Translate this page into:
Variability in quadrupled hamstring tendon autograft diameter in North Indian population and its impact on anterior cruciate ligament (ACL) reconstruction outcomes
*Corresponding author: Anil Kapoor, Department of Orthopedics, IVY Hospital Mohali, Punjab, India. anil88gmch@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta RK, Poudel N, Dudeja V, Bansal H, Kapoor A. Variability in quadrupled hamstring tendon autograft diameter in North Indian population and its impact on anterior cruciate ligament (ACL) reconstruction outcomes. J Arthrosc Surg Sports Med. 2023;4:40-2. doi: 10.25259/JASSM_20_2023
Abstract
Objectives:
This study aimed to see the mean quadruple hamstring tendon (HT) graft in the North Indian population and the effect of height and gender on graft diameter.
Materials and Methods:
Three hundred and twelve patients who underwent anterior cruciate ligament reconstruction using quadruple HT graft with preserved insertions were included in the study. Quadruple graft diameter is calculated using a sizing tube and its correlation with height, gender, and body mass index was calculated. All patients were followed up for a minimum of 2 years, and the incidence of graft failure was calculated.
Results:
The mean graft diameter in the present study was 7.6 mm; taller patients and male gender have thicker grafts. About 63% of patients had graft diameters <8 mm. The incidence of graft failure rate was 2.5% and 0.8% in patients with graft diameters <8 mm and ≥8 mm, respectively.
Conclusion:
In the present study, the average quadruple HT graft diameter in the Indian population was 7.6 mm, and graft diameter depends on the height and gender of the patient.
Keywords
Anterior cruciate ligament (ACL)
Sports injuries
Hamstring tendon graft
INTRODUCTION
Arthroscopic anterior cruciate ligament reconstruction (ACLR) remains the mainstay of treatment for anterior cruciate ligament (ACL) tear.[1] Hamstring tendon (HT) graft and bone patellar tendon bone graft (BPTB) are commonly used autografts for ACLR.[2] Till now, the BPTB graft is considered a superior graft for ACLR.[3] However, in the past two decades, HT graft has become more popular due to fewer donor site morbidities, but the downside of HT graft is the variable diameter of the graft. Recent studies suggested that a graft diameter of 8 mm is associated with a higher graft failure rate and inferior functional outcomes.[4-7] To counter this problem, many surgeons have now even shifted to peroneus longus graft;[8,9] However, some surgeons still believe that peroneus longus graft should be reserved for multi-ligamentous injury.
HT graft diameter depends on the height, gender, and ethnicity of the patient.[10-13] HT graft of 8 mm or more is common among the Western population; however, in the Asian population where the average height is relatively shorter, it is expected to have a smaller diameter graft. In the present study, it was hypothesized size of 8 mm or more graft size will not be feasible to achieve in the majority of the patients using quadruple HT graft, and the graft failure rate will be higher in patients with graft size <8 mm.
MATERIALS AND METHODS
Three hundred twelve patients (252 males and 60 females) with ACL injury were included in the study. Consent for participation in the study was received from all the patients. Both professional and recreational were enrolled in the study. Patients age <16 years, undergoing revision ACL surgery, suffering from inflammatory arthritis, or having a premature graft amputation while harvesting were excluded from the study. HT graft with preserved tibial insertion was used in all the patients.[14] Sizing tubes calibrated to 0.5 mm (Smith and Nephew Ltd., Mumbai, India) were used to measure the diameter of quadrupled hamstring autograft [Figure 1]. The minimum diameter allowing smooth graft passage was recorded as the graft diameter for the study. Fiber tape is not used in any of the cases. Depending on the diameter of the graft, patients were categorized into two groups: <8 mm and ≥8 mm. Patient anthropometric measurement (height, weight, and body mass index) was taken. A minimum follow-up of 24 months was achieved in all the patients.
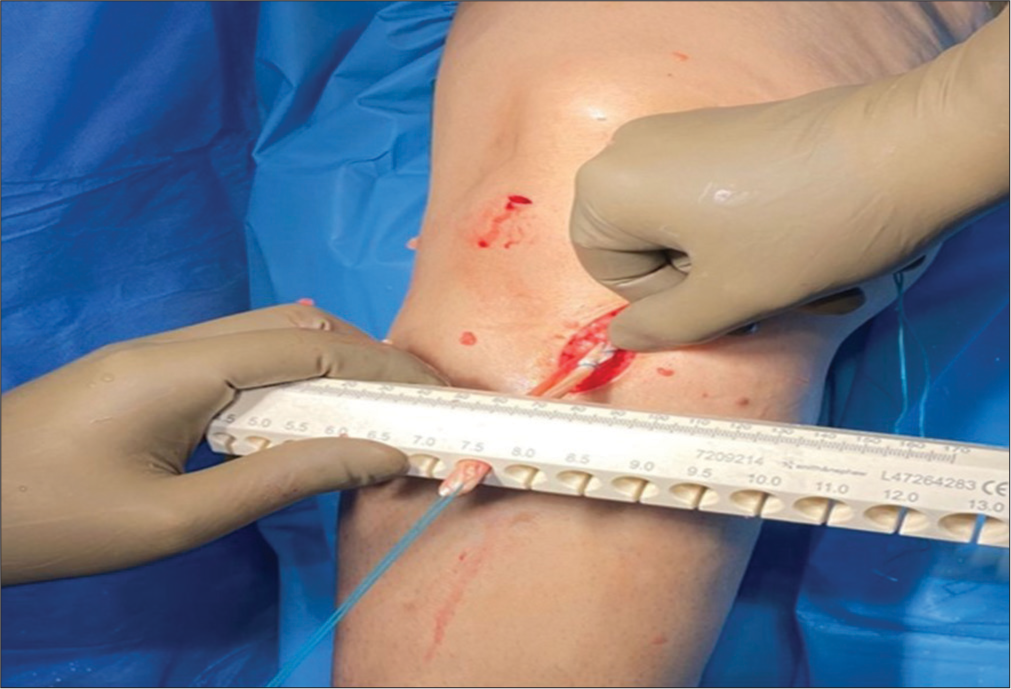
- Quadrupled hamstring autograft measured using 0.5-mm incremented sizing tubes.
RESULTS
A total of 312 patients were included in the study, with a mean age of 24.7 ± 3.6 years. There were 252 males and 60 females in this study. The HT graft diameter was 7.6 ± 0.6 mm (females 7.1 ± 0.4 mm and males 7.7 ± 0.5 mm). One hundred and ninety-seven patients had graft diameters <8 mm, and 115 patients had graft diameters ≥8 mm [Figure 2]. It was observed that graft size depends on the height and gender of the patient [Table 1]. 6/312 (2%) patients had graft rupture; all these patients underwent revision ACLR using BPTB graft. 5/197 patients with graft diameter ≥8 mm and 1/115 patients with graft diameter <8 mm had graft failure at a mean follow-up of 34 ± 6.3 months.
| <8 mm (n=197) |
>8 mm (n=115) |
P-value | |
|---|---|---|---|
| Mean age (years) | 24.9±5.2 | 24.5±5.1 | n.s. |
| Gender | 139:58 | 113:2 | 0.0001 |
| Height (cm) | 168.8±5.4 | 179.8±6.9 | 0.0001 |
| Weight (kg) | 67.3±7.3 | 77.2±10.5 | 0.0001 |
| Body mass index | 23.5 | 23.9 | n.s |
| Graft rupture | 5/197(2.5%) | 1/115 (0.8%) |
n.s.: Not significant
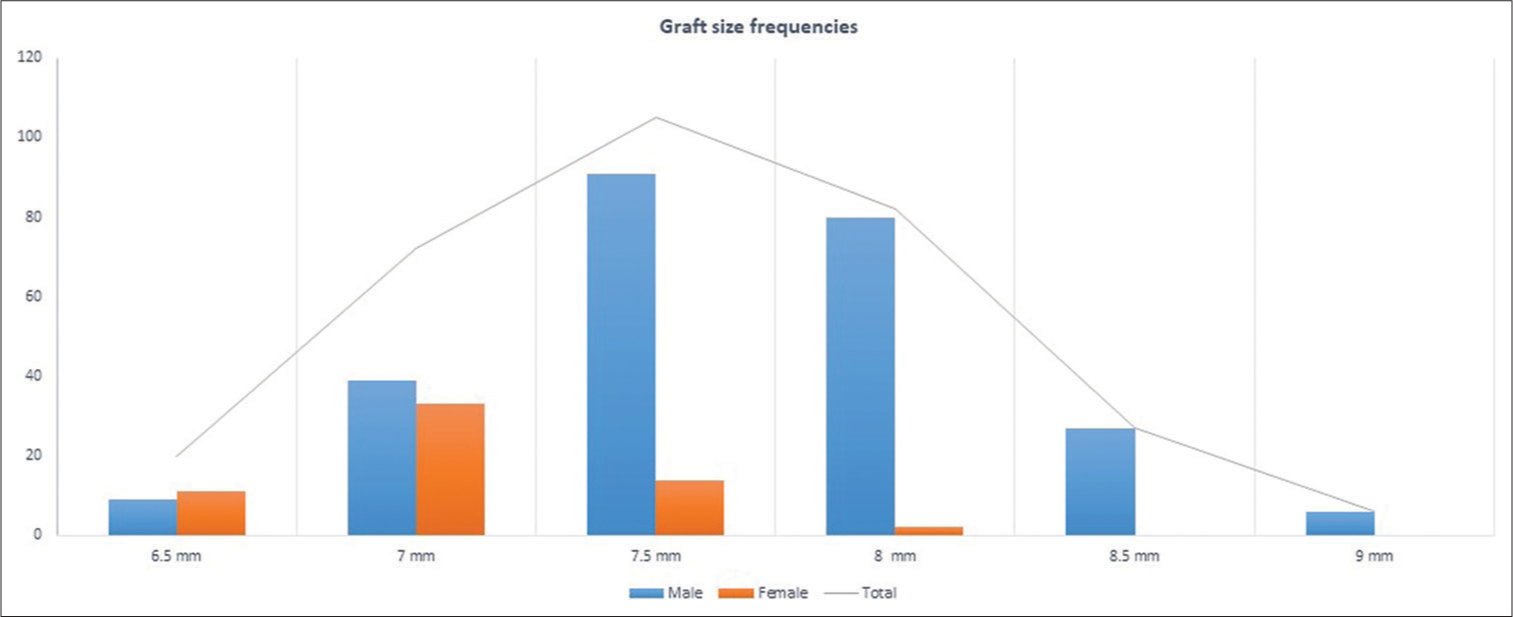
- Variation of graft size among male and female patients.
DISCUSSION
The mean graft diameter in this study came out to be 7.6 ± 0.6 mm. 63% of patients are unable to achieve a diameter of 8 mm or more. Previous studies suggested that the mean graft diameter in the Indian population varies from 7.5 mm to 8 mm.[11,15,16]
The present study suggested that graft diameter depends on the height and gender of the patient. These results are in agreement with previous literature, which suggested that graft diameter is higher in taller and male patients.[10-12]
Graft diameter is a topic of concern among arthroscopic surgeons, especially for the Asian population. To achieve the magical number of 8 mm, many innovative techniques have been adopted by surgeons, such as the use of five or six-stand HT grafts, the use of fiber tape, or alternative grafts (peroneus longus or BPTB graft). Although most of the previous studies that suggested the magical number of 8 mm for ACL graft are from the Western population, there is limited data on the Indian population.
In this study, the graft failure rate at two years of follow-up was 2% (6/312). The graft failure rate was 2.5% and 0.8% in patients with graft diameters <8 mm and ≥8 mm, respectively. The total number of patients with graft failure is few; therefore, the effect of graft size on graft rupture cannot be established. Park et al. observed a 4% graft failure rate at a minimum 2-year follow-up.[17] In previous studies, it was observed that graft size <8 mm is associated with higher graft failure.[18,19] A study of a large cohort with graft rupture is required to establish the relationship between graft diameter and graft failure rate among the Indian population.
The results of the present study suggested that a size of 8 mm could not be achieved in the majority of the patients. It is also still unclear whether this magical number of 8 mm is required for all ACLRs. In native knee, ACL cross-sectional diameter is variable and depends on age, sex, and anthropometric measurement of the patient.[20,21] If a graft of 8 mm or more is used in a knee whose native ACL volume is less, it can cause overstuffing of the knee. ACL graft diameter is still a controversial topic, and there is a need for further research before we adopt the policy of a minimum of 8-mm graft diameter in all ACLR surgery for the Indian population.
CONCLUSION
In the present study, the average quadruple HT graft diameter in the Indian population was 7.6 mm, and graft diameter depends on the height and gender of the patient.
Ethical approval
Institutional Review Board approval is not required as it is an observational study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Ravi Gupta is on the Editorial Board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Current trends in anterior cruciate ligament reconstruction. Am J Sports Med. 1999;27:821-30.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft is associated with higher and earlier return to sports as compared to hamstring tendon graft. Knee Surg Sports Traumatol Arthrosc. 2020;28:3659-65.
- [CrossRef] [PubMed] [Google Scholar]
- Controversies in ACL reconstruction: bone-patellar tendon-bone anterior cruciate ligament reconstruction remains the gold standard. Sports Med Arthrosc Rev. 2009;17:242-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hamstring autograft size importance in anterior cruciate ligament repair surgery. EFORT Open Rev. 2018;3:93-7.
- [CrossRef] [PubMed] [Google Scholar]
- Autograft diameter in ACL reconstruction: Size does matter. SICOT J. 2021;7:16.
- [CrossRef] [PubMed] [Google Scholar]
- Does hamstring graft size affect functional outcome and incidence of revision surgery after primary anterior cruciate ligament (ACL) reconstruction? Cureus. 2022;14:e21158.
- [CrossRef] [Google Scholar]
- Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526-31.
- [CrossRef] [PubMed] [Google Scholar]
- Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3552-9.
- [CrossRef] [PubMed] [Google Scholar]
- Single bundle ACL reconstruction with peroneus longus tendon graft: 2-years follow-up. J Clin Orthop Trauma. 2020;11:S332-6.
- [CrossRef] [PubMed] [Google Scholar]
- Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature review. Int Orthop. 2016;40:173-81.
- [CrossRef] [PubMed] [Google Scholar]
- Hamstring graft size and anthropometry in south Indian population. J Clin Orthop Trauma. 2013;4:135-38.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of anthropometric features on graft diameter in ACL reconstruction. Arch Orthop Trauma Surg. 2013;133:215-8.
- [CrossRef] [PubMed] [Google Scholar]
- Can pre-operative measures predict quadruple hamstring graft diameter? Knee. 2010;17:81-3.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction using hamstring tendon autograft with preserved insertions. Arthrosc Tech. 2016;5:e269-74.
- [CrossRef] [PubMed] [Google Scholar]
- Quadrupled hamstring graft diameter adequacy in anterior cruciate ligament reconstruction using patient anthropometry: A prospective cohort study in Indian males. Cureus. 2021;13:e15920.
- [CrossRef] [Google Scholar]
- Does hamstring tendon graft diameter affect the outcome of anterior cruciate ligament surgery? Sports Orthop Traumatol. 2019;35:166-70.
- [CrossRef] [Google Scholar]
- Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1111-8.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of hamstring autograft diameter on graft failure rate in Chinese population after anterior cruciate ligament reconstruction. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2020;22:45-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30:882-90.
- [CrossRef] [PubMed] [Google Scholar]
- Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry: A cadaveric study. Am J Sports Med. 2005;33:1492-8.
- [CrossRef] [PubMed] [Google Scholar]
- Age, sex, body anthropometry, and ACL size predict the structural properties of the human anterior cruciate ligament. J Orthop Res. 2011;29:993-1001.
- [CrossRef] [PubMed] [Google Scholar]







