is placed in a trough on the medial aspect of the patella. This increases the surface area for the graft to be incorporated, allowing better healing in the cancellous bone.
In addition, one of the sutures from the anchors in patella is used for transfixing the graft to the retinaculum as well as the periosteum. This reinforces the patellar attachment of MPFL significantly.
We propose that these modifications result in a stronger fixation and early healing which, in turn, allows early mobilization and has a lower chance of failure. We have not seen any failures as yet.
Complications
Patients who had occasional anterior knee pain or femoral tunnel pain were managed conservatively using ice packs.
For the patients having patellar apprehension in sports or daily activities, we advised them to use an external patella supporting brace during activities.
The strength of our study is that it is a cohort of 40 patients with a mid-term mean follow-up of 2 years and a minimum follow-up of 1 year. It has been described that most redislocations after surgery occur within the first 2 years.[28] As such, our 2-year average follow-up represents a study population whose surgical outcome is likely to be stable.
This study had several limitations. First of all, the surgeries were performed by a single surgeon at a single center. Second, we were limited by the retrospective nature of the study; the radiological parameters were not systematically recorded and hence could not be presented. Third, among all the patients contacted for the last follow-up, most of them answered the Kujala score online or over the phone. Finally, another weakness was that our study lacked a control group but since there is no definite gold standard for the treatment of patellar instability, it was not possible to identify a control group for comparison.
In our opinion, studies with larger sample size and a longer follow-up are required to assess the outcome of isolated MPFL reconstruction in properly selected patients for patellar instability.
CONCLUSION
In properly selected patients with recurrent patellar instability, isolated MPFL reconstruction appears to be a safe and efficient surgical procedure for the stabilization of patella, with a low failure rate. Consistent good results with early rehabilitation can be obtained using suture anchors to fix the implant on patella and using the described technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7:121-7.
- [CrossRef] [Google Scholar]
- Patellofemoral instability: Evaluation and management. J Am Acad Orthop Surg. 1997;5:47-57.
- [CrossRef] [PubMed] [Google Scholar]
- An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98:417-27.
- [CrossRef] [PubMed] [Google Scholar]
- Operative treatment of primary patellar dislocation does not improve medium-term outcome: A 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76:699-704.
- [CrossRef] [PubMed] [Google Scholar]
- Acute traumatic primary patellar dislocation: Long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15:62-6.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: A systematic review. Am J Sports Med. 2010;38:181-8.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial torsion: A method of assessment and a survey of normal children. Clin Orthop Relat Res. 1972;86:183-6.
- [CrossRef] [Google Scholar]
- Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298-306.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801-4.
- [CrossRef] [PubMed] [Google Scholar]
- Medial patellofemoral ligament: Cadaveric investigation of anatomy with MRI, MR arthrography, and histologic correlation. AJR Am J Roentgenol. 2008;191:490-8.
- [CrossRef] [PubMed] [Google Scholar]
- Three layers of the medial capsular and supporting structures of the knee: MR imaging-anatomic correlation. Radiographics. 2000;20:S83-9.
- [CrossRef] [PubMed] [Google Scholar]
- Medial patellofemoral ligament reconstruction: A new technique. BMC Musculoskelet Disord. 2007;8:22.
- [CrossRef] [PubMed] [Google Scholar]
- The anterior aspect of the knee joint. J Bone Joint Surg Am. 1981;63:351-6.
- [CrossRef] [PubMed] [Google Scholar]
- The anatomy and isometry of the medial patellofemoral ligament: Implications for reconstruction. Am J Sports Med. 2004;32:1509-13.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682-93.
- [CrossRef] [PubMed] [Google Scholar]
- Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59-65.
- [CrossRef] [PubMed] [Google Scholar]
- Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87:36-40.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of lesions of the medial patellofemoral ligament in patellar dislocation. Int Orthop. 1999;23:260-3.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med. 1997;25:213-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes and predictive factors for failure with isolated MPFL reconstruction for recurrent patellar instability: A series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med. 2019;47:1323-30.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13:516-21.
- [CrossRef] [PubMed] [Google Scholar]
- Hamstring graft fixation in MPFL reconstruction at the patella using a transosseous suture technique. Knee Surg Sports Traumatol Arthrosc. 2010;18:1542-4.
- [CrossRef] [PubMed] [Google Scholar]
- Medial patellofemoral ligament reconstruction using a bone groove and a suture anchor at patellar: A safe and firm fixation technique and 3-year follow-up study. J Orthop Surg. 2016;11:138.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of transosseous tunnels on patella fracture risk after medial patellofemoral ligament reconstruction: A cadaveric study. Arthroscopy. 2018;34:513-8.
- [CrossRef] [PubMed] [Google Scholar]
- Patella fracture after medial patellofemoral ligament reconstruction using suture anchors. Knee. 2013;20:605-8.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar fracture after MPFL reconstruction, a case report. MOJ Orthop Rheumatol. 2016;6:228.
- [CrossRef] [Google Scholar]
- Biomechanical evaluation of classic solid and all-soft suture anchors for medial patellofemoral ligament reconstruction. Am J Sports Med. 2017;45:1622-6.
- [CrossRef] [PubMed] [Google Scholar]
- Acute patellar dislocation in children and adolescents: A randomized clinical trial. J Bone Joint Surg Am. 2008;90:463-70.
- [CrossRef] [PubMed] [Google Scholar]






