Translate this page into:
Recent advances and future trends in foot and ankle arthroscopy

*Corresponding author: Venu Kavarthapu, Department of Trauma and Orthopaedics, Kings College Hospital, Denmark Hill, London, United Kingdom. drvenu@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Osarumwense D, Kavarthapu V. Recent advances and future trends in foot and ankle arthroscopy. J Arthrosc Surg Sport Med 2020;1(1):133-40.
Abstract
Foot and ankle arthroscopy (AA) has evolved slowly since its first descriptions over 40 years ago but today stands as a reliable and well-established part of the foot and ankle surgeons’ armamentarium. Modern technological advances in instrumentation, imaging, and biological reconstructive materials have helped push the boundaries of what is doable with this treatment modality. This article explores the origins and applications of foot and AA. It also takes a look at what is coming ahead in this exciting sphere of foot and ankle surgery.
Keywords
Ankle
Foot
Arthroscopy
History
Trends
INTRODUCTION
Ankle arthroscopy (AA) is now a well-established alternative in the treatment armamentarium of the foot and ankle surgeon. In addition to being a diagnostic tool, it gives the surgeon therapeutic applications in the same sitting using a minimally invasive technique. Its evolution, however, was slow to reach present acceptance and reliability since the early systematic descriptions of this procedure in 1939[1] using a 2.7 mm diameter arthroscope. Masaki Watanabe is regarded as a pioneer and “father of arthroscopy” with considerable success in knee arthroscopy.[2] In 1972, he published the first series of 28 AA patients using a newly developed self-focusing small joint 1.7 mm arthroscope.[3] From his series of 67 cadaveric arthroscopies, Chen, in 1976, further described the surgical technique and arthroscopic anatomy of the ankle joint.[4] The inadequacy of instrumentation and surgical techniques to overcome the difficulties related to suboptimal visualization and poor access to the relevant damaged structures within such a constrained joint contributed to the slow uptake and popularity of AA. It also limited the indications for its early use to just diagnosis and treatment of loose bodies, soft tissue, or bony impingements, with reports of varying success.[5-8] A 21-point systematic examination of the ankle joint was also developed to help with achieving a reproducible diagnostic examination of the ankle joint.[7] These early arthroscopic procedures were performed through the anterior approach as adequate visualization and access to the central and more posterior aspects of the ankle joint were problematic.[9,10] To improve the situation, a new invasive and fixed distraction device was introduced in the 1980s, using pins in the tibia and calcaneus.[11] However, to avoid any added morbidity from the skeletal pin sites, a non-invasive distraction technique was also developed.[12] Development and refinement of a separate posterior approach[13] opened up the possibilities of accessing posterior ankle and subtalar joints pathologies. These improvements in instrumentation, joint access and visualisation made arthroscopic intervention possible for more pathologies, including for tendons around the ankle joint and smaller joints of the foot.[14-17]
At the turn of the century, the indications for foot and AA were well established. These ranged from intra-articular loose bodies, osteochondral injuries,[18] impingements, arthritis, tendinopathies, and various other sports pathologies around the ankle joints [Figure 1].[15,19-21]
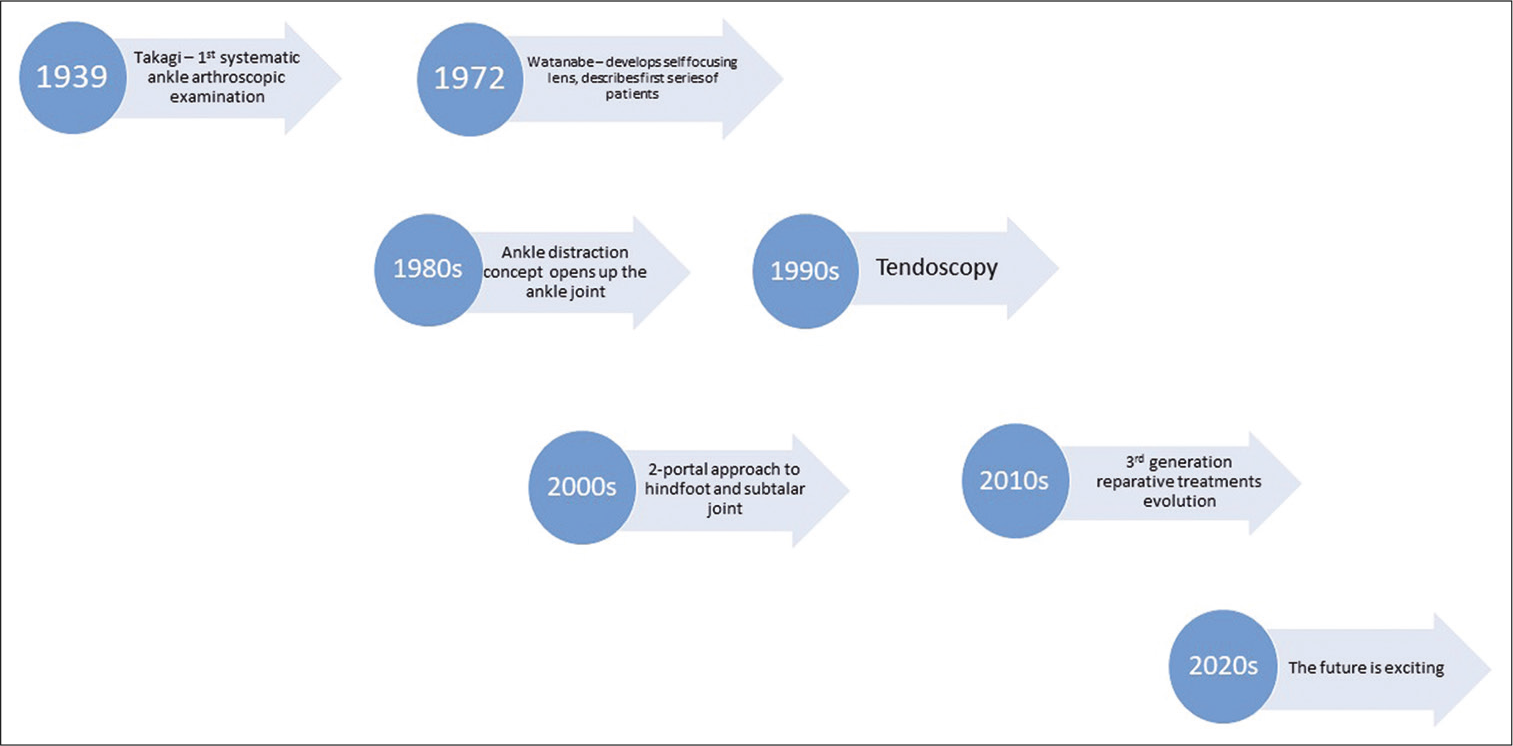
- Illustrative historical developments in foot and ankle arthroscopy.
The aim of this article is to give readers an update on the spectrum of foot and AA procedures currently being performed and highlight the upcoming developments.
AA – HOW IS IT PERFORMED?
The method of AA is largely dictated by the pathology that needs to be addressed. It is usually performed under general anesthesia and as an outpatient procedure. This can be supplemented with a regional block at surgeons or anesthetist discretion. Anteriorly placed portals with the patient in supine position are used for most anterior and centrally located pathology, whereas the posterior approach with patient prone to hind foot and subtalar problems. A lateral decubitus position has also been described that allows for the placement of both anterior and posterior portals with rotation of the same side hip as needed.[22] A thorough knowledge of the foot and ankle anatomy is essential to guide safe and accurate placement of both anterior and posterior arthroscopic portals and to understand the pathology being investigated.
SET UP
Patient positioning is dependent on the surgeons preferred approach and the work to be done. Hence, patient can be supine or prone as desired. A tourniquet is usually applied above the knee and this can be placed in a thigh holder to help fix the limb and flex the hip joint. Alternatively, a bolster can be placed underneath knee to achieve 20–45° of knee flexion, along with a side support placed at thigh region to reduce hip external rotation.
To distract or not
Distraction of the ankle joint has been popular due to its perceived advantage of increasing visualization and protection of the ankle joint surface from iatrogenic damage. A non-invasive ankle distraction strap can be applied and attached to a sterile rope run over a pulley with weights attached to its end to achieve adequate distraction. More popular option is to attach the ankle strap to a sterile ankle distractor devise that is attached to the operating table. Some surgeons prefer the ankle distraction strap attached to a sterile rope and tied around the waist of the performing surgeon who applies the traction dynamically. Excessive distraction, particularly with the ankle in plantar flexion, can lead to tightening of the anterior ankle joint capsule and thus reduce the working area. This can limit access to the anterior and posterior ankle pathologies. It is critical that the ankle joint is kept in neutral flexion position, particularly during anterior ankle compartment access and procedure. However, some studies have shown that distraction may not be necessary to perform anterior AA.[23] In a cadaveric study, De Leeuw et al. showed that a significantly increased and safe anterior working area can be created with the foot in dorsiflexion during AA.[24] However, if applied, distraction force should only be used for up to 60 min at a time, to reduce any risk of traction damage to the peripheral nerves in the foot and ankle.
INSTRUMENTATION
The instruments used in AA are similar to larger joints but on a smaller scale. Different length arthroscopes are available, with the shorter length allowing for a decreased lever arm effect. These arthroscopes usually have 30° or 70° viewing angle and come with 4 mm, 3.5 mm, or 2.7 mm diameter, the larger diameters can deliver more irrigation fluid and thus obviate the need for additional portals for this function. Even smaller 2.0 mm diameter arthroscopes have been developed for the smaller joints of the foot. A whole range of appropriately sized additional accessories including graspers, osteotomes, shavers, burrs, curettes, knives, punches, radiofrequency probes, and suction equipment is also available.
PORTAL PLACEMENT
There are three main portals considered as the workhorses of AA, the anterolateral, anteromedial, and posterolateral portals. Additional portals and entry points can be used as needed depending on the pathology being addressed. To help with accurate portal placement, the surgeon should use an indelible marker pen to mark out the position of important structures and landmarks around the ankle joint prior to inflating the tourniquet. These include the anterior dorsalis pedis artery, deep peroneal nerve, tibialis anterior tendon, great saphenous vein, peroneus tertius tendon, malleoli, and the joint line [Figure 2]. Because of their closeness to the anterolateral portal, it is critical that the superficial peroneal nerve and its branches are identified and marked. Its position is made more prominent by inversion with plantar flexion of the foot and passive flexion of the toes. A nick in the skin marks the portal entry point and a blunt trocar or mosquito forceps are used to spread the subcutaneous tissue and gain access into the distended joint.
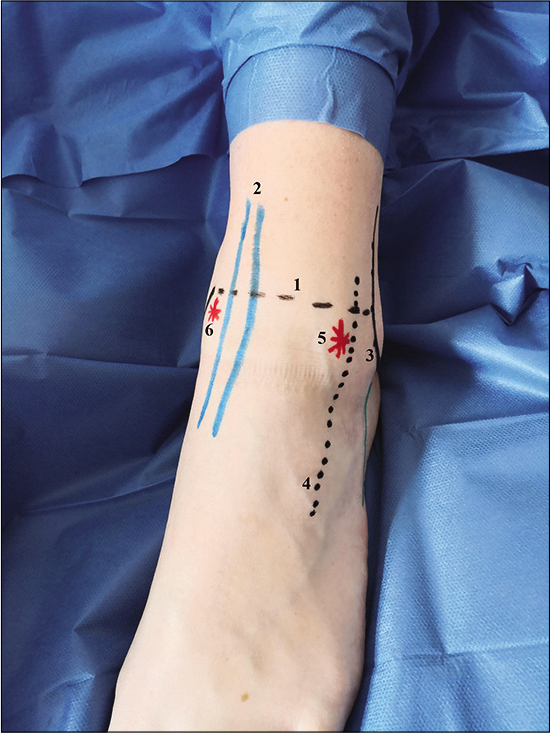
- Anterior ankle portals with landmarks. 1 = Ankle joint line, 2 = tibialis anterior tendon, 3 = lateral malleolus, 4 = superficial peroneal nerve, 5= anterolateral portal, 6= anteromedial portal.
Anteromedial portal
This is the first portal to be established and is positioned just medial to the tibialis anterior tendon at the level of the joint line. At this point, the ankle joint is distended with 20 ml of normal saline injected through the marked entry portal. This allows safe placement of the portal without damaging the articular cartilage. A nick in the skin marks the portal entry point and a mosquito forceps are used to spread the subcutaneous tissue and gain access into the distended joint. The 2.7 mm arthroscope trocar and cannula are inserted into the portal and then the trocar is replaced with a 2.7 mm 30° arthroscope. The anteromedial portal is usually regarded as the vision portal for most arthroscopic work in this joint.
Anterolateral portal
This portal is established under direct vision with visualization of a 25G needle. Point of insertion is usually lateral to the peroneus tertius tendon at the level of the joint line. It is regarded as the work portal for most of the instrumentation and its location can be varied according to the position of the lesion being treated. Care must be taken to avoid nearby neurovascular structures, especially the superficial peroneal nerve and its branches.
Posterolateral portal
The patient can be prone or in the semi-decubitus position. First of two posterior portals, posterolateral portal’s position can be marked just lateral to the Achilles tendon at a level of a line parallel with the sole and drawn from the tip of the lateral malleolus to meet the Achilles tendon [Figure 3]. A nick in the skin and mosquito forceps is used to spread the soft tissue and access the joint. It can also be made under direct vision after the arthroscope from the anteromedial portal is place in the posterior part of the joint, through the notch of Harty, to visualize tip of needle inserted just lateral to the Achilles tendon as described above. Once access is gained, a 4.0 mm 30° arthroscope is inserted. In the hind foot arthroscopy, this is regarded as the vision portal.
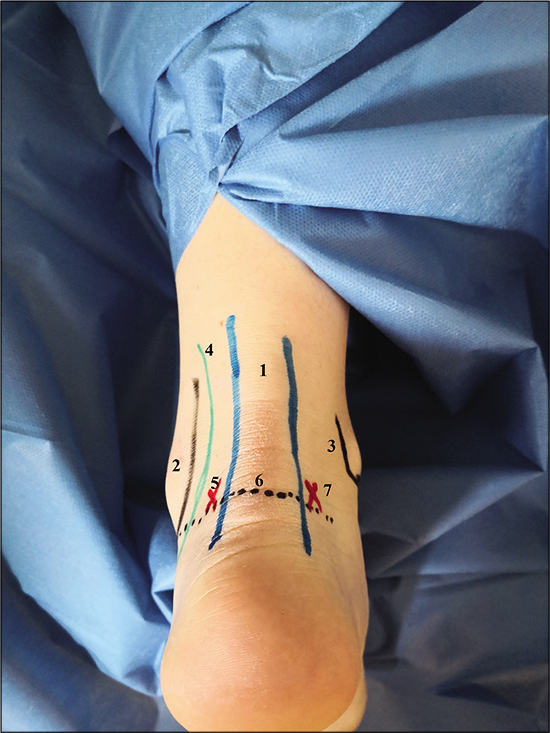
- Posterior portals and landmarks. 1 = Achilles tendon, 2 = lateral malleolus, 3 = medial malleolus, 4 = peroneal tendons, 5 = posterolateral portal, 6 = line from tip of lateral malleolus, 7 = posteromedial malleolus.
Posteromedial portal
This is made at the same level as the posterolateral portal on the medial aspect of the Achilles tendon [Figure 4]. A nick in the skin and mosquito forceps is used to spread the soft tissue and access the joint till the tip of the forceps is visualized through the posterolateral arthroscope. The forceps are then replaced with a shaver under direct vision. The shaver is used to remove the fatty tissue and joint capsule to expose the posterior aspect of the ankle and subtalar joint. Identification of the flexor hallucis longus (FHL) tendon by moving the first metatarsophalangeal joint is the first step before commencing the actual arthroscopic examination. The posterior tibia nerve and artery are at risk with this portal. This posteromedial portal is regarded as the work portal in this approach.
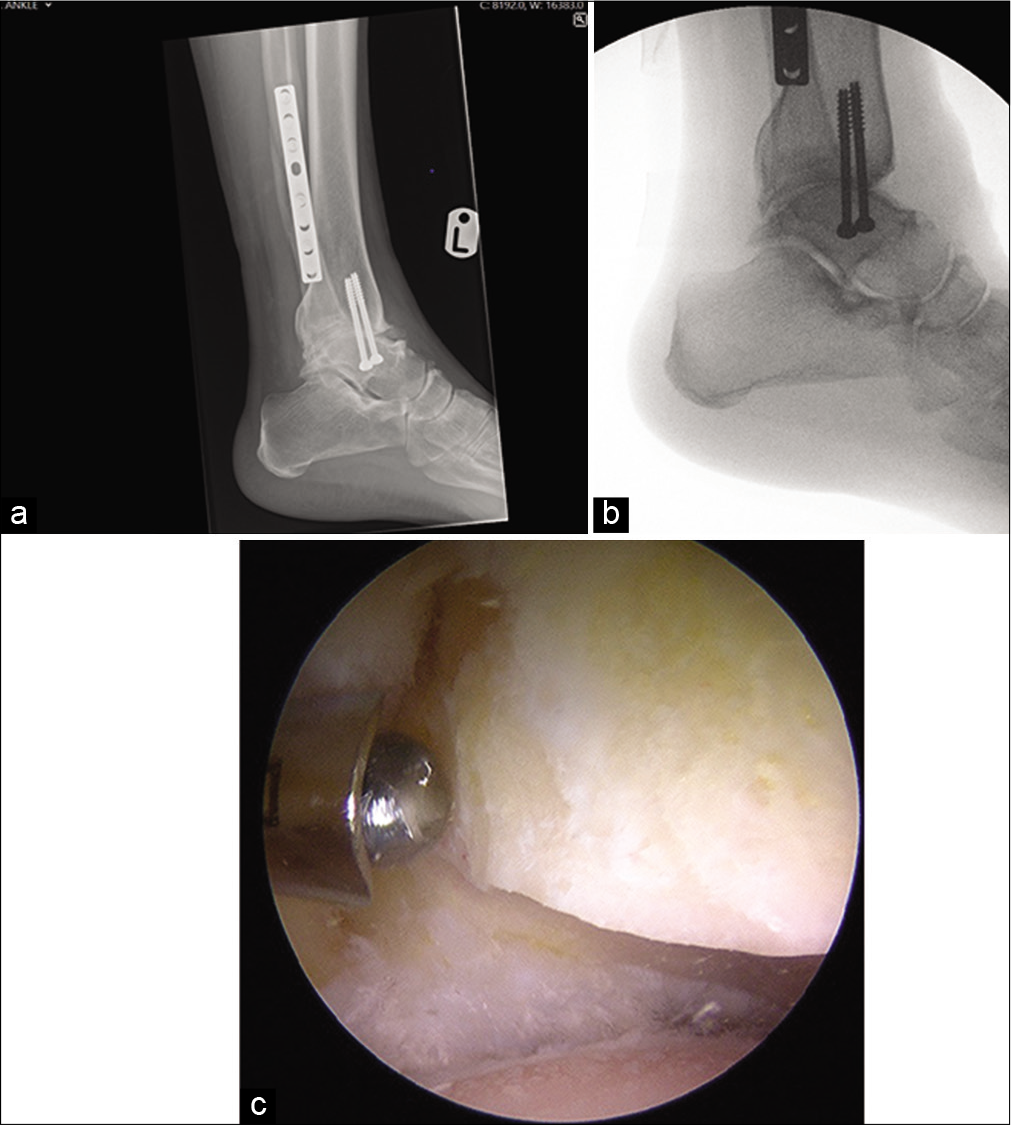
- (a) Weight-bearing lateral view radiograph of left (L) ankle showing post traumatic bony spurs at anterior lip of distal tibia and dorsal aspect of neck of talus causing anterior ankle impingement. (b) Intraoperative fluoroscopy picture following resection of anterior ankle spurs demonstrating adequate excision. (c) Intraoperative arthroscopy view of ankle joint from lateral portal demonstrating adequate excision of distal tibial anterior bone spur using a burr.
Others
The posterocentral portal through the Achilles tendon is seldom used due to the potential morbidity associated with this tendon. The transmalleolar portal is an accessory portal used during the treatment of osteochondral lesions of the talus. K-wires can be passed through the medial, lateral malleolus, and/or through a transtalar approach to drill these lesions.
ANTERIOR ANKLE PATHOLOGY
Indications for anterior AA range include synovitis, anterior ankle impingement syndromes, osteochondral lesions of talus (OLT) ligamentous injury repair, ankle arthritis, and certain ankle fractures.
Anterior ankle impingement
This presents as pain in anterior aspect of the ankle and associated with decreased range of movement in dorsiflexion. Impingement can be soft tissue or bony in nature with multifactorial etiology, including recurrent blunt trauma or chronic joint instability.[25] Bony traction spurs from plantar flexion movements of the ankle joint form along the rim of the distal tibia, just distal to the attachment of the anterior capsuloligamentous structures of the ankle joint [Figure 4a-c]. Bony spurs also form along the anterior neck of the talus from recurrent forced dorsiflexion movement and along the medial aspect of the joint from chronic joint instability.[26] The bony spur formed along the anteromedial aspect of the neck of the talus, often seen in footballers, is referred to as anteromedial impingement. The anterior capsular attachments extend up to 8 mm proximal to distal anterior tibia rim, arthroscopic debridement is possible without violation of the capsule, even without distraction of the ankle joint.[10] Soft-tissue impingement is the most common cause of chronic ankle pain and has been attributed to impingement of hypertrophic damaged soft tissue within the anterolateral gutters resulting from inversion sprain injuries of the ankle joint.[7] The inferior fascicle of the anterior tibiofibular ligament has been identified as the main soft-tissue injured, causing hypertrophy and irritation of the talus dome.[27] Arthroscopic treatment usually commences after failure of conservative treatment and entails debridement of any pathological bony osteophytes or soft tissue where found. Studies have shown very good outcomes compared with open debridement with success rates of up to 70–95% in the literature.[28,29]
OLT
These are lesions caused by damage to the articular cartilage and also extending to the underlying bone with over 50% of these lesions occurring in the central parts of the talus. Patients often present with a history of ankle trauma, along with pain and swelling within the ankle joint. Localized and point tenderness in the OLT area is often difficult to elicit, particularly in the posteriorly placed lesions. Pre-operative CT imaging is beneficial to pinpoint the exact location of the lesion and direct the most appropriate surgical approach to be used. MRI imaging is also helpful in describing the morphology of the lesion including the extent of associated hyaline cartilage damage. Raikin et al., in their descriptive MRI study on localization and morphology of OLT, established a nine-grid scheme of the talar dome. In their study of 424 patients, they found that 53% of lesions occurred in the centromedial aspect of the talus and 26% in the centrolateral aspect of the talus.[30]
Treatment of OLT is dependent on several factors including severity of symptoms, age, and size of lesions. Conservative treatment has been advocated for children and adolescents[31] with good results; however, this is less successful in adults.[18] Arthroscopic debridement and microfracture are now considered the first-line surgical treatment for symptomatic OLT. Good success rates for this treatment have been reported with one study of 50 patients showing maintenance of initial success from this surgical treatment with a median American Orthopaedic Foot and Ankle Society (AOFAS) score of 88 out of scale of 100 after a mean follow-up of 144 months.[32] However, the size of the lesions has been shown to effect outcome of treatment. Studies have suggested lesions >15 mm in diameter carry higher risk of failure.[33] For such lesions, the alternative options to microfracture include osteochondral autograft transplantation[34] or matrix-induced autologous chondrocytes implantation.[35]
Ankle instability
Lateral ankle instability is due to the incompetence of anterior talofibular ligament (ATFL) and the calcaneofibular ligament usually caused by recurrent inversion injuries. Open Brostrom-Gould anatomical ligament repair/reconstruction has been the traditional treatment, but arthroscopic repair has now developed and become a reliable alternative with good results. Vega et al. described an all inside arthroscopic lateral collateral ankle ligament repair in 16 patients with ankle instability.[36] The procedure included repair of the ATFL and/or the calcaneofibular ligament with patients showing increased AOFAS score from 67 to 97 at final follow-up. Further reconstructive procedures using autograft or allograft have been developed, especially when there is insufficient residual ligament tissue for repair.[37,38] Matsui et al. showed equivalent clinical results when comparing arthroscopic with open repair for ankle instability after 1 year follow-up.[39]
POSTERIOR ANKLE AND HIND FOOT PATHOLOGY
Indications for posterior hind foot arthroscopy include loose bodies, posterior ankle impingement, FHL, and Achilles tendon problems, OLT, subtalar conditions, and Haglund’s deformity. The procedure is usually performed with the patient prone and on an outpatient basis. Two portal arthroscopic approaches are now well established and excision of small amount of fat and some of the posterior joint capsule will in addition give access to the subtalar joint.
Posterior ankle impingement
This presents with pain in the posterior aspect of the ankle from hyperplantar flexion of the foot. This can lead to the displacement of an os trigonum, hypertrophied posterior talar process causing impingement, and/or FHL synovitis. CT and MRI scans are used to evaluate the type of causative lesion. Following failed conservative treatment, arthroscopic debridement of any of these causative lesions is performed. Several studies have reported good results from arthroscopic debridement with less complications and quicker return to full activities compared to open surgical debridement for posterior ankle impingement.[40,41]
Subtalar joint
The two portal posterior approaches with patient in the prone position have enabled the emergence of arthroscopic subtalar joint arthrodesis and excision of talocalcaneal coalition procedures. Studies have shown very good outcomes for arthroscopic subtalar arthrodesis with fusion rates of up to 100% reported in the literature.[42] Subtalar arthroscopic talocalcaneal coalition resection has also showed good results. One review paper analyzing studies on posterior ankle and hindfoot arthroscopic procedures reported an improvement of pre-operative AOFAS scores by 40 points to up to 90 points postoperatively and fusion rates of up to 86%.[43]
Tendoscopies
The term tendoscopy was coined by van Dijk et al. in his paper on endoscopic examination of the peroneal and Achilles tendon sheaths.[15] Since then, tendoscopic procedures have been described for most tendons around the ankle joint. Most of the studies in the literature have shown good outcomes but are of Level IV and V evidence. Still, because of its safety and reliability, some of these procedures have now become an important part of the foot and ankle surgeon’s management options either as the sole treatment or as an adjunct for tendinopathy problems.[44] The most common indications for tendoscopic procedures described are the non-insertional Achilles tendinopathy, peroneal tendon tears and tenosynovitis, and posterior tibialis tenosynovitis Stages I and II.[45]
ANKLE FRACTURE FIXATION
The high incidence of chondral lesions and other intra- articular abnormalities present following ankle fractures and other traumatic injuries is well known with a rate of almost 80% in a study of 288 patients.[46] Arthroscopy allows for clear visualization and assessment of these and any associated syndesmotic and ligamentous injuries.[47,48] There is also the potential for their concurrent treatment during internal fixation of ankle and talar fractures as the arthroscopy allows assessment of fracture reduction and articular congruity, in particular, the triplane injuries in children. Talar dome osteochondral fractures benefit from arthroscopy-assisted reduction of the fracture fragment and fixation under direct arthroscopic vision. Posterior dome osteochondral fractures are challenging to access using standard arthroscopy portals and attempts were made successfully using a transmalleolar approach through which the fracture fragment fixation screw was passed under arthroscopic view and the fragment fixed.[49] A study comparing open fracture fixation with arthroscopy assisted fixation showed superior AOFAS scores in the arthroscopy assisted group after a 40-month follow-up period.[50]
ANKLE ARTHRITIS AND ARTHODESIS
Arthroscopic ankle arthrodesis is usually performed with patient supine through the traditional anterior portals. Occasional use of an additional posterolateral portal to get better access to the posterior cartilage and lateral gutters can be used. Studies have shown an equivalent or better results including fusion rates, length of stay, and functional outcomes, when compared to an open procedure both in the short and long term.[51,52] It has also been used to correct and achieve ankle fusion in the presence of greater than 15° planar deformity that has traditionally been used as a cutoff to proceed to open arthrodesis [Figure 5].[52]
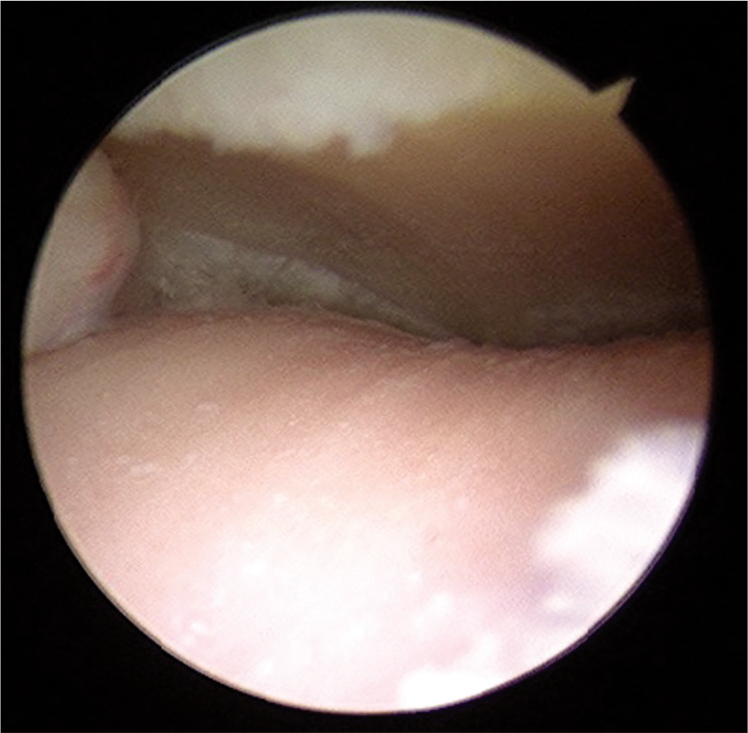
- Intraoperative arthroscopy view of ankle joint from the medial portal demonstrating complete chondral loss along with eburnation of talar dome.
HALLUX ARTHROSCOPY
Improvements in instrumentation have led to increasing interest in arthroscopic evaluation and treatment of disorders of the big toe. Indications for hallux arthroscopy include for hallux rigidus, hallux valgus deformity, loose bodies, and osteochondritis dissecans. In his case report from 1988, Bartlett described his technique of arthroscopic debridement treatment for osteochondritis dissecans of the first metatarsal head.[16] Since then, further arthroscopic techniques have been described for hallux deformities including for lateral soft-tissue release, arthrodesis, and focal osteochondral lesions of the first metatarsophalangeal joint, all with good outcomes.[53-55]
THE FUTURE
The gradual evolution of foot and ankle arthroscopic techniques from simple diagnostic to the current third- generation procedures has revolutionized foot and ankle diagnosis and treatment.[56] Our understanding of chronic ankle instability has also evolved with recognition of the contribution of medial ankle ligament damage, leading to refinement of our treatment strategies. This has led to the development of arthroscopic reconstructive procedures of the anterior tibiotalar ligament portion of the deltoid ligament.[57,58] As noted with other major joints, the development of modern orthobiologics and their delivery mechanisms has seen the emergence of a potential fourth generation of regenerative arthroscopic treatments for conditions such as OLT. Early results using techniques have shown at least similar outcomes compared to the more established microfracture treatments.[59,60] The concept of office arthroscopy is becoming more popular due to technological advancements in fine caliber foot and ankle instrumentation. Studies have described safe and reliable examination and treatment of common foot and ankle pathologies.[61,62]
Acknowledgment
Authors wish to acknowledge the assistance of Dr. Isobel Pilkington< Mr. Segun Akilapa and Mr. Raju Ahluwalia.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Venu Kavarthapu is on the Editorial Board of the Journal.
References
- Giants of orthopaedic surgery: Masaki Watanabe MD. Clin Orthop Relat Res. 2013;471:2443-8.
- [CrossRef] [PubMed] [Google Scholar]
- Selfoc-arthroscope (Watanabe No 24 Arthroscope). Monograph. Tokyo: Teishin Hospital; 1972.
- [Google Scholar]
- Clinical and cadaver studies on the ankle joint arthroscopy. J Jpn Orthop Assoc. 1976;50:631.
- [Google Scholar]
- Anterior ankle pain in sports medicine: Aetiology and indications for arthroscopy. Arch Orthop Trauma Surg. 1991;110:3-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic and operative arthroscopy of the ankle; technique and indications. Bull Hosp Jt Dis. 1985;45:38-47.
- [Google Scholar]
- New concepts (Distraction) in ankle arthroscopy. Arthroscopy. 1988;4:160-7.
- [CrossRef] [Google Scholar]
- A simple distraction technique for ankle arthroscopy. Arthroscopy. 1988;4:103-5.
- [CrossRef] [Google Scholar]
- A 2 portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871-6.
- [CrossRef] [PubMed] [Google Scholar]
- Tendoscopy (tendon sheath endoscopy) for overuse tendon injuries. Oper Tech Sports Med. 1997;5:170-8.
- [CrossRef] [Google Scholar]
- Arthroscopic management of osteochondritis dessicans of the first metatarsal head. Arthroscopy. 1988;4:51-4.
- [CrossRef] [Google Scholar]
- Arthroscopy of the ankle and foot. J Bone Joint Surg Am. 1993;75:1233-42.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003;8:233-42.
- [CrossRef] [Google Scholar]
- Anterior and posterior ankle impingement. Foot Ankle Clin. 2006;11:663-83.
- [CrossRef] [PubMed] [Google Scholar]
- Tendoscopy of the peroneal tendons. Foot Ankle Clin. 2006;11:415-20.
- [CrossRef] [PubMed] [Google Scholar]
- Operative arthroscopy of the ankle; three years' experience. Clin Orthop. 1985;199:46-53.
- [CrossRef] [Google Scholar]
- Fixed distraction is not necessary for anterior ankle arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2009;17:1399-400.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior ankle arthroscopy, distraction or dorsiflexion. Knee Surg Sports Traumatol Arthrosc. 2010;18:594-600.
- [CrossRef] [PubMed] [Google Scholar]
- Etiology of anterior ankle impingement syndrome: A descriptive anatomical study. Foot Ankle Int. 2004;25:382-6.
- [CrossRef] [PubMed] [Google Scholar]
- Ankle arthroscopic surgery. Sports Med Arthrosc Rev. 2018;26:190-5.
- [CrossRef] [PubMed] [Google Scholar]
- Minor or occult ankle instability as a cause of anterolateral pain after ankle sprain. Knee Surg Sports Traumatol Arthrosc. 2016;24:1116-23.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior tibiotalar spurs: A comparison of open versus arthroscopic debridement. Foot Ankle. 1992;13:125-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of anterolateral impingement of the ankle. J Foot Ankle Surg. 2010;49:219-23.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondral lesions of the Talus: Localisation and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int. 2007;28:154-61.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of osteochondral lesions in the ankle: A guideline from the group clinical tissue regeneration of the german society of orthopaedics and traumatology (DGOU) Z Orthop Unfall. 2017;155:92-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of osteochondral defects of the talus: Outcomes at eight to twenty years of follow up. J Bone Joint Surg Am. 2013;95:519-25.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of osteochondral lesions of the talus. Clin Podiatr Med Surg. 2016;33:521-30.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic autologous chondrocyte implantation in the ankle joint. Knee Surg Sports Traumatol Arthrosc. 2014;22:1311-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of deep articular talus lesions by matrix associated autologous chondrocyte implantation-results at five years. Int Orthop. 2012;36:2279-85.
- [CrossRef] [PubMed] [Google Scholar]
- All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot Ankle Int. 2013;34:1701-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic anatomical reconstruction of the lateral ankle ligaments. Knee Surg Sports Traumatol Arthrosc. 2016;24:998-1002.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle. Knee Surg Sports Traumatol Arthrosc. 2016;24:1003-6.
- [CrossRef] [PubMed] [Google Scholar]
- Early recovery after arthroscopic repair compared to open repair of the anterior talofibular ligament for lateral instability of the ankle. Arch Orthop Trauma Surg. 2016;136:93-100.
- [CrossRef] [PubMed] [Google Scholar]
- Hindfoot endoscopy for posterior ankle impingement syndrome and flexor halluces longus tendon disorders. Foot Ankle Clin. 2015;20:139-47.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic versus open excision of os trigonum for the treatment of posterior ankle impingement syndrome in an athletic population: A randomized controlled study with 5-year follow up. Am J Sports Med. 2017;45:1388-94.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior ankle and subtalar arthroscopy: Indications, technique and results. Curr Rev Musculoskelet Med. 2012;5:164-70.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of hindfoot and ankle pathologies with posterior arthroscopic techniques. EFORT Open Rev. 2017;2:230-40.
- [CrossRef] [PubMed] [Google Scholar]
- Foot and ankle tendoscopy: Evidence-based recommendations. Arthroscopy. 2014;30:755-65.
- [CrossRef] [PubMed] [Google Scholar]
- Foot and ankle tendoscopies: Current concepts review. EFORT Open Rev. 2016;1:440-7.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br. 2000;82:345-51.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: A systematic review of the literature. Arch Orthop Trauma Surg. 2009;129:227-35.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic diagnosis of tibiofibular syndesmosis disruption. Arthroscopy. 2001;17:836-43.
- [CrossRef] [PubMed] [Google Scholar]
- Transmalleolar approach for arthroscopy-assisted headless screw fixation of an osteochondral talar dome fracture. J Foot Ankle Surg. 2018;57:622-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of combined intraarticular disorders in the acute distal fibular fractures. J Trauma. 2004;57:1303-7.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic ankle arthrodesis: A 2-15 year follow up study. Arthroscopy. 2018;34:1641-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic ankle arthrodesis: A review of current concepts and technique. Tech Foot Ankle. 2020;19:19-25.
- [CrossRef] [Google Scholar]
- Arthroscopic arthrodesis of the first metatarsophalangeal joint in hallux valgus deformity. Arthrosc Tech. 2017;6:e1481-7.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic lateral soft tissue release for hallux valgus. J Foot Ankle Surg. 2020;59:210-2.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of focal osteochondral lesions of the first metatarsophalangeal joint. J Orthop Surg Res. 2017;12:95.
- [CrossRef] [Google Scholar]
- Ankle arthroscopy: No-distraction and dorsiflexion technique is the key for ankle arthroscopy evolution. Arthroscopy. 2018;34:1380-2.
- [CrossRef] [PubMed] [Google Scholar]
- The role of the medial ligaments in lateral stabilisation of the ankle joint: An in vitro study. Knee Surg Sports Traumatol Arthrosc. 2015;23:1900-6.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous matrix-induced chondrogenesis: A systematic review of the clinical evidence. Am J Sports Med. 2019;47:222-31.
- [CrossRef] [PubMed] [Google Scholar]
- Extracellular matrix allograft and particulate cartilage allograft for osteochondral lesions of the knee and ankle joints: A sytematic review. Am J Sports Med. 2018;46:1758-66.
- [CrossRef] [PubMed] [Google Scholar]
- Two-millimetre diameter operative arthroscopy of the ankle is safe and effective. Knee Surg Sports Traumatol Arthrosc. ;2020
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic reconstruction of the anterior tibiotalar ligament using a free tendon graft. Arthrosc Tech. 2020;9:e541-7.
- [CrossRef] [PubMed] [Google Scholar]






