Translate this page into:
Advances and future trends in elbow arthroscopy
*Corresponding author: Paul M. Robinson, Department of Trauma and Orthopaedics, Peterborough City Hospital, North West Anglia NHS Foundation Trust, Bretton Gate, Peterborough, PE3 9GZ, United Kingdom. paul.robinson1@nhs.net
-
Received: ,
Accepted: ,
How to cite this article: Robinson PM. Advances and future trends in elbow arthroscopy. J Arthrosc Surg Sport Med 2020;1(1):32-43.
Abstract
Elbow arthroscopy has evolved since its inception and is now a commonly used technique in the diagnosis and treatment of elbow pathology. It has many indications, from the removal of intra-articular loose bodies to the management of elbow osteoarthritis and fractures. In this paper, we will discuss the full spectrum of elbow arthroscopy covering recent evidence, surgical techniques, advances, and future trends.
Keywords
Elbow
Arthroscopy
Endoscopy
Fracture
Osteoarthritis
INTRODUCTION
Elbow arthroscopy has evolved since its inception and is now a commonly used technique in the diagnosis and treatment of elbow pathology. It has many indications, from the removal of intra- articular loose bodies to the management of elbow osteoarthritis and fractures. In this paper, we will discuss the full spectrum of elbow arthroscopy covering recent evidence, surgical techniques, advances, and future trends.
Established indications and procedures for elbow arthroscopy include debridement for septic arthritis, removal of loose bodies, management of osteoarthritis and inflammatory arthritis, radial head excision, contracture release, treatment of osteochondritis dissecans (OCD), and tennis elbow release.
Newer and evolving indications for elbow arthroscopy include those for acute elbow injuries, fracture management, and instability assessment and management (acute and chronic).[1,2] Less commonly, elbow arthroscopy can be used in arthroplasty cases for the assessment and biopsy of the symptomatic total elbow replacement (TER) and as an aid to visualization during cement removal in revision TER.
Endoscopic procedures around the elbow have also been described. These include the endoscopic management of distal biceps pathology, olecranon bursa debridement, and cubital tunnel release.
INVESTIGATION AND PRE-OPERATIVE PLANNING
Plain radiographs are of value in many cases, particularly in cases of elbow stiffness and in acute or chronic trauma cases. Standard anteroposterior and lateral views are obtained.
It is important to know about any previous surgery or pathology of the elbow that could distort the normal anatomy, particularly the anatomy of the neurovascular structures. The previous surgery to the ulnar nerve is particularly relevant. It is vital to know the position of the ulnar nerve and if it was previously transposed. If there is suspicion that the ulnar nerve has been transposed, elbow arthroscopy should not be attempted.
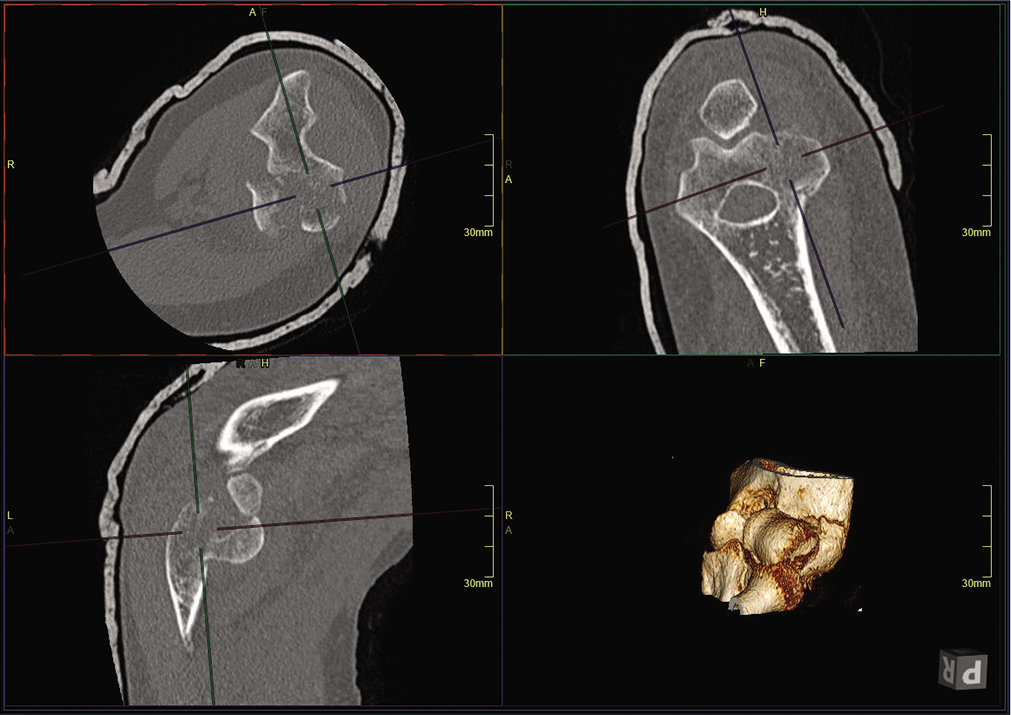
In cases of stiffness or where loose bodies are suspected, computed tomography (CT) scan or magnetic resonance imaging (MRI) scan is recommended for diagnostic purposes and to aid pre-operative planning. Both adequately visualize loose bodies and osteophytes. MRI is superior for imaging of non-osseous loose bodies, plica, ligaments, tendons, muscles, and the cartilage of the joint surfaces.
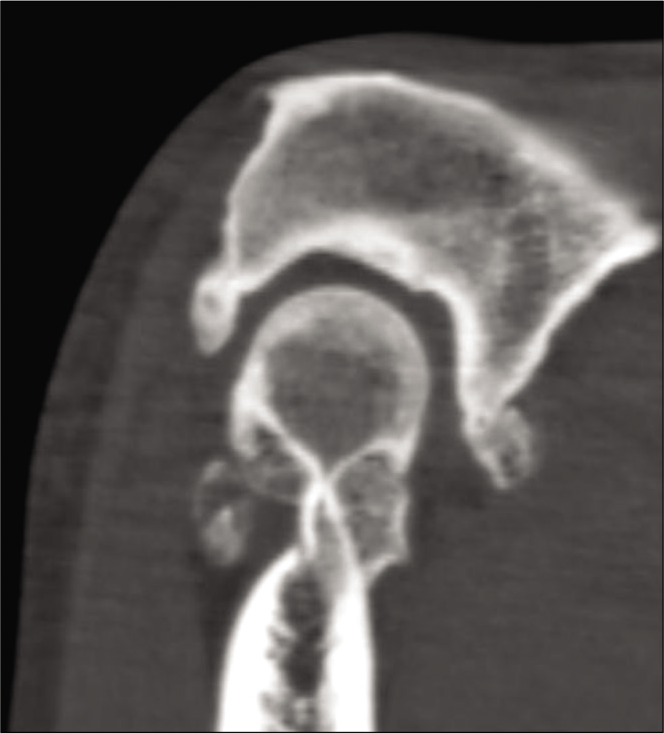
CT scanning with three-dimensional (3D) reformatting (axial, sagittal, and coronal planes) and volume-rendered 3D reconstructions is particularly helpful in trauma cases and before debridement for elbow stiffness [Figure 1]. More recently, imaging software has become available that allows the surgeon to reformat the CT images in the desired plane, allowing unparalleled understanding of the osseous anatomy [Figure 2].
- Computed tomography scan of an elbow with primary osteoarthritis. Osteophytes can be seen at the coronoid tip and olecranon tip. Osteophytes are also seen in the olecranon and coronoid fossae.
- Computed tomography scan of capitellum fracture with axial, coronal, and sagittal reconstructions (formatted by the operating surgeon in the desired planes) and volume rendered three-dimensional image.
The combination of CT scanning, 3D printing, and computer navigation has been tested and feasibly could help to improve the accuracy of bone removal during arthroscopic debridement for elbow OA.[3] Finite element analysis has also been used to analyze the most important areas of bone to remove to regain maximum elbow movement.
MRI scanning is excellent for identifying loose bodies, both osseous and non-osseous [Figure 3]. Loose bodies can have an attachment to the joint capsule and they may not be considered truly “loose;” however, these may still cause locking symptoms and pain if they become incarcerated between the joint surfaces. MRI is useful in this situation.
- Magnetic resonance imaging scan highlighting loose bodies in the anterior compartment of the elbow and osteophytes at the coronoid tip and olecranon tip.
PATIENT POSITIONING
The most common position is the lateral decubitus position. The patient can be supported with either individual hip supports at the pelvis or they can be positioned on a “bean bag” [Figure 4], which we find quicker than using individual supports. It is important to ensure adequate padding of pressure areas. A recent advance in practice is the use of an arm positioner. This is sterile draped into the surgical field and it can be moved intraoperatively by the surgeon, providing excellent access to the elbow [Figure 5]. Whatever arm support is used, it is important to ensure that there is enough clearance between the arm and the chest of the patient to enable unimpeded use of the arthroscope and instruments.

- Lateral positioning on bean bag.

- Mobile arm positioner, sterile draped into the surgical field.
EQUIPMENT
It is helpful to have both a large joint and small joint arthroscope available. A small joint arthroscope can be useful when working in the posterolateral compartment. A 30° and 70° large joint scope are used in most cases.[4] An end-vented cannula theoretically reduces fluid extravasation compared with a side-vented cannula.
ANESTHESIA
General and/or regional anesthesia can be used. Regional anesthesia is used in cases where good post-operative analgesia is required for early post-operative passive mobilization. This is particularly useful after elbow contracture release.
Another option for analgesia is to infiltrate the joint with local anesthesia at the beginning of the procedure. Ropivacaine at a concentration of 0.5% or lower has the lowest chondrotoxicity when compared with lidocaine, bupivacaine, levobupivacaine, and mepivacaine.[5] If regional or intra- articular analgesia is used, it is important to remember that the patient’s neurological examination immediately after the procedure may be abnormal.
PORTALS
When accessing the anterior compartment of the elbow, the more proximal medial and lateral portals are the safest in terms of avoiding nerve injuries (proximal anteromedial and proximal anterolateral portals). We would suggest that standardized portal nomenclature is used, as described in the paper by Camp et al.[6]
PROCEDURES
Debridement for septic arthritis
Septic arthritis of the elbow joint can occur in otherwise healthy patients without pre-existing elbow disease. Arthroscopic irrigation and synovectomy are safe and effective in patients with septic arthritis and result in good functional outcomes.[7]
SYNOVECTOMY
Rheumatoid arthritis
Synovectomy is an established procedure in the treatment of elbow RA.[8] It is efficacious in RA patients (Larsen Grade 3 or less), resulting in an increase in ROM, increased MEPS, and reduced VAS.[9] Other authors have described good results in RA up to Larsen Grade 4, showing that benefit can be felt in more arthritic elbows.[10]
Hemophilia
Arthroscopic synovectomy has been shown to be both clinically and cost effective in reducing recurrent elbow hemarthroses. These patients must be covered with replacement therapy during the perioperative period.[11] An MDT approach with the hematology team is essential.
OSTEOCAPSULAR ARTHROPLASTY
Indications
Primary osteoarthritis
There are specific indications for the arthroscopic treatment of elbow arthritis. Marginal osteophytes that are limiting elbow flexion and extension can be removed arthroscopically [Figures 6-10], [Videos 1-5], improving movement and preventing painful impingement at terminal extension and flexion. The ulnohumeral cartilage is often preserved in these patients and mid-arc pain is not commonly a problem. The anterior capsule can also be released to improve elbow extension.
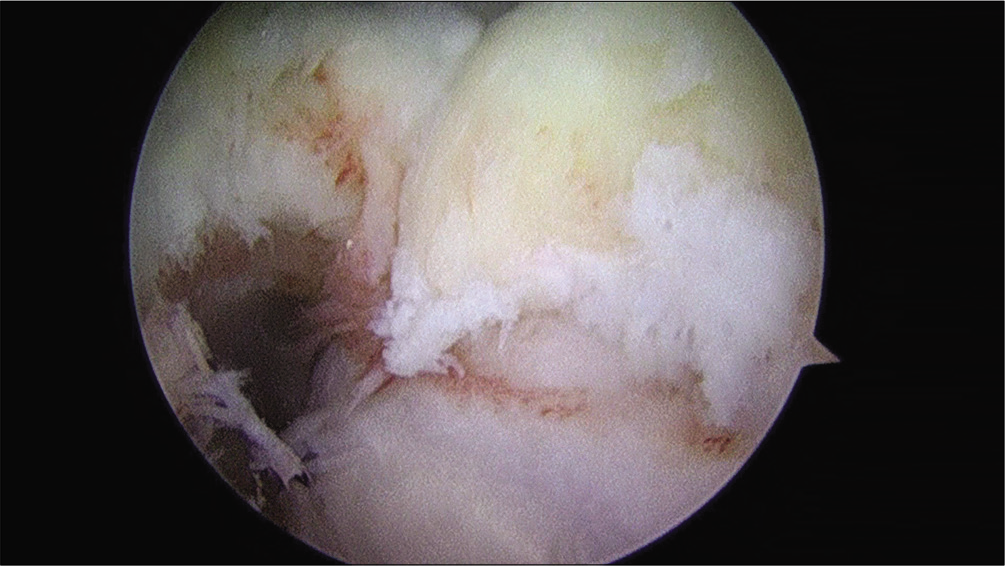
- Operative photograph. Anterior humeral bone spur and osteophyte in the coronoid fossa, viewed from proximal anterolateral portal.
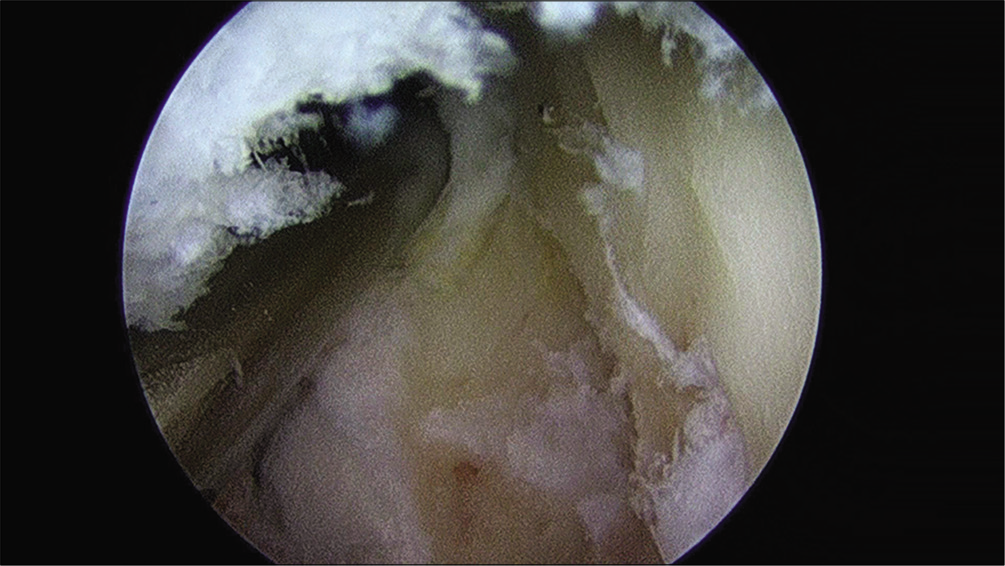
- Operative photograph. After removal of the anterior humeral bone spur and osteophyte from the coronoid fossa, viewed from proximal anterolateral portal.
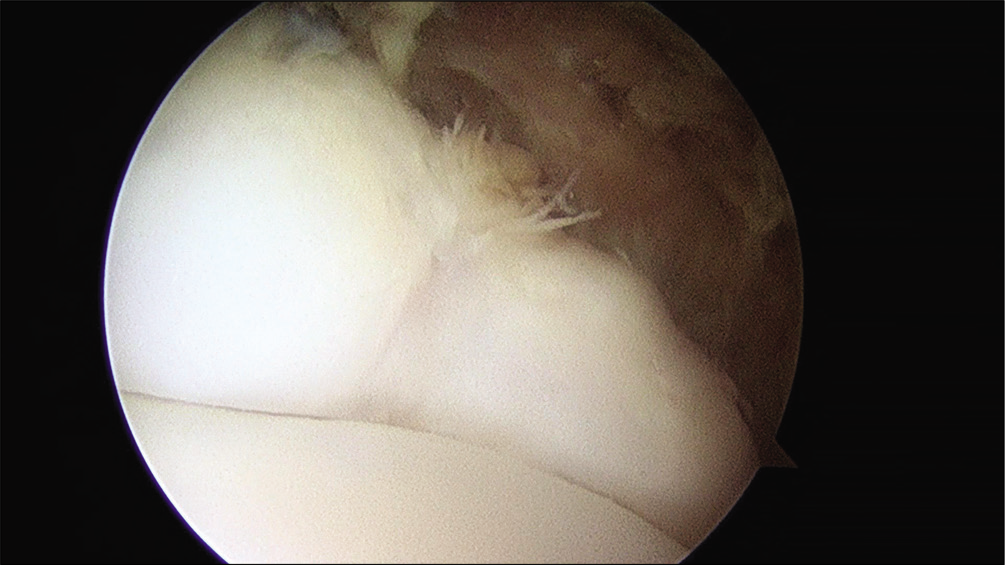
- Operative photograph. Coronoid osteophyte, viewed from proximal anteromedial portal.
- Operative photograph. Coronoid osteophyte removal with burr, viewed from proximal anterolateral portal.
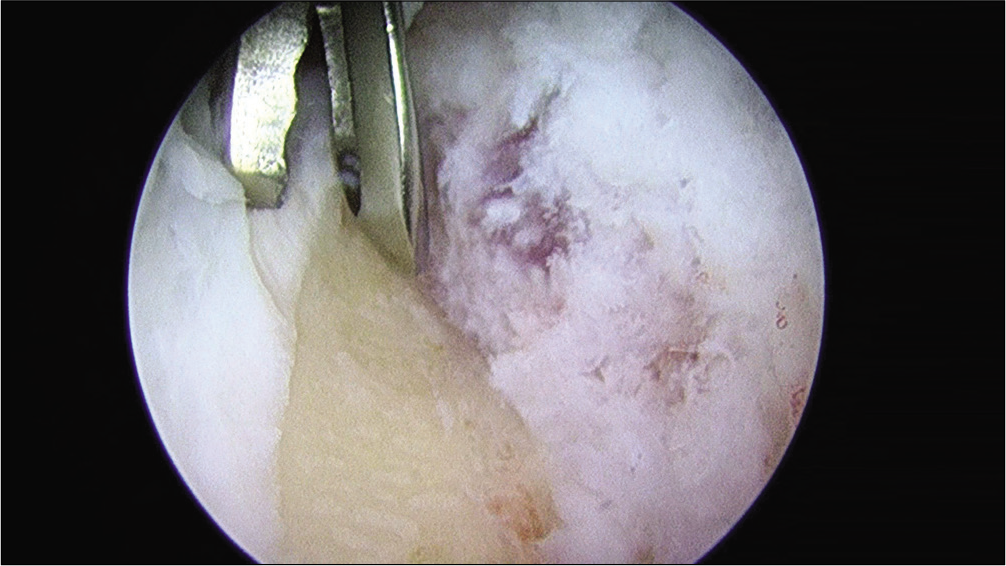
- Operative photograph. Coronoid osteophyte, removal of the remaining cartilaginous osteophyte, viewed from proximal anterolateral portal.
Symptomatic loss of the functional flexion-extension arc of 30–130° is an indication for osteocapsular arthroplasty.[12] Some essential daily tasks require more movement than this.[13] Therefore, lesser contractures can be treated surgically if they are causing functional problems, but it is important to manage patient expectations and clearly inform the patient that the elbow range of movement will most likely not be returned to normal. True locking of the elbow is also an indication for arthroscopy and loose bodies are removed easily. Pain caused by widespread loss of the ulnohumeral joint cartilage is not relieved by arthroscopic surgery (resting pain or pain experienced throughout the arc of movement) and it is better treated with other procedures such as joint resurfacing with interposition arthroplasty, partial, or total joint replacement.[14]
Pronation-supination loss is much less reliably corrected by arthroscopy, unless radial head excision is going to be performed.
A systematic review in 2017 concluded that arthroscopic debridement for primary OA of the elbow results in a statistically significant and a clinically relevant improvement in elbow range of motion and clinical outcomes with low complication and reoperation rates.[15]
In more severe cases, patients should also be consented for open treatment. This is particularly relevant in post-traumatic cases where arthroscopic management may not be possible due to intra-articular scaring.
When compared, arthroscopic and open debridement yields similar results. A recent systematic review found that no difference in patient-reported functional outcomes was found between open and arthroscopic procedures. Patients who underwent open debridement had worse pre-operative ROM and decreased post-operative motion compared with arthroscopic patients. The open group had a larger improvement in flexion than the arthroscopic group (19 vs. 10), but the arthroscopic group had greater final post-operative flexion (128 vs. 123). Conclusions drawn from the change in flexion and final flexion are limited by selection bias. There was a paucity of literature to compare forearm pronation and supination.[16] Others have found open surgery to give a better improvement in flexion. This may be related to open surgery involving a release of the posterior band of the medial collateral ligament (MCL). Therefore, we should consider open posterior MCL release with or without ulnar nerve anterior transposition when flexion is a problem.[17,18]
In their series of patients undergoing arthroscopic osteophyte resection and capsulectomy for primary OA, Adams et al. reported 2-year results of significantly improved flexion, extension, supination, MEPI, and pain.[19] Similar results have been reported by others.[20-22]
Pre-operative arc of motion is perhaps the main pre- operative factor affecting the outcome of arthroscopic debridement for OA. A pre-operative motion arc of 80° or more is recommended.[23]
Arthroscopic Outerbridge-Kashiwagi procedure is possible and has had good results.[24,25] In the procedure, the floor of the olecranon fossa is fenestrated to prevent impingement of the tip of the olecranon in extension and the tip of the coronoid in flexion. A potential pitfall is damage and weakening of the columns of the humerus or articular cartilage/subchondral bone of the trochlea or capitellum due to inaccurate penetration with the burr. This is made more likely by the presence of large osteophytes in the olecranon fossa that distort the normal anatomy. The risk of this can be reduced using fluoroscopy and a cannulated drill to penetrate the floor of the olecranon fossa in the correct position. A front cutting burr is also useful in the procedure.
Interposition arthroplasty is an option for severe elbow OA where the cartilage of the joint surfaces has been lost. One problem with this procedure is that it can destabilize the elbow. To reduce this problem, arthroscopically assisted interposition arthroplasty has been described, which allows the preservation of the MCL.[26]
RADIAL HEAD EXCISION
Radial head excision was first described by Lo and King.[27] It is indicated in symptomatic radiocapitellar OA or post- traumatic arthritis. Excision can be carried out using anterior portals, direct lateral and posterolateral portals, or a combination of all.
Excision can either be carried out in isolation or combined with osteocapsular arthroplasty. Arthroscopic joint release and radial head resection for stiffness with radiocapitellar OA in both OA and post-trauma patients have had good results.[28]
Radial head excision after trauma has also been reported. Early and late arthroscopic excision is possible, with good outcomes.[29,30] It is essential to ensure that the elbow injury pattern is one that will not lead to instability once the radial head is excised (i.e. the MCL is intact).
POST-TRAUMATIC ELBOW STIFFNESS
Osteocapsular arthroplasty is indicated to improve elbow range of movement in post-traumatic contractures and good results have been reported.[31-33] The results are comparable after arthroscopic treatment for post-traumatic and non- traumatic contracture.[34]
Non-operative treatment should be exhausted before considering surgery (physiotherapy, static progressive or dynamic splinting program).
Post-traumatic elbow contracture should be approached with caution due to the potential for intra-articular adhesions and the possibility of altered neurovascular anatomy. It can be difficult to enter the joint because of this and patients should be consented for conversion to an open procedure if necessary.
For severe contractures, an extra-articular starting point for capsulectomy has been described if it is not possible to enter the joint.[35] This should be done with extreme caution and only after considerable arthroscopic experience due to the closer proximity of neurovascular structures.
VALGUS EXTENSION OVERLOAD
This is prevalent in baseball players.[36,37] It leads to posteromedial impingement. O’Driscoll hypothesizes that the posterior or posteromedial pain is due to a fractured olecranon osteophyte.[38] It is clinically diagnosed with the extension impingement test or arm bar test. CT scan is the most helpful investigation.
Loss of terminal extension (≥35° flexion contracture) in high-level athletes can be corrected to near normal levels of elbow extension with arthroscopic release.[39]
Adolescent baseball players treated arthroscopically for posteromedial impingement have had good results.[40]
POSTERIOR ELBOW IMPINGEMENT
Boxers, in particular, are prone to this problem that can be successfully treated by arthroscopic debridement.[41,42] This has also been demonstrated in other athletes.[43,44]
ULNAR NERVE
Awareness of the ulnar nerve is of paramount importance in all elbow surgery. It should be located by palpation before arthroscopic surgery. Palpation for locating the ulnar nerve is only accurate proximal to the medial epicondyle.[45]
Ulnar nerve decompression is usually an open procedure, but some authors report good results of endoscopic release in combination with arthroscopic capsulectomy and osteophyte excision.[46]
DELAYED ONSET ULNAR NEURITIS (DOUN)
When correcting severe elbow contractures, there is a risk of inducing DOUN. In their series, O’Driscoll reported a rate of 11%. Some of these were rapid onset and progressive, accompanied by deteriorating ROM within 1 week of surgery. Risk factors for DOUN include a diagnosis of HO, pre-operative neurological symptoms, and a lower pre-operative arc of motion. The incidence and severity of DOUN can be reduced by performing a limited open release or transposition of the ulnar nerve at the beginning of the procedure. Rapid onset progressive DOUN should be treated with urgent ulnar nerve decompression or transposition.[47,48]
Williams et al. found that in those undergoing open and arthroscopic contracture release (but not ulnar nerve release), there was 8% occurrence of new persistent ulnar nerve symptoms. The rate of developing postoperative symptoms was higher if patients had preoperative flexion ≤100°.[49]
OCD
OCD of the humeral capitellum most commonly affects young athletes engaged in sports that repetitively stress the elbow. It is characterized by localized injury of subchondral bone of the humeral capitellum. To determine the best treatment option, it is important to differentiate between stable and unstable lesions. Stable lesions can be treated with rest, whereas unstable lesions, as well stable lesions that do not resolve with non-operative treatment, may require a surgical approach. MRI is the best imaging study to evaluate OCD lesions and to determine the stability of the OCD fragment. Arthroscopic surgery is becoming the standard treatment of capitellar OCD and gives good results. The distal ulnar portal has been described for this purpose.[50] It affords good exposure to the posterolateral capitellum for arthroscopic microfracture, drilling, burring, and local debridement of lesions. Differing degrees of elbow flexion enable access.
Arthroscopic debridement and microfracture for OCD of the capitellum yield good clinical results. Predictors of a better outcome are open capitellar physis as well as loose body removal and shorter duration of preoperative symptoms.[51] Microfracture in teenage athletes yields good results and allows return to sports at the same level.[52] Removal of loose body, drilling/microfracture for Grade IV elbow OCD shows good results 2 years after the procedure in adolescents.[53]
Other arthroscopic treatments that have shown good results include osteochondral autograft transfer (OAT), debridement, and fixation.
Arthroscopic OAT for the capitellum has encouraging mid- term results.[54] Donor site morbidity is a drawback of any OAT procedure.
Arthroscopic debridement alone of capitellar OCD lesions has yielded good results.[55]
Fixation of unstable OCD can also be achieved arthroscopically.[56,57]
OCD of the humeral trochlea is a different entity to that of the capitellum. It is rare and may cause problems, particularly in the adolescent athlete.[58]
FRACTURE MANAGEMENT
The indications for arthroscopic fracture management in the elbow are growing.[59] Arthroscopy can be used to perform reduction either directly or indirectly, check reduction, and perform fixation.
RADIAL HEAD
There has been work around the use of arthroscopy in the management of radial head fractures. Some of this has focussed on fracture patterns and portal placement for safe and effective treatment. The location of fracture lines in the radial head is predictable and this can help us to assess which operative strategies will work best for particular patterns.[60] From anterolateral and anteromedial portals, a 220° arc of the radial head is accessible.[61] Using more distally placed anterolateral and anteromedial portals can provide better screw placement, but with the added risks to neurovascular structures that are associated with the use of distal portals.[62]
The technique of arthroscopic radial head fracture fixation has been described by Rolla et al.[63] Michels et al. reported a series of Mason 2 radial head fractures reduced and fixed arthroscopically with mostly excellent results.[64] The technique is technically demanding.
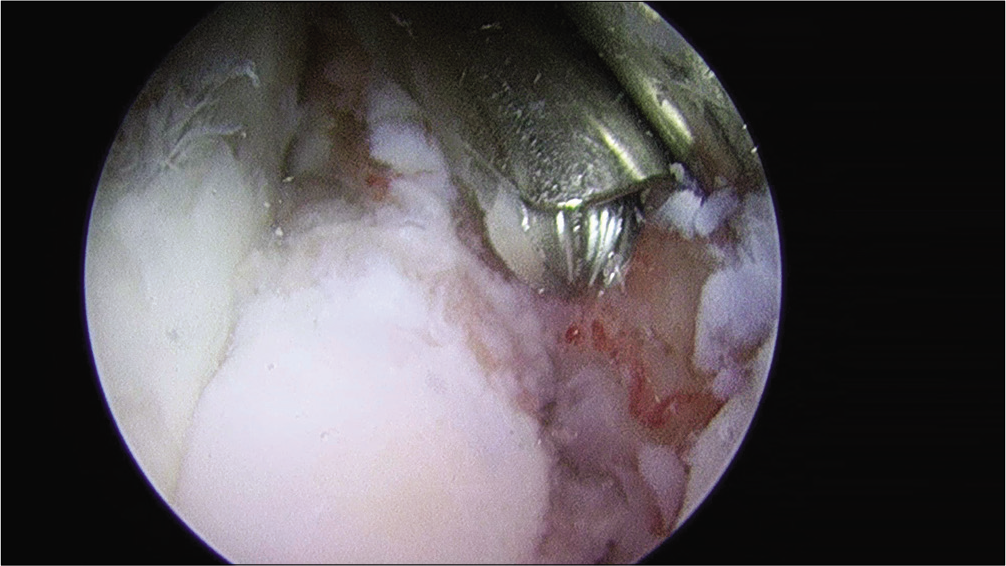
CAPITELLUM
Hardy et al. described arthroscopic reduction and fixation of a Type I Hahn-Steinthal capitellum fracture.[65] Arthroscopic- assisted reduction can be achieved with the ability to assess the quality of reduction. Fixation can then be achieved with posterior to anterior cannulated compression screws. Involvement of the lateral column of the distal humerus may mean that a stable fixation cannot be achieved arthroscopically. In these cases, open reduction and fixation are necessary, with reduction and plating of the lateral column [Figures 2, 11 and 12].
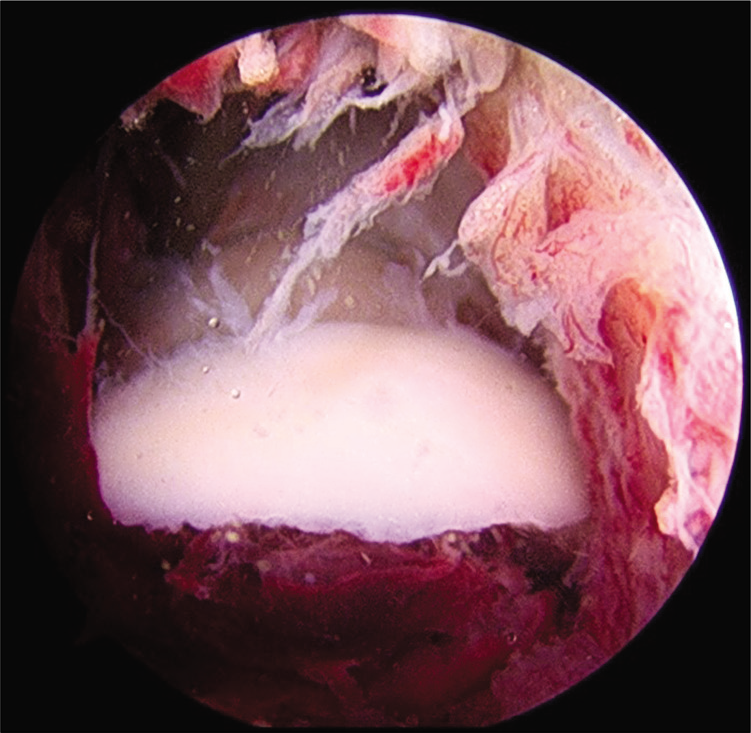
- Arthroscopic view of capitellum fracture fragment, viewed from proximal anteromedial portal.

- Arthroscopic view of capitellum fracture fragment after reduction, viewed from proximal anteromedial portal.
CORONOID
The technique and indications for arthroscopic treatment of coronoid fractures are evolving.[66-71] Coronoid fractures are usually part of a complex injury pattern. It is important to understand these patterns and the associated injuries that often need to be addressed. The coronoid can be assessed and treated arthroscopically in certain situations.
Lee et al. reported a series of terrible triad injuries that were treated entirely arthroscopically.[72] The coronoid was fixed in all patients with Kirschner wires or pull-out sutures. About 17% had radial head fractures treated with screws or Kirschner wires and 46% had a fragment excised. The lateral collateral ligament was repaired in all patients. They report good outcomes (arc 5–133°) with 17% coronoid non-union.
Coronoid fixation has so far been achieved by retrograde passage of threaded wires and pull-out sutures. Work is ongoing to assess new anterior and anteromedial portals for antegrade fixation of coronoid fractures.[73,74] It must be stressed that these approaches have a much higher risk of neurovascular injury.
OLECRANON BURSITIS
Surgery for olecranon bursitis is sometimes avoided due to concerns about wound complications and healing problems. This has led to the exploration of endoscopic techniques by some authors. Endoscopic bursectomy for olecranon bursitis can be performed either intra- or extra-bursal.[75,76]
DISTAL BICEPS TENDON
Endoscopic treatment of distal biceps tendon pathology has been described. It can be used to assess and treat partial tears, excise the symptomatic bicipitoradial bursa, and repair acute and chronic ruptures.[77-80]
TENNIS ELBOW (LATERAL EPICONDYLITIS)
The mainstay of treatment for tennis elbow is physiotherapy. However, in the small percentage of patients whose condition is resistant to non-operative treatment, functional outcomes of both open and arthroscopic releases are good. Patients may report less pain with arthroscopic release. Although the risk of complications is similar regardless of technique, the risk of infectious complications may be slightly higher with open releases.[81]
Two recent randomized trials comparing arthroscopic and open surgery for lateral epicondylitis found that both procedures were effective, with no major differences in outcomes.[82,83]
The advantage of arthroscopy over open treatment is that coexisting pathologies such as radiocapitellar OA can be diagnosed.[84]
Mullett et al. described four anatomical relationships of the annular ligament, lateral capsule, and radial head in cadavers.[85] This was further studied by Tsuji et al. who concluded that the synovial fold is physiologic capsular tissue located on the proximal edge of the annular ligament. It is distinct from the annular ligament but has a close correlation with the common extensor tendon enthesis at the lateral epicondyle.[86]
Almost one half of patients suffering from recalcitrant lateral epicondylitis display signs of lateral ligamentous laxity, and over 85% demonstrate at least one intra-articular abnormality. The most frequent findings are synovitis and lateral capitellar chondropathy, which correlate significantly with the presence of lateral ligamentous laxity. Arrigoni et al. hypothesized that this supports a sequence of pathologic changes that result from a symptomatic minor instability of the lateral elbow SMILE condition.[87]
PLICA SYNDROME
A plica associated with catching and aching treated by arthroscopic excision was first described by Clarke.[88] Antuna and O’Driscoll described the painful snapping elbow associated with hypertrophic synovial folds and radiocapitellar chondromalacia. Symptoms were relieved in most patients by arthroscopic debridement of the plica.[89] The snapping occurs between approximately 80° and 110° of flexion with the forearm in pronation. The snapping is often reproducible by passively flexing the pronated elbow (flexion-pronation test). The range of movement is usually normal. Arthroscopic examination may show a transient interposition and compression of the plica.[89,90]
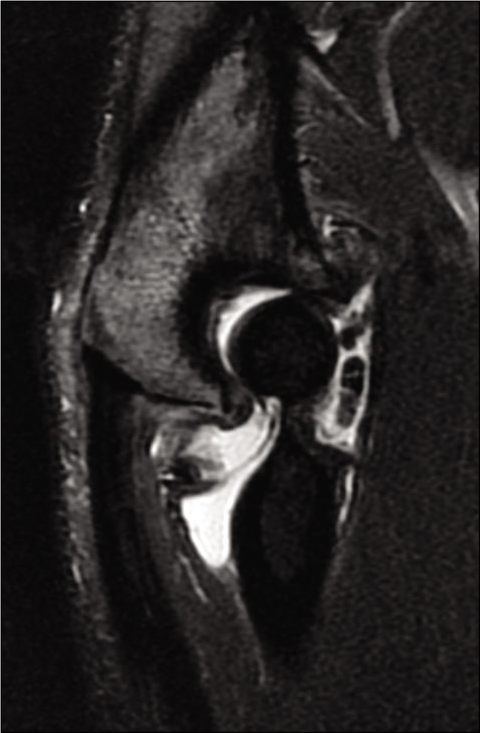
Plica can be seen on MRI [Figure 13] and correlate with arthroscopic findings.[91]
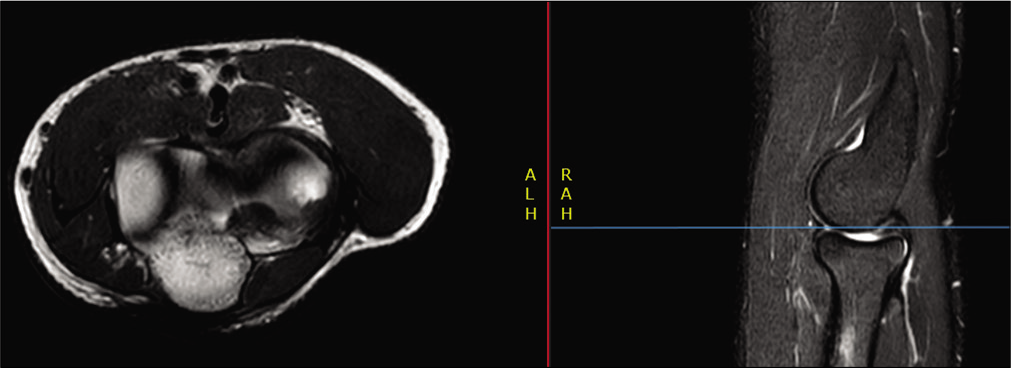
- Axial and sagittal sequences from magnetic resonance imaging scan showing a Plica. This can be seen protruding into the posterior aspect of the radiocapitellar joint on the sagittal sequence and covering the posterior part of the radial head on the axial sequence.
Several authors have reported improvement of symptoms from arthroscopic excision.[88-96] It is important to remember that there is potential for iatrogenic injury to the lateral ulnar collateral ligament (LUCL) when excising synovial folds in the radiocapitellar compartment. The lateral 25% of the radial head is overlaid by the LUCL, up to a maximum of 40%.[97]
INSTABILITY
Arthroscopic treatment mainly focusses on the LUCL. It should be noted that in a normal elbow, arthroscopic visualization of the MCL is limited.[98,99] Only the most anterior part of the anterior MCL is visible. The entire posterior bundle can be seen through posterior portals. Placing the arthroscope in the posteromedial gutter should be done with caution, because this places direct pressure on the ulnar nerve.
In acute injury, the LUCL can be repaired arthroscopically.[100] Good results have been reported in athletes and high-demand patients after simple elbow dislocation.[101]
The LUCL can also be repaired as part of terrible triad injuries and posteromedial rotatory instability injuries.[70,72,102]
Arthroscopy is also of value in assessing chronic instability such as posterolateral rotatory instability (PLRI). In lower grade PLRI, LUCL plication has had promising results.[103]
PEDIATRIC
Arthroscopy in the pediatric elbow has several indications (fracture reduction and fixation, contracture release, debridement, diagnostic, loose body removal, and treatment of OCD). It has been found to have an acceptable safety profile when used by specialist surgeons.[104,105]
Andelman reported good outcomes of arthroscopic contracture release in pediatric patients. Contractures were mostly after radial head fracture. There was a good improvement in flexion-extension arc (that was better than the improvement in pronosupination).[106]
In the treatment of lateral condyle fractures, the arthroscope has been used to check reduction after initial K-wire insertion. This may avoid open reduction. If adequate reduction is confirmed, a further K-wire is inserted or the elbow is re-reduced and checked again arthroscopically.[107,108] Arthroscopy has also been used in reduction and percutaneous pinning of radial neck fractures.[109]
POST-OPERATIVE REHABILITATION
The minimally invasive nature of arthroscopy causes less tissue damage and theoretically is advantageous for early rehabilitation. Good post-operative physiotherapy and patient information are essential for a good outcome.
CONTINUOUS PASSIVE MOVEMENT (CPM)
The use of CPM to prevent elbow stiffness is based on sound scientific theory.[110] There are non-randomized reports of the successful use of CPM after open elbow contracture release.[111,112] Conventionally, the use of CPM to help maintain the ROM gained surgically is logical; however, there is currently no evidence that it improves the final range of movement achieved.[112] There are ongoing randomized controlled trials to clarify this.[113]
Regional nerve block allows excellent post-operative pain relief during initial CPM. Patients have found this to be a positive experience. Both patients and staff should be aware of the potential for skin damage in the insensate arm when using CPM.
CONCLUSION
The indications for elbow arthroscopy continue to evolve as surgical techniques and knowledge in the field advance. It is essential that those undertaking elbow arthroscopy obtain proper training through cadaveric simulation courses and surgical fellowships to optimise patient outcomes and to avoid complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
References
- Elbow arthroscopy in acute injuries. Knee Surg Sports Traumatol Arthrosc. 2012;20:2542-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of elbow fractures. Hand Clin. 2015;31:651-61.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of the registration accuracy of navigation-assisted arthroscopic debridement for elbow osteoarthritis. J Shoulder Elbow Surg. 2019;28:2400-8.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the 70 degrees arthroscope for improved visualization with common arthroscopic procedures. Arthroscopy. 2010;26:1684-96.
- [CrossRef] [PubMed] [Google Scholar]
- Chondrotoxic effects of local anesthetics on human knee articular cartilage: A systematic review. PM R. 2019;11:379-400.
- [CrossRef] [PubMed] [Google Scholar]
- Basics of elbow arthroscopy Part I: Surface anatomy, portals, and structures at risk. Arthrosc Tech. 2016;5:e1339-43.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical results after arthroscopic treatment for septic arthritis of the elbow joint. Arthroscopy. 2014;30:673-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic synovectomy of the elbow for rheumatoid arthritis. A prospective study. J Bone Joint Surg Br. 1997;79:770-2.
- [CrossRef] [Google Scholar]
- Arthroscopic synovectomy for the rheumatoid elbow. Arthroscopy. 2010;26:1195-202.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic synovectomy for the rheumatoid elbow: A short-term outcome. J Shoulder Elbow Surg. 2004;13:652-5.
- [CrossRef] [PubMed] [Google Scholar]
- The role of arthroscopic synovectomy in the management of hemarthrosis in hemophilia patients: Financial perspectives. Arthroscopy. 2002;18:789-94.
- [CrossRef] [PubMed] [Google Scholar]
- A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872-7.
- [CrossRef] [PubMed] [Google Scholar]
- Functional elbow range of motion for contemporary tasks. J Bone Joint Surg Am. 2011;93:471-7.
- [CrossRef] [PubMed] [Google Scholar]
- Posttraumatic elbow arthritis in the young adult: Evaluation and management. J Am Acad Orthop Surg. 2012;20:704-14.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic debridement for primary degenerative osteoarthritis of the elbow leads to significant improvement in range of motion and clinical outcomes: A systematic review. Arthroscopy. 2017;33:2255-62.
- [CrossRef] [PubMed] [Google Scholar]
- The clinical impact of arthroscopic vs. Open osteocapsular debridement for primary osteoarthritis of the elbow: A systematic review. J Shoulder Elbow Surg. 2020;29:689-98.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcome of osteocapsular arthroplasty for primary osteoarthritis of the elbow: Comparison of arthroscopic and open procedure. Arthroscopy. 2019;35:1083-9.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical outcomes for post-traumatic stiffness after elbow fracture: Comparison between open and arthroscopic procedures for intra-and extra-articular elbow fractures. J Shoulder Elbow Surg. 2019;28:1998-2006.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoarthritis of the elbow: Results of arthroscopic osteophyte resection and capsulectomy. J Shoulder Elbow Surg. 2008;17:126-31.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic debridement in the treatment of patients with osteoarthritis of the elbow, based on computer simulation. Bone Joint J. 2014;96:237-41.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of elbow osteoarthritis. J Hand Surg Am. 2017;42:640-50.
- [CrossRef] [PubMed] [Google Scholar]
- Retrospective comparative analysis of elbow arthroscopy used to treat primary osteoarthritis with and without release of the posterior band of the medial collateral ligament. Arthroscopy. 2017;33:1506-11.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic debridement for primary osteoarthritis of the elbow: Analysis of preoperative factors affecting outcome. J Shoulder Elbow Surg. 2014;23:1381-7.
- [CrossRef] [PubMed] [Google Scholar]
- The arthroscopic ulnohumeral arthroplasty: From mini-open to arthroscopic surgery. Minim Invasive Surg. 2011;2011:798084.
- [CrossRef] [PubMed] [Google Scholar]
- The outerbridge-kashiwaghi procedure in elbow arthroscopy. Acta Orthop Belg. 2010;76:468-71.
- [Google Scholar]
- Arthroscopically assisted elbow interposition arthroplasty without hinged external fixation: Surgical technique and patient outcomes. J Shoulder Elbow Surg. 2015;24:947-54.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic elbow joint release with radial head resection arthroplasty: 12 cases. Orthop Traumatol Surg Res. 2015;101:735-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic radial head excision in managing elbow trauma. Int Orthop. 2012;36:2507-12.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic excision of the radial head: Clinical outcome in 12 patients with post-traumatic arthritis after fracture of the radial head or rheumatoid arthritis. Arthroscopy. 2001;17:918-23.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of arthroscopic arthrolysis for the post-traumatic elbow stiffness. Knee Surg Sports Traumatol Arthrosc. 2015;23:2715-20.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of post-traumatic elbow contracture. J Shoulder Elbow Surg. 2002;11:624-9.
- [CrossRef] [PubMed] [Google Scholar]
- Elbow arthroscopy in stiff elbow. Knee Surg Sports Traumatol Arthrosc. 2014;22:467-73.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic arthrolysis of posttraumatic and non-traumatic elbow stiffness offers comparable clinical outcomes. BMC Musculoskelet Disord. 2019;20:285.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic extracapsular capsulectomy of the elbow: A neurovascularly safe technique for high-grade contractures. Arthroscopy. 2007;23:789-92.
- [CrossRef] [PubMed] [Google Scholar]
- Elbow arthroscopy for treatment of valgus extension overload. Arthrosc Tech. 2018;7:e705-10.
- [CrossRef] [PubMed] [Google Scholar]
- Elbow arthroscopy: Treatment of the thrower's elbow. Instr Course Lect. 2006;55:95-107.
- [Google Scholar]
- Editorial commentary: It's the fracture, not the fragment, that causes the pain: Posteromedial elbow impingement in baseball players. Arthroscopy. 2018;34:111-3.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic restoration of terminal elbow extension in high-level athletes. Am J Sports Med. 2010;38:2509-15.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcome of arthroscopic treatment for posteromedial elbow impingement in adolescent baseball players. Arthroscopy. 2018;34:105-10.
- [CrossRef] [PubMed] [Google Scholar]
- Boxer's elbow: Internal impingement of the coronoid and olecranon process. A report of seven cases. J Shoulder Elbow Surg. 2017;26:376-81.
- [CrossRef] [PubMed] [Google Scholar]
- Posterolateral elbow impingement in professional boxers. Am J Sports Med. 2008;36:328-32.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment successfully treats posterior elbow impingement in an athletic population. Knee Surg Sports Traumatol Arthrosc. 2018;26:306-11.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of posterior impingement of the elbow in athletes: A medium-term follow-up in sixteen cases. J Shoulder Elbow Surg. 2009;18:279-82.
- [CrossRef] [PubMed] [Google Scholar]
- Locating the ulnar nerve during elbow arthroscopy using palpation is only accurate proximal to the medial epicondyle. Knee Surg Sports Traumatol Arthrosc. 2019;27:3254-60.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic ulnar nerve decompression in the setting of elbow osteoarthritis. J Hand Surg Am. 2012;37:663-8.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed-onset ulnar neuritis after release of elbow contracture: Preventive strategies derived from a study of 563 cases. Arthroscopy. 2014;30:947-56.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed-onset ulnar neuritis after release of elbow contractures: Clinical presentation, pathological findings, and treatment. Am J Sports Med. 2014;42:2113-21.
- [CrossRef] [PubMed] [Google Scholar]
- The contracted elbow: Is ulnar nerve release necessary? J Shoulder Elbow Surg. 2012;21:1632-6.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondritis dissecans of the capitellum: A review of the literature and a distal ulnar portal. Arthroscopy. 2011;27:122-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcome after arthroscopic debridement and microfracture for osteochondritis dissecans of the capitellum. Am J Sports Med. 2017;45:2312-8.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondritis dissecans of the elbow: Excellent results in teenage athletes treated by arthroscopic debridement and microfracture. Croat Med J. 2012;53:40-7.
- [CrossRef] [PubMed] [Google Scholar]
- Early results of drilling and/or microfracture for grade IV osteochondritis dissecans of the capitellum. J Pediatr Orthop. 2016;36:803-9.
- [CrossRef] [PubMed] [Google Scholar]
- Encouraging mid-term outcomes for arthroscopic autologous osteochondral transplant (OAT) in capitellum osteochondritis dissecans (OCD) Knee Surg Sports Traumatol Arthrosc. 2019;27:3291-6.
- [CrossRef] [PubMed] [Google Scholar]
- Results of arthroscopic debridement for osteochondritis dissecans of the elbow. Br J Sports Med. 2006;40:966-9.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of arthroscopic treatment of osteochondritis dissecans of the capitellum and description of the technique. J Shoulder Elbow Surg. 2015;24:1607-12.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic technique for fragment fixation using absorbable pins for osteochondritis dissecans of the humeral capitellum: A report of 4 cases. Knee Surg Sports Traumatol Arthrosc. 2010;18:831-5.
- [CrossRef] [PubMed] [Google Scholar]
- Osteochondritis dissecans of the humeral trochlea: Characterization of a rare disorder based on 28 cases. Am J Sports Med. 2019;47:2167-73.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of acute elbow fractures. Chir Main. 2006;25(Suppl 1):S114-20.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of the transverse pattern of Mason II radial head fractures and its usefulness in arthroscopic osteosynthesis, Anatomo-surgical study. Rev Esp Cir Ortop Traumatol. 2019;63:12-9.
- [CrossRef] [Google Scholar]
- An anatomic evaluation of arthroscopic access to the radial head. Arthroscopy. 2017;33:953-8.
- [CrossRef] [PubMed] [Google Scholar]
- Modified anteromedial and anterolateral elbow arthroscopy portals show superiority to standard portals in guiding arthroscopic radial head screw fixation. Knee Surg Sports Traumatol Arthrosc. 2019;27:3276-83.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of fractures of the radial head. Arthroscopy. 2006;22:233, e1-6
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of Mason Type 2 radial head fractures. Knee Surg Sports Traumatol Arthrosc. 2007;15:1244-50.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of capitellum fracture of the humerus. Arthroscopy. 2002;18:422-6.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic-assisted treatment of coronoid fractures. Arthroscopy. 2007;23:1060-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopically assisted coronoid fracture fixation: A preliminary report. Clin Orthop Relat Res. 2008;466:3147-52.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic fixation of coronoid process fractures through coronoid tunnelling and capsular plication. Joints. 2016;4:153-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopically assisted surgery for coronoid fractures. Orthopedics. 2015;38:742-6.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopically-assisted fixation of anteromedial coronoid facet fracture and lateral ulnar collateral ligament repair for acute posteromedial rotatory fracture dislocation of the elbow. Shoulder Elbow. 2019;11:378-83.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: Do we need to treat all lesions operatively in elbow terrible triad? Arthroscopy. 2020;36:441.
- [CrossRef] [PubMed] [Google Scholar]
- Case series of all-arthroscopic treatment for terrible triad of the elbow: Indications and clinical outcomes. Arthroscopy. 2020;36:431-40.
- [CrossRef] [PubMed] [Google Scholar]
- No neurovascular damage after creation of an accessory anteromedial portal for arthroscopic reduction and fixation of coronoid fractures. Knee Surg Sports Traumatol Arthrosc. 2019;27:314-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic reduction and fixation of coronoid fractures with an exchange rod-a new technique. J Orthop Surg Res. 2017;12:9.
- [CrossRef] [PubMed] [Google Scholar]
- Olecranon extrabursal endoscopic bursectomy. Tech Hand Up Extrem Surg. 2013;17:173-5.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic bursal resection: The olecranon bursa and prepatellar bursa. Arthroscopy. 2000;16:249-53.
- [CrossRef] [Google Scholar]
- Treatment of partial distal biceps tendon tears. Sports Med Arthrosc Rev. 2008;16:154-61.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic resection of the bicipitoradial bursa. Sports Med Arthrosc Rev. 2016;24:7-10.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic repair of acute and chronic retracted distal biceps ruptures. J Hand Surg Am. 2016;41:e501-7.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic repair of distal biceps tendon using an EndoButton. Arthroscopy. 2005;21:897.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of tennis elbow surgery: Open versus arthroscopic versus percutaneous release of the common extensor origin. Arthroscopy. 2017;33:1260-8.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic versus open lateral release for the treatment of lateral epicondylitis: A prospective randomized controlled trial. Arthroscopy. 2018;34:3177-84.
- [CrossRef] [PubMed] [Google Scholar]
- The nirschl procedure versus arthroscopic extensor carpi radialis brevis debridement for lateral epicondylitis. J Shoulder Elbow Surg. 2017;26:118-24.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral compartment cartilage changes and lateral elbow pain. Acta Orthop Belg. 2009;75:37-40.
- [Google Scholar]
- Arthroscopic treatment of lateral epicondylitis: Clinical and cadaveric studies. Clin Orthop Relat Res. 2005;439:123-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic, macroscopic, and microscopic anatomy of the synovial fold of the elbow joint in correlation with the common extensor origin. Arthroscopy. 2008;24:34-8.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-articular findings in symptomatic minor instability of the lateral elbow (SMILE) Knee Surg Sports Traumatol Arthrosc. 2017;25:2255-63.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic, lateral synovial fringe (plica) of the elbow joint. Arthroscopy. 1988;4:112-6.
- [CrossRef] [Google Scholar]
- Snapping plicae associated with radiocapitellar chondromalacia. Arthroscopy. 2001;17:491-5.
- [CrossRef] [PubMed] [Google Scholar]
- Snapping elbow caused by hypertrophic synovial plica in the radiohumeral joint: A report of three cases and review of literature. Arch Orthop Trauma Surg. 2010;130:347-51.
- [CrossRef] [PubMed] [Google Scholar]
- Prominent synovial plicae in radiocapitellar joints as a potential cause of lateral elbow pain: Clinico-radiologic correlation. J Shoulder Elbow Surg. 2018;27:1349-56.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and diagnostic outcomes in arthroscopic treatment for posterolateral plicae impingement within the radiocapitellar joint. Medicine (Baltimore). 2019;98:e15497.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic resection of humeroradial synovial plica for persistent lateral elbow pain. J Orthop Surg (Hong Kong). 2015;23:11-4.
- [CrossRef] [PubMed] [Google Scholar]
- The posterolateral plica: A cause of refractory lateral elbow pain. J Shoulder Elbow Surg. 2006;15:367-70.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of posterolateral elbow impingement from lateral synovial plicae in throwing athletes and golfers. Am J Sports Med. 2006;34:438-44.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral sided snapping elbow caused by a meniscus: Two case reports and literature review. Knee Surg Sports Traumatol Arthrosc. 2010;18:840-4.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic relations between the lateral collateral ligament and the radial head: Implications for arthroscopic resection of the synovial fold of the elbow. Knee Surg Sports Traumatol Arthrosc. 2015;23:3421-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic assessment of the medial collateral ligament complex of the elbow. Am J Sports Med. 1995;23:396-400.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic visualization of the medial collateral ligament of the elbow. J Shoulder Elbow Surg. 2019;28:2232-7.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical technique for arthroscopic lateral collateral ligament repair. JBJS Essent Surg Tech. 2016;6:e33.
- [CrossRef] [PubMed] [Google Scholar]
- A preliminary report of acute and subacute arthroscopic repair of the radial ulnohumeral ligament after elbow dislocation in the high-demand patient. Arthroscopy. 2014;30:679-87.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes of arthroscopic lateral ulnar collateral ligament repair with or without intra-articular fracture. J Orthop Surg (Hong Kong). 2020;28:2309499020908348.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic R-LCL plication for symptomatic minor instability of the lateral elbow (SMILE) Knee Surg Sports Traumatol Arthrosc. 2017;25:2264-70.
- [CrossRef] [Google Scholar]
- Pediatric elbow arthroscopy: Indications and safety. J Shoulder Elbow Surg. 2017;26:1862-6.
- [CrossRef] [PubMed] [Google Scholar]
- Elbow arthroscopy in children and adolescents: Analysis of outcome and complications. Eur J Med Res. 2018;23:42.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic elbow contracture release in the pediatric patient. J Pediatr Orthop. 2018;38:e507-13.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of arthroscopy-assisted closed reduction and percutaneous pinning for a displaced pediatric lateral condylar humeral fracture. J Pediatr Orthop. 2019;39:e548-51.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic-assisted reduction and percutaneous external fixation of lateral condyle fractures of the humerus. Arthroscopy. 2007;23:1131.e1-4.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic reduction and percutaneous fixation of a radial neck fracture in a child. Arthroscopy. 2004;20(Suppl 2):90-3.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous passive motion (CPM): Theory and principles of clinical application. J Rehabil Res Dev. 2000;37:179-88.
- [Google Scholar]
- Outcomes of open arthrolysis of the elbow without post-operative passive stretching. J Bone Joint Surg Br. 2012;94:348-52.
- [CrossRef] [PubMed] [Google Scholar]
- Open elbow contracture release: Postoperative management with and without continuous passive motion. J Hand Surg Am. 2009;34:858-65.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous passive motion and physical therapy (CPM) versus physical therapy (PT) versus delayed physical therapy (DPT) after surgical release for elbow contractures; a study protocol for a prospective randomized controlled trial. BMC Musculoskelet Disord. 2017;18:484.
- [CrossRef] [PubMed] [Google Scholar]






