Translate this page into:
Retraction of infrapatellar fat pad during arthroscopy of the knee

*Corresponding author: Srinivas B. S. Kambhampati, Department of Orthopaedic Surgery, Sri Dhaatri Orthopaedic Maternity and Gynaecology Center, Vijayawada, Andhra Pradesh, India. kbssrinivas@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kambhampati SB, Chittoor SP. Retraction of infrapatellar fat pad during arthroscopy of the knee. J Arthorsc Surg Sport Med 2021;2(1):81-3.
Abstract
One of the most important requirements for a good arthroscopic procedure is a clear view of the operating field. Infrapatellar fat pad is known to obstruct the field of view inside the knee for an arthroscopic surgeon. A clear view also shortens the operating time and saves valuable time under tourniquet. Different methods have been used to either avoid the fat pad, shave the fat pad, or retract to give a clear view inside the knee joint. We describe a technique using sutures which is simple, safe, inexpensive, reproducible, and effective in providing retraction of the fat pad.
Keywords
Fat pad retraction
Arthroscopy knee
Infrapatellar fat pad
INTRODUCTION
Infrapatellar fat pad is a dynamic, deformable, and mobile structure during movements of the knee.[1] Its role in the function of the knee is poorly understood and is known to have a stabilizing effect on patella in extremes of knee flexion.[2] It has been established that its resection alters the patellar biomechanics and the knee kinematics.[3]
Fat from the infrapatellar fat pad has been accepted as a major block to proper viewing during arthroscopy of the knee. In addition to providing a clear view, moving fat pad out of the field would shorten the operating time, reduce interruptions, and increase confidence of the operating surgeon.
Techniques have been recommended to improve visualization either by avoiding the fat pad by placing a high lateral portal[4] or using a rubber retractor in the form of a rubber tube or a glove finger.[5] These have their own advantages and disadvantages as discussed in the discussion section. We report a technique using sutures (No 2 Ethibond) to improve visualization of the knee by retracting the fat pad anteriorly.
TECHNIQUE
Standard anterolateral (AL) and anteromedial (AM) portals are placed for knee arthroscopy and the arthroscope introduced through the standard viewing portal. If excessive fat is visualized, a single no. 2 Ethibond suture is taken (frequently used during anterior cruciate ligament [ACL] graft preparations), looped and the needle at the end removed. The suture is loaded into a knot pusher and the knot pusher is passed from the AM portal into the AL portal along with the loop of suture created by passing the suture through [Figure 1]. The free ends of the suture remain outside the AM portal. Once the loop exits outside the AL portal, it can be cut to create two independent sutures and the knot pusher removed. We will now have two sutures [Figure 2] that can be used flexibly to retract the fat pad and the anterior structures away from the intercondylar notch.
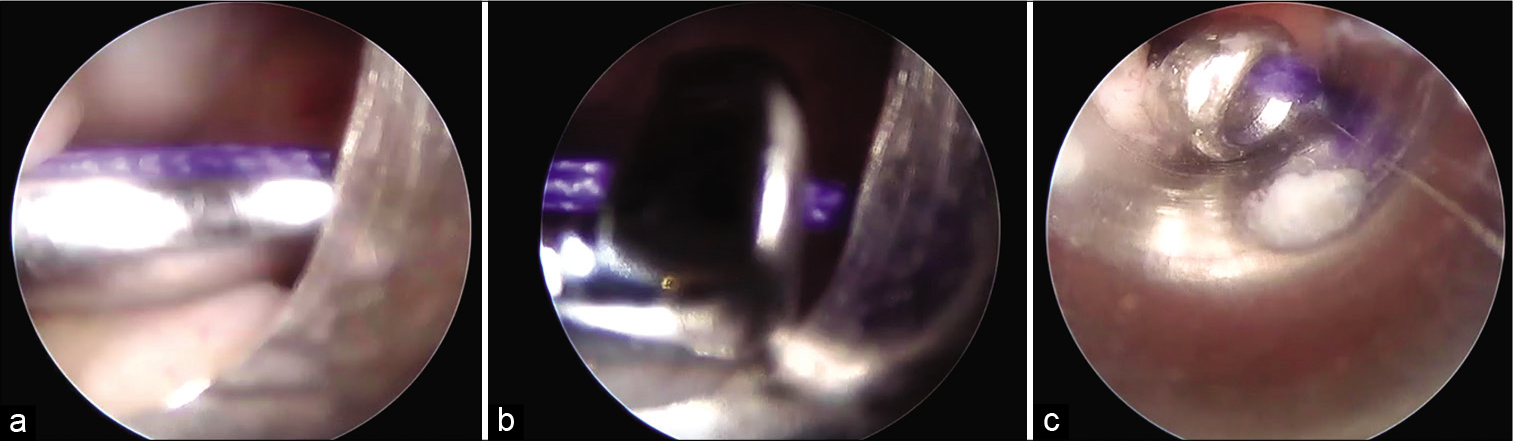
- Passing suture using knot pusher. (a) Knot pusher with suture in the joint, (b) knot pusher captured in the cannula, (c) knot pusher with suture pushed into cannula retracting the scope.

- Two separate loops created with single pass using knot pusher. Vicryl is shown here but our preference is Ethibond size 2 or 5.
One suture may be used to retract proximally and anteriorly and the other used to retract distally and anteriorly to pull the fat pad away from the notch and make the view better, taking care not to involve the anterior horns of the menisci or the anterior intermeniscal ligament. It may fail to clear completely in all cases but gives valuable space and holds the fat pad off from interfering with the procedure. If the patellar tendon moves anteriorly, the fat pad by virtue of its attachment to the patellar tendon also moves anteriorly.
This maneuver is especially useful on higher flexion angles of the knee when the patellar tendon gets taut and pushes the fat pad into the notch and also while working on anterior horns, anterior roots [Figure 3], or the anterior parts of the body of the medial and lateral menisci. Figure shows how the fat pad is pulled forward away from the anterior part of the tibial plateau giving much needed space to work on the anterior part of the meniscus. The portals can be used for routine work without obstruction from the sutures. Care must be taken to avoid shaving the suture while working close. In the case depicted (a 1-year-old ACL injury with rupture of anterior root of medial meniscus), the anterior root of medial meniscus ruptured and retracted away from the plateau due to chronicity of the injury and hence had to be dissected to reposition on the plateau. This required retraction of the fat pad and anterior soft tissues to visualize the anterior part of the meniscus which slid off the anterior plateau. With increased pull, the patellar tendon is seen moving anteriorly and hence along with it, the fat pad is pulled away.
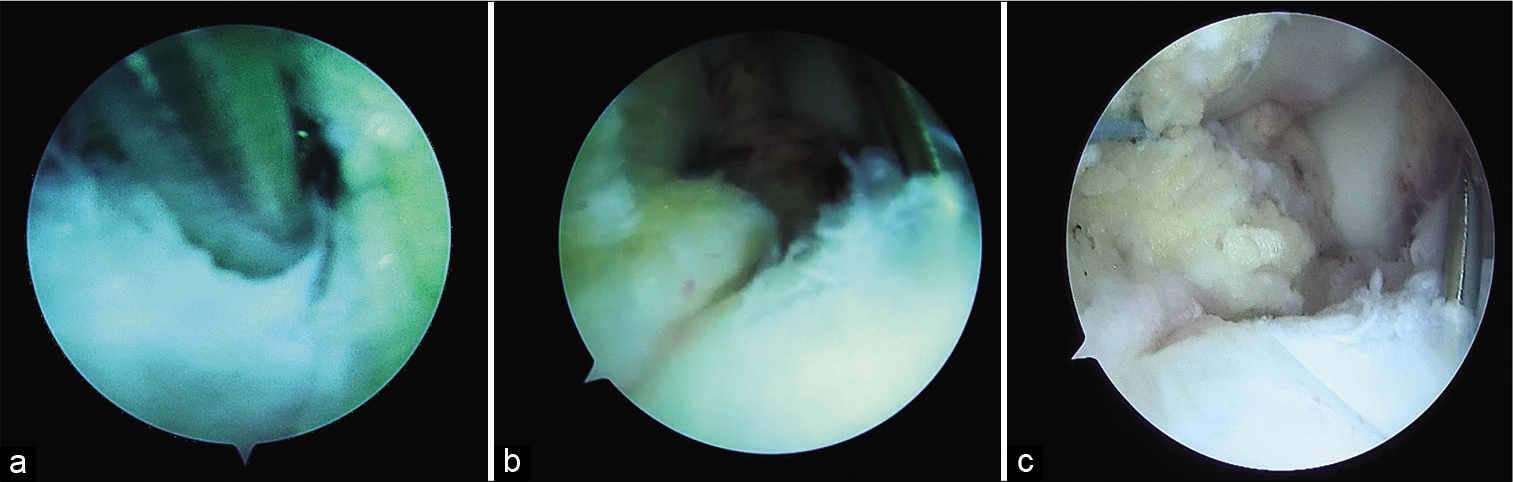
- Intra-articular view. (a and b) Need for scope to place close to wire to avoid fat pad from blocking view (a: Proximity of fat pad from 2 O’clock to 5 O’clock position), (c) Ethibond suture is seen retracting the partially excised fat pad at 10 O’clock position and giving a clearer view and space.
DISCUSSION
While the high portal can avoid the fat pad, it may still catch some part of the fat pad, especially on higher flexion angles of the knee, and could also limit viewing of posterior parts of the medial and lateral compartments for meniscal work which require lower placement of the scope. The rubber tubing technique proposed cannot be used in patients with latex allergy.
We accept that our technique is not a fool proof method and may not clear the fat pad entirely in all situations. The suture could cut through the fat pad occasionally and the pad could again get in way but, if the patellar tendon is retracted, the fat pad, which is attached to the tendon, will be pulled away too indirectly by the sutures to create valuable space to work inside the knee at the same time preserving the fat pad. Partial excision of fat pad may be needed sometimes but would entail removal of less than what is otherwise required. Fat pad interference also requires the scope to be placed close to the object of inspection reducing the field of vision around the object [Figure 3a and b]. When retracted, the scope could be pulled back enabling a zoomed-out view of the object and structures around it [Figure 3c].
The suture may be difficult to pass if the portals are placed close to the patellar tendon as the distance between the portals is very short. For standard positions of the AL and AM portals, this difficulty may not be seen. To minimize damage to the fat pad by the knot pusher itself, it may be visualized inside the knee when placed through the AM portal. It is then guided to the scope and the arthroscope is then disconnected from the cannula and the knot pusher pushed through the cannula which is withdrawn out of the portal to guide the pusher out of the knee. The inferosuperior spread of the sutures intra-articularly would depend on the orientation of the portals. Horizontal portals would have a narrow spread compared to vertically placed AL and AM portals. Any suture material may be used but our preference is size 2 or 5 Ethibond. The retraction is better in extended positions of the knee as the patellar tendon is relatively lax but the requirement is more in higher flexion angles when the fat pad is pushed posteriorly by a stretched patellar tendon closer to the notch at these angles of knee flexion.
Another advantage of placing sutures in the portal for retraction is that passing instruments and the scope become easier as the portal is maintained open by the suture. This is an easy technique, safe, does not require special equipment or skills other than the knot pusher, is fast to apply, and gains valuable tourniquet time apart from reducing interruptions from the blockage by the fat pad.
Further studies are required to identify the role of this technique and extent of clearance achieved in various knee arthroscopic procedures.
CONCLUSION
Suture retraction is a useful technique to retract infrapatellar fat pad, particularly while working on anterior root and horn injuries of the meniscus and provides valuable space on deep flexion of the knee.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Srinivas Kambhampati is on the Editorial Board of the Journal.
References
- The infrapatellar fat pad is a dynamic and mobile structure, which deforms during knee motion, and has proximal extensions which wrap around the patella. Knee Surg Sports Traumatol Arthrosc. 2018;26:3515-24.
- [CrossRef] [PubMed] [Google Scholar]
- Infrapatellar fat pad pressure and volume changes of the anterior compartment during knee motion: Possible clinical consequences to the anterior knee pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2005;13:135-41.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical and kinematic influences of a total infrapatellar fat pad resection on the knee. Am J Sports Med. 2004;32:1873-80.
- [CrossRef] [PubMed] [Google Scholar]
- High lateral portal for sparing the infrapatellar fat-pad during ACL reconstruction. Orthop Traumatol Surg Res. 2011;97:870-3.
- [CrossRef] [PubMed] [Google Scholar]
- The rubber fat pad retractor: Use in arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:332-3.
- [CrossRef] [Google Scholar]







