Translate this page into:
History of wrist arthroscopy

*Corresponding author: Gregory I. Bain, Department of Orthopaedics and Trauma Surgery, Flinders University and Flinders Medical Centre, Adelaide, Australia. admin@gregbain.com.au
-
Received: ,
Accepted: ,
How to cite this article: Baker A, Whipple TL, Poehling GG, Bain GI. History of wrist arthroscopy. J Arthrosc Surg Sport Med 2020;1(1):44-64.
Abstract
The history of wrist arthroscopy is a global one, founded on the development of the arthroscope in Japan in the first half of the 20th century. Japanese surgeons Kenji Takagi and Masaki Watanabe helped develop the arthroscope and the techniques and concepts of arthroscopy, with a focus on the knee. With the improvement in optics, lighting. and miniaturization, arthroscopy of the wrist could be more safely performed. In the 1980’s Terry Whipple, Gary Poehling and James Roth brought a standardized, safe, and reproducible approach to wrist arthroscopy. They conducted courses, revolutionized teaching, and added publications. This led to an explosion in the clinical utilization of wrist arthroscopy and further development of new techniques. In 2005, Christophe Mathoulin created the European Wrist Arthroscopy Society (EWAS) which conducted cadaveric workshops, initially in Europe and then throughout the world. In 2015, PC Ho created the Asia Pacific Wrist Association, which has provided meetings and workshops throughout Asia. Recently, EWAS became International Wrist Arthroscopy Society, truly providing an international approach. This article brings these periods together and presents a thorough picture of the development of wrist arthroscopy.
Keywords
History
Arthroscopy
Joint
Orthopedics
Wrist
Minimally invasive
Development
INTRODUCTION
Wrist arthroscopy has a rich history, from the foundations laid by the early experiments in arthroscopic technology By Kenji Takagi and Masaki Watanabe in Japan in the early 20th century, to the modern therapeutic applications spreading into the soft-tissue spaces of the wrist and forearm. Miniaturization of existing technologies was a key factor in allowing the passion for arthroscopy to extend to the wrist, driven by individuals such as Terry Whipple (USA), Gary Poehling (USA), and James Roth (Canada).
This early period revolved around the formation of safe access portals and surgical technique, but quickly progressed into therapeutic applications for the technology. Throughout the 1990s and 2000s, these therapeutic options have flourished with the support of surgeons around the world and their professional organizations: European Wrist Arthroscopy Society (EWAS), International Wrist Arthroscopy Society (IWAS), and Asia Pacific Wrist Association (APWA). Education in the skill of wrist arthroscopy is at the forefront of their mission, allowing more and more patients to gain benefit from the procedure.
This article draws on the stories of influential figures in the history of arthroscopy including Takagi, Watanabe, Hiroshi Ikeuchi (Japan), and Robert Jackson (Canada); seminal papers; and an interview of Whipple and Poehling conducted by Greg Bain (Australia) in October 2019. Together these sources bring together the global perspectives of the development and evolution of wrist arthroscopy as a diagnostic and therapeutic tool.
THE EARLY DEVELOPMENT OF ARTHROSCOPY
The origin and development of arthroscopy evolved in Japan in the early 20th century. In 1918, Takagi [Figure 1] utilized a 7.3 mm Charrier No. 22 Cystoscope to perform an arthroscopy on a cadaveric tuberculosis knee joint.[1] Within the next 2 years, Takagi began using a modified cystoscope clinically and successfully diagnosed tuberculosis in the knee joint of patients [Figure 2].[2] At around the same time, in 1921 in Switzerland, Eugen Bircher [Figure 3] published the first clinical arthroscopy report.[3] This report described a procedure using a Jacobaeus laparoscope with oxygen dilatation [Figure 4]. In 1925, Philip Kreuscher (USA) described the use of arthroscopy for the assessment of meniscal injuries.[4]
![Kenji Takagi (Japan), a pioneer of arthroscopy. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., preface, Copyright 1979, with permission from Springer.[2]](/content/115/2020/1/1/img/JASSM-1-044-g001.png)
- Kenji Takagi (Japan), a pioneer of arthroscopy. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., preface, Copyright 1979, with permission from Springer.[2]
![Kenji Takagi’s No. 1 Arthroscope from 1931, 3.5 mm diameter. Reprinted from Atlas of arthroscopy, 3rd edition, Watanabe et al., History of arthroscopy, p. 2, Copyright 1979, with permission from Springer.[2]](/content/115/2020/1/1/img/JASSM-1-044-g002.png)
- Kenji Takagi’s No. 1 Arthroscope from 1931, 3.5 mm diameter. Reprinted from Atlas of arthroscopy, 3rd edition, Watanabe et al., History of arthroscopy, p. 2, Copyright 1979, with permission from Springer.[2]
![Eugen Bircher (Switzerland) published the first clinical arthroscopy report in 1921, performing the procedure with a laparoscope. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., History of Arthroscopy, p. 3, Copyright 1979, with permission from Springer.[2]](/content/115/2020/1/1/img/JASSM-1-044-g003.png)
- Eugen Bircher (Switzerland) published the first clinical arthroscopy report in 1921, performing the procedure with a laparoscope. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., History of Arthroscopy, p. 3, Copyright 1979, with permission from Springer.[2]
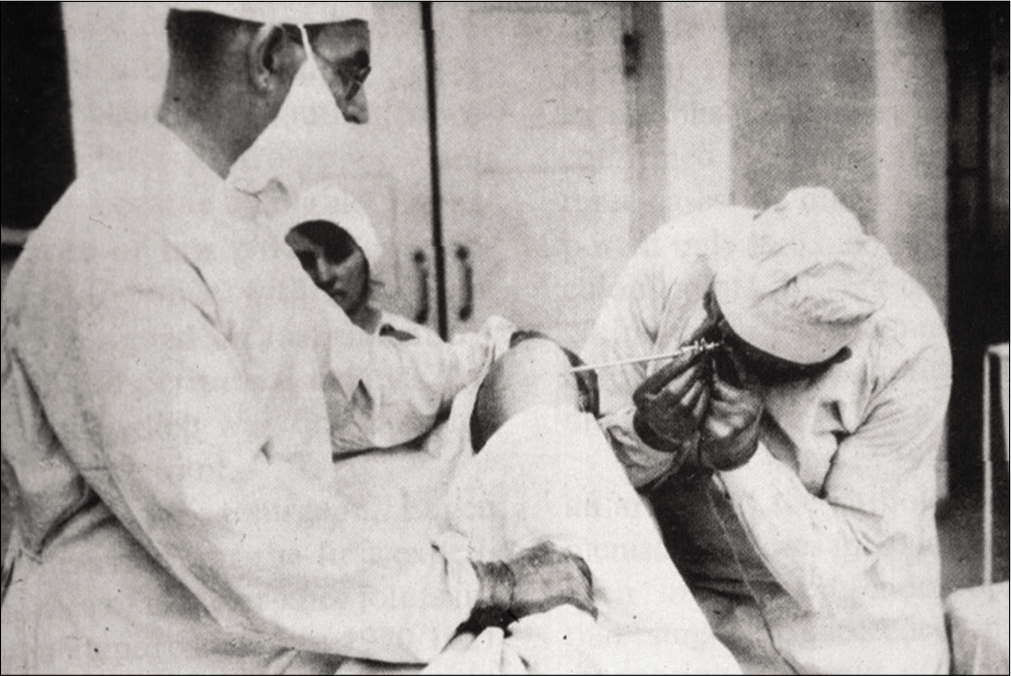
- Eugen Bircher performing knee arthroscopy in the 1920s. Reprinted from The Journal of Arthroscopic and Related Surgery, Vol 19, no. 7, Kieser CW, Jackson RW, Eugen Bircher (1882–1956) the first knee surgeon to use diagnostic arthroscopy, p 773., Copyright 2003, with permission from Elsevier.
For many years, Takagi’s work was thought to be the initial foray into arthroscopy. But in 2001, Jackson and Christopher Kieser (USA) discovered that there was a report of arthroscopy from 6 years earlier![5] A presentation in 1912 by Severin Nordentoft (Denmark) outlined the use of a 5 mm device that he termed an arthroscope to examine a knee joint.
These early explorations focused largely on the knee joint; however, Michael Burman (USA) [Figure 5] outlined the use of arthroscopy in other joints in 1931.[6] Burman examined more than 90 joints, including knees (40), hips (20), shoulders (25), wrists (4), and 2 or 3 ankle or elbow joints. They experimented with various methods of joint distention, including combinations of distilled water, saline, boric acid solutions, and various gases. Traction was also utilized, and he noted that traction increases the joint space of the wrist “as much as one-eighth to one-quarter of an inch.”
![Michael Burman (USA) was one of the first surgeons to experiment with the use of arthroscopy in joints other than the knee, examining hips, shoulders, wrists, ankles, and elbows in the early 1930s. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., History of Arthroscopy, p. 3, Copyright 1979, with permission from Springer.[2]](/content/115/2020/1/1/img/JASSM-1-044-g005.png)
- Michael Burman (USA) was one of the first surgeons to experiment with the use of arthroscopy in joints other than the knee, examining hips, shoulders, wrists, ankles, and elbows in the early 1930s. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., History of Arthroscopy, p. 3, Copyright 1979, with permission from Springer.[2]
FROM DIAGNOSTIC TO THERAPEUTIC ARTHROSCOPY
Initially arthroscopy was purely a diagnostic tool; however, even this was difficult, due to the cumbersome nature of the viewing ports, the diameter of the scopes and their fragile incandescent light bulbs! With the early arthroscope models, their light sources were offset from the end of the scope, making them particularly vulnerable. On a number of occasions, these light bulbs broke off and were lost within the knee joint.[7] When this first happened, Ikeuchi reported the problem to his mentor Watanabe [Figure 6]. Watanabe suggested to use a second arthroscope to locate the light bulb, and through another portal, retrieve the bulb with a pair of forceps. When this adversity next occurred, therapeutic arthroscopy was born!
![Masaki Watanabe made many contributions to the technical development of the arthroscope. He was the first to develop standardized methods of arthroscopy and published the first Atlas of arthroscopy.[1] Courtesy Gary Poehling.](/content/115/2020/1/1/img/JASSM-1-044-g006.png)
- Masaki Watanabe made many contributions to the technical development of the arthroscope. He was the first to develop standardized methods of arthroscopy and published the first Atlas of arthroscopy.[1] Courtesy Gary Poehling.
This inspired Ikeuchi to consider the therapeutic possibilities for arthroscopy, and Watanabe began to experiment with different procedures. This included using a punch biopsy (1950), excision of a giant cell tumor (1955), and removal of a loose body (1961).[7] Perhaps most significantly, in 1962 the first arthroscopic partial meniscectomy was performed on a 17-year-old male following a basketball injury.[8]
Following on from Takagi’s early explorations of arthroscopy, Watanabe had continued to develop their arthroscopes, leading to the first production arthroscope being manufactured in 1959. This was the No. 21 [Figure 7], which offered both direct and side viewing telescopes, had a 6 mm sheath encompassing the scope and the tungsten light bulb carrier.[9,10] It really had amazing optics; a wide field of vision, 100° in air and 88° in water, and a focal length from 1 mm to infinity. Watanabe described this as being as if “a human eye has been placed there.”
- The Watanabe No. 21 was the first production arthroscope and had optics that brought its field of view close to that of the human eye. Courtesy Gary Poehling.
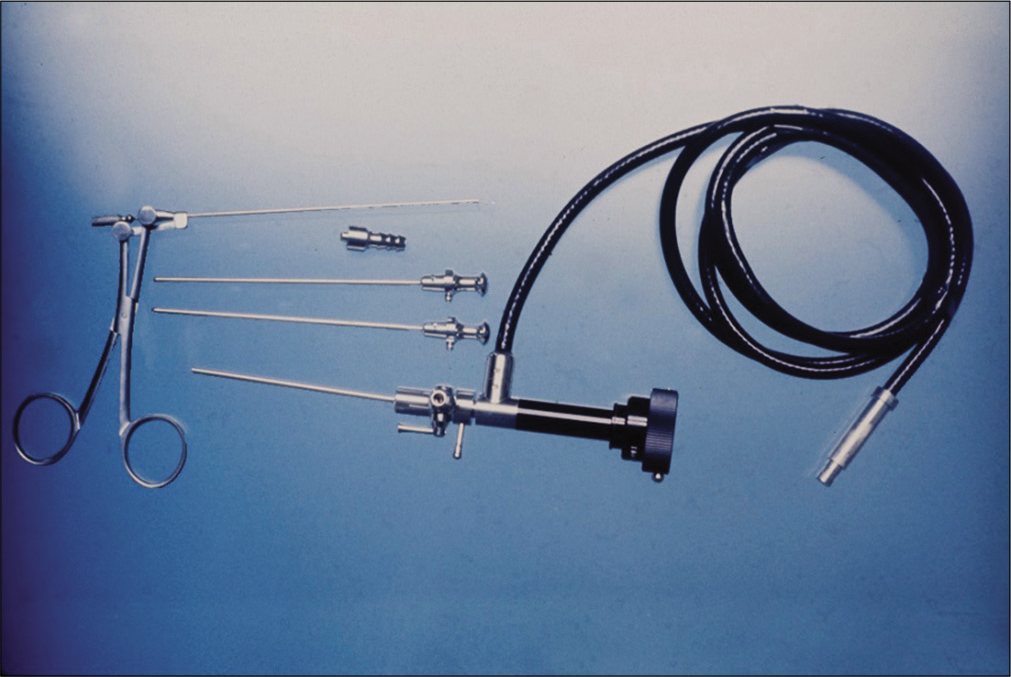
REFINEMENT OF SMALL JOINT ARTHROSCOPY
Arthroscopy was not commonly used in small joints initially as the scopes were large and fragile. In the early 1970s, advances allowed smaller diameter arthroscopes.[9] Early endoscopes were modeled on telescopes, with glass lenses separated by air [Figure 8] Hopkins developed the rod lens, which were thicker and larger.[11] However, the rod lens also allowed significantly more light to be transmitted and were more robust, meaning that miniaturization was possible. While the 2.7 mm No. 11 arthroscope was small enough to be utilized in the wrist joint, it did not focus well.[12] The second key development that allowed small joint arthroscopy to flourish was a fiber-optic lighting system, starting with the Selfoc technology developed by the Nippon Sheet Glass Company (Japan). These systems allowed small scopes to focus clearly with a wide viewing angle.[12]
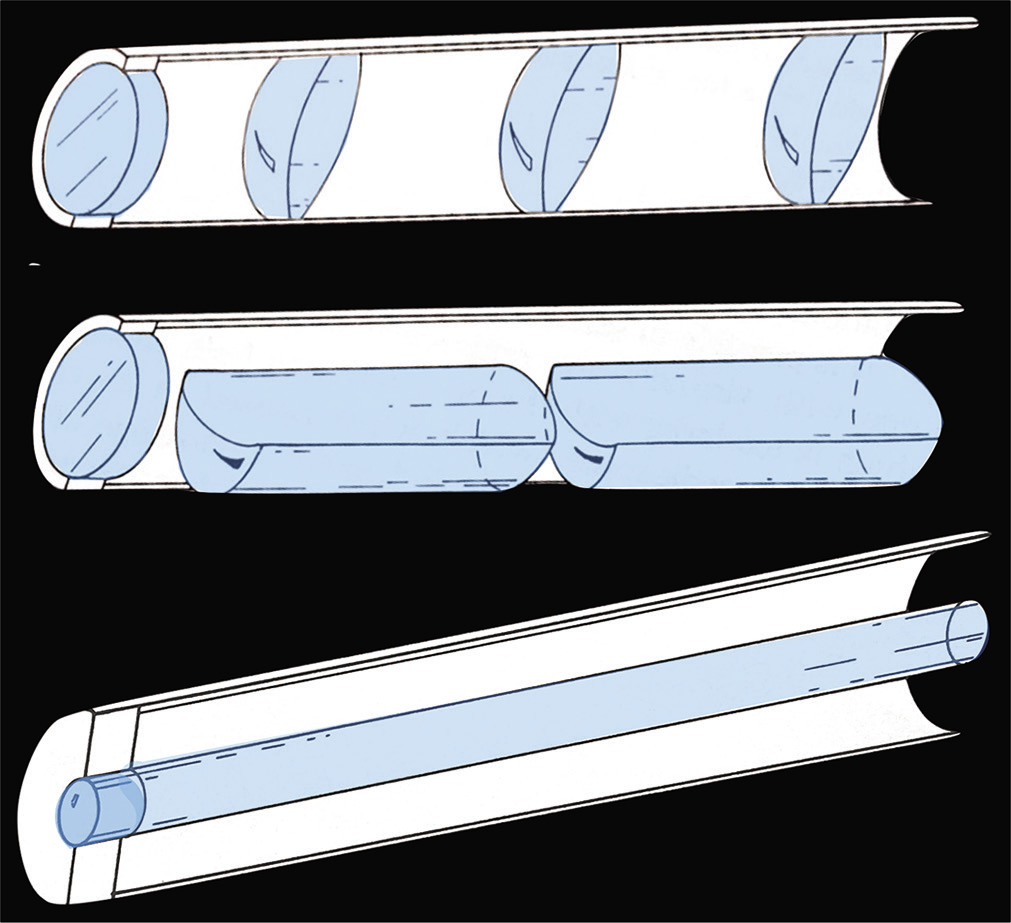
- Early lenses were based on telescopes, with convex lens separated by air. The development of the rod lens allowed more light to be transmitted through a thinner diameter, enabling miniaturization of scopes for use in small joints. Adapted from Arthroscopic surgery: Principles and practice, 3rd edition, Johnson LL, p. 1481, Copyright 1986, with permission from The C.V. Mosby Company.
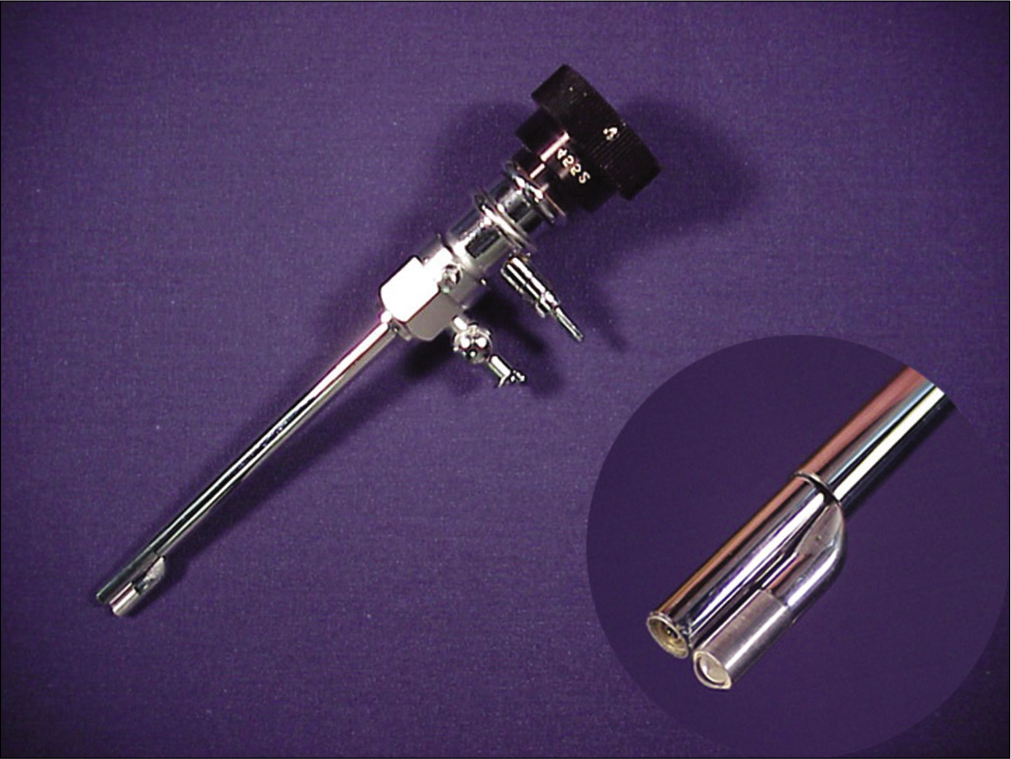
In 1970, the 1.7 mm No. 24 arthroscope was developed, which took advantage of the Selfoc system, allowing a wide angle of vision and clear focus utilizing a small diameter. Initially, the No. 24 was 1.7 mm in diameter, with a viewing angle of 55–70°. Watanabe used this scope to examine 21 wrists in 1970–1972. By 1978, the No. 24 was available in four different sizes, from 1.7 mm to 3.2 mm, as well as a direct viewing and fore-oblique design [Figure 9].[9] The No. 24 arthroscope was also referred to as the Selfoc scope highlighting its technological advancement, and in the USA it was marketed under the name Needlescope by Dyonics.
![A diagram from the third edition of the Atlas of Arthroscopy showing the viewing arc of the direct and fore- oblique options of the No. 24 Arthroscope. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., Present State of Arthroscopy, p. 29, Copyright 1979, with permission from Springer.[2]](/content/115/2020/1/1/img/JASSM-1-044-g009.png)
- A diagram from the third edition of the Atlas of Arthroscopy showing the viewing arc of the direct and fore- oblique options of the No. 24 Arthroscope. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., Present State of Arthroscopy, p. 29, Copyright 1979, with permission from Springer.[2]
The No. 24 scope had a long, thin lens 134 mm long by 1 mm. This rod lens was crucial for the development of small joint arthroscopy, but was also brittle and had a real propensity to break. The initial scope had an inverted image. The development of the Amici prism (two prisms in series) allowed the image to be corrected [Figure 10].[11]
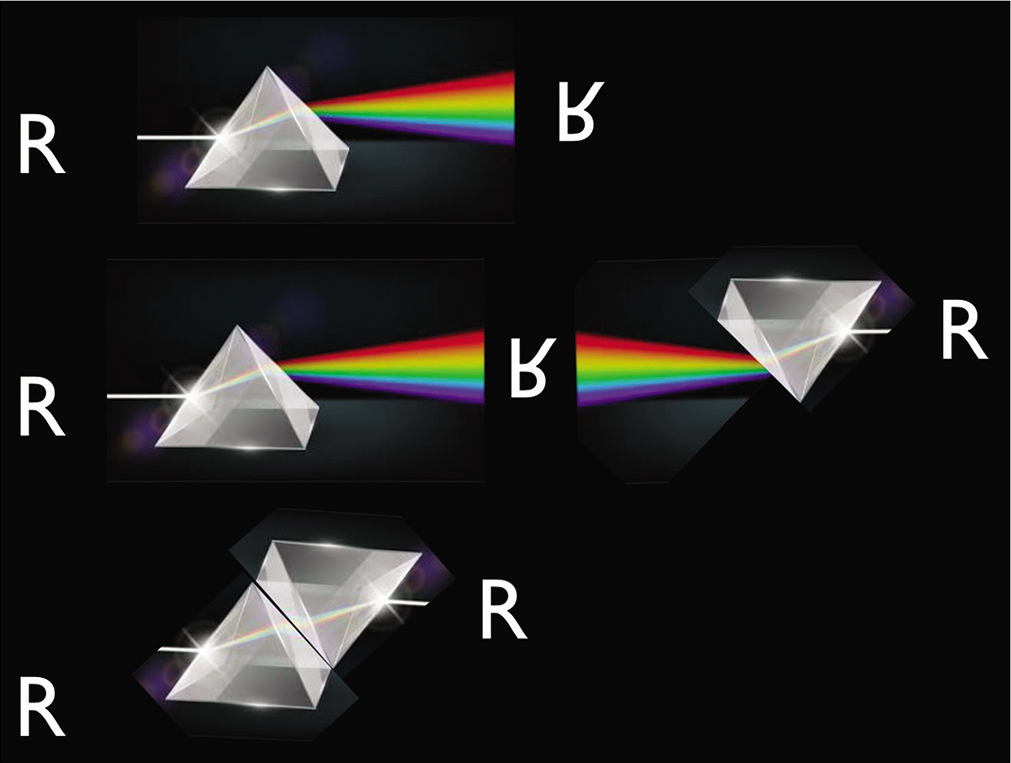
- The Amici Prism was a key development, as it allowed the image transmitted by the lens to be oriented correctly. The two prisms in series flipped the image, corrected the inverted image from early scopes. Copyright Gregory Bain.
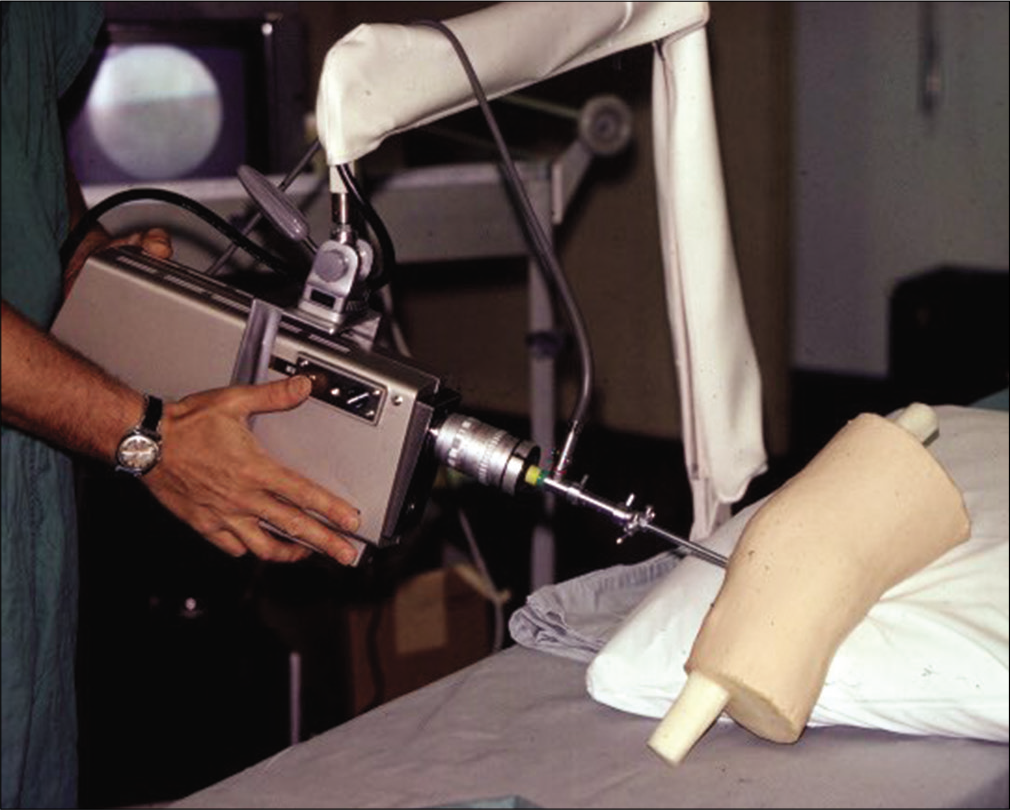
- An early camera, shown in use with a knee arthroscopy teaching model (1975). Courtesy Gary Poehling.
While the diameter of the scopes themselves had become small enough to use in the wrist joint, the size of the camera remained an issue. The early cameras were cumbersome to use, and placed significant stress on the arthroscope due to their weight and size [Figure 11]. The size quickly progressed from the size of a bread box, down to the size of a fist [Video 1]. The smaller chip cameras were much more maneuverable and therefore opened new possibilities for arthroscopy in small joints [Figure 12].[13] Recently the arthrex nanoscope has been developed, which has the camera in the tip of the scope, placing the camera inside the patient. There is a cable from the camera to the monitor, which can be manipulated or bent, and so is much less likely to be damaged.
![A smaller “chip” camera, demonstrated by James Roth.[35] Copyright James Roth. Reprinted from The Wrist and its Disorders, 3rd edition, Roth JH, Whipple TL. Wrist arthroscopy, p. 108–28, Copyright 1988, with permission from W. B. Saunders Company.](/content/115/2020/1/1/img/JASSM-1-044-g012.png)
- A smaller “chip” camera, demonstrated by James Roth.[35] Copyright James Roth. Reprinted from The Wrist and its Disorders, 3rd edition, Roth JH, Whipple TL. Wrist arthroscopy, p. 108–28, Copyright 1988, with permission from W. B. Saunders Company.
Video 1:
Video 1: Terry Whipple explains how the improvements in camera technology allowed greater possibilities for wrist arthroscopy. Courtesy Gregory Bain (https://dx.doi.org/10.25259/JASSM_29_2020).The initial scopes were soaked in a chemical sterilizer. Some camera/light systems were placed in sterilized plastic sleeves. Chen (Japan) described the use of formalin gas chambers for sterilization of his scopes.[14] The scopes used today are developed to withstand the heat and pressure of repeated autoclave sterilization. Single use arthroscopes are now being developed.
EARLY WRIST ARTHROSCOPY
In Watanabe’s early attempts at wrist arthroscopy, he utilized the No. 24 arthroscope.[2] He developed dorsal approaches on the ulnar side of the extensor pollicis longus tendon to access the radiocarpal joint[2] [Figure 13]. Watanabe reported on wrist arthroscopies (67 cases), including visualization of the distal radioulnar joint. He also included thumb carpometacarpal joint, metacarpophalangeal joints (39), and interphalangeal joint arthroscopies (9).[2]
![Image of Watanabe’s wrist arthroscopy portals from the third edition of Masaki Watanabe’s book – Atlas of Arthroscopy (1979).[2] Copyright Masaki Watanabe. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., Arthroscopy of Joints other than Knee, p. 140, Copyright 1979, with permission from Springer.[2]](/content/115/2020/1/1/img/JASSM-1-044-g013.png)
- Image of Watanabe’s wrist arthroscopy portals from the third edition of Masaki Watanabe’s book – Atlas of Arthroscopy (1979).[2] Copyright Masaki Watanabe. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe et al., Arthroscopy of Joints other than Knee, p. 140, Copyright 1979, with permission from Springer.[2]
In 1979, Chen published his findings of over 90 small joint arthroscopic procedures of the wrist and hand, which heralded the beginning of clinical wrist arthroscopy.[14] Chen acknowledges Watanabe, and used similar dorsal portals between the EPL and EDC, or between EDC and EDM [Figure 14]. These were termed the dorsoradial and dorsoulnar portals.
![Chen (Japan) published a series of clinical and cadaveric small joint arthroscopy in 1979, utilizing similar portals to Watanabe.[14] He acknowledged learning the techniques from Watanabe. Reprinted from Arthroscopy of the Wrist and Finger Joints, Vol 10, Chen YC, Orthopedics Clinic of North America, p. 723–33, Copyright 1979 with permission from W. B. Saunders Company. APL: Abductor pollicis longus; ECR: Extensor carpi radialis longus and brevis; ECU: Extensor carpi ulnaris; EDC: Extensor digitorum communis; EPB: Extensor pollicis brevis; EPL: Extensor pollicis longus.](/content/115/2020/1/1/img/JASSM-1-044-g014.png)
- Chen (Japan) published a series of clinical and cadaveric small joint arthroscopy in 1979, utilizing similar portals to Watanabe.[14] He acknowledged learning the techniques from Watanabe. Reprinted from Arthroscopy of the Wrist and Finger Joints, Vol 10, Chen YC, Orthopedics Clinic of North America, p. 723–33, Copyright 1979 with permission from W. B. Saunders Company. APL: Abductor pollicis longus; ECR: Extensor carpi radialis longus and brevis; ECU: Extensor carpi ulnaris; EDC: Extensor digitorum communis; EPB: Extensor pollicis brevis; EPL: Extensor pollicis longus.
In 1981, Lanny Johnson (USA) published an extensive textbook on arthroscopy.[15] It included his early experiments with wrist arthroscopy, using a needlescope. His descriptions demonstrated that there was a distinct lack of standardization in approaches to the wrist at this time. He attempted to access the wrist through the anatomic snuffbox [Figure 15]; however, it is not clear how successful this was. Johnson also noted a 1978 survey of American Academy of orthopedic surgeons members, which found that only 6% had utilized arthroscopy for joints other than the knee (50% had performed knee arthroscopy).
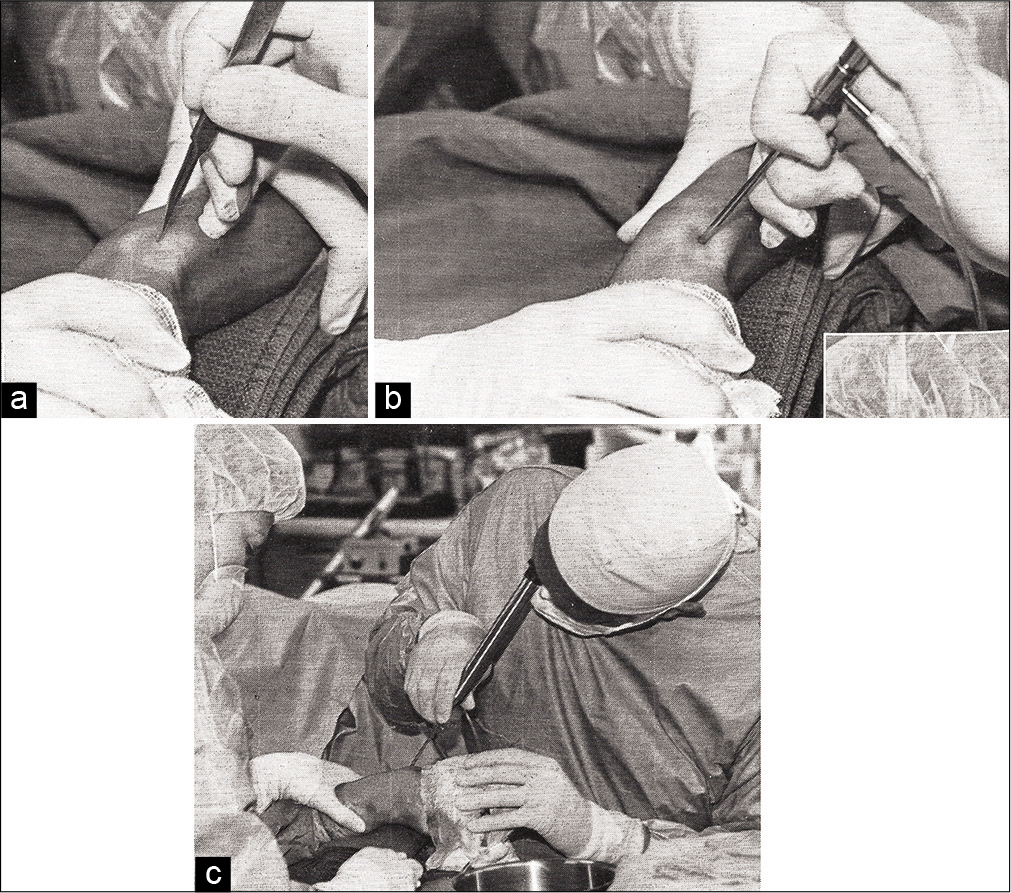
- (a) Lanny Johnson published major text books on arthroscopy. He used a “laceration of the skin only, avoiding superficial branch of the radial nerve” to enter the radio-ulnar joint through the snuff box to assess the wrist. (b) Another image from Lanny Johnson’s arthroscopy textbook, showing his technique to insert a Needlescope into the radioulnar joint. Reproduced from Lanny Johnson. (c) Lanny Johnson using a needlescope to view the distal radioulnar joint. Reproduced from Lanny Johnson. Copyright Lanny Johnson. Reprinted from Arthroscopic surgery: Principles and practice, 3rd edition, Johnson LL, p. 1481, Copyright 1986, with permission from The C.V. Mosby Company.
A MATCH WAS STRUCK
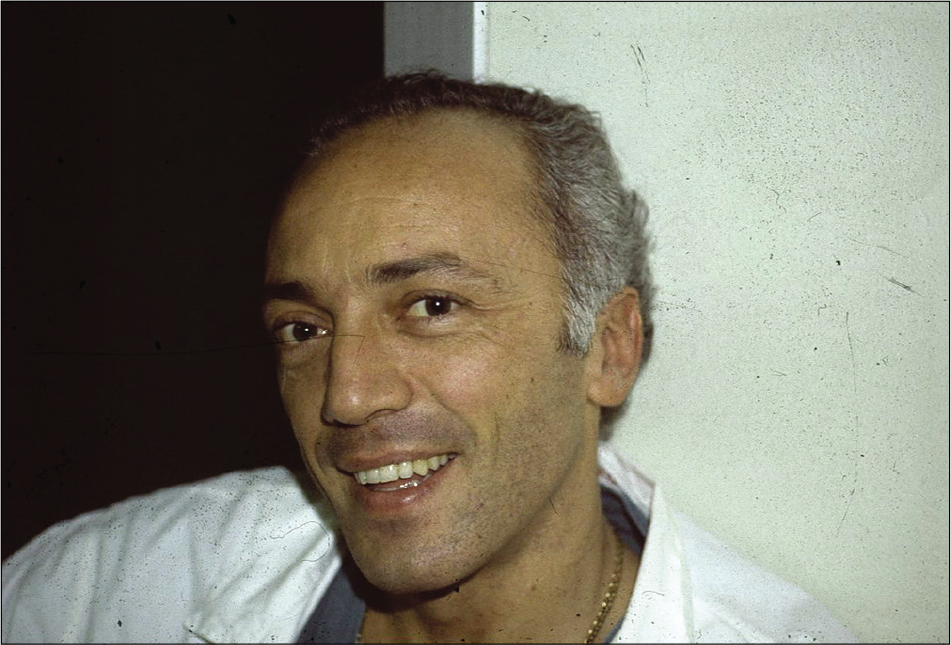
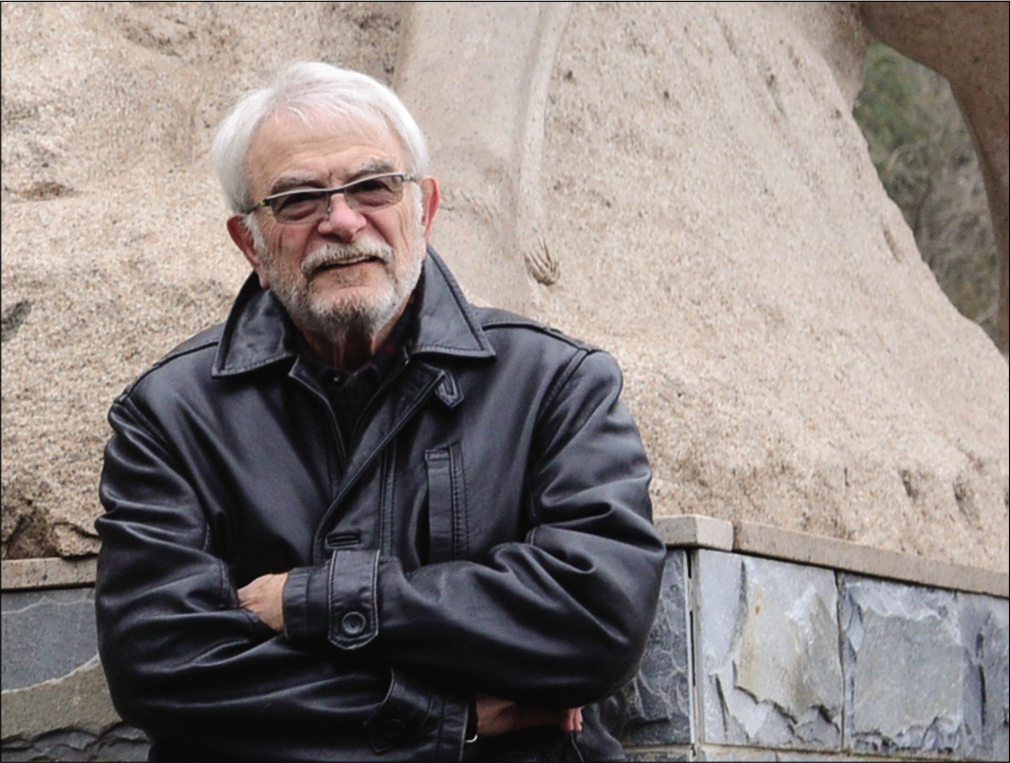
Interesting insights into the early development are provided by Terry Whipple and Gary Poehling (USA). In 1972, American surgeon Captain Poehling was posted to Japan as part of his military medical duty [Figure 16]. Before his departure, he asked his department director, Leonard Goldner [Figure 17], if there was anything he would like to have him bring back. Goldner replied “A Watanabe No. 26 please.” He subsequently purchased the 1.9 mm arthroscope from Watanabe [Figure 18]. When Poehling returned in 1972 with the arthroscope, he was appointed head of arthroscopy, while only being a junior resident! [Video 2]. Unfortunately, Poehling only succeeded in completing half of the first case, before the fragile scope broke. In 1975, Poehling moved to Winston-Salem, and handed the arthroscopy mantle to 1st year resident Whipple.

- Captain Gary Poehling during his Air Force service in the Japan in 1970–1972. Courtesy Gary Poehling.
- Leonard Goldner (USA) was an important mentor to Gary Poehling and Terry Whipple. On his return from service in Japan, Goldner appointed Poehling to be the Director of Arthroscopy. When Poehling left, Whipple was appointed to this position. Courtesy Gary Poehling.
- A Watanabe No. 26 Arthroscope, the same model Gary Poehling purchased and brought back to the United States of America in 1972. Courtesy Gary Poehling.
Whipple describes that he was fortunate to have worked for sports orthopedic surgeon Frank Bassett [Figure 19] in 1976–1977, who allowed him to insert the arthroscope into the knee joint before performing an open meniscectomy. Whipple also performed arthroscopies on cadaveric knees. Both of these opportunities enabled him to develop a better understanding of knee anatomy and principles of arthroscopy, specifically for accessing regions of the joint from two coordinated portal vantages simultaneously.[16] Despite this initial insight, there were where still struggles and barriers to bringing these concepts into clinical practice.

- Frank Bassett (USA) was a sports orthopedic surgeon who allowed Terry Whipple to practice arthroscopic techniques in the knee before open procedures in 1976–1977. Image courtesy of Dukes Athletics.
In early 1985, Whipple enlisted a sports medicine fellow, Jack Powell (USA), to help develop a safe approach to wrist arthroscopy [Video 3]. The proximity of the tendons, nerves, and vessels that traverse the wrist joint make arthroscopic access to the joint difficult and potentially dangerous. Powell and Whipple undertook cadaveric studies to define the optimal wrist arthroscopy portals, and named them according to the extensor compartments of the wrist [Figure 20]. The portals for the radiocarpal, midcarpal, and distal radioulnar joints were all described.[17] Whipple also developed the traction tower and Chinese finger traps to enable joint distraction. Together these developments provided a method and terminology for the description of safe and reliable portals that could be widely and safely used. These concepts remain valid to this day, 35 years later!
![(a) This diagram is from Whipple’s 1986 paper on wrist arthroscopy techniques, showing the portals which are still utilized today.[17] Courtesy Terry Whipple. (b) This dissection of the dorsal aspect of the wrist visualizes Whipple and Powell’s wrist arthroscopy portals as they relate to the extensor compartments of the wrist. Courtesy Terry Whipple. Each extensor compartment is numbered (1-6). DRUJ: Distal radioulnar joint; ECU: Extensor carpi ulnaris; MC: Mid-carpal.](/content/115/2020/1/1/img/JASSM-1-044-g020.png)
- (a) This diagram is from Whipple’s 1986 paper on wrist arthroscopy techniques, showing the portals which are still utilized today.[17] Courtesy Terry Whipple. (b) This dissection of the dorsal aspect of the wrist visualizes Whipple and Powell’s wrist arthroscopy portals as they relate to the extensor compartments of the wrist. Courtesy Terry Whipple. Each extensor compartment is numbered (1-6). DRUJ: Distal radioulnar joint; ECU: Extensor carpi ulnaris; MC: Mid-carpal.
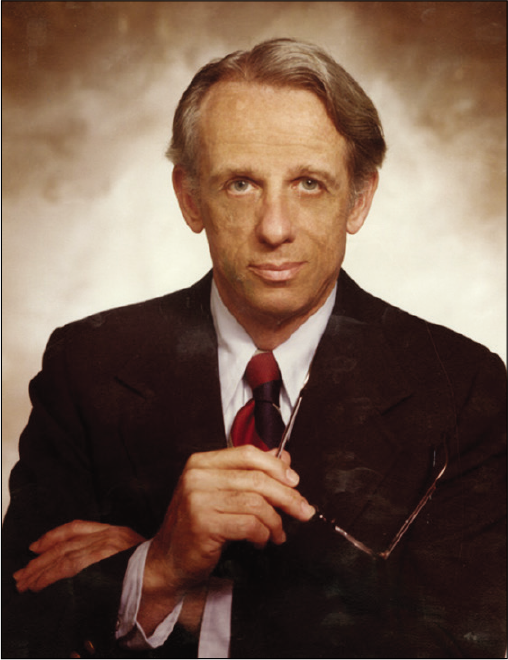
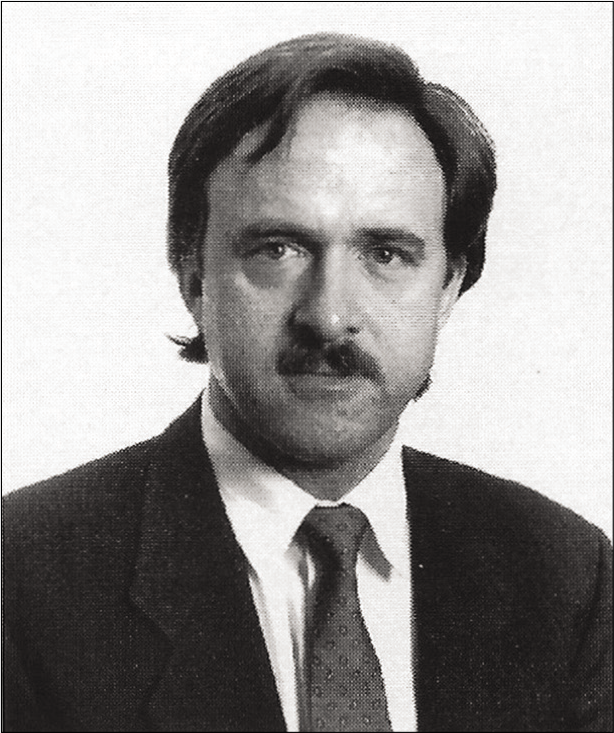
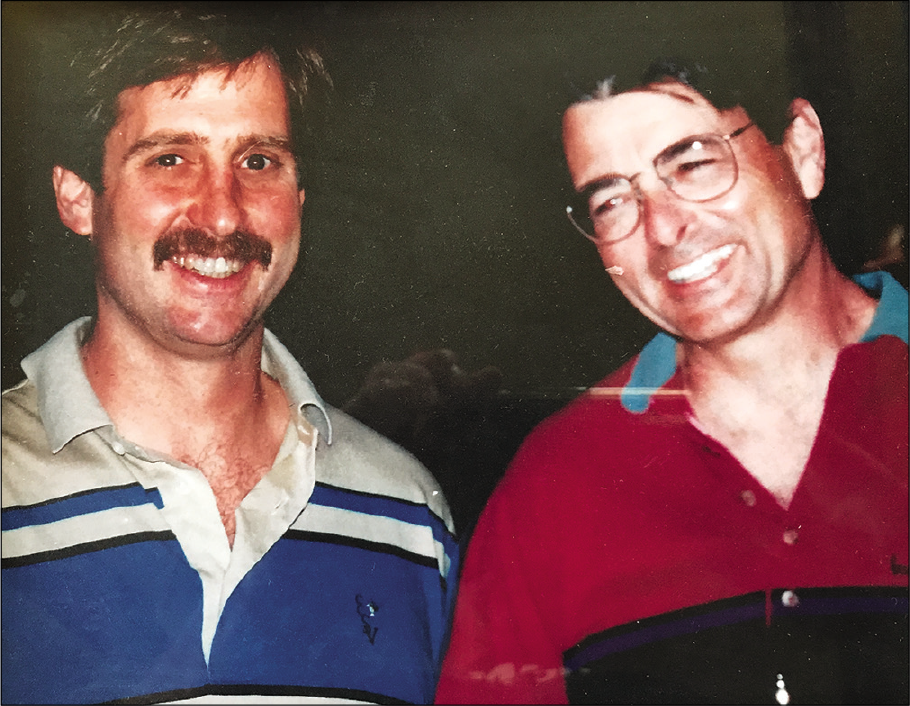
In May 1985, Whipple [Figure 21], Poehling, and James Roth from the University of Western Ontario, Canada [Figure 22], met at the International Society of the Knee meeting, and had a dinner at the Winkler Hotel in Salzburg, Austria [Figure 23]. They realized that they each had an interest in hand surgery and also arthroscopy. It was there that they developed their plan to evolve wrist arthroscopy and introduce it to the surgeons of North America. They considered there were three major components required: Whipple developed a shorter arthroscope, miniaturized surgical instruments and a teaching model [Figure 24], Poehling organized a cadaveric laboratory course for noted American wrist surgeons, and Roth wrote a paper about wrist arthroscopy [Video 4].
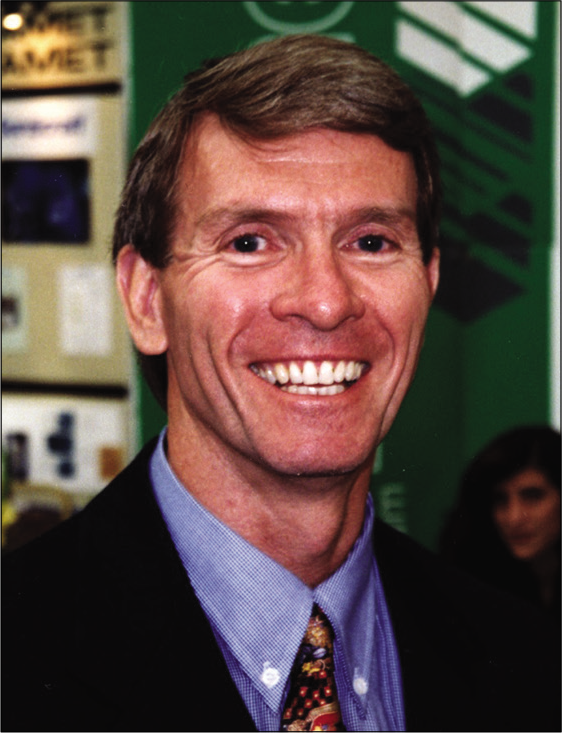
- Terry Whipple performed cadaveric dissections to create the named extensor compartment portals we use today. He developed the traction tower and finger traps. These aspects allowed wrist arthroscopy to become safe and standardized.

- James Roth (Canada) operating with Sports Orthopedic Surgeon Peter Fowler (right), who became Foundation President of ISAKOS. Courtesy Graham King.

- Terry Whipple, Gary Poehling and James Roth at the Winkler Hotel in Salzburg, Austria during the 1985 International Knee Association meeting. All three were interested in hand and wrist surgery. They agreed on a strategy to introduce wrist arthroscopy to the USA: Whipple would develop a teaching model, Poehling organized a course, and Roth wrote a paper. Courtesy Gary Poehling.

- Whipple’s teaching model allowed him to demonstrate techniques for wrist arthroscopy in a controlled and repeatable environment. It was also hugely beneficial in planning procedures, as the maneuvers required could be rehearsed until perfected before undertaking the procedure. Courtesy Terry Whipple.
In 1986, the first wrist arthroscopy course took place in Winston-Salem, North Carolina, USA [Figure 25]. Whipple, Poehling and Roth wanted to avoid the acrimony and resistance that had earlier marred the introduction of knee arthroscopy to the USA [Video 5]. It was clear that inviting the most accomplished hand surgeons of the period would be important in garnering widespread acceptance of their new technique. They discussed this with mentor, James Urbaniak (USA) [Figure 26], (President of the American Society for Surgery of the Hand [ASSH]), who helped create the list of eminent wrist surgeons, and then personally invited them to attend [Video 6]. A total of 57 were invited, of which 47 attended, including 10 former ASSH presidents.
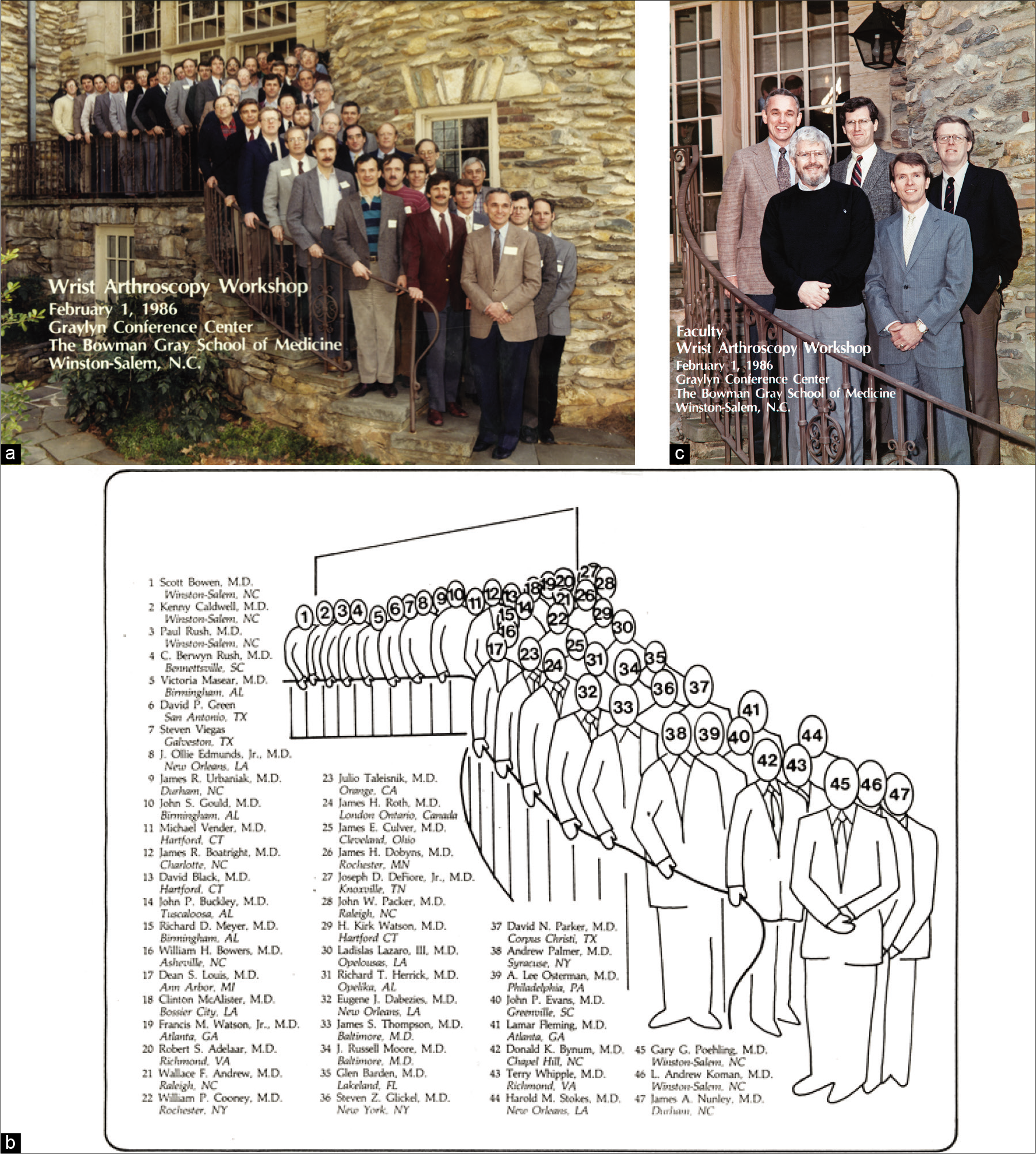
- (a-c) Attendees at the first wrist arthroscopy workshop at the Bowman Gray School of Medicine, Winston Salem, USA 1986. This was the start of the new era, which enabled wrist arthroscopy to be promoted and developed in an organized way. (a) Photograph, (b) diagram of names of attendees, (c) the faculty. Courtesy Gary Poehling.

- James Urbaniak (USA) assisted in the smooth introduction of wrist arthroscopy in the USA. He invited 57 senior surgeons, including 10 Presidents of the American Society of Surgery of the Hand. Of these 47 surgeons attended. Courtesy Gary Poehling.
During this meeting, the young Whipple provided a demonstration of how to perform arthroscopy. Having completed the demonstration, including how to assess the triangular fibrocartilage (TFC). Senior surgeon, Bill Bowers, an acknowledged leader in anatomy and surgical techniques[18] asked “How do you know that the TFC is intact.” Whipple spritely suggested that he could palpate the TFC, and if need be, arthroscope the distal radio-ulnar joint. Having never performed DRUJ arthroscopy, he proceeded to do so. As history will indicate, he introduced the scope that enabled all to see the internal anatomy. Bowers subsequently replied that he had learnt more about the wrist joint anatomy from the arthroscopic demonstration, than he had learnt from years of detailed cadaveric dissections.
As part of this same meeting, Whipple prepared a video presentation of wrist arthroscopy techniques. This included the cadaveric dissections, description of the portals, diagnostic arthroscopy, and use of an arthroscopy tower and finger traps. Basic techniques were demonstrated including synovectomy, TFC debridement, and removal of loose bodies. However, it also included advanced techniques such as: Reduction and fixation of distal radius fractures, stabilization of scapholunate instability with multiple Kirschner wires – the arthrofibrosis technique – and fixation of scaphoid fractures with the Herbert Whipple cannulated headless screw. It was a master class, in 1986, and again remains relevant to this day [Video 7]!
This clear demonstration, of basic and advanced techniques, to the leaders of hand surgery was strategically brilliant. Many of the senior hand surgeons probably never performed wrist arthroscopy themselves, but most importantly they encouraged their junior colleagues to embrace this new phenomenon [Figure 27]. Some of the other younger surgeons who attended subsequently made their own contributions, including Cooney et al.,[19] Osterman and Raphael [Figure 28],[20-23] Palmer,[24,25] Viegas and Ballantyne, Viegas[26-29] [Figure 29], and Nagle [Figure 30].[30,31]

- Leonard Goldner (USA, center bottom) performs his first wrist arthroscopy at the first Wrist Course in 1986. A young Bill Cooney (center top) and Andy Koman (right) look on. Both later made significant contributions to the development of wrist arthroscopy. Courtesy Gary Poehling.
- Lee Osterman (USA) made many contributions to wrist arthroscopy. He developed techniques for dorsal wrist ganglion excision, triangular fibrocartilage injuries, distal radius fractures, and carpal instability. He has also been one of the great teachers. Reprinted from Atlas of the Hand Clinics, Vol 11, Osterman L, Foreward, p. ii-iv, Copyright 2006 with permission from W. B. Saunders Company.

- Dan Nagle (USA) was involved in the development of the clinical application of lasers in wrist arthroscopy. Courtesy Daniel Nagle.
BROADENING THE POSSIBILITIES
The initial clinical use of wrist arthroscopy followed the early era of knee arthroscopy, focusing on the diagnostic possibilities. With increasing experience, and more durable, smaller scopes, more therapeutic applications became possible. The miniaturization of instruments was a key step in allowing therapeutic wrist arthroscopy.[32]
As the clinical applications of wrist arthroscopy broadened, there became a need to compare its efficacy against other modalities. In 1986, Roth and Richard Haddad compared wrist arthroscopy to arthrography in the diagnosis of ulnar wrist pain.[33] The arthroscopy was superior to arthrography for identifying TFC tears. This was an award-winning paper that helped wrist arthroscopy be considered the “gold standard for diagnosis.”[34]
In 1988, Roth wrote on the interest in developing arthroscopic surgery for the wrist, following on from its successful use in the knee, shoulder, and ankle. He aimed to reduce the rate of arthrotomy, which was associated with a poor prognosis.[35] Roth also described a number of therapeutic arthroscopic procedures in 1988. Central excisions of unstable TFC tears, synovectomy, and loose body removal were all undertaken.[36] They were exciting days for wrist arthroscopy. Problems such as ulnar sided wrist pain would now be debrided with hand held instruments. He later reported on the “-ectomy” procedures, which were arthroscopic excisions within the wrist.[37] It included proximal row carpectomy.
Furthermore, in 1988, Whipple outlined the use of powered instruments for wrist arthroscopy.[38] The use of such instruments was already well described in the knee and shoulder. The benefits conferred by powered instruments, such as faster tissue resection, and a built-in suction-aspiration system could now be utilized for wrist arthroscopy. Not all powered instruments could be successfully miniaturized due to the limitations posed by the smaller diameter of wrist arthroscopes.
In 1992, Whipple published the first textbook dedicated to wrist arthroscopy, “Arthroscopic Surgery: The Wrist” [Figure 31]. In this publication, Whipple clearly described the principles and practice of wrist arthroscopy, supported with good imaging and photos. The book also outlines therapeutic roles for arthroscopy with intra-articular synovectomy, arthroscopic assisted reduction and fixation of distal radius fractures and many more procedures.[12] The book sold out.
![Terry Whipple and his 1992 textbook, “Arthroscopic Surgery: The Wrist.” It was the first text book on wrist arthroscopy. It sold out![12] Courtesy Gregory Bain.](/content/115/2020/1/1/img/JASSM-1-044-g031.png)
- Terry Whipple and his 1992 textbook, “Arthroscopic Surgery: The Wrist.” It was the first text book on wrist arthroscopy. It sold out![12] Courtesy Gregory Bain.
There were advances made in the understanding of anatomy by Viegas and Ballantyne, Viegas[26-29] and Richard (Dick) Berger[39-41] [Figure 32]. In 1995, the use of arthroscopy in joints other than the midcarpal, radiocarpal, and DRUJ had begun in earnest, including the use within the soft-tissue compartments of the forearm.[42] Increasing use of the arthroscope for therapeutic means within the wrist was also expected at this stage. Randall Culp (USA) [Figure 33] described a technique for arthroscopic proximal row carpectomy and highlighted the importance of complications.[43,44]
![Randall Culp “Randy” (USA) worked with Lee Osterman, and developed many new techniques. He also contributed to our knowledge of complications.[44] Reproduced from Hand Clinics. W. B. Saunders Company.](/content/115/2020/1/1/img/JASSM-1-044-g033.png)
- Randall Culp “Randy” (USA) worked with Lee Osterman, and developed many new techniques. He also contributed to our knowledge of complications.[44] Reproduced from Hand Clinics. W. B. Saunders Company.
Osterman developed many arthroscopic techniques, including resection of dorsal wrist ganglion in 1995,[23] and further reported a detailed technique in 2003.[45] Other contributions include technique for debridement of TFC injuries,[20] arthroscopic reduction and internal fixation of distal radius fractures,[21] evaluation and treatment of carpal instability,[22] and techniques for proximal row carpectomy.[43]
In 1993, Guillaume Herzberg (France) [Figure 34] published a landmark review of 157 perilunate dislocations.[46] 20 years later, Herzberg described the concept of perilunate injury, not dislocated (PLIND), and demonstrated the value of wrist arthroscopy in ensuring accurate early diagnosis of such injuries.[47]
Mathoulin (France) [Figure 35] described a case series of arthroscopic reduction and fixation of intra-articular distal radius fractures, a procedure that had been discussed throughout the 1990s.[48] Mathoulin has also evolved the concepts of the anatomy of the scapholunate interval, the EWAS classification of scapholunate instability and techniques for scapholunate capsulodesis.[49-52] However, clearly his biggest contribution was in establishing and developing EWAS, which built a platform, to take wrist arthroscopy to the world.[53,54]

- Christophe Mathoulin (France) as a guest speaker at the 3rd Italian Wrist Course, 2003. He has played a significant role in creating the European Wrist Arthroscopy Society, which has run courses all over the world. EWAS evolved into the International Wrist Arthroscopy Society in 2019. Courtesy Riccardo Luchetti.
Joe Slade (USA) [Figure 36] described the arthroscopic reduction and percutaneous fixation of scaphoid fractures in 2001 using a dorsal approach.[55,56] In the early 2000s, Wong and Ho (Hong Kong) [Figure 37] outlined procedures for scaphoid fractures,[57] limited wrist fusion,[58] and volar ganglion resection.[59] In 2001, Luchetti et al. (Italy) [Figure 38] reported on arthroscopic wrist arthrolysis for post-traumatic and post-surgical wrist stiffness.[60]
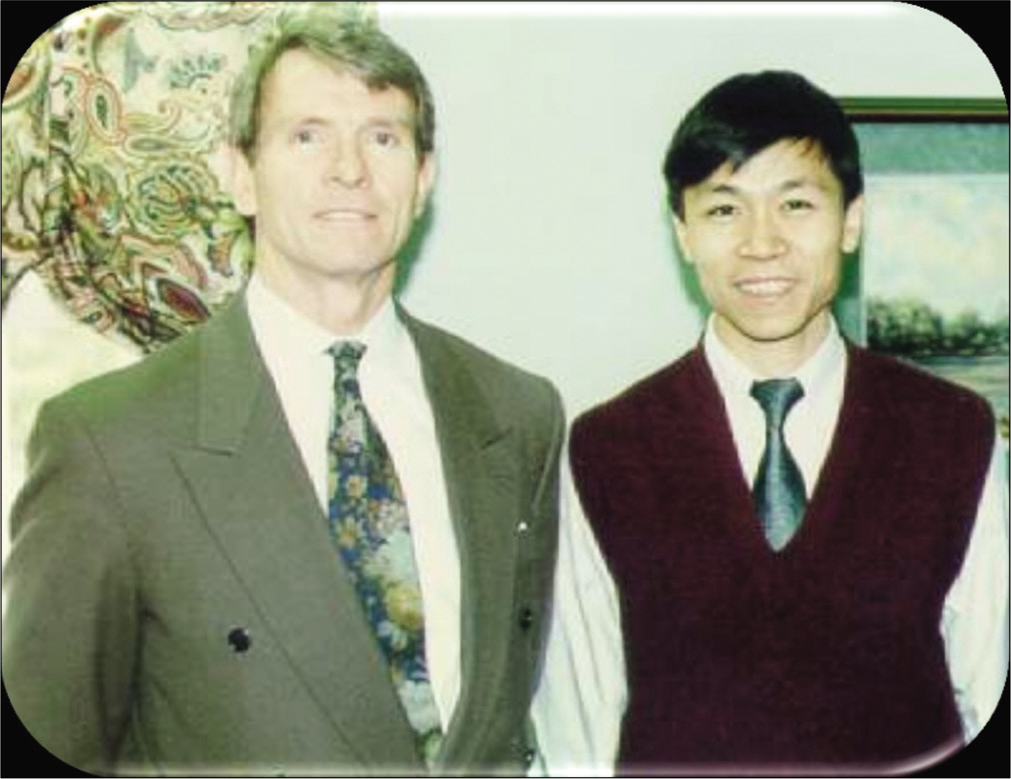
- PC Ho visited Terry Whipple in 1996 to learn more about wrist arthroscopy. A couple of years later, PC Ho started the Hong Kong wrist arthroscopy course. Courtesy Terry Whipple.
- Riccardo Luchetti was important in the evolution of wrist arthroscopy in Italy and Europe. Courtesy Riccardo Luchetti.
In 2006, Greg Bain (Australia) [Figure 39] developed an approach to arthroscopic assessment and management of Kienbock’s disease. This was very different to Lichtman’s radiological classification [Figure 40], but yet complimented it.[61] Bain made other contributions including the in-side out volar portal, management of intra-osseous ganglions, and ulnar styloid impaction.[62-68]

- Greg Bain (Australia) and PC Ho at the Hong Kong Hand Society meeting in 1995. Courtesy PC Ho.
- David Lichtman (USA) has contributed significantly to many conditions of the wrist, including Kienbock’s disease and carpal mechanics. Courtesy PC Ho.
In many other fields of endoscopic surgery, fluid is not necessary for distention of the joint. While fluid was considered essential for many years for wrist arthroscopy, Francisco (Paco) del Piñal et al. [Figure 41] described a technique for dry arthroscopy in 2007.[69] The dry arthroscopy compliments his other contributions, of management of distal radius fractures and malunions.[70] In addition, Piñal has made contributions with his EWAS text books on wrist arthroscopy (distal radius fractures and ulnar sided pain) and redefined our understanding of chronic regional pain syndrome (CRPS).[71-73]
![Francisco (Paco) del Piñal (Spain) has played an important role in the development of dry arthroscopy,[69,70] management of distal radius fractures and malunions. Recently he has changed our understanding of CRPS.[71-73] He has also contributed with quality EWAS arthroscopic texts. Courtesy Dr Paco del Piñal.](/content/115/2020/1/1/img/JASSM-1-044-g041.png)
- Francisco (Paco) del Piñal (Spain) has played an important role in the development of dry arthroscopy,[69,70] management of distal radius fractures and malunions. Recently he has changed our understanding of CRPS.[71-73] He has also contributed with quality EWAS arthroscopic texts. Courtesy Dr Paco del Piñal.
The development of our understanding and management of TFC tears has been developed with important contributions including Palmer’s classification of TFC tears,[24] Poehling’s inside-out suture technique, Andrea Atzei (Italy) [Figure 42], and Luchetti’s TFC tear classification[74] and Toshi Nakamura’s (Japan) [Figure 43] anatomical and clinical studies.[75] Jan-Ragnar Haugstvedt (Norway) developed techniques for the TFC tears and lunotriquetral tears [Figure 44].[76-78]

- Andrea Atzei (Italy) has worked alongside Ricardo Luchetti in Italy to create the Wrist Group of the Italian Society for Surgery of the Hand. He has also contributed to our knowledge of triangular fibrocartilage injuries, and wrist arthrolysis. Courtesy Ricardo Luchetti.

- Toshi Nakamura (Japan) has contributed to our knowledge of Triangular Fibrocartilage injuries. He was President of EWAS in 2011–2012 and is the current editor of the Journal of Wrist Surgery. Courtesy PC Ho.
The development of our understanding and management of scapholunate instability have included important contributions such as Whipple’s arthrofibrosis technique,[79] William Geissler’s (USA) [Figure 45] 1996 arthroscopy classification of scapholunate instability,[80] Tommy Lindau’s (Sweden) [Figure 46] study of the natural history of TFC and scapholunate ligament tears with distal radius fractures,[81] and more recently Mathoulin’s technique of scapholunate tenodesis.[49] Other important contributions have been made by Marc Garcia-Elias (Spain) [Figure 47][82,83] and Brunelli and Brunelli (Italy).[84]
![William Geissler (USA) was involved with development of the scapholunate classification and arthroscopic management of sports injuries.[80] Courtesy William Geissler.](/content/115/2020/1/1/img/JASSM-1-044-g045.png)
- William Geissler (USA) was involved with development of the scapholunate classification and arthroscopic management of sports injuries.[80] Courtesy William Geissler.
![Tommy Lindau (Sweden) provided quality long-term prospective studies of ligamentous injuries associated with distal radius fractures.[81] Courtesy PC Ho.](/content/115/2020/1/1/img/JASSM-1-044-g046.png)
- Tommy Lindau (Sweden) provided quality long-term prospective studies of ligamentous injuries associated with distal radius fractures.[81] Courtesy PC Ho.
There have been other areas of the hand and wrist where the arthroscope has been used. The most popular of these is the endoscopic carpal tunnel release. Ichiro Okutsu (Japan) and James Chow (USA) separately described the endoscopic management of carpal tunnel syndrome in 1989.[85,86] In 1992, a single portal technique was described by John Agee (USA) using a pistol grip device with a retractable blade.[87]
The endoscopic treatment of a number of other nerve compression syndromes has also been described including release of Guyon’s canal release, pronator teres syndrome, and radial tunnel syndrome.[88] The most popular of these is endoscopic release of the cubital tunnel as described by Hoffmann and Siemionow (Germany).[89] Other therapeutic endoscopic procedures being developed around the wrist include vessel, nerve, tendon and bone grafts, tendon transfers, fasciotomy, bursectomy, and pisiform excision.[65] Endoscopic surgical releases have also been described for the 1st extensor compartment, compartment syndrome, and intersection syndrome.
There are contributions by so many. Others who have also contributed include Lars Aldofsson (Sweden)[90] [Figure 48], Tyson Cobb (USA) [Figure 49],[91] Alejandro Badia (USA),[92,93] Buddy Savoie (USA) [Figure 50],[80] Weiss et al. [Figure 51],[94] Thurston and Stanley (England),[95] Dan Nagle (USA)[30,31,96] [Figure 30], Slutsky (USA)[96-99] [Figure 52], Peter Jorgsholm (Denmark),[100] and Del Gaudio and Haerle [Figure 53].[101]
![Lars Aldoffsson (Sweden) was an early leader of wrist arthroscopy in the Nordic countries. He developed the concepts of arthroscopic management of synovitis of the wrist.[90] Courtesy PC Ho.](/content/115/2020/1/1/img/JASSM-1-044-g048.png)
- Lars Aldoffsson (Sweden) was an early leader of wrist arthroscopy in the Nordic countries. He developed the concepts of arthroscopic management of synovitis of the wrist.[90] Courtesy PC Ho.

- Tyson Cobb (USA) has been involved with the development of resection arthroplasty for the SLAC wrist and endoscopic procedures. Courtesy Tyson Cobb.
- Felix “Buddy” Savoie (USA, left, with Dr Dick Caspari) has contributed to the understanding of injuries associated with distal radius fractures. Courtesy Buddy Savoie.
![Arnold-Peter Weiss (USA) has contributed to our knowledge of intercarpal ligament injuries.[85] Courtesy Arnold-Peter Weiss.](/content/115/2020/1/1/img/JASSM-1-044-g051.png)
- Arnold-Peter Weiss (USA) has contributed to our knowledge of intercarpal ligament injuries.[85] Courtesy Arnold-Peter Weiss.
![Max Haerle (Germany) has been involved with the development of the vascularized bone grafts and scapholunate instability.[101] He has also been actively involved in the leadership of FESSH, EWAS and IWAS. Courtesy Max Haerle.](/content/115/2020/1/1/img/JASSM-1-044-g053.png)
- Max Haerle (Germany) has been involved with the development of the vascularized bone grafts and scapholunate instability.[101] He has also been actively involved in the leadership of FESSH, EWAS and IWAS. Courtesy Max Haerle.
TIMELINE
1912 – Severin Nordentoft (Denmark) reports arthroscopic examination of the knee joint[5]
1918 – Kenji Takagi (Japan) performs arthroscopy on a TB knee using a 7.3 mm cystoscope[1]
1921 – Eugen Bircher (Switzerland) publishes the first clinical arthroscopy report[3]
1931 – Michael Burman (USA) publishes the first report of wrist arthroscopy[6]
1957 – Masaki Watanabe’s Atlas of Arthroscopy (1st edition) published [Figure 54][102]
1970 – Masaki Watanabe (Japan) releases the 1.9 mm No. 24 Arthroscope, for small joints[9]
1972 – Gary Poehling (USA) purchases No. 26 arthroscope for Leonard Goldner (USA)
1979 – YC Chen (Japan) reports 90 wrist and finger joint arthroscopies, with No. 24 arthroscope[14]
1979 – Stryker chondrotome developed to mechanically resect soft tissue[103]
1984 – Terry Whipple and Jack Powell (USA) Cadaver dissections and development of named safe wrist arthroscopy portals, traction towers, and finger traps[17]
1986 – Gary Poehling, Terry Whipple (USA), and James Roth (Canada) organize the first wrist arthroscopy course in Winston-Salem, USA
1986 – Terry Whipple (USA) published paper on Techniques of Wrist Arthroscopy[17]
1989 – James Chow (USA) describes a technique for endoscopic carpal tunnel release[86]
1990 – Luigi Pederzini and Riccardo Luchetti (Italy) organize first Italian upper limb arthroscopy course, with guest speaker James Roth (Canada) [Figure 55]
1992 – Terry Whipple (USA) publishes first textbook on wrist arthroscopy: “Arthroscopic Surgery – The Wrist” (Lippincott)[12]
1997 – PC Ho (Hong Kong) organizes first Hong Kong Wrist Arthroscopy Course
1999 – Riccardo Luchetti and Andrea Atzei (Italy) create the Wrist Group of the Italian Society for Surgery of the Hand. First meeting in Verona
2005 – Christopher Mathoulin (France) founded the EWAS. First EWAS cadaveric arthroscopy workshop in Strasbourg [Figure 56]
2007 – Francisco del Piñal (Spain) reports dry wrist arthroscopy technique[69]
2012 – David Slutsky (USA) inaugural editor-in-chief, journal of wrist surgery.[104] Toshi Nakamura is the current editor
2015 – PC Ho (Hong Kong), Foundation President of APWA
2019 – EWAS evolves into the IWAS. Terry Whipple and Christophe Mathoulin both made honorary lifetime presidents.[53]
![The first edition of Watanabe’s Atlas of arthroscopy featured hand painted depictions of the view down the arthroscope, as Watanabe believed that the photos were not of adequate quality.[102] In later editions, Watanabe included photos taken through the arthroscope. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe M, Takeda S, Ikeuchi H, History of Arthroscopy, p. 10, Copyright 1979, with permission from Springer.[2]](/content/115/2020/1/1/img/JASSM-1-044-g054.png)
- The first edition of Watanabe’s Atlas of arthroscopy featured hand painted depictions of the view down the arthroscope, as Watanabe believed that the photos were not of adequate quality.[102] In later editions, Watanabe included photos taken through the arthroscope. Reprinted from Atlas of Arthroscopy, 3rd edition, Watanabe M, Takeda S, Ikeuchi H, History of Arthroscopy, p. 10, Copyright 1979, with permission from Springer.[2]

- James Roth and Luigi Pederzini together at an Italian upper limb arthroscopy course in 1990. Courtesy Luigi Pederzini.
![Terry Whipple (front and center) a pioneer of wrist arthroscopy is surrounded by past and future presidents of the EWAS in 2013, at the IRCAD-EITS center in Strasbourg, France. From left to right standing: past presidents: Didier Fontes (France), Riccardo Luchetti (Italy), Francesco de Piñal (Spain), Terry Whipple, Tommy Lindau (Sweden/UK), Toshiyasu Nakamura (Japan), Max Haerle (Germany), and David Slutsky (USA), with upcoming presidents Andrea Atzei (Italy) and Pak-Cheong Ho (Hong Kong). Front row (kneeling): founder of the EWAS, Christophe Mathoulin (France) and secretary general, Jan-Ragnar Haugstvedt (Norway).[54]](/content/115/2020/1/1/img/JASSM-1-044-g056.png)
- Terry Whipple (front and center) a pioneer of wrist arthroscopy is surrounded by past and future presidents of the EWAS in 2013, at the IRCAD-EITS center in Strasbourg, France. From left to right standing: past presidents: Didier Fontes (France), Riccardo Luchetti (Italy), Francesco de Piñal (Spain), Terry Whipple, Tommy Lindau (Sweden/UK), Toshiyasu Nakamura (Japan), Max Haerle (Germany), and David Slutsky (USA), with upcoming presidents Andrea Atzei (Italy) and Pak-Cheong Ho (Hong Kong). Front row (kneeling): founder of the EWAS, Christophe Mathoulin (France) and secretary general, Jan-Ragnar Haugstvedt (Norway).[54]
Videos
Please visit the article in HTML to watch the video at https://dx.doi.org/10.25259/JASSM_29_2020
Video 1: Terry Whipple explains how the improvements in camera technology allowed greater possibilities for wrist arthroscopy. Courtesy Gregory Bain.
Video 2:
Video 2: Gary Poehling describes Leonard Goldner’s decision to place him in charge of arthroscopy on his return from Japan as only a junior resident. Courtesy Gregory Bain.Video 3:
Video 3: Terry Whipple discusses how the portals for wrist arthroscopy were developed with Jack Powell. Courtesy Gregory Bain.Video 4:
Video 4: Gary Poehling explains the origins of the plans to bring wrist arthroscopy to the USA. He, Terry Whipple and James Roth met at the International Knee Association meeting in Salzburg, Austria in 1985. They realized they were all hand surgeons, and created a plan to develop, teach, and standardize wrist arthroscopy. Courtesy Gregory Bain.Video 5:
Video 5: Terry Whipple outlines the battleground that faced younger knee surgeons who were keen to integrate arthroscopic techniques into their practice. Courtesy Gregory Bain.Video 6:
Video 6: James Urbaniak’s assistance was important in providing an invitation to the senior American surgeons for the first wrist arthroscopy workshop. Courtesy Gregory Bain.Video 7:
Video 7: Gary Poehling reminisces on the excitement of the early days of wrist arthroscopy. Courtesy Gregory Bain.Acknowledgments
Kimberley Bryant for assistance in preparation of manuscript
Christophe Mathoulin Max Haerle Riccardo Luchetti PC Ho Jan-Ragnar Haugstvedt Guillaume Herzberg Graham King Dan Nagle Toshi Nakamura Lee Osterman David Slutsky Steven Viegas. Buddy Savoie Luigi Pederzini
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Semilunar cartilage disease: A plea for the early recognition by means of the arthroscope. Ill J Med. 1925;47:290-2.
- [Google Scholar]
- Severin nordentoft: The first arthroscopist. Arthroscopy. 2001;17:532-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopy or the direct visualization of joints: An experimental cadaver study. J Bone Joint Surg. 1931;13:669-95.
- [Google Scholar]
- Giants of orthopaedic surgery: Masaki Watanabe MD. Clin Orthop Relat Res. 2013;471:2443-8.
- [CrossRef] [PubMed] [Google Scholar]
- The early days of arthroscopic surgery in Japan. Arthroscopy. 1988;4:222-5.
- [CrossRef] [Google Scholar]
- Diagnostic uses of arthroscopy In: McKibbin B, ed. Recent Advances in Orthopaedics (2nd ed). Edinburgh: Churchill Livingstone; 1975. p. :218-34.
- [Google Scholar]
- The basics of wrist arthroscopy In: Whipple TL, ed. Arthroscopic Surgery-the Wrist. Philadelphia, PA: J. B. Lippincott; 1992. p. :7-9.
- [Google Scholar]
- Instrumentation for small joints: The arthroscope. Arthroscopy. 1988;4:45-6.
- [CrossRef] [Google Scholar]
- Arthroscopic Surgery: Principles and Practice (3rd ed). St Louis: The C. V. Mosby Company; 1986.
- [Google Scholar]
- Arthroscopic examination of the knee-polypuncture technique with percutaneous intra-articular manipulation. J Bone Joint Surg. 1978;80:444-58.
- [CrossRef] [Google Scholar]
- Distal radioulnar joint arthroplasty: The hemiresection-interposition technique. J Hand Surg Am. 1985;10:169-78.
- [CrossRef] [Google Scholar]
- Arthroscopy of the wrist: Anatomy and classification of carpal instability. Arthroscopy. 1990;6:133-40.
- [CrossRef] [Google Scholar]
- Arthroscopic debridement of triangular fibrocartilage complex tears. Arthroscopy. 1990;6:120-4.
- [CrossRef] [Google Scholar]
- Arthroscopic reduction and internal fixation of distal radius fractures. Orthop Clin North Am. 1995;26:739-48.
- [Google Scholar]
- Carpal instability: Evaluation and treatment. J Am Acad Orthop Surg. 1993;1:10-7.
- [CrossRef] [PubMed] [Google Scholar]
- Triangular fibrocartilage complex lesions: A classification. J Hand Surg. 1989;14:594-606.
- [CrossRef] [Google Scholar]
- Anatomic and biomechanical analysis of the arthroscopic wafer procedure. Arthroscopy. 1992;8:204-12.
- [CrossRef] [Google Scholar]
- Intraarticular ganglion of the dorsal interosseous scapholunate ligament: A case for arthroscopy. Arthroscopy. 1986;2:93-5.
- [CrossRef] [Google Scholar]
- Wrist anatomy: Incidence distribution and correlation of anatomic variations tears and arthrosis. J Hand Surg Am. 1993;18:463-75.
- [CrossRef] [Google Scholar]
- The lunatohamate articulation of the midcarpal joint. Arthroscopy. 1990;6:5-10.
- [CrossRef] [Google Scholar]
- Arthroscopic treatment of degenerative tears of the triangular fibrocartilage. Hand Clin. 1994;10:615-24.
- [Google Scholar]
- Radiocarpal arthroscopy and arthrography in the diagnosis of ulnar wrist pain. Arthroscopy. 1986;2:234-43.
- [CrossRef] [Google Scholar]
- Evaluation of the triangular fibrocartilage complex tears by arthroscopy, arthrography, and magnetic resonance imaging. Arthroscopy. 1992;8:191-7.
- [CrossRef] [Google Scholar]
- Wrist arthroscopy In: Lichtman DM, ed. The Wrist and Its Disorders. Philadelphia, PA: W. B. Saunders Company; 1988. p. :108-28.
- [Google Scholar]
- Hand instrumentation for small joint arthroscopy. Arthroscopy. 1988;4:126-8.
- [CrossRef] [Google Scholar]
- The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;38:32-40.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of complex fractures of the distal radius. Combined use of internal and external fixation and arthroscopic reduction. Hand Clin. 1993;9:603-12.
- [Google Scholar]
- Arthroscopic anatomy of the wrist and distal radioulnar joint. Hand Clin. 1999;15:393-413.
- [Google Scholar]
- The future of arthroscopic surgery in the hand and wrist. Hand Clinics: Advanced Wrist Arthroscopy and Endoscopy. 1995;11:97-9.
- [Google Scholar]
- Arthroscopic proximal row carpectomy. Tech Hand Up Extrem Surg. 1997;1:116-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic excision of dorsal carpal ganglion cysts. Oper Tech Plast Reconstr Surg. 2002;9:118-23.
- [CrossRef] [Google Scholar]
- Perilunate dislocations and fracture-dislocations: A multicenter study. J Hand Surg. 1993;18:768-79.
- [CrossRef] [Google Scholar]
- Perilunate injuries, not dislocated (PLIND) J Wrist Surg. 2013;2:337-45.
- [CrossRef] [PubMed] [Google Scholar]
- Intérêt de l'arthroscopie du poignet dans le traitement des fractures articulaires du 1/4 inférieur du radius: A propos de 27 cas interest in wrist arthroscopy for treatment of articular fractures of the distal radius: Report of 27 cases. Chir Main. 2001;20:342-50.
- [CrossRef] [Google Scholar]
- Extensor carpi radialis brevis ligamentoplasty and dorsal capsulodesis for the treatment of chronic post-traumatic scapholunate instability. Chir Main. 2010;29:172-9.
- [CrossRef] [PubMed] [Google Scholar]
- The EWAS classification of scapholunate tears: An anatomical arthroscopic study. J Wrist Surg. 2013;2:105-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic dorsal capsuloligamentous repair in chronic scapholunate ligament tears. Hand Clin. 2011;27:563-72.
- [CrossRef] [PubMed] [Google Scholar]
- Lésion du ligament scapho-lunaire: Intérêt de l'arthroscopie, propositions thérapeutiques à propos d'une série de 62 patients scapholunate ligament injury: Value of arthroscopy, therapeutic proposals for a series of 62 patients. Mém Acad Natl Chir. 2004;3:62-72.
- [Google Scholar]
- Letter to the editor, EWAS milestone achieved in Strasbourg. J Wrist Surg. 2014;3:64-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic reduction and percutaneous fixation of scaphoid fractures with a novel dorsal technique. Orthop Clin North Am. 2001;32:247-61.
- [CrossRef] [Google Scholar]
- Percutaneous internal fixation of selected scaphoid nonunions with an arthroscopically assisted dorsal approach. J Bone Joint Surg Am. 2003;85:20-32.
- [CrossRef] [PubMed] [Google Scholar]
- Minimal invasive management of scaphoid fractures: From fresh to nonunion. Hand Clin. 2011;27:291-307.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic partial wrist fusion. Tech Hand Up Extrem Surg. 2008;12:242-65.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic resection of volar ganglion of the wrist: A new technique. Arthroscopy. 2003;19:218-21.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic assessment and classification of Kienbock's disease. Tech Hand Up Extrem Surg. 2006;10:8-13.
- [CrossRef] [PubMed] [Google Scholar]
- Results of arthroscopic debridement for isolated scaphotrapeziotrapezoid arthritis. J Hand Surg. 2003;28:729-32.
- [CrossRef] [Google Scholar]
- Arthroscopic excision of ulnar styloid in stylocarpal impaction. Arthroscopy. 2006;22:677.e1-e3.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic capsular release for contracture of the wrist: A new technique. Arthroscopy. 2000;16:106-10.
- [CrossRef] [Google Scholar]
- The future: Endoscopic surgery of the wrist and forearm In: Savoie FH, Field LD, Steinmann SP, eds. The Elbow and Wrist: AANA Advanced Arthroscopic Surgical Techniques. New Jersey: Slack Incorporated; 2016. p. :417-24.
- [Google Scholar]
- Anatomical reduction of intra-articular fractures of the distal radius. An arthroscopically-assisted approach. J Bone Joint Surg Br. 2000;82:79-86.
- [CrossRef] [PubMed] [Google Scholar]
- New advances in wrist arthroscopy. Arthroscopy. 2008;24:355-67.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic capsular shrinkage for midcarpal instability of the wrist. J Bone Joint Surg. 2003;85B:177.
- [Google Scholar]
- Dry arthroscopy of the wrist: Surgical technique. J Hand Surg. 2007;32:119-23.
- [CrossRef] [PubMed] [Google Scholar]
- Dry arthroscopy of the wrist: Its role in the management of articular distal radius fractures. Scand J Surg. 2008;97:298-304.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic Management of Distal Radius Fractures. Berlin, Heidelberg: Springer-Verlag; 2010. p. :264.
- [CrossRef] [Google Scholar]
- Arthroscopic Management of Ulnar Pain. Berlin, Heidelberg: Springer-Verlag; 2012. p. :374.
- [CrossRef] [Google Scholar]
- Complete avulsion of the distal posterior interosseous nerve during wrist arthroscopy: A possible cause of persistent pain after arthroscopy. J Hand Surg Am. 1999;24:240-2.
- [CrossRef] [PubMed] [Google Scholar]
- Lesioni capsulelegamentose della radio-ulnare distale e fibrocartilagine triangolare capsule ligament injuries of the distal radioulnar and triangular fibrocartilage In: Landi A, Catalano F, Luchetti R, eds. Trattato di Chirurgia Della Mano. Italy: Verduci Editore Roma; 2006. p. :159-87.
- [Google Scholar]
- Origins and insertions of the triangular fibrocartilage complex: A histological study. J Hand Surg Br. 2001;26:446-54.
- [CrossRef] [PubMed] [Google Scholar]
- Results of repair of peripheral tears in the triangular fibrocartilage complex using an arthroscopic suture technique. Scand J Plast Reconstr Surg Hand Surg. 1999;33:439-47.
- [CrossRef] [PubMed] [Google Scholar]
- LT tears and arthroscopic repair. Arthroscopic Management of Ulnar Pain 2012
- [CrossRef] [Google Scholar]
- Long term results after arthroscopic resection of lesions of the triangular fibrocartilage complex. Scand J Plast Reconstr Surg Hand Surg. 2001;35:79-83.
- [CrossRef] [PubMed] [Google Scholar]
- The role of arthroscopy in the treatment of scapholunate instability. Hand Clin. 1995;11:37-40.
- [Google Scholar]
- Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg. 1996;78:357-65.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg. 2000;25:464-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dorsal scapholunate ligament injury: A classification of clinical forms. J Hand Surg Eur Vol. 2013;38:165-9.
- [CrossRef] [PubMed] [Google Scholar]
- Three-ligament tenodesis for the treatment of scapholunate dissociation: Indications and surgical technique. J Hand Surg. 2006;31:125-34.
- [CrossRef] [PubMed] [Google Scholar]
- A new surgical technique for carpal instability with scapholunate dissociation. Surg Technol Int. 1996;5:370-4.
- [Google Scholar]
- Endoscopic management of carpal tunnel syndrome. Arthroscopy. 1989;5:11-8.
- [CrossRef] [Google Scholar]
- Endoscopic release of the carpal ligament: A new technique for carpal tunnel syndrome. Arthroscopy. 1989;5:19-24.
- [CrossRef] [Google Scholar]
- Endoscopic release of the carpal tunnel: A randomized prospective multicenter study. J Hand Surg. 1992;17:987-95.
- [CrossRef] [Google Scholar]
- Endoscopically assisted nerve decompression of rare nerve compression syndromes at the upper extremity. Arch Orthop Trauma Surg. 2013;133:575-82.
- [CrossRef] [PubMed] [Google Scholar]
- The endoscopic management of cubital tunnel syndrome. J Hand Surg. 2006;31:23-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic synovectomy of the rheumatoid wrist. J Hand Surg Br. 1993;18:92-6.
- [CrossRef] [Google Scholar]
- Arthroscopic resection arthroplasty of the radial column for SLAC wrist. J Wrist Surg. 2014;3:114-22.
- [CrossRef] [PubMed] [Google Scholar]
- Suture welding for arthroscopic repair of peripheral triangular fibrocartilage complex tears. Tech Hand Up Extrem Surg. 2007;11:45-50.
- [CrossRef] [PubMed] [Google Scholar]
- The floating lunate: Arthroscopic treatment of simultaneous complete tears of the scapholunate and lunotriquetral ligaments. Hand (NY). 2009;4:250-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg Am. 1997;22:344-9.
- [CrossRef] [Google Scholar]
- Hamato-lunate impingement: An uncommon cause of ulnar-sided wrist pain. Arthroscopy. 2000;16:540-4.
- [CrossRef] [PubMed] [Google Scholar]
- The management of dorsal radiocarpal ligament tears. J Am Soc Surg Hand. 2005;5:167-74.
- [CrossRef] [Google Scholar]
- Factors associated with arthroscopically determined scaphoid fracture displacement and instability. J Hand Surg. 2012;37:1405-10.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic partial resection of the ulnar head for ulnocarpal decompression. Oper Orthop Traumatol. 2016;28:263-9.
- [CrossRef] [PubMed] [Google Scholar]
- United States Patent and Trademark Office. Official Gazette of the United States Patent and Trademark Office: Patents. . 1981;1007:127.
- [Google Scholar]


![Steve Viegas (USA) been a leader in the advancement of the understanding of wrist arthroscopy, anatomy and biomechanics.[26-29] He has also been involved been involved in the development of the treatment of scapholunate ligament lesions. Courtesy PC Ho.](/content/115/2020/1/1/img/JASSM-1-044-g029.png)
![Richard (Dick) Berger (USA) been a leader in the advancement of the understanding of wrist anatomy and biomechanics.[39-41] Courtesy PC Ho.](/content/115/2020/1/1/img/JASSM-1-044-g032.png)
![Guillaume Herzberg (France) has made contributions to the perilunate injuries and their arthroscopic management.[46,47] Courtesy PC Ho.](/content/115/2020/1/1/img/JASSM-1-044-g034.png)
![Joe Slade (USA) was a dynamic personality who was actively involved the advancements of arthroscopic management of scaphoid fractures.[55,56] Courtesy PC Ho.](/content/115/2020/1/1/img/JASSM-1-044-g036.png)
![Jan-Ragnar Haugstvedt (Norway) developed techniques for the management of ulnar sided wrist disorders including TFC tears and lunotriquetral instability.[76-78] He has also been actively involved in the leadership of EWAS and IWAS. Courtesy PC Ho.](/content/115/2020/1/1/img/JASSM-1-044-g044.png)
![Marc Garcia-Elias (Spain) has made many contributions to the understanding of anatomy, patho-anatomy and treatment of wrist injuries.[82,83] Courtesy Marc Garcia-Elias.](/content/115/2020/1/1/img/JASSM-1-044-g047.png)
![David Slutsky (USA) established the Journal of Wrist Surgery in 2012.[104] He also published many other papers and texts.[96-99] Courtesy Dr Gregory Bain.](/content/115/2020/1/1/img/JASSM-1-044-g052.png)




