Translate this page into:
Recent advances and future trends in shoulder arthroscopy

*Corresponding author: Deepak N. Bhatia, Department of Shoulder Elbow and Wrist Surgery, Sportsmed Mumbai, Mumbai, Maharashtra, India. shoulderclinic@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: DeNiese P, Bhatia DN. Recent advances and future trends in shoulder arthroscopy. J Arthrosc Surg Sport Med 2020;1(1):16-22.
Abstract
Shoulder arthroscopy has evolved significantly over the past decade. Treatment algorithms have evolved in sync with results from cadaveric, biomechanical, and clinical studies, and newer minimally invasive and biomechanically proven surgical techniques have replaced suboptimal procedures. Advances in arthroscopy have influenced three key aspects of shoulder problems: Anterior instability, rotator cuff tears, and osteoarthritis. A new frontier of “endoscopic” extra-articular procedures has evolved and these procedures have convincingly replaced traditional open surgeries. The current evidence suggests a growing trend for arthroscopic procedures in joint preservation and restoration.
Keywords
Shoulder arthroscopy
Latarjet procedure
Rotator cuff
Biceps autograft
INTRODUCTION
Shoulder arthroscopy has evolved significantly over the past decade. Basic science studies have provided vital insights into pathoanatomy of common disabling injuries and failure mechanisms of surgical procedures. Treatment algorithms have evolved in sync with results from cadaveric, biomechanical, and clinical studies, and newer minimally invasive and biomechanically proven surgical techniques have replaced suboptimal procedures. Innovations in medical devices have led to the development of newer biomaterials and delivery devices and biomechanically superior fixation implants. Advances in surgical skills and technical expertise have led to a new frontier of endoscopic extra-articular procedures that have convincingly replaced traditional open surgeries. This article presents a summary of the most recent advances in shoulder arthroscopy and futuristic trends in management of common shoulder problems.
SHOULDER ARTHROSCOPY PROCEDURES
Advances in arthroscopy have positively influenced three major shoulder problems: Anterior instability, rotator cuff tears, and osteoarthritis.
Anterior glenohumeral instability
Arthroscopic management of shoulder instability has undergone a paradigm shift after introduction of the concept of significant glenohumeral bone defects.[1,2] Several recent clinical and biomechanical studies have challenged the standard definition of “critical” glenoid bone loss of 25%. Recent clinical and biomechanical studies have reported a high failure rate of arthroscopic repair with “subcritical” bone loss ranging from 13.5% to 17% and biomechanical studies have redefined critical loss as 15% of the largest anteroposterior width of glenoid for defects perpendicular to the superoinferior glenoid axis.[3-5] Cadaveric analysis of sequential changes in glenoid geometry with progressive bone loss suggests that a significant change in glenoid area and arc length occurs between glenoid width loss between 10% and 20%, and a significant change in glenoid version (retroversion to anteversion) is seen with glenoid bone loss over 20–30%.[6] This analysis is supported by biomechanical data that show a decrease in stability even with glenoid bone loss as small as 2 mm (7.5%) of the glenoid width. It is recommended that bony restoration should be performed whenever bone loss exists and particularly for defects that are in line with the superior-inferior axis of the glenoid.[7]
Decision-making algorithms for anterior instability have undergone modifications based on the newer clinical and basic science studies. The interrelationship of glenoid and humeral defects (glenoid track concept) has evolved and two subgroups of on-track lesions (peripheral-track and central- track lesions) have been suggested. Peripheral-track lesions with the Hill-Sachs occupancy ≥75% resulted in significantly worse outcomes without recurrent instability events when assessed with a disease-specific quality of life questionnaire.[8] The Glenoid Track Instability Management Score (GTIMS) incorporated the glenoid track concept into the instability severity index score and the study found that the GTIMS could possibly more accurately predict failure after arthroscopic Bankart repair and therefore could be used to identify patients better suited for a Latarjet procedure.[9] An “integrated algorithmic approach” based on sequential alteration of several glenoid geometry parameters suggested that glenoids with defects up to 10% of widest anteroposterior diameter were not significantly different from those of normal glenoids, and therefore, soft-tissue repairs were recommended for this subgroup.[6,10] The significance of 10% glenoid defect was further highlighted in a recent study that analyzed a statistical model of anatomic risk factors to predict recurrent instability after primary arthroscopic capsulolabral repair; the analysis demonstrated a 7.5 times increased risk of failure with glenoid bone loss more than 10% and this was also the largest contributor to post-operative failure in the statistical model.[11]
The overall evidence favors three key surgical procedures in anterior instability:
Arthroscopic Bankart repair combined with remplissage procedure
In a systematic review of the treatment of subcritical glenoid bone loss, the addition of a Hill-Sachs remplissage procedure to anterior labral repair demonstrated favorable rates of recurrent instability and a negligible loss of external rotation when compared with isolated Bankart repair.[12] At a minimum 10-year follow-up analysis, Bankart repair combined with remplissage showed better functional results (mobility and stability scores) than Bankart repair only without the limitations of pain and restriction of motion.[13] Finally, a concomitant remplissage procedure did not correlate with subjective patient dissatisfaction.[14] Newer remplissage techniques involve trans-tendon double-pulley techniques and specialized remplissage knots (double-barrel remplissage) and a tripod-pulley technique [Figure 1].[15-17]

- A double-barrel remplissage technique is demonstrated. Trans-tendon anchors are inserted into the Hill-Sachs lesion (left image) and a sliding self-retaining double-pulley knot (double- barrel knot) is used to approximate the infraspinatus into the humeral defect (right image). H: Humeral head, IS: Infraspinatus.
Open bone grafting procedures
A prospective randomized study analyzed the Latarjet and iliac crest bone graft transfer procedures for the treatment of anterior shoulder instability with glenoid bone loss and found no difference in clinical and radiologic outcomes.[18] Recent basic science studies have analyzed the restorative possibilities of Latarjet procedures (classic and congruent- arc modifications) and distal clavicular autograft (DCA) procedure for instability-related anterior glenoid bone loss.[6,19] The classic Latarjet and DCA were suitable for glenoid defects of 20–25% and the congruent-arc Latarjet corrected all articular parameters even in 30–40% defects.
Arthroscopic bone grafting procedures
Open glenoid grafting can now be performed with arthroscopic techniques; several arthroscopic bone grafting procedures have emerged recently and mid-term results are encouraging [Figure 2]. Development of specialized instrumentation and graft fixation devices (cortical button and screws) has made these procedures safe and reproducible. A biomechanical evaluation of graft fixation techniques found that cortical button and screw fixation techniques exhibited comparable biomechanical strength for coracoid bone block fixation.[20] A more recent analysis suggested that the cortical button fixation did not resist direct loads to the graft as much as traditional screw fixation; however, bony damage to the surrounding anatomy was more extensive in screw fixation.[21] In a clinical study, button fixation for Latarjet showed higher rates of recurrent dislocation compared to screw fixation.[22] Newer techniques include arthroscopic iliac crest grafting, implant-free J-bone grafting, and arthroscopic congruent- arc Latarjet procedure.[23-25] A multicenter analysis of learning curves showed that surgical time in arthroscopic Latarjet significantly reduced after 20 cases; however, complication rates did not decrease over this time.[26]

- Arthroscopic Latarjet procedure is shown. G: Glenoid, Co: Coracoid.
Rotator cuff tears
The treatment of rotator cuff tears has undergone changes in the recent past and arthroscopic management of massive and potentially irreparable tears has evolved by innovations in three key areas:
Rotator cuff repairs and healing
Bioinductive scaffolds and arthroscopic delivery techniques are emerging technologies that may enhance healing potential of partial and massive rotator cuff tears. In a preclinical canine model, biological scaffolds augmented healing of articular-sided partial-thickness supraspinatus tears when compared with debridement, and decellularized human dermal allograft and amnion matrix cord scaffolds were found to have advantages over the bovine collagen patch.[27] A 2-year follow-up of large and massive rotator cuff repairs that were augmented with a bioinductive collagen scaffold patch suggested 96% radiological healing rate and no adverse events attributed to the implant.[28] In a multicenter prospective study, use of a bioinductive collagen scaffold was found to be safe and effective for intermediate- to high- grade partial-thickness rotator cuff tears of the supraspinatus tendon.[29]
Rotator cuff repair and autograft augmentation
Biceps autograft augmentation of the repaired rotator cuff has been used to recreate the superior capsular restraint and for simultaneous cuff augmentation during repair. In a large series of massive and potentially irreparable tears, the proximally attached long head of biceps tendon was used as an autograft in specific cases to augment poor quality tissue in posterosuperior tendons.[30] In a recent study, structural and clinical outcomes of three surgical techniques for massive posterosuperior tears (double-row repair, transosseous-equivalent repair with absorbable patch reinforcement, and Superior Capsular Reconstruction (SCR) with biceps autograft) were analyzed; at 24 months, the infraspinatus tendon remained healed in three-fourths of the repair group and the patch augmented group and in 100% of the biceps autograft group.[31] Biomechanical evaluation of the biceps autograft for SCR found that the biceps autograft with appropriate distal insertion on the greater tuberosity recentered the humeral head on the glenoid and provided stability in cuff deficiency [Figure 3].[32]
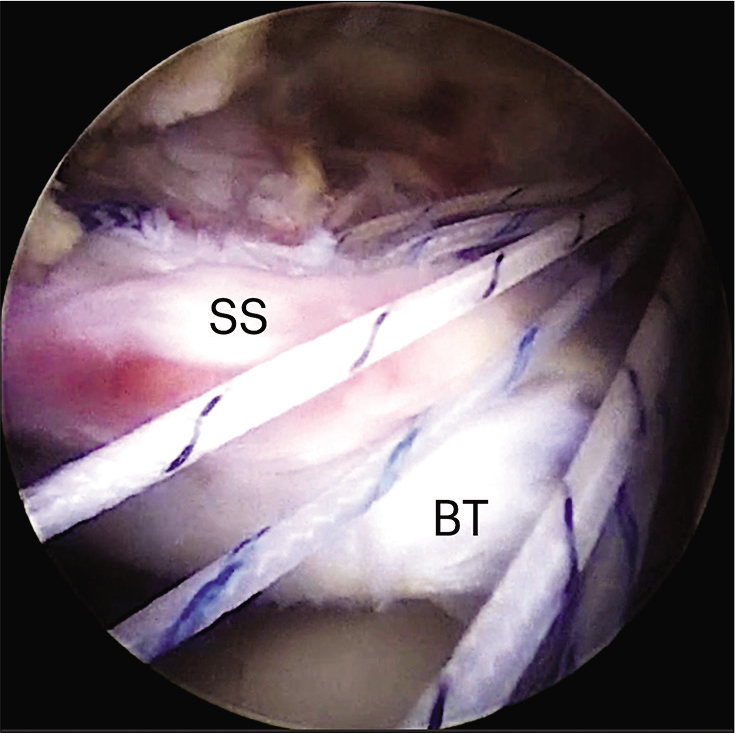
- Arthroscopic superior capsular reconstruction and cuff augmentation using the biceps autograft are demonstrated (SS: Supraspinatus, BT: Long biceps tendon).
Superior Capsular Reconstruction
Arthroscopic superior capsular reconstruction (SCR) has gained popularity and several techniques with different reconstruction tissues are currently in use. Clinical outcomes using a dermal allograft at 2 years have shown successful outcomes in 72%; graft failure was found in 16%; and revision to replacement was necessary in 12% of patients.[33]
A review of clinical outcomes comparing fascia lata autograft and human dermal allograft in arthroscopic SCR for irreparable rotator cuff tears suggested significant and clinically important improvements in clinical outcomes in both groups; however, the graft tear rate was found to be high (fascia lata autograft 5–32% and human dermal allograft 20–75%.).[34]
Glenohumeral arthritis
Arthroscopic procedures for joint preservation in severe glenohumeral osteoarthritis (GHOA) have shown favorable outcomes and should be considered in appropriately selected young and active patients. Arthroscopic glenoid resurfacing using a dermal allograft was found to be a safe option in younger patients with an acceptable rate of revision to prosthetic arthroplasty (23%) at short-term to midterm follow-up.[35] These results are similar to the previous studies that reported successful outcomes in two-thirds of patients who underwent this procedure.[36] In another study, the comprehensive arthroscopic management (CAM) procedure for GHOA showed 76.9% survivorship rate at a minimum of 5 years postoperatively. Further studies are necessary to evaluate long-term outcomes and durability after joint preserving procedures [Figure 4].[37]

- Arthroscopic options in glenohumeral osteoarthritis are demonstrated. Glenohumeral debridement and large osteophyte (OS) resection (arrows, left image) are combined with release of the axillary pouch capsule (Ax). Arthroscopic biological resurfacing is performed using a dermal allograft (G, right image) (H: Humeral head). (Right image: Courtesy Joe de Beer, used with permission).
ANESTHESIA AND POSITIONING IN SHOULDER ARTHROSCOPY
Several studies have evaluated the risk involved with shoulder arthroscopy in the beach chair position. Intravenous general anesthesia and controlled hypotension in the beach chair position (65°) were found to affect cerebral blood flow and cerebral oxygenation; the incidence of cerebral desaturation events was 25% and there were no neurological deficits.[38] In another study, pre-operative interscalene brachial plexus (BP) block and advanced age were risk factors associated with symptomatic hypotensive bradycardic events in the beach chair position.[39] The beach chair position angle was shown to affect cerebral oxygenation, and there was a linear decline in cerebral oxygenation as the position angle increased.[40] The current recommendations suggest that beach chair and lateral position are safe and successful methods for patient positioning in shoulder arthroscopic procedures without conclusive evidence of superiority of one position to the other.[41]
EMERGING FRONTIERS IN SHOULDER ARTHROSCOPY
Endoscopic extra-articular procedures
Shoulder “endoscopy” is a new and emerging frontier in arthroscopy and involves surgical procedures in extra-articular regions of the shoulder. The procedures are technically challenging and potential iatrogenic complications are possible.
Brachial plexus endoscopy
Lafosse et al. have described an all-endoscopic technique for infra- and supraclavicular brachial plexus (BP) neurolysis and have reported significant functional improvements in the selected patients suffering from non-specific neurogenic thoracic outlet syndrome.[42] The authors suggest that endoscopy may be an advantageous tool in selected cases of BP nerve sheath tumors and have further reported an all- endoscopic resection of an infraclavicular BP schwannoma.[43]
Endoscopic proximal humeral plate removal
Implant removal after proximal humerus fracture fixation can be performed endoscopically and may be combined with arthrolysis.[44,45] These techniques involve endoscopic dissection in the subdeltoid and upper arm region and have several advantages over conventional open removal of implants [Figure 5].

- Endoscopic proximal humeral plate removal is shown. Careful dissection is performed in the subdeltoid and upper arm region and the axillary nerve (arrow, left image) is identified and protected. The plate is dissected off (arrows, right image) from the humeral head (h) and retrieved through a “plate portal” in the upper arm.
Scapulothoracic endoscopy
Scapulothoracic endoscopy and scapuloplasty can be performed using a new two-portal technique that uses intraoperative landmarks for accurate orientation.[46] Arthroscopic management of snapping scapula syndrome yields improvement in pain, crepitus, and range of motion in a majority of patients; however, most patients experience residual symptoms. Lower pre-operative mental status score, longer duration of symptoms, and greater age were associated with poorer outcomes [Figure 6].[47,48]

- Scapulothoracic endoscopy is shown. Scapuloplasty and resection of the Luschka’s tubercle (TL) are demonstrated. Inset image shows the portals and position for the procedure.
Tendon transfers
Endoscopic harvest and transfer of tendons (latissimus dorsi, teres major, and pectoralis minor) have been described by several authors and are a minimally invasive alternative to open surgery.[49-51]
Office-based needle arthroscopy
In-office needle arthroscopy is a new minimally invasive diagnostic procedure that allows the patient to actively participate in the diagnostic process and avoids the need for advanced imaging.[52] The technology has evolved for use during surgery and single-portal rotator cuff and labral repairs have been described.[53,54]
FUTURE TRENDS
Arthroscopic procedures and techniques are evolving at a rapid pace and current evidence suggests a future role for joint preservation and restoration procedures. Arthroscopic techniques like remplissage are safe and durable and likely to be commonly used to address larger Hill-Sachs lesions with minimal glenoid bone loss.[55] Arthroscopic bone grafting has shown technical and outcome advantages; however, the technique is limited by a steep learning curve and complications rates remain unaffected by surgical experience.[56] Bioinductive scaffolds have the potential to enhance healing rates of repaired tendons, and further clinical evaluation to assess their utility is necessary. SCR appears to be a solution to avoid prosthetic replacement in irreparable rotator cuff tears; however, graft thickness is crucial to achieve the desired results of the original procedure.[57] Mobilization and repair of potentially irreparable rotator cuff tears in combination with biceps autograft for augmentation is an attractive and cost-effective option, and the combination has the advantage of preserving the cuff and superior capsule.[58,59] Finally, joint preservation procedures for GHOA have stood the test of time and are likely to be adopted and evaluated further.[60]
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
The author certifies that he has no commercial associations (e.g., consultancies, stock ownership, and equity interest) that might pose a conflict of interest in connection with the submitted article. The senior author (DN Bhatia) retains the copyright to the images, videos, and content in this chapter.
References
- Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging hill-Sachs lesion. Arthroscopy. 2000;16:677-94.
- [CrossRef] [PubMed] [Google Scholar]
- Management of anterior shoulder instability without bone loss: Arthroscopic and mini-open techniques. Shoulder Elbow. 2011;3:1-7.
- [CrossRef] [Google Scholar]
- Redefining “critical” bone loss in shoulder instability: Functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43:1719-25.
- [CrossRef] [PubMed] [Google Scholar]
- Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic bankart repair. Am J Sports Med. 2017;45:1975-81.
- [CrossRef] [PubMed] [Google Scholar]
- What is the critical value of glenoid bone loss at which soft tissue bankart repair does not restore glenohumeral translation, restricts range of motion, and leads to abnormal humeral head position? Am J Sports Med. 2016;44:2784-91.
- [CrossRef] [PubMed] [Google Scholar]
- Bone defect-induced alteration in glenoid articular surface geometry and restoration with coracoid transfer procedures: A cadaveric study. J Shoulder Elbow Surg. 2019;28:2418-26.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of defect orientation and size on glenohumeral instability: A biomechanical analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24:533-9.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral-track and central-track hill-Sachs lesions: A new concept of assessing an on-track lesion. Am J Sports Med. 2020;48:33-8.
- [CrossRef] [PubMed] [Google Scholar]
- Glenoid track instability management score: Radiographic modification of the instability severity index score. Arthroscopy. 2020;36:56-67.
- [CrossRef] [PubMed] [Google Scholar]
- Bone Defects in Anterior Shoulder Instability: New Techniques and Cadaveric Insights to Optimize the Algorithm. In: Presented at Shoulder and Elbow Society of Australia (SESA) Biennial Conference. Perth, Australia, 2018.
- [Google Scholar]
- Predicting failure after primary arthroscopic bankart repair: Analysis of a statistical model using anatomic risk factors. Arthroscopy. 2020;36:964-70.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrence rate of instability after remplissage for treatment of traumatic anterior shoulder instability: A systematic review in treatment of subcritical glenoid bone loss. Arthroscopy. 2018;34:2894-907.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of remplissage on global shoulder outcome: A long-term comparative study. Arthroscopy. 2019;35:1362-7.
- [CrossRef] [PubMed] [Google Scholar]
- Factors related to patient dissatisfaction versus objective failure after arthroscopic shoulder stabilization for instability. J Bone Joint Surg Am. 2019;101:1070-6.
- [CrossRef] [PubMed] [Google Scholar]
- Double-Barrel remplissage: An arthroscopic all-intra-articular technique using the double-barrel knot for anterior shoulder instability. Arthrosc Tech. 2015;4:e65-70.
- [CrossRef] [PubMed] [Google Scholar]
- The “double-barrel” knot: A new sliding knot for arthroscopic soft tissue fixation using single-pulley and double-pulley techniques. Tech Hand Up Extrem Surg. 2013;17:128-33.
- [CrossRef] [PubMed] [Google Scholar]
- The tripod-pulley technique for arthroscopic remplissage in engaging hill-Sachs lesions. Arthrosc Tech. 2017;6:e1675-84.
- [CrossRef] [PubMed] [Google Scholar]
- Neer award 2019: Latarjet procedure vs. Iliac crest bone graft transfer for treatment of anterior shoulder instability with glenoid bone loss: A prospective randomized trial. J Shoulder Elbow Surg. 2019;28:1298-307.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoarticular distal clavicle autograft for the management of instability-related glenoid bone loss: An anatomic and cadaveric study. J Shoulder Elbow Surg 2020:S1058-2746.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical comparison of screw fixation versus a cortical button and self-tensioning suture for the latarjet procedure. Orthop J Sports Med. 2018;6:2325967118777842.
- [CrossRef] [PubMed] [Google Scholar]
- Cortical suture button fixation vs. Bicortical screw fixation in the latarjet procedure: A biomechanical comparison. J Shoulder Elbow Surg 2020:S1058-2746.
- [CrossRef] [PubMed] [Google Scholar]
- Latarjet with cortical button fixation is associated with an increase of the risk of recurrent dislocation compared to screw fixation. Knee Surg Sports Traumatol Arthrosc. ;2019
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic iliac crest bone grafting in recurrent anterior shoulder instability: Minimum 5-year clinical and radiologic follow-up. Knee Surg Sports Traumatol Arthrosc. ;2020
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic, implant-free bone-grafting for shoulder instability with glenoid bone loss. JBJS Essent Surg Tech. 2020;10:e0109.1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic congruent-arc shoulder bone-block for severe glenoid bone defect: Preliminary report. Orthop Traumatol Surg Res. 2017;103:441-6.
- [CrossRef] [PubMed] [Google Scholar]
- Learning curves in the arthroscopic latarjet procedure: A multicenter analysis of the first 25 cases of 5 international surgeons. Arthroscopy. 2019;35:2304-11.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of biologic scaffolds for augmentation of partial rotator cuff tears in a canine model. J Shoulder Elbow Surg 2020:S1058-2746.
- [CrossRef] [Google Scholar]
- Evaluation of healing rates and safety with a bioinductive collagen patch for large and massive rotator cuff tears: 2-year safety and clinical outcomes. Am J Sports Med. 2019;47:1901-8.
- [CrossRef] [PubMed] [Google Scholar]
- Radiologic and clinical evaluation of a bioabsorbable collagen implant to treat partial-thickness tears: A prospective multicenter study. J Shoulder Elbow Surg. 2018;27:242-51.
- [CrossRef] [PubMed] [Google Scholar]
- Massive, Retracted and Fatty Infiltrated Triple Tendon Rotator Cuff Tears: Arthroscopic Repair Techniques for “Irreparable” Tears.
- Superior capsular reconstruction with the long head of the biceps autograft prevents infraspinatus retear in massive posterosuperior retracted rotator cuff tears. Am J Sports Med. 2020;48:1430-8.
- [CrossRef] [PubMed] [Google Scholar]
- Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105:257-63.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic superior capsular reconstruction of the shoulder using dermal allograft. Orthopedics. 2020;2020:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fascia lata autograft versus human dermal allograft in arthroscopic superior capsular reconstruction for irreparable rotator cuff tears: A systematic review of clinical outcomes. Arthroscopy. 2020;36:579-91.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic joint preservation in severe glenohumeral arthritis using interpositional human dermal allograft. Arthroscopy. 2017;33:1920-5.
- [CrossRef] [Google Scholar]
- Arthroscopic debridement and biological resurfacing of the glenoid in glenohumeral arthritis. Knee Surg Sports Traumatol Arthrosc. 2010;18:1767-73.
- [CrossRef] [PubMed] [Google Scholar]
- Survivorship and patient-reported outcomes after comprehensive arthroscopic management of glenohumeral osteoarthritis: Minimum 5-year follow-up. Am J Sports Med. 2016;44:3206-13.
- [CrossRef] [PubMed] [Google Scholar]
- The beach chair position for shoulder surgery in intravenous general anesthesia and controlled hypotension: Impact on cerebral oxygenation, cerebral blood flow and neurobehavioral outcome. J Clin Anesth. 2019;53:40-8.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors associated with hypotensive bradycardic events during open shoulder surgery in the beach chair position. Korean J Anesthesiol. ;2020
- [CrossRef] [Google Scholar]
- The effect of the beach-chair position angle on cerebral oxygenation during shoulder surgery. J Shoulder Elbow Surg. 2017;26:1670-5.
- [CrossRef] [PubMed] [Google Scholar]
- Patient positioning in shoulder arthroscopy: Which is best? Joints. 2019;7:46-55.
- [CrossRef] [PubMed] [Google Scholar]
- All-endoscopic brachial plexus complete neurolysis for idiopathic neurogenic thoracic outlet syndrome: A prospective case series. Arthroscopy. 2017;33:1449-57.
- [CrossRef] [PubMed] [Google Scholar]
- All-endoscopic resection of an infraclavicular brachial plexus schwannoma: Surgical technique. Arthrosc Tech. 2018;7:e869-73.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic removal of proximal humerus locking plates. Knee Surg Sports Traumatol Arthrosc. 2010;18:409-11.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic removal of proximal humerus plates in chronic post-traumatic shoulder stiffness. Arthrosc Tech. 2017;6:e375-81.
- [CrossRef] [PubMed] [Google Scholar]
- Scapulothoracic endoscopy for the painful snapping scapula: Endoscopic anatomy and scapuloplasty technique. Arthrosc Tech. 2015;4:e551-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of snapping scapula syndrome: Outcomes at minimum of 2 years. Arthroscopy. 2017;33:726-32.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of snapping scapula syndrome improves pain and functional outcomes, although a high rate of residual symptoms has been reported. Knee Surg Sports Traumatol Arthrosc. 2018;26:221-39.
- [CrossRef] [PubMed] [Google Scholar]
- Combined fully arthroscopic transfer of latissimus dorsi and teres major for treatment of irreparable posterosuperior rotator cuff tears. Arthrosc Tech. 2019;9:e147-57.
- [CrossRef] [PubMed] [Google Scholar]
- All-arthroscopic latissimus dorsi transfer. Arthrosc Tech. 2016;5:e607-13.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic-assisted pectoralis minor transfer for irreparable tears of the upper two-thirds of the subscapularis tendon: Surgical technique. Arthrosc Tech. 2017;6:e1501-5.
- [CrossRef] [PubMed] [Google Scholar]
- Office-based needle arthroscopy: A standardized diagnostic approach to the shoulder. Arthrosc Tech. 2020;9:e521-5.
- [CrossRef] [PubMed] [Google Scholar]
- Single-incision rotator cuff repair with a needle arthroscope. Arthrosc Tech. 2020;9:e419-23.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoscopic single-incision anterior labrum repair. Arthrosc Tech. 2020;9:e297-301.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: If you want your arthroscopic bankart repairs to be durable for 10 years consider treating the hill-Sachs lesion with remplissage. Arthroscopy. 2019;35:1368-9.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: Arthroscopic latarjet: Is it ready for prime time? Arthroscopy. 2019;35:1062-3.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: Shoulder superior capsular reconstruction: When a systematic review of a procedure can be misleading. Arthroscopy. 2019;35:1278-9.
- [CrossRef] [PubMed] [Google Scholar]
- Massive Rotator Cuff Repair with Biceps Augmentation using TwinFix TM, Webinar. 2019. Available from: https://www.smith-nephew.com/education/resources/video/2019/arthroscopy/massive-rotator-cuff-repair-with-biceps-augmentation-using-twinfix [Last accessed on 2020 May 17]
- [Google Scholar]
- The rotator cuff and the superior capsule: Why we need both. Arthroscopy. 2016;32:2628-37.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: Is shoulder joint preservation an endangered species? Let's save the glenoid. Arthroscopy. 2017;33:1926-7.
- [CrossRef] [PubMed] [Google Scholar]






