Translate this page into:
Modified technique of Indirect arthroscopic distal clavicle resection

*Corresponding author: Ravinder Kant Manocha, Department of Orthopaedics, Northern Railway Central Hospital, New Delhi, India. rkmanocha@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta S, Manocha RK, Mishra K. Modified technique of Indirect arthroscopic distal clavicle resection. J Arthorsc Surg Sport Med 2021;2(1):73-80.
Abstract
Distal clavicle resection is an accepted surgical treatment option for unremitting acromioclavicular joint arthritis. Indirect arthroscopic approach is preferred when an additional subacromial or glenohumeral diagnostic or therapeutic procedure is contemplated. However, concomitant subacromial decompression and acromial overhang removal, which is integral to indirect approach vis-a-vis direct approach, have additional risks of stiffness and acromial fracture. A modification in indirect approach technique is demonstrated which not only reduces these risks but also improves accuracy and safety of distal clavicle resection. The pros and cons are discussed in detail with reference to relevant literature.
Keywords
AC joint pain
Modified arthroscopic mumford procedure
Arthroscopic distal clavicle excision
Indirect arthroscopic distal clavicle excision
AC joint artritis
INTRODUCTION
Arthritis remains the primary cause of acromioclavicular joint (ACJ) pain and is often associated with distal clavicular osteolysis. Osteolysis occurs as a consequence of cumulative microtrauma resulting from repeated overhead lifting or throwing or heavy labor.[1] In the absence of acute trauma, repetitive stressful activity results in subchondral stress fractures and a subsequent hyper-vascular response[2] leading ultimately to resorption of distal clavicle. A chronic pain sharply localized to ACJ aggravated by cross-adduction of the affected shoulder is typical presentation. Provocative tests for the clinical diagnosis of ACJ pain include active compression test, Paxinos test, and Buchberger test.
Non-operative treatment remains invariable initial treatment in ACJ arthritis and includes nonsteroidal anti-inflammatory medicines, physical therapy, activity modification, and local anesthetic and corticosteroids injections.[2] Activity modification includes avoidance of pain causing repetitive motions, such as push-ups, dips, flies, and bench press exercises. Physical therapy focuses on maintaining active range of movement (ROM) and increasing muscle strength for scapular stabilization.
Surgical treatment is option for patients when non-operative modalities fail to provide adequate pain relief and persistent symptoms continue to interfere with activities of daily living. Surgery, entails producing a gap by resection of bone from distal clavicle mainly to prevent abutment between distal clavicle and medial acromion during movement.[3] This procedure can be performed by open or arthroscopic approach.
Arthroscopic approach may be “Bursal sparing Direct” or “Indirect Bursal” approach. Factors such as avoidance of AC ligament damage, clavicular instability, and post-operative pain influence the choice of surgical approach. Here, we present a case report in which indirect arthroscopic technique of resection of lateral end of clavicle was modified to achieve more efficient avoidance of AC ligament damage and clavicular instability.
CASE REPORT
A 27-year-old male, wrestler by profession came to us with pain in AC joint area for the past 2 years, with difficulty in overhead abduction of right arm. He had already received conservative management including activity modification (not participated in wrestling bout for >1 year) and steroid injections without any lasting relief. Two shots of steroid injections were repeated at our center without relief.
On clinical examination, tenderness localized to AC joint and aggravation of pain with cross body adduction was elicited. X-rays: Anteroposterior, Axillary, Zanca, and simultaneous B/L shoulder weight bearing view were done [Figure 1a-d]. CT [Figure 2a-f] and MRI [Figure 2g-p] were done to confirm the diagnosis. Radiographic studies revealed cystic changes, sclerosis, irregular shape, and arthrosis of articular surface of distal clavicle with degeneration of articular disc and AC joint space narrowing with suggestion on MRI of Type II acromion causing impingement of supraspinatus tendon and hyperintensity in supraspinatus and infraspinatus myotendinous complex. Patient therefore underwent Arthroscopic Indirect distal clavicle excision (DCE) by a modified technique as described below.

- (a) AP view (b) axillary view (c) zanca view (d) simultaneous AP of both shoulders – weight bearing.
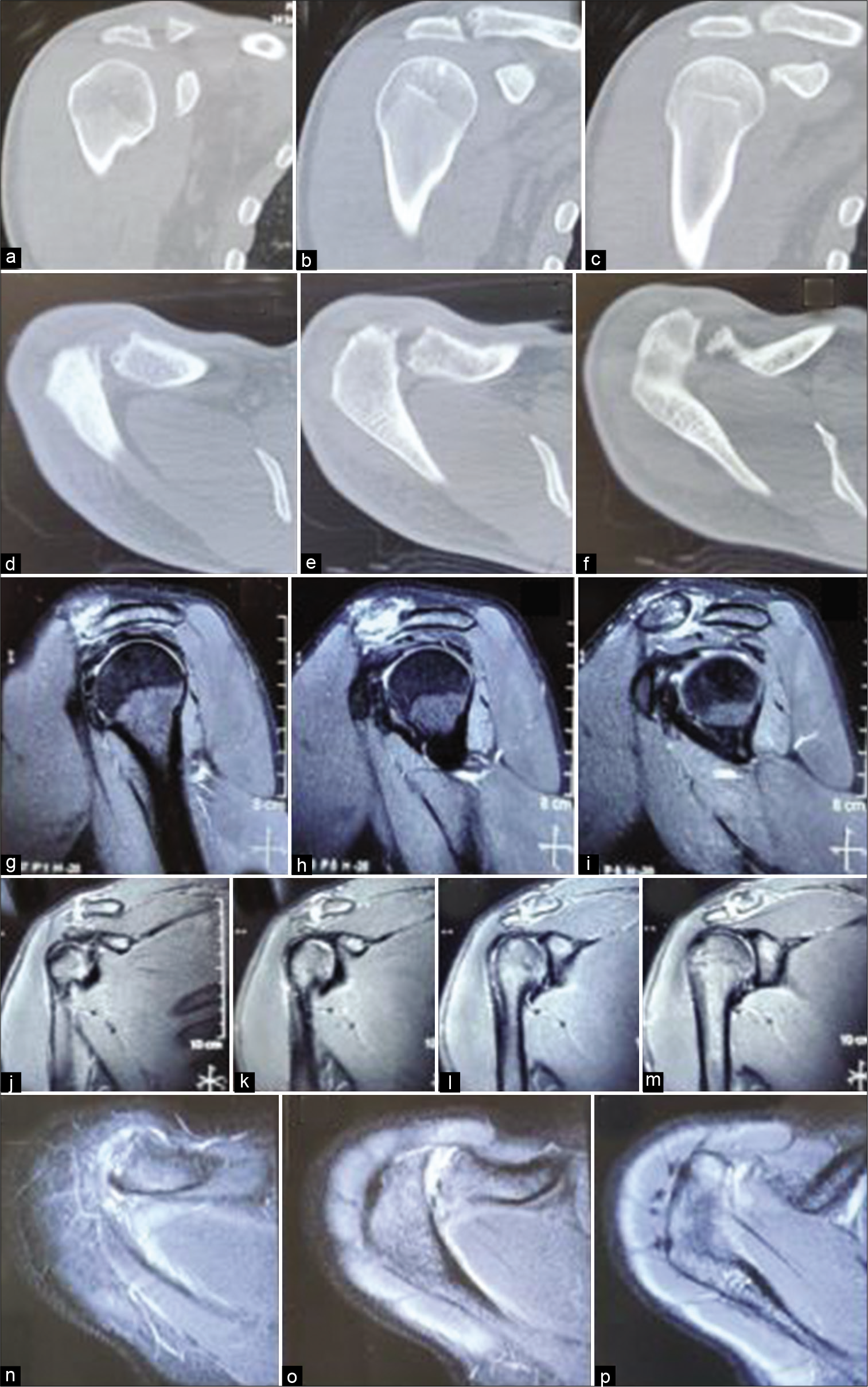
- (a-c) CT coronal section Anterior to Posterior, (d-f) CT transverse section Superior to Inferior, (g-i) MRI coronal section Lateral to Medial, (j-m) MRI coronal section Anterior to Posterior (n-p) MRI transverse section Superior to Inferior: Please not subchondral cyst, joint space reduction and osteophytes in CT; and synovitis, edema and degenerate articular disc in MRI.
Patient could not follow-up regularly or receive structured rehabilitation exercises because of corona epidemic and was called at 6 months for clinical and functional assessment. He had already started gym training and was able to do 250 dips without pain at present compared to less than 50 before surgery. He was, however, much away from 1000 dips he was able to do 3 years back before the start of his acromioclavicular pain. His pre-operative UCLA score of 11 had improved to 29 and Constant score from 35 to 78. Patient “strongly agreed” that the procedure had met his expectations. Post-operative radiological studies and ROM at 6 months is shown in [Figure 3a-i].
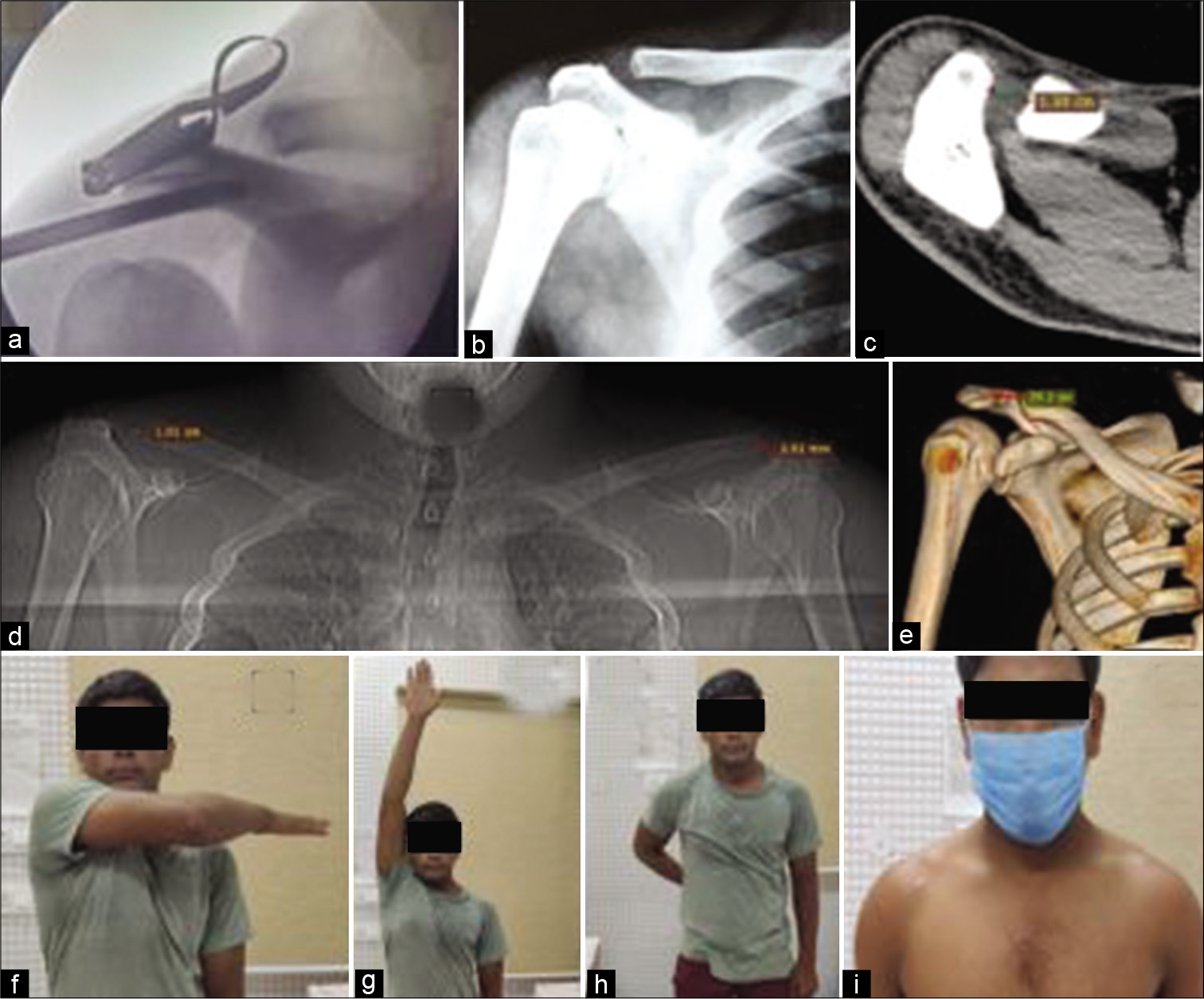
- (a) Intraoperative C-arm Image (b) post-operative X-ray (c) CT of ACJ at 6 months follow-up (d) comparative AC joint space measurements (e) CT reconstruction at 6 months post-operative (f-h) ROM of operated shoulder (i) cosmetic results. Note Anterior ACJ portal and lateral portal.
OPERATIVE TECHNIQUE-MODIFIED INDIRECT APPROACH
Under general and regional interscalene block anesthesia, the patient was operated in beach chair position. Glenohumeral arthroscopy revealed no abnormality. Modifications are highlighted in bold italics:
Step No.1: Posterolateral and Lateral portal were used for arthroscopy of Subacromial space. Both portals were placed 5 mm more anterior, closer to area of interest, than standard
Step No.2: A needle was passed percutaneously across ACJ to enter into the subacromial space. While viewing with a standard 4.0 mm 30 Degree scope from posterolateral portal, the needle was rocked back and forth [Video 1 = 0–3 s, Figure 4a] to localize the site (and not joint space) of AC Joint. This trick permitted accurate localization of site of AC Joint, allowing us to stay focused to the site of pathology thereby avoiding unnecessary ablation of normal bursaltissue [Figure 4b and c].
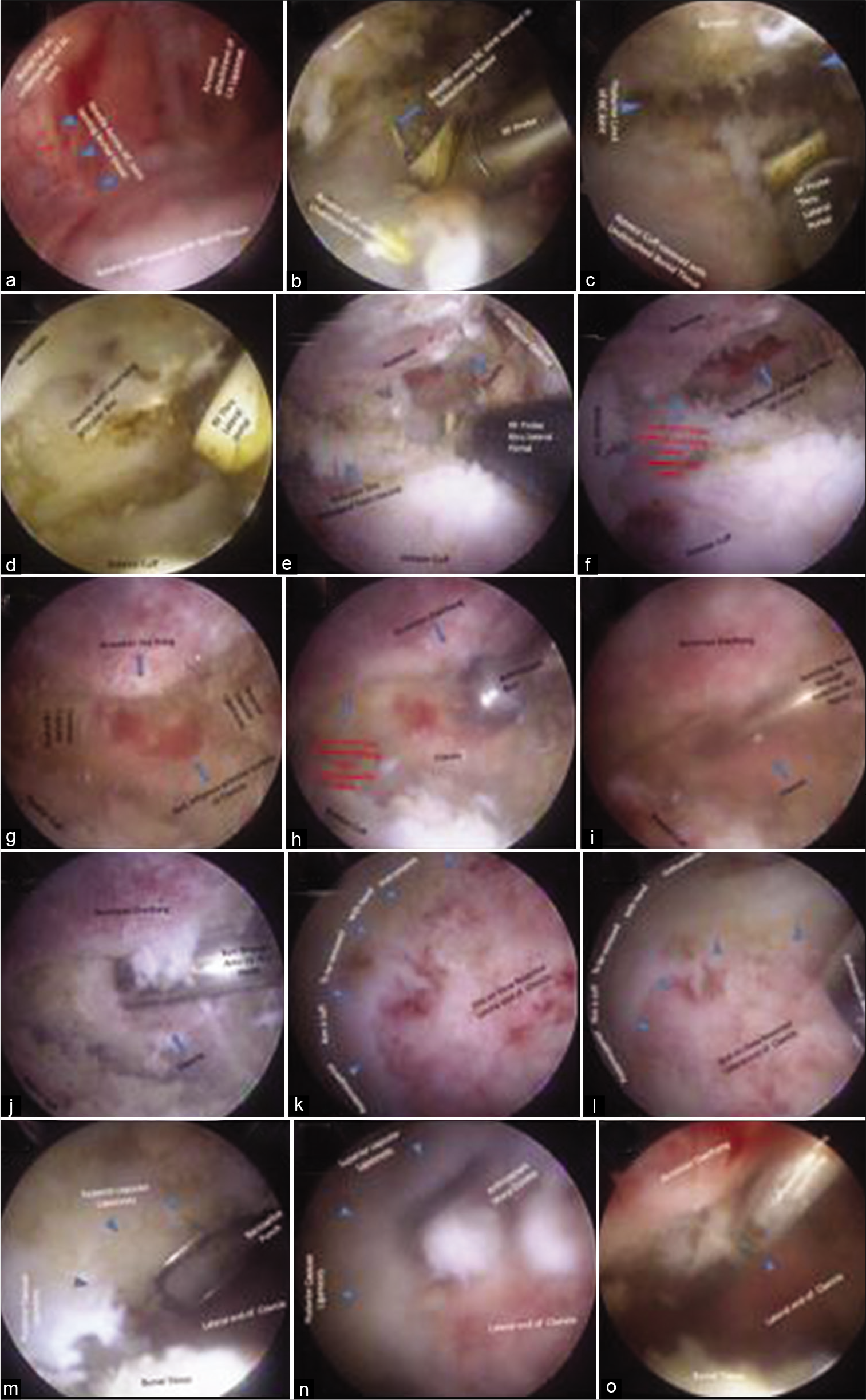
- (a and b) Needle localized in subacromial space to restrict ablation to AC joint. (c and d) AC Joint view without and with clavicle pressed down (e and f) View of minimally shaved acromial overhang and inflamed lateral end of clavicle (g) view with 700 scope. (h) Clavicle resection thru lateral portal, (i) anterior ACJ portal, (j) clavicle resection thru anterior portal, (k and l) posterosuperior rim left unviolated during motorized resection, (m and n) posterosuperior rim removal with punch and curette, (o) calibrated probe measurement of length of resection.
Step No.3: Both posterolateral and lateral portals were used alternatively as working and viewing portals. Access to ACJ was established by viewing from posterolateral and ablation through lateral portal [Video 1 = 3–36 s].
Step No.4: The bone seen moving on external downward manual pressure medial to needle was identified as distal clavicle [Video 1 = 37–44 s]. A degenerated articular disc was covering the articular end of clavicle and was excised [Video 1 = 1 m 19 s–2 m 11 s, Figure 4d and e]. Removal of articular disc brought red, inflamed, and angry looking articular surface in view [Figure 4f].
Step No.5: Lateral acromial overhang is shaved with 3 mm round burr only just enough to accommodate 70°Arthroscope with its 6 mm sheath and no more to prevent weakening of acromion [Video 1 = 2 m 11 s–2 m 53 s, Figure 4f].
Step No.6: At this point we used 70-degree scope from lateral portal to gain visualization of whole of clavicle end around the acromial overhang [Video 1 = 3 m 1 s–3 m 32 s, Figure 4g].
Step No.7: Early part of excision of lateral end of clavicle was done from Lateral portal only [Figure 4h] while viewing from posterolateral portal. Burr through lateral portal automatically saves posterosuperior part of clavicle because the acromial overhang prevents access of straight burr to posterosuperior clavicle [Video 1 = 3 m 33 s–4 m 24 s] andavoids injury to posterosuperiorligaments.
Step No.8: Anterior portal tangential to the articular surface of clavicle is then created under arthroscopic guidance [Video 1 = 4 m 25 s–4 m 33 s, Figure 4i]. Posterosuperior clavicle which was inaccessible to straight burr from lateral portal is easily accessed from anterior portal [Figure 4j]. Excision of clavicle using burr from anterior portal [Video 1 = 4 m 34 s–5 m 35 s] is continued. In the final leg clavicle was pressed downward to remove bone from posterosuperior corner [Video 1 = 5 m 36 s–5 m 58 s]leaving a thin superior and posterior rim deliberately un-violated [Figure 4k and l].
Step No.9: Removal of posterosuperiorrim was done by narrowlinebasket punch and arthroscopic curette [Figure 4m and n]. These instruments provide excellent tactile feedback and careful piecemeal removal could be done without causing damage to superoposterior capsule.
Step No.10: Excised length was gauzed with a calibrated probe [Figure 4o] introduced through Lateral Portal while viewing through posterolateralportal. In all 10 mm of lateral end of clavicle was excised. Probe can be placed at anterior edge, center, and posterior edge to verify adequacy and accuracy of clavicle excision [Video 1 = 7 m 39 s–8 m 0 s]. Adequacy of excision was repeatedly measured bycalibrated probe and was evident all through arthroscopy. Fluoroscopy was used only for confirmation at the end of procedure.
Step No.11: Integrity of posterosuperior capsule and ACJ ligaments was checked arthroscopically as well as by cross adduction movement.
Controlled analgesia in post-operative period and cuff and collar sling was applied for a week for control of pain. The patient began to perform gentle active and active assisted range of motion (ROM) exercises on the day after surgery. The level of physical therapy progressed to full active ROM exercises and isometric exercises. Strengthening exercise within the patient’s tolerance level was permitted 6 weeks after surgery. Structured supervised rehabilitation could not be administered because of COVID-19 epidemic and lockdown. Patient followed up with us only 6 months after surgery and now structured rehabilitation for restoration to his sports has been started.
DISCUSSION
At the outset it must be emphasized that surgical treatment modalities for ACJ arthritis are reserved for patients in whom conservative management for at least 6 months have failed to provide pain relief and persistent symptoms continue to interfere with activities of daily living. Our case was subjected to surgical treatment after 2 years of conservative treatment, at least 6 months of that was under our care.
Distal clavicular excision (Mumford procedure) is a well-accepted treatment for un-remitting painful ACJ arthritis especially in sports persons. A systematic review concluded that the arthroscopic approach, enabled a faster return to activities while obtaining similar long-term outcomes as open procedure.[4] Besides a shortened recovery time, the arthroscopic procedure has several other advantages over open DCE including precise and reproducible resection of bone, preservation of the deltoid and the trapezius, diagnosis of the associated pathologies of glenohumeral joint and subacromial space, minimal scar formation, and cosmetic merits.[4]
Direct (Bursal Sparing)[5] and indirect (through Subacromial Space)[6] are two arthroscopic methodologies widely used. The direct, or superior, arthroscopic technique require a 2.7-mm arthroscope and small sized mechanized burr to begin excision and larger 4-mm arthroscope and instruments to complete the procedure.[7] Direct approach is ideal for patients with isolated AC joint pathology where exploration of the subacromial space is not required.[7] Indirect approach is popular choice when an additional diagnostic or interventional procedure is contemplated in subacromial space or glenohumeral joint, namely, acromioplasty, and/or subacromial decompression, and superior labral debridement or rotator cuff repair.[6] Pensak et al.[4] cautioned that concomitant ASD, which is integral to indirect arthroscopic approach, carries additional risk of adhesions in the subacromial space with resultant stiffness; and of stress fractures of the acromion if removal of the acromial spur is excessive.
Variables such as patient occupation, age, degree of activity limitation, shoulder dominance, and patient goals should be considered by both patient and physician before a decision concerning surgical treatment is made. Our choice in favor of indirect Bursal approach was influenced by patient’s anxiety in view of suggestions of impingement and partial tear in MRI, to have his shoulder evaluated fully to take an informed decision to continue with his sport as wrestler. No additional abnormality was, however, found on arthroscopic examination either in glenohumeral joint or subacromial space.
We were, however, fully cognizant of the additional risk[7] that a subacromial approach poses and hence modification in form of “Step 2 of Operative technique” was incorporated to reduce possibility of adhesions in subacromial space and use of 70° scope was done as in “Step 5 of Operative Technique” to reduce removal of bone from acromion to reduce stress fractures.
Guiding placement of portals by introducing a needle is a standard technique in all arthroscopies. A needle is passed routinely from anterior to posterior direction to guide placement of anterior ACJ portal in a standard technique of arthroscopic DCE.[8] Needle passed from superior to inferior direction across the ACJ into subdeltoid space is another commonly employed trick in arthroscopic DCE to verify the AC joint space. Since verification of joint space is the objective, this step is employed after most of bursectomy and inferior capsular tissue ablation as well as partial minimal removal of undersurface of acromion.[9] Needle is visible in subdeltoid space as soon as it crosses the ACJ from superior to inferior direction.
Our use of the needle is different in objective, indication as well as methodology. Indication was limiting the ablation of normal bursal tissue to reduce the risk of adhesions. Objective was not to localize the joint space but to locate the site of ACJ. Methodology was to rock the needle back and forth and observe the movement of bursal tissue. Needle was not directly visible till much later. This permitted identification of location of subarticular bursal tissue and ablation was then limited to only the area underneath ACJ.
An early placement before start of ablation has been described in literature by Minamikawa et al.[10] but again for a different objective. He introduced two needles across ACJ into subdeltoid space as well as two K wires at 15 mm distance medially into clavicle marking anterior-posterior and medial limits of resection. His objective was not to limit the bursal ablation but to make clavicle resection accurate. Rocking the needle and identifying the site of movement caused by the needle when it is still under cover of bursaltissue to limit the ablation to only the subarticular bursaltissue and inferior capsule as described in this article is a complete novelty not suggested before to the best of our literature search efforts.
70° arthroscope use for visualization of entire AC joint through standard posterolateral and lateral portals has been described in the literature.[11] We reiterate that the use of 70° scope allows to look around the overhang obviating the need for bone removal from acromion thereby reducing risk of iatrogenic fracture of acromion. Saving acromion strength may have been of particularly value in a wrestler.
Adequate resection of clavicle without damaging the posterosuperior capsule and AC ligaments is critical to good clinical outcome and essential to prevent heterotrophic ossification and instability of clavicle.[5] Our modifications of arthroscopic gauzing of excised length of clavicle and and prevention of damage to posterosuperior capsule are particularly noteworthy.
Resection of articular end of Clavicle per se causes instability. Blazar et al.[12] noted anteroposterior motion of the clavicle was increased by an average of 5.5 mm, compared to a normal shoulder, following both open and arthroscopic techniques. Resection of large amounts of the distal clavicle (>15 mm) leads to more instability due to the inherent damage caused to AC ligaments as well as to the trapezoid part of coracoclavicular ligament. Nuber and Brown[3] brought attention to horizontal instability of the clavicle caused due to disruption of AC ligaments which causes pain due to abutment against the spine of scapula
Probes/Stylus is integral to any arthroscopic procedure and is commonly referred to as extension of palpating finger of the surgeon. Literature[8] justifiably emphasizes using stylus to check “completely removed clavicular bone up to its cranial and posterior margins.” Probe use as a measuring device is also not uncommon in various arthroscopic procedures. Arthroscopic estimation of glenoid bone loss, referencing to the bare area as center and comparing anterior and posterior lengths from bare area, immediately comes to mind
To the best of our effort at search of literature, probes have not yet been used to monitor the progress of excision of lateral end of clavicle. Most of authors[1-7] refer to length (10 mm) of acromionizer burr to gauze the excised length. It is pertinent to mention here that we used small rounded burr because in our experience 5 × 10 mm cylindrical burr substantially obstructs view in small space of AC joint. Using calibrated probe to measure and using a shorter and lower profile round burr for excision is, in our opinion, another way to exercise greater control in bone resection under better viewing.
The calibrated probe that we used had scales readable directly in mm. Commonly used probes are laser marked at a least count of 2 mm for measurement and one needs to count the number of laser marks from the tip to deduce the length being measured. We believe directly readable scales were important as both clavicle excision and monitoring of progression of clavicle excision were done from lateral portal while the view was being obtained from posterolateral portal. Counting the number of laser mark, when the probe is moving away from the viewing arthroscope, in almost a parallel trajectory is not very efficient.
Structures providing maximum restraint to clavicle are superior and posterior portions of the AC ligaments. Indirect arthroscopic technique per se, avoids the more superior portions of the AC ligament, and reduces the risk of joint instability. However, even in indirect approach, the final leg of surgery involves using burr from anterior portal when these ligaments are under risk of damage
We modified our operative technique to reduce this risk. Nearly 70% of the excision was done from lateral portal which reduces the final leg of surgery to remaining 30% only reducing risk per se to that much only. Second, we did not use burr all the way and stopped short leaving thin posterosuperior rim to be removed with sharp arthroscopic curette and narrowline basket punch. These manual, non-motorized instruments give much better tactile feedback and removal of bone from posterosuperiorcorner without causing damage to soft tissue is that much more efficient.
Inadequacy and non-uniform resection are greater problem than excess resection. Neer[13] reported that inadequate resection of the posterior aspect of the distal clavicle during arthroscopic procedures can cause abutment with the acromion leading to pain. Pensak et al.[4] stated that even in hands of experienced arthroscopists, issues of inadequate resection of the superior aspect of the AC joint, and/or incomplete posterior resection may occur and leads to poor outcomes. He added that occasionally, one may encounter patient with a clavicle that has a large sagittal width, which can complicate the procedure and possibly compromise the outcome. Biz et al.[8] have shown use of stylus to check posterosuperior margin.
Pensak et al. point about possibility of larger sagittal width in some cases, besides already emphasized point of inaccessibility of posterosuperior corner from lateral portal, prompted us to recommend resection of about 30% to be always done from anterior portal even though all 100% length excision of anteroinferior clavicle can be safely done from lateral portal.
The use of narrowlinepunch and sharp curette coupled with only small burr from anterior portal occupying the ACJ space, with ACJ space increased for maneuvering because 70% of clavicle end have been already excised from lateral portal, with view of entire joint using 70° scope from anteroinferiorcorner, permits such good unobstructed arthroscopic visualization, and micromanagement of bone removal from posterosuperiorcorner that even in clavicle with large sagittal width incomplete resection is much less likely. And finally, calibrated probe can be placed at various points on lateral end of clavicle, in our modified technique, to gauze whether the resection is uniform or not.
CONCLUSION
Arthroscopic DCE using the modifications suggested by us may be a value addition in achieving safety, accuracy of arthroscopic DCE by indirect approach which, though, a reliable and reproducible technique for the treatment of painful osteoarthritis of the ACJ lesions in active patients engaged in overhead throwing and contact sports and heavy labor, has increased risk of stiffness due to subacromial adhesions and iatrogenic acromial stress fractures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Ravinder Kant Manocha is on the Editorial Board of the Journal.
Videos available on:
References
- Arthroscopic resection of the distal clavicle in osteoarthritis of the acromioclavicular joint. Indian J Orthop. 2016;50:379-83.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic resection of the acromioclavicular joint. Am J Sports Med. 1993;21:71-7.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of acromioclavicular joint injuries and results. Clin Sports Med. 2003;22:301-17.
- [CrossRef] [Google Scholar]
- Open versus arthroscopic distal clavicle resection. Arthroscopy. 2010;26:697-704.
- [CrossRef] [PubMed] [Google Scholar]
- Osteolysis of the distal clavicle: Long-term results of arthroscopic resection. Arthroscopy. 2000;16:600-5.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of arthroscopic resection of the distal clavicle with concomitant subacromial decompression. Arthroscopy. 2003;19:805-9.
- [CrossRef] [Google Scholar]
- Arthroscopic distal clavicle resection. Oper Tech Sports Med. 2004;12:18-26.
- [CrossRef] [Google Scholar]
- Clinical review of patients subjected to mini-Mumford arthroscopy. Muscles Ligaments Tendons J. 2012;2:137-41.
- [Google Scholar]
- Arthroscopic distal clavicle excision, Technique and early results. Clin Orthop Relat Res. 1994;301:181-4.
- [CrossRef] [Google Scholar]
- Technique for Arthroscopic Resection of the Distal Clavicle in Patients with Symptomatic Acromioclavicular Joint Osteoarthritis: A Retrospective Study. 2020
- [CrossRef] [Google Scholar]
- Arthroscopic resection of the distal clavicle with concomitant subacromial decompression: A case series. Malays Orthop J. 2014;8:59-62.
- [CrossRef] [PubMed] [Google Scholar]
- Anteroposterior instability of the distal clavicle after distal clavicle resection. Clin Orthop Relat Res. 1998;348:114-20.
- [CrossRef] [Google Scholar]






