Translate this page into:
Variations in functional outcome based on hamstring autograft thickness estimated using transportal technique in arthroscopic anterior cruciate ligament reconstruction
*Corresponding author: S. Venkatesh Kumar, Department of Orthopaedics, Dhanalakshmi Srinivasan Medical College and Hospital, Perambalur, Tamil Nadu, India. mailvenkatesh91@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Radhik KR, Arumugam AK, Manooj Kumar V, Venkatesh Kumar S, Koramutla HK. Variations in functional outcome based on hamstring autograft thickness estimated using transportal technique in arthroscopic anterior cruciate ligament reconstruction. J Arthrosc Surg Sports Med. doi: 10.25259/JASSM_58_2024
Abstract
Objectives:
We aimed to study the functional outcome difference in arthroscopic anterior cruciate ligament reconstruction (ACLR) using hamstring autograft thickness between more than 85% and ≤85%.
Materials and Methods:
In our study, 50 patients with anterior cruciate ligament (ACL) tears were operated with arthroscopic ACLR using an autologous hamstring graft. The anteroposterior diameter (APD) of the tibial footprint of ACL is measured using an arthroscopic ruler using a transportal and the graft thickness of more than 70% of the tibial footprint APD was used. The international knee documentation committee and knee society score (KSS) were compared between the groups in the 1st month, 6th month, and 12th month between autograft thickness of >85% and ≤85%.
Results:
The mean IKDC scores of patients with graft thickness >85% were higher compared to graft thickness ≤85% in the 6th and 12th post-operative months, with a statistically significant difference at the 12th post-operative month. The mean KSS scores of patients with graft thickness >85% were higher compared to graft thickness ≤85% at the 3rd, 6th, and 12th post-operative months, with a statistically significant difference at the 12th post-operative month.
Conclusion:
The functional scores were better for autograft thickness of more than 85% compared to autograft thickness of ≤85% at short-term follow-up of the 3rd and 6th post-operative month with a statistical difference at long-term follow-up of the 12th month.
Keywords
Anterior cruciate ligament reconstruction
Hamstring autograft thickness
International Knee Documentation Committee score
Knee Society score
Transportal approach
INTRODUCTION
The arthroscopic anterior cruciate ligament reconstruction (ACLR) is one of the most common surgeries in orthopedic surgery done for complete anterior cruciate ligament (ACL) tears.[1] Several studies have also shown that autograft and allograft (patellar tendon, hamstring tendon, tibialis anterior, and Achilles tendons) may successfully reconstruct the ACL.[2,3] However, no convincing data currently exist regarding recent trends for the appropriate thickness of the graft to be used, especially in the Indian subcontinent. Adequate thickness of the graft for a primary ACLR determines the functional and morbidity status following the surgery, thereby providing better outcomes in the ACL deficient knees. The study’s major goal is to assess the average anterior-posterior diameter (APD) of the tibial footprint during arthroscopic ACLR and its functional outcome to determine optimum graft thickness using a transportal technique.
MATERIALS AND METHODS
Sample size
This prospective study was carried out in a tertiary care center from August 2019 to March 2021 in South India. The Institutional Ethical Committee has sanctioned our study in 50 patients with ACL tears calculated by the “Complete Enumeration Method” by which, taking all the cases that comes between the study periods.
Participants
Out of 100 patients who were screened, 50 were selected according to the criteria [Table 1].
| Inclusion criteria | Exclusion criteria |
|---|---|
| MRI confirmed 20–50-year-old patients with full thickness ACL tear |
|
MRI: Magnetic resonance imaging, ACL: Anterior cruciate ligament, PCL: Posterior cruciate ligament
Allocation and implementation
After taking informed consent, the target population was selected with similar baseline characteristics.
Interventions
The anteromedial and anterolateral portals were made and diagnostic examination of the knee was done to diagnose any associated injury to the knee. The ACL footprint was identified and remnants were removed from the tibial notch. The APD of the tibial footprint of ACL is measured using an arthroscopic ruler through transportal [Figures 1 and 2]. The gracilis and semitendinosus tendons were harvested and prepared. The ideal graft thickness of more than 70% of the tibial footprint APD was adhered to in all the cases.

- Arthroscopic ruler.
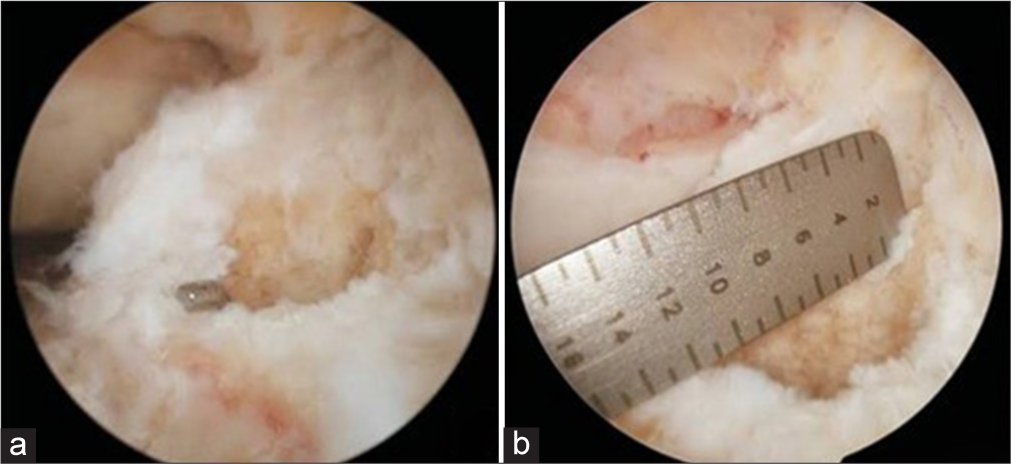
- (a) The anteroposterior diameter of the tibial footprint of the anterior cruciate ligament is measured using (b) an arthroscopic ruler.
The femoral footprint has marked at the center with an awl. The anatomical femoral and tibial tunnels were prepared meticulously to prevent non-anatomical tunnel placements in both coronal and sagittal planes. We used a fixed loop device and the graft was fixed to the femur. Following that, repeated flexing-extending cycles of the knee were done to pre-install the graft. The tibial fixation was done with an ideal amount of tension using absorbable interference screws. After performing ACL reconstruction, other minor Grade-1 and 2 meniscal tears were identified and conservative management was carried out accordingly.
Objectives
To determine the average thickness of the autograft compared to the normal tibial footprint of the ACL of the individual using an arthroscopic ruler
To determine the postoperative clinical outcome at the 3rd month, 6th month, and 1st year postoperatively to assess the outcomes.
Outcomes
The assessment was done using:
The average thickness of the autograft for ACL was measured using an arthroscopic ruler
-
The functional outcome postoperatively was done using
International Knee Documentation Committee (IDKC)
Knee society score (KSS).
Statistical analysis
To find the significant difference between the bivariate samples in independent groups, the independent sample t-test was used.
Post-operative protocol
Proper wound care, along with phase 1–4 ACL rehabilitation protocol was followed. The sutures were removed on an average of 12th post-operative day. The patients were followed up post operatively at 3rd month, 6th month, and 12th months. The Lachman test, anterior drawer test, pivot shift test, and knee’s range of motion were examined clinically. The X-rays were taken to study the screw location and tunnel positioning. The functional scoring was done using IKDC and KSS scores.
RESULTS
Observations and results
In our study, the average age was 26 years. The youngest patient was 23 years old, while the oldest was 45. Magnetic resonance imaging confirmed associated medial meniscal tear in 10% and lateral meniscal injury in 4% of our patients with no occurrences of concomitant medial and lateral meniscal tears. We measured tibial footprint APD in our patients, with six patients having 9 mm (12%), 20 patients having 10 mm and 11 mm each (80% in total), and four patients having 12 mm anterior-posterior (AP) diameter (8%). The maximum number of patients had a mean APD of 10–11 mm [Table 2].
| Frequency | Percentage | |
|---|---|---|
| Gender | ||
| Female | 10 | 20 |
| Male | 40 | 80 |
| Mechanism of injury | ||
| Road traffic accident | 26 | 52 |
| Sport | 24 | 48 |
| Side | ||
| Left | 20 | 40 |
| Right | 30 | 60 |
| Associated injury | ||
| Grade-III lateral meniscal injury | 1 | 2 |
| Grade-III medial meniscal injury | 3 | 6 |
| Nil | 46 | 92 |
| Graft % | ||
| ≤85% | 24 | 48 |
| >85% | 26 | 52 |
| Tibial footprint anteroposterior diameter | ||
| 9 mm | 6 patients | 12 |
| 10 mm | 20 patients | 40 |
| 11 mm | 20 patients | 40 |
| 12 mm | 4 patients | 8 |
IDKC score
The mean IKDC scores of patients with graft thickness ≤85% were slightly better compared to graft thickness >85% at 3rd post-operative month with a statistically insignificant difference. However, the mean IKDC scores of patients with graft thickness >85% were higher compared to graft thickness ≤85% in the 6th and 12th post-operative months. However, the difference was statistically insignificant at the 6th postoperative months with a statistically significant difference at the 12th post-operative month [Table 3].
| IDKC | Graft % | n | Mean | SD | t-value | P-value |
|---|---|---|---|---|---|---|
| Pre | ≤85 | 24 | 51.54 | 7.03 | 1.199 | 0.237# |
| 26 | 49.23 | 6.60 | ||||
| 3 months | ≤85 | 24 | 63.17 | 6.08 | 0.808 | 0.423# |
| 26 | 61.88 | 5.13 | ||||
| 6 months | ≤85 | 24 | 77.25 | 8.11 | 1.401 | 0.169# |
| 26 | 80.00 | 5.37 | ||||
| 12 months | ≤85 | 24 | 85.83 | 9.02 | 2.454 | 0.019* |
| 26 | 91.15 | 5.84 |
KSS score
The mean KSS scores of patients with graft thickness >85% were higher compared to graft thickness ≤85% at 3rd, 6th, and 12th post-operative months. However, the difference was statistically insignificant at 3rd and 6th post-operative months with a statistically significant difference at the 12th postoperative month [Table 4].
| KSS | Graft (%) | N | Mean | SD | t-value | P-value |
|---|---|---|---|---|---|---|
| Pre | ≤85 | 24 | 76.17 | 13.57 | 0.375 | 0.709# |
| 26 | 74.92 | 9.68 | ||||
| 3 months | ≤85 | 24 | 23.33 | 6.36 | 0.462 | 0.646# |
| 26 | 24.19 | 6.75 | ||||
| 6 months | ≤85 | 24 | 67.96 | 17.82 | 1.514 | 0.137# |
| 26 | 74.77 | 13.88 | ||||
| 12 months | ≤85 | 24 | 75.75 | 13.94 | 1.995 | 0.05* |
| 26 | 82.54 | 10.49 |
DISCUSSION
ACLR with the hamstring tendon has become a common and most preferred tendon graft for surgeons and it has shown itself to be efficient inadequately selected individuals.[4] A good functional outcome depends on graft size, tunnel position, fixation methods, treatment of associated lesions, and proper rehabilitation after surgery. Biomechanically, both hamstring and bone patellar tendon bone graft show similar properties.[5] We used absorbable interference screws for graft fixation in all our cases. Several recent meta-analyses and network meta-analyses have demonstrated a similar functional outcomes in the fixation methods.[6,7]
We studied the variance in the functional outcome of autograft thickness at the tibial footprint measured using an arthroscopic ruler through an arthroscopic trans-portal approach during ACLR. The femoral footprint occupies 70% of the area compared to tibial insertion and the substance of ACL constitutes only about 50% of tibial insertion. This shows that the tibial insertion footprint is the single most important measurement required for pre-operative planning of individualized ACLR.[8,9]
The APD of the tibial footprint aids in determining the graft’s adequacy and the ideal thickness of the graft to be placed should be >70% of the tibial footprint APD[10] and it is one of the important components to regain a functionally stable knee joint. Furthermore, an inadequate graft size may result in graft failure. However, the literature on the autograft thickness on the functional outcome is rare. Hence, we studied the difference in functional outcome in ACLR autograft thickness between graft thickness >85% and graft thickness ≤85%.
Studies have shown that revision surgery is more common among grafts with a diameter of 7 mm or less.[11,12] According to Spragg et al.,[11] the patients that required revision surgery more often with the graft thickness falling between 7.0 and 7.5 mm on the lesser side. Mariscalco et al.[12] state that an inadequate graft size is directly proportional to poor functional score and increased revision rate. Treme et al.[13] proposed that the graft diameter of <7 mm will have a higher risk of failure. Conte et al.[14] state that the ACLR using hamstring autograft with a diameter 8 mm or more increases the success rates compared to graft diameter <8 mm. Howe et al.[15] reported that 96% patients were content with their functional results, while only 4% patients had unsatisfied results in their long-term follow-up.
Similarly, Chen et al.[16] reported to have normal or nearly normal IKDC scores in 91% patients undergoing ACL surgery. Khajotia et al.[17] recorded a mean graft diameter of 8.24 mm from their study and the IKDC score was normal in 84% of patients and only 26% of patients had an abnormal score. Chodavarapu et al.[18] state that with a mean graft diameter of 7.9 mm that 84% of patients regained pre-injury level activity. The post-operative IDKC scores were 0–60 in 72% patients and 24% patients had a score at 60–70.
The mean IKDC scores of patients with graft thickness ≤85% were insignificantly higher than graft thickness >85% at 3rd post-operative month, but the scores of patients with graft thickness >85% were insignificantly higher than graft thickness ≤85% in the 6th postoperative month. However, the IDKC score difference was statistically higher for graft thickness >85% than graft thickness >85% at the 12th postoperative month. The mean KSS scores of patients with graft thickness >85% were insignificantly higher compared to graft thickness ≤85% at 3rd and 6th post-operative months. However, the KSS score difference was statistically higher for graft thickness >85% than graft thickness >85% at the 12th post-operative month.
Hence, both the IDKC and KSS scores were better for graft thickness >85% compared to graft thickness ≤85% at the early post-operative months with a statically significant better scores for graft thickness >85% at 12th post-operative month. From our study, we can say that the functional outcomes were better for patients with graft thickness more than or equal to 85%.
Confounding factors of this study are anatomical femoral tunnel placements, femoral tunnel diameter, graft bending angle, and graft fixation methods.[19] The post-operative stiffness, instability, infection, arthrofibrosis, complex regional pain syndrome, and synovitis were the common complications[20] and were not recorded in our study. Clinically, studies comparing different hamstring and quadriceps tendon graft preparations, thickness, and fixation are needed. Larger comparative studies are also needed to validate the results for the specific study populations. Finally, the current literature lacks long-term follow-up studies and higher level of evidence studies is also needed.
CONCLUSION
Our study evaluated the relationship between ACL graft APD thickness and patient-reported functional outcome scores, which was done rarely in the literature. We conclude from our study that the patients with graft thickness more than 85% of tibial AP footprint had better short-term functional outcome and a significant long-term outcome at 12th post-operative month compared to patients with ≤85% graft thickness in arthroscopic ACL reconstruction using transportal approach.
Author contributions
KRR and HKK: Conceptualization and supervision; SVK, KRR, AKA, VMK: Writing- original draft preparation. KRR: Data acquisition, analysis and interpretation. SVK and KRR: Critical review and final approval.
Ethical approval
The research/study was approved by the Institutional Review Board at Narayana Medical College, Nellore, number NMC/Adm/Ethics/approval/Ortho/005/11/2019, dated November 19, 2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am. 1980;62:259-70.
- [CrossRef] [PubMed] [Google Scholar]
- Graft selection in anterior cruciate ligament reconstruction. Sports Med Arthrosc Rev. 2020;28:41-8.
- [CrossRef] [PubMed] [Google Scholar]
- ACL Study Group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Knee Surg Sports Traumatol Arthrosc. 2021;29:3871-6.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction in patients over 40 years using hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2010;18:68-72.
- [CrossRef] [PubMed] [Google Scholar]
- Current trends in graft choice for anterior cruciate ligament reconstruction-Part I: Anatomy, biomechanics, graft incorporation and fixation. J Exp Orthop. 2023;10:37.
- [CrossRef] [PubMed] [Google Scholar]
- Bone-patellar tendon-bone autografts versus hamstring autografts using the same suspensory fixations in ACL reconstruction: A systematic review and meta-analysis. Orthop J Sports Med. 2019;7:2325967119885314.
- [CrossRef] [PubMed] [Google Scholar]
- What is the best femoral fixation of hamstring autografts in anterior cruciate ligament reconstruction?: A meta-analysis. Clin Orthop Relat Res. 2011;469:1075-81.
- [CrossRef] [PubMed] [Google Scholar]
- The concept of complete footprint restoration with guidelines for single-and double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:699-706.
- [CrossRef] [PubMed] [Google Scholar]
- Size of the tibial footprint of anterior cruciate ligament: MRI study. BBMed. 2020;4:21-5.
- [Google Scholar]
- The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:1475-81.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29:1948-53.
- [CrossRef] [PubMed] [Google Scholar]
- Hamstring graft size prediction: A prospective clinical evaluation. Am J Sports Med. 2008;36:2204-9. Erratum in: Am J Sports Med. 2009;37:836
- [CrossRef] [PubMed] [Google Scholar]
- Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30:882-90.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction using quadriceps patellar tendon graft. Part I. Long-term followup. Am J Sports Med. 1991;19:447-57.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon autograft: Clinical outcome in 4-7 years. Knee Surg Sports Traumatol Arthrosc. 2006;14:1077-85.
- [CrossRef] [Google Scholar]
- Functional outcome of arthroscopic reconstruction of anterior cruciate ligament tear using peroneus longus tendon autograft. Int J Res Orthop. 2018;4:898.
- [CrossRef] [Google Scholar]
- Analysis of functional outcome of anterior cruciate ligament reconstruction using quadruple hamstring graft. Int J Res Orthop. 2017;3:877-82.
- [CrossRef] [Google Scholar]
- ACL graft matching: Cadaveric comparison of microscopic anatomy of quadriceps and patellar tendon grafts and the femoral ACL insertion site. Am J Sports Med. 2022;50:2953-60.
- [CrossRef] [PubMed] [Google Scholar]
- Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg. 2015;3:220-40.
- [Google Scholar]






