Translate this page into:
Significance of critical shoulder angle as predictor in rotator cuff tear
*Corresponding author: Monika Verma, Department of Orthopaedics, Mahatma Gandhi Mission Medical College and Hospital, Aurangabad, Maharashtra, India. doctormonikaverma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gadekar G, Verma M, Dhytadak D. Significance of critical shoulder angle as predictor in rotator cuff tear. J Arthrosc Surg Sports Med. 2023;4:43-7. doi: 10.25259/JASSM_18_2023
Abstract
Objectives:
A critical shoulder angle (CSA) is the angle between the line drawn from the Glenoid’s superior and inferior margins and a line drawn from the inferior glenoid margin to the lateral border of acromion. The study aims to establish the significance of CSA as a predictor in RCT.
Materials and Methods:
Data points were collected retrospectively from 196 patients with shoulder pain who visited out-patient department or were in an inpatient orthopedics ward. The diagnosis of those patients of either a RCT or a normal shoulder was confirmed using ultrasonography or magnetic resonance imaging. Then, two investigators, unaware of the status of RCT or non-RCT (NRCT), calculated the CSA. Later, these data points were compared using an unpaired t-test, which helped to determine the accuracy of CSA in diagnosing RCT and the optimal cutoff.
Results:
We included 196 patients in our studies, out of which 101 patients had RCT s, that is, in the RCT group and 95 in the NRCT group. The CSA was higher in the RCT group (P < 0.01) than in the NRCT group.
Conclusion:
At the end of the study, we concluded that there is a significant correlation between CSA and RCT that CSA is significantly greater in patients with RCT.
Keywords
Critical shoulder angle
Rotator cuff tear
Shoulder pain
INTRODUCTION
During the evolution of human beings, the upper limb needed more mobility to accommodate a wide variety of tasks, which became possible due to the larger humeral head compared to the Glenoid, which creates a mismatch in size, that is, there is a trade-off of stability for mobility. Hence, the stability of this joint depends on two types of stabilizers: Static and Dynamic. Static stabilizers are capsule, labarum, and dynamic stabilizers are rotator cuffs.
The rotator cuff is formed by the tendinous confluence of four muscles, supraspinatus muscle, infraspinatus, teres minor, and subscapularis. They help in shoulder movements, abduction, external rotation, and internal rotation. They also prevent superior translocation of the humerus.
Most rotator cuff tears (RCTs) occur in a previously diseased cuff, like degeneration of the rotator cuff.[1] These degenerated rotator cuff progresses to partial or full-thickness tears. Most commonly, the supraspinatus tendon is involved. Among the patients who undergo rotator cuff repair, only 8% of them are due to trauma.[2]
When we speak about partial thickness tears of a rotator cuff, we refer to tendon involvement <50% of the thickness, which does not lead to muscle retraction.[1] These partial tears of RCT can be intra-substance, bursal-sided, or articular-sided (under the surface). The latter constitute ~90% of partial tears.[3] These generally do not present with weakness but cause pain, which is generally more significant than a complete tear.
On the other hand, total thickness tear involves complete disruption of the rotator cuff fiber, which causes communication of both articular and bursal spaces.
The extent of the lesion is assessed in radiographs AP and mediolateral direction. It is classified as a small lesion (1–3 cm), medium (3–5 cm), and large (>5 cm). The involvement of 2 or more tendons is termed massive, and the reconstruction procedure is more complex than the small or medium lesions.[4] If the tears are significantly larger, they might get retracted and undergo fatty degeneration, which becomes an irreversible change over time.[5] RCTs are prevalent, and it has shown a gradually increasing trend, primarily due to the advent of investigations like magnetic resonance imaging (MRI). However, despite this intervention, most patients with RCT remain undetected as many are asymptomatic.
RCT can present a spectrum of symptoms, from shoulder pain and restricted movements to hardly any symptoms. RCTs are very prevalent, and this prevalence differs in different age groups; approximately 15–20% in 60-year-old patients, 30% in 70-year-old patients, and 36–50% in people aged 80 years old. The prevalence of RCT increases with an increase in age. Moreover, the prevalence of RCT in the general population is about 22.1%.[6,7] Regarding its contribution to shoulder pain, RCT accounts for approximately 30–70% of shoulder pain.[6] The etiology of RCT is of two types intrinsic and extrinsic. Intrinsic being microtrauma, degeneration, and hyper-perfusion, and the latter include overuse of the cuff and chronic impingement syndrome.[8]
Recent studies have shown anatomical factors like critical shoulder angle (CSA) are related to RCT.[9] Before establishing this relationship, let us become familiar with CSA. This angle is between the line of the superior to the inferior bony margin of the glenoid and the inferior bony margin of the glenoid to the lateral margin of the acromion. The CSA can indicate glenoid inclination and lateral extension of the acromion.[10] Studies like[11-13] have also reported the significance of CSA in patients with RCT. Among the studies mentioned earlier, study[12] also reported similar results for degenerative RCT, which is CSA being higher in them than in the normal population.
Although several studies have associated radiographic assessment measures like CSA with RCT, there has yet to be a study that can determine the accuracy of these parameters in predicting RCT.[11-13]
Studies like[11-13] have also reported the significance of CSA in patients with RCT. Among the earlier studies, study[12] also reported similar results for degenerative RCT, with CSA higher than the average population.
Some studies have mentioned the diagnostic value of the CSA in RCTs, but its prognostic value still needs to be determined. In the study by Docter et al.,[14] which is a review of 12 studies, Docter et al. found a variation of this angle among age groups. Although the incidence of re-tear is higher in the group, who were found to have CSA >38° but clinically, they had the same outcome.[14]
In a retrospective study conducted by Gumina et al., no significant variation in CSA was observed among genders or sides. However, the study did find a linear correlation between CSA and age.[15]
According to a meta-analysis by Docter et al., there is an association between the higher value of CSA and chronic, full-thickness RCT. The study also demonstrated a greater risk of re-tear in cases with higher CSA values, but interestingly, no significant association was found between CSA and the functional outcome of RCR.[14]
MATERIALS AND METHODS
We conducted a retrospective record-based study at a medical hospital from 2022 to 2023. We included participants in this study from the inpatient and outpatient departments of orthopedics. This study is approved by the Ethics Committee for Research on Human Subjects, MGM, Maharashtra.
Inclusion criteria
The following criteria were included in the study:
Patients between the ages of 40–60
Patients complaining of shoulder pain and restricted shoulder joint movement
Patients consented to undergo investigations such as shoulder X-ray, ultrasonography (USG), and MRI
Patients with X-ray shoulder AP were taken with standard protocol.
Exclusion criteria
The following criteria were excluded from the study:
Patients previously operated on the same shoulder
Patients with glenohumeral osteoarthritis or acromioclavicular arthritis, which could influence CSA
Patient not giving consent
Patients with shoulder X-rays which are not with standard protocol.
The MRI or USG reports of one hundred and ninety six patients were studied, and confirmation of RCT or normal shoulder was made. One hundred and fifty patients underwent MRI, and forty six patients underwent USG. Out of these, ninety patients were reported normal through MRI, and five patients were reported normal through USG.
Then, radiographs of those patients were collected, and three independent investigators who were orthopedic surgeons-assessed radiographs and calculated CSA by drawing the line from the superior to the inferior bony margin of the glenoid and the inferior bony margin of the Glenoid to the lateral margin of the acromion and the angle between them is recorded as CSA. This is demonstrated in Figure 1. After calculating CSA, the patients were distributed into RCT and non-RCT (NRCT). After this CSA of both groups is compared using an unpaired t-test. We have summarized the method of our study in flow chart 1.
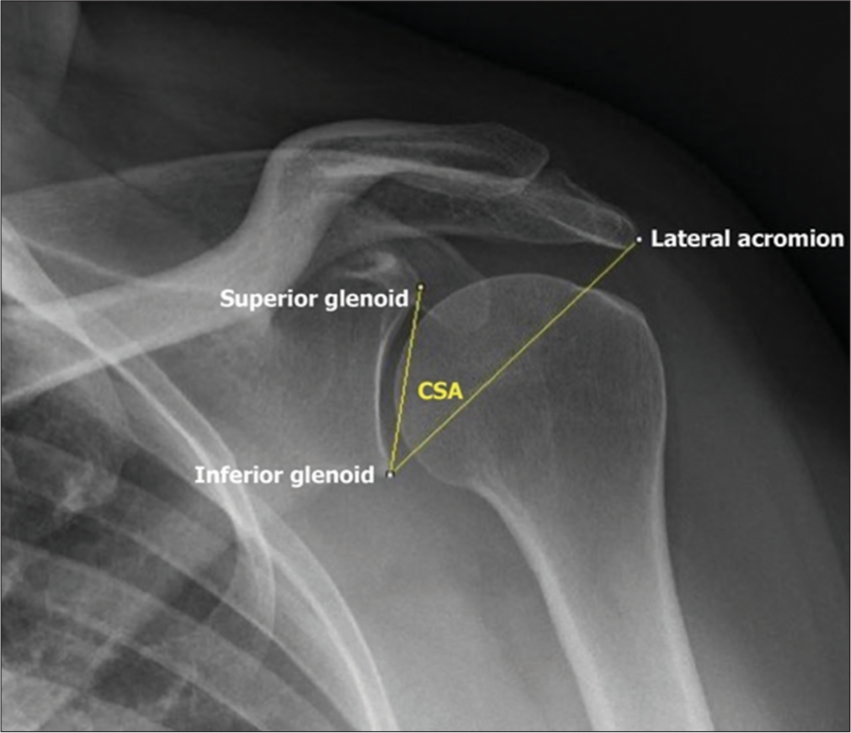
- Demonstrating, the calculation of critical shoulder angle (CSA).
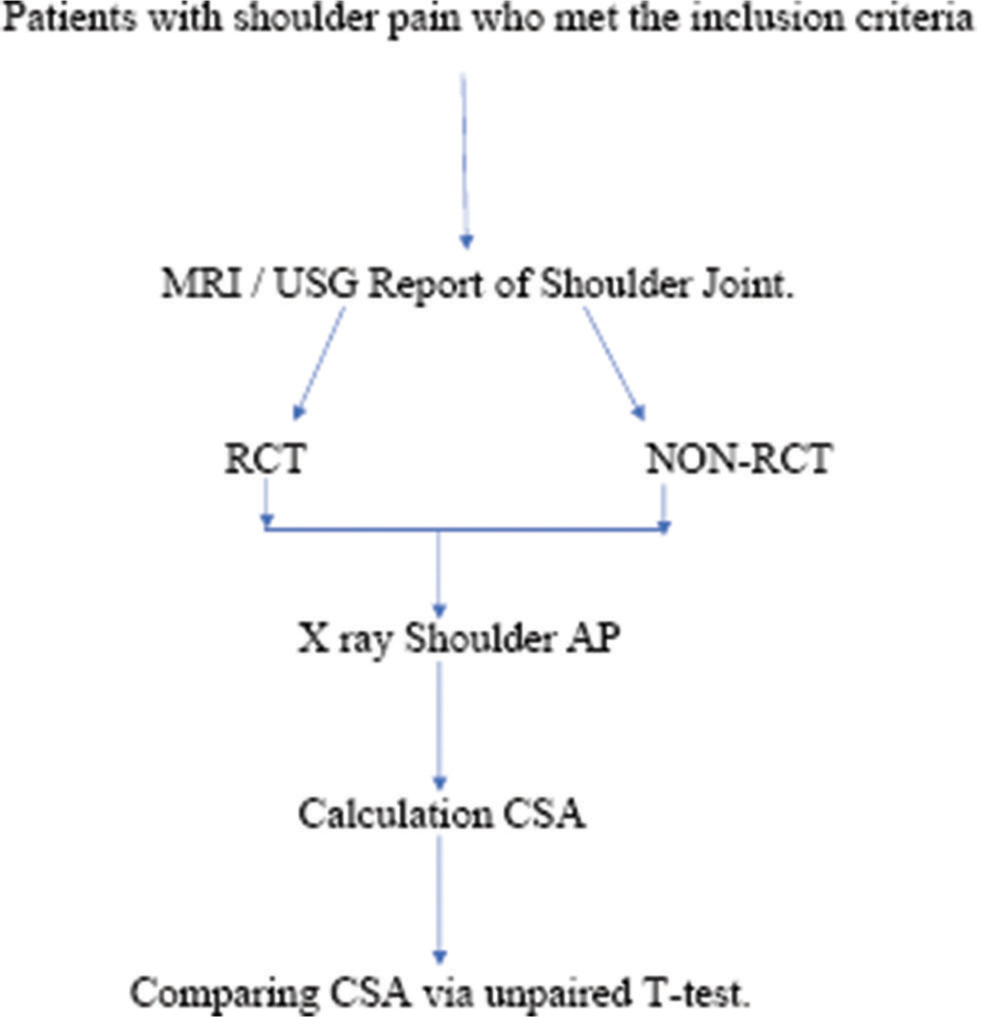
- Study flow chart. RCT: Rotator cuff tear, AP: Antero-posterior view, CSA: Critical shoulder angle.
Radiographic evaluation of CSA
After MRI or USG confirmation of the RCT X-ray of the patients was examined. This X-ray is taken initially before MRI or USG is advised. This X-ray is taken in a standing position with a beam descending and tilted to 20 depressed to ensure an accurate assessment of radiological features. AP shoulder was taken as per protocol. Moreover, CSA was measured as described by Blonna et al.[16]
According to the Suter-Henninger criteria,[17] an A1 view shows the glenoid in profile with the coracoid overlapping the superior rim of the glenoid. Hence, the transverse glenoid measures 0 mm; the RTL equals 0 in this case. The CSA, for example, is 30.7° (normal range of 30°–35°).
The same scapula as in the previous case, with no flexion or extension, but the shoulder is rotated to 10° of anteversion, which will yield a D1 view, on which the glenoid cup is now visible. The RTL equals 0.18, which is below the 0.25 cutoff proposed by Hou et al.[18] The CSA deviates by 1.5°, which is below the 2° allowable error but still in the normal range. (C) The scapula is now rotated into 20° of anteversion, and the RTL equals 0.32, which exceeds the cutoff value of 0.25. The measured CSA is 37.8°, which aberrantly errs into the range indicative of a RCT, which leads to a change in the clinical interpretation of this scapula.
According to Hou et al.,[16] RTL is ratio of the transverse to longitudinal projected length of the glenoid (diameter of the lateral glenoid outline), and the RTL is quite specific and sensitive for identifying an image that is adequate for accurate measurement of CSA. Scapula from patients with RCT shows a higher correlation between the RTL and error in CSA prediction than the general population, but as the RTL increases, an error in CSA prediction longitudinal projected length of the glenoid.[18]
For the sake of accuracy, we have used only A1 views in our study. That is, the X-rays had minimal overlapping of the anterior and posterior edges of the glenoid cavity.
Furthermore, CSA was calculated between the line from joining the superior and inferior glenoid to the line from the most lateral border of the acromion. To ensure the accuracy of measurement of CSA, independent observers measured in two different incidences,[19] each image was measured 3 times, and the mean value was calculated and used in this study. An experienced and capable physician performed radiological investigations such as USG and MRI as routine practice and was unaware of the study and radiographic CSA measurement due to the nature of the study, which is retrospective. The previous studies[20] have estimated that diagnostic accuracy of USG for full-thickness RCT was more than 0.90 for sensitivity and specificity. For partial thickness RCTs, specificity was more than 0.9.
Statistical analysis
After calculating CSA for each group, we subdivided all participants into the RCT and NRCT groups based on ultrasound or MRI findings. Then, baseline 1:1 matching for demographic data was done from records. After this step, the CSA of both groups was done using an unpaired t-test.
RESULTS
P-value for this study is <0.01 that sensitivity and specificity were calculated to be 73.2% and 70.5%, respectively, in predicting SS tendinopathy.
DISCUSSION
In a study by Gerber et al.,[19] a comparison was made of the joint reaction force of CSA of more than 38 for more than 33 patients with RCT.
They also reported that an increased CSA could result in a decrease in the stability of the joint, and this instability leads to increased work for the supraspinatus tendon, which can lead to tearing after repetitive use.
Docter et al.: carried out meta-analysis to demonstrate the association of higher value of CSA and RCT. In his study, he found that CSA was not efficient in predicting the outcome of rotator cuff repair.[14]
There was another meta-analysis by Tashjian that is worth mentioning; in this study, he included 70 papers; and noticed that as the age increased, the CSA also increased. Smoking and genetics also increase the risk of RCT.[21]
Viehöfer et al., in their retrospective study, observed that the shoulder X-ray of normal patients had a comparatively smaller value of CSA than patients with RCT. They hypothesized an increase in the ratio of glenohumeral joint shear to joint compression forces as the value of CSA increases. This will cause increase stress on supraspinatus loads to stabilize the shoulder joint in abduction.[7]
Blonna et al., in their cohort study, concluded that raised CSA value is associated with an increased risk of RCT, larger cuff tear, and osteoarthritis of the shoulder joint.[16]
While other authors like Gumina et al., in their retrospective study, observed that the CSA does not vary significantly with gender or side. Though it does have a linear correlation between CSA and age.[15] While Kim et al. found no relationship between CSA and RCT and mentioned that higher CSA in RCT can signify a preexisting osteophyte.[11]
Kirsch et al. conducted a cohort study and observed that CSA stand-alone could predict the patient outcome after arthroscopic repair.[22]
Bjarnison et al. this study was a retrospective case – control study. It comprised 184 patients, 97 with RCT and 87 with OA. No causal relationship between CSA and RCT was found; however, there was a 2.25 OR of developing OA, given that the patient had a CSA <30°.[23]
In our study, we have included patients who visited us with shoulder pain and routinely advised shoulder AP and axial for these patients. However, many institutes do not have these facilities; hence, it is crucial that we have some radiological parameters available to screen for the RCT.
A high CSA can be a guiding light in this situation. A high CSA indicated high acromial coverage and glenoid inclination, contributing to vulnerability to RCTs from impingement.
We conducted this study on the Indian population and found that CSA can be considered an objective assessment tool for predicting whether the patient has RCT. However, we had limitations because we enrolled only those patients who consented to a USG or MRI. Hence, patients without any symptoms of RCT were omitted. Hence, more extensive research is required.
The cause of RCT is multi-factorial; it includes extrinsic and intrinsic factors; studies have shown an association of CSA with impingement, which is an extrinsic factor of RCTs.
The mean age of the patient in the RCT group is 54.34, and in the NRCT group is 51.87. For elaborate age distribution refer to Table 1. The age range for the RCT group is 40– 60 years and the mean age of the NRCT group is 40–60 years. Considering the gender distribution of both the groups, we found that the RCT group had a sex ratio of 0.6833 which is 683.33 females per 1000 males, whereas the sex ratio for the NRCT group is 0.9, which is 900 females per 1000 males [Table 2].
| Age | Group A (case) | Group B (normal) |
|---|---|---|
| 40–45 years | 23 | 10 |
| 45–50 years | 20 | 21 |
| 50–55 years | 22 | 25 |
| 55–60 years | 36 | 39 |
| Total | 101 | 95 |
| Gender | Group A | Group B |
|---|---|---|
| Male | 60 | 50 |
| Female | 41 | 45 |
| 101 | 95 |
The CSA was significantly higher in the RCT group than in the NRCT group. The mean CSA for the RCT group is 42.19, and for the NRCT group was calculated to be 33.89. The typical CSA range is 30–35, and the RCT group has a mean value above 35 [Tables 3 and 4]. That signifies that it can function as a predictor of RCT.
| CSA | Group A | Group B |
|---|---|---|
| Mean CSA | 42.19 | 33.89 |
CSA: Critical shoulder angle
| Group | RCT group | NRCT group |
|---|---|---|
| Mean CSA | 42.19 | 33.89 |
| SD | 5.09 | 3.33 |
| SEM | 0.51 | 0.34 |
CSA: Critical shoulder angle, SD: Standard deviation, SEM: Standard error of mean, RCT: Rotator cuff tear, NRCT: Non-rotator cuff tear
The confidence interval was calculated to be 8.3 ± 1.22 (Mean CSA of the RCT group – Mean CSA of the NRCT group)-95% of this confidence interval of this difference from 7.08 to 9.52.
CONCLUSION
Mean CSA for the RCT group is 42.19, and for the NRCT group was calculated to be 33.88; with this, we can conclude that the mean CSA was above the normal range of 30–35° in patients with RCTs.
In cases of RCT, the observed angle was found to be significantly increased as indicated by P < 0.01 in this study
It is predictive of RCT even in the absence of osteoarthritis of the shoulder joint, as in this study, we have excluded patients with glenohumeral osteoarthritis or acromioclavicular arthritis, which could influence CSA
We observed that the number of patients with RCT increased with age, showing a positive correlation with this demographic value.
Limitations of the study
We do acknowledge that our study has its own set of limitations. Particularly, the sample size, which is relatively small and was collected from a single tertiary care center, including only the Indian population, prevented the generalization of the study. Another drawback of this study is that it only includes patients with shoulder pain and does not include those without symptoms of RCT.
Hence, further study with a larger sample size, including different ethnicity, is required as well.
Ethical approval
This study is approved by Ethics Committee for Research on Human Subjects, MGM, Maharashtra. Approval number 2023/03. Approval date 1/01/2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have not used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Financial support and sponsorship
Nil.
References
- The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br. 2003;85:3-11.
- [CrossRef] [PubMed] [Google Scholar]
- Rotator cuff disease of the shoulder. J Bone Joint Surg Am. 1985;67:974-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of partial rotator cuff tears in young athletes: A preliminary report. Am J Sports Med. 1997;25:299-305.
- [CrossRef] [PubMed] [Google Scholar]
- The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505-15.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550-4.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop. 2013;10:8-12.
- [CrossRef] [PubMed] [Google Scholar]
- A larger critical shoulder angle requires more rotator cuff activity to preserve joint stability. J Orthop Res. 2016;34:961-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and biological aspects of rotator cuff tears. Muscles Ligaments Tendons J. 2013;3:70-9.
- [CrossRef] [PubMed] [Google Scholar]
- Large critical shoulder angle has higher risk of tendon retear after arthroscopic rotator cuff repair. Am J Sports Med. 2018;46:1892-900.
- [CrossRef] [PubMed] [Google Scholar]
- Critical shoulder angle and acromial index do not influence 24-month functional outcome after arthroscopic rotator cuff repair. Am J Sports Med. 2017;45:2989-94.
- [CrossRef] [PubMed] [Google Scholar]
- Can a high acromion index predict rotator cuff tears? Int Orthop. 2012;36:1019-24.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of individual scapular anatomy and degenerative rotator cuff tears. J Shoulder Elbow Surg. 2014;23:536-41.
- [CrossRef] [PubMed] [Google Scholar]
- The critical shoulder angle is associated with rotator cuff tears and shoulder osteoarthritis and is better assessed with radiographs over MRI. Knee Surg Sports Traumatol Arthrosc. 2016;24:2244-51.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between the critical shoulder angle and the incidence of chronic, full-thickness rotator cuff tears and outcomes after rotator cuff repair: A systematic review. Arthroscopy. 2019;35:3135-43.e4.
- [CrossRef] [PubMed] [Google Scholar]
- Critical shoulder angle (CSA): Age and gender distribution in the general population. J Orthop Traumatol. 2022;23:10.
- [CrossRef] [PubMed] [Google Scholar]
- Predominance of the critical shoulder angle in the pathogenesis of degenerative diseases of the shoulder. J Shoulder Elbow Surg. 2016;25:1328-36.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of radiographic viewing perspective and demographics on the critical shoulder angle. J Shoulder Elbow Surg. 2015;24:e149-58.
- [CrossRef] [PubMed] [Google Scholar]
- The ratio of the transverse to longitudinal diameter of the glenoid projection is of good predictive value for defining the reliability of critical shoulder angle in nonstandard anteroposterior radio-graphs. Arthroscopy. 2021;37:438-46.
- [CrossRef] [PubMed] [Google Scholar]
- Supraspinatus tendon load during abduction is dependent on the size of the critical shoulder angle: A biomechanical analysis. J Orthop Res. 2014;32:952-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: A systematic review and meta-analysis. Br J Sports Med. 2015;49:1316-28.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589-604.
- [CrossRef] [PubMed] [Google Scholar]
- Is there an association between the “critical shoulder angle” and clinical outcome after rotator cuff repair? Orthop J Sports Med. 2017;5:2325967117702126. Doi: 10.1177/2325967117702126
- [CrossRef] [PubMed] [Google Scholar]
- The critical shoulder angle is associated with osteoarthritis in the shoulder but not rotator cuff tears: A retrospective case-control study. J Shoulder Elbow Surg. 2017;26:2097-102.
- [CrossRef] [PubMed] [Google Scholar]






